Abstract
Background and aim: Choledochal cysts are congenital segmental aneurysmal dilatations of any portion of bile ducts, most commonly of the main portion of the common bile duct. The classification system of choledochal cysts is based on the site of the cyst or dilatation and currently includes 5 major types. The purpose of our study is to describe the imaging findings of a new variant of choledochal cyst.
Materials and Methods: Six patients (4 children and 2 adults, 4 females and 2 males, 3-67 year old) were evaluated by US, CT, CT-cholangiography, MRI, magnetic resonance cholangiopancreatography (MRCP) and endoscopic retrograde cholangiopancreatography (ERCP), because of jaundice, abdominal pain and a palpable mass.
Results: A new type of choledochal cyst was demonstrated in all cases. In this new variant apart from the dilatation of the common hepatic and the common bile duct, dilatation of the central portion of the cystic duct was also observed, giving a bicornal configuration to the cyst.
Conclusion: The imaging findings of a new variant of choledochal cyst with participation of the cystic duct are described. We propose the classification of this type of choledochal cyst as a new subtype of Todani I cyst, namely Todani ID.
Keywords: choledochal cyst, US, CT-Cholangiography, MRCP, ERCP
Choledochal cysts are congenital cystic dilatations of any portion of the bile ducts, most often occurring in the main portion of the common bile duct1-6. Although choledochal cysts are considered a disorder of childhood and infancy, the ages in reported cases range from newly born to 80 years old; however 60% of such cysts are diagnosed in patients less than 10 years old2,7.
Choledochal cysts were first described by Vater in 1723. In 1959 Alonso-Lej et al described 3 types of choledochal cysts, which were later modified by Todani et al4,8. Multiple theories try to explain the etiology of choledochal cysts. Their origin may be related to an abnormal choledochopancreaticoductal junction that allows chronic reflux of pancreatic enzymes into the bile duct, resulting in weakening and dilatation of the duct, and subsequent formation of a cyst1,9.
Materials and methods
The period 2001-2009, we evaluated 6 patients (4 children and 2 adults, 4 females and 2 males, 3-67 year old,) with several imaging modalities because of jaundice, abdominal pain and a palpable mass. The first imaging procedure for all patients was US. Axial and oblique sagittal images were obtained by a real-time Siemens Sonoline G60S device. MRI of the upper abdomen and magnetic resonance cholangiopancreatography (MRCP) were subsequently performed in all patients. MR-examinations were performed in a Siemens Expert Plus 1T scanner. Axial and coronal T2-weighted HASTE images (TR:6ms, TE:60ms), as well as axial post-contrast T1- weighted FLASH images (TR:11ms, TE:4,2ms) were obtained. Both MIP (maximum-intensity-projection) reconstruction with its source images and single-slice projection images were available for evaluation. CT examination and CT-Cholangiography were performed using a Picker 5000 PQ scanner. CT-Cholangiography was performed by intravenous infusion of hepatobiliary contrast agent (Billiscopin) during 20 minutes. One hour later axial CT images were obtained. 3-D reconstructions of CT-images were also evaluated.
Results
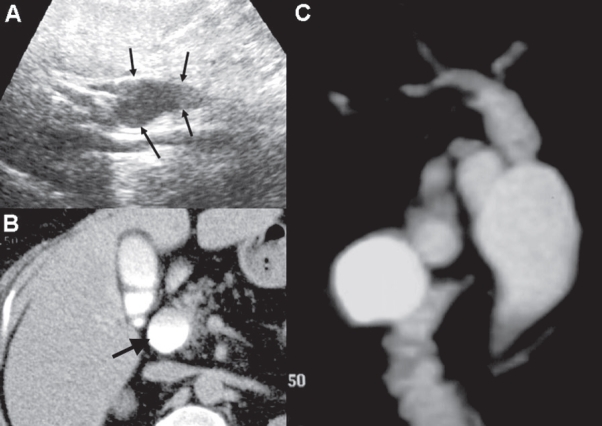
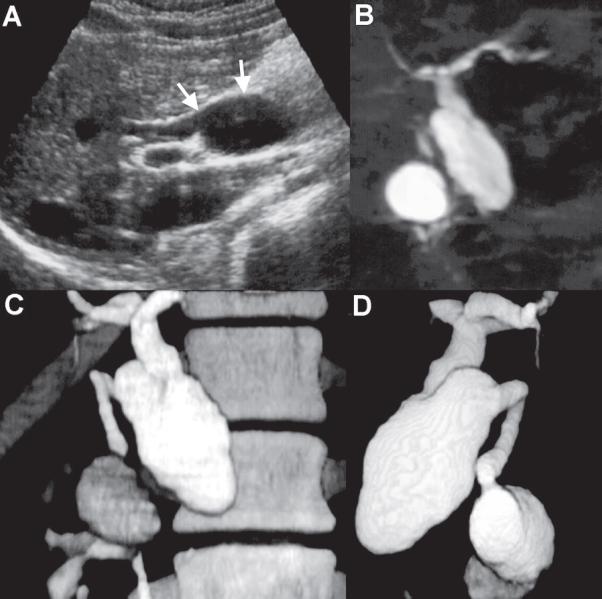
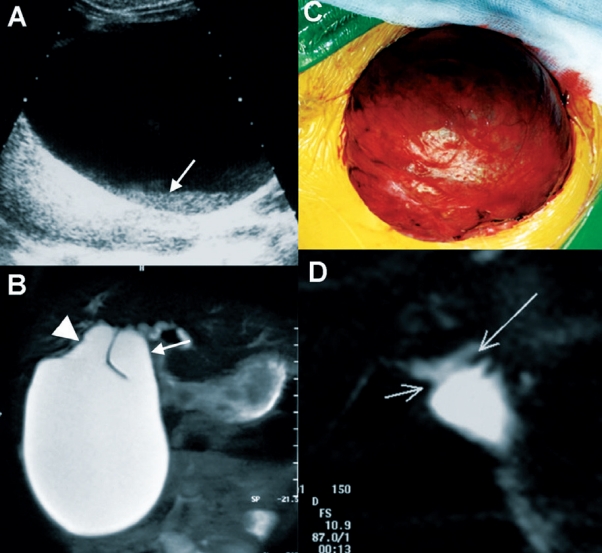
US showed cystic dilatation of the common bile duct extending towards the porta hepatis, while the gallbladder was demonstrated separate from this cyst. In one case, bile sludge was observed within the dilated duct (Figure 1A, 2A, 3A). The diagnosis of choledochal cysts was considered as the most possible, particularly in the 4 children, and further imaging evaluation was suggested.
Figure 1: A. Abdominal US, demonstrating a dilated common bile duct (arrows). B. CT after intravenous infusion of hepatobiliary contrast agent (Billiscopin) showing the dilated common bile duct (arrow). C. On MRCP, dilatation of the common bile duct, common hepatic duct and the proximal portion of the cystic duct give the choledochal cyst a bicornal configuration.
Figure 2: A. US demonstrating a dilated common and hepatic bile duct. B. MRCP and C,D. CT-Cholangiography demonstrating the bicornal configuration of the cyst due the a proximally dilated cystic duct.
Figure 3: A. A huge dilatation of the common bile duct containing bile sludge (arrow) is observed on US. B. MRCP showing an atypical Todani type I choledochal cyst with dilatation of the common bile duct, the common hepatic duct (arrow) and the proximal portion of the cystic duct (arrowhead). C. Photograph of the choledochal cyst during surgery. D. Post operative MRCP after Roux-en-Y hepaticojejunostomy.
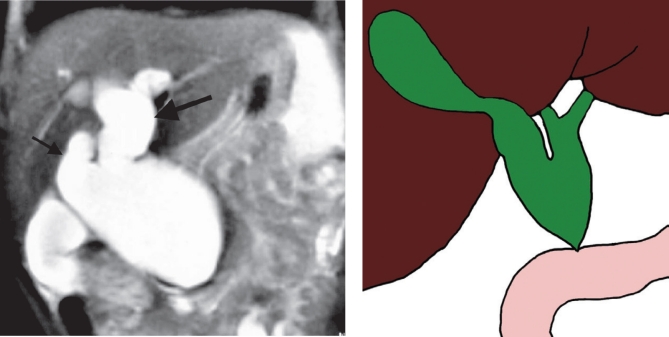
CT examination of the upper abdomen revealed a cystic mass, entering hepatic hilum and demonstrated the relationships with adjacent structures with more accuracy than ultrasonography. CT-Cholangiography and MRCP revealed choledochal cysts and even more details about the morphology of the biliary tree. There was cystic dilatation of the common hepatic and the common bile duct, which was classified as atypical Todani type I choledochal cyst. The proximal part of the cystic duct was also visualized dilated, giving a bicornal configuration to the cyst (Figure 1-4). MRCP demonstrated a normal pancreatobiliary junction in all patients. Endoscopic retrograde cholangiopancreatography (ERCP) was additionally performed in 4 cases preoperatively, and confirmed the normal pancreatobilliary union in these cases. In all patients that were operated, the surgical findings correlated exactly with the imaging findings. No coexistent malignancy was found either at surgery or at histopathologic examination.
Figure 4: A. Coronal T2-Haste image showing an atypical Todani type I choledochal cyst. Apart from the dilatation of the common bile duct, there is dilatation of the common hepatic duct (large arrow) and the proximal portion of the cystic duct (small arrow). B. Schematic representation of atypical Todani type I choledochal cyst with dilatation of the common bile duct, the common hepatic duct and the proximal portion or the cystic duct.
Discussion
Choledochal cysts are relatively rare congenital disorders of biliary tree, usually discovered in infancy or childhood. They are congenital cystic dilatations of any portion of the bile ducts, but most often occur in the main portion of the common bile duct1-6. More than twothirds of the reported cases are from Japan, with a female predominance1,2,7. The ages of reported cases range from neonates to 80 years old; however 60% of choledochal cysts are diagnosed before the age of 102,6,7.
There are many theories about the etiology of the bile duct cysts. The common channel theory proposed by Babbit et al is the most widely accepted theory. According to their theory, there is an abnormal pacreatobiliary duct union that allows reflux of pancreatic secretions into the biliary system during a critical stage of its development 9. The common bile duct and pancreatic duct normally unite within the sphincter of Oddi to form a common channel which opens into the middle portion of the duodenum. An anomalous pancreatobiliary junction has two features that are relevant to formation of choledochal cysts. One is that the union of pancreatic duct and common bile duct is located far from the duodenum, creating a long common channel. The other is the angle of this junction. Consequently chemical and enzymatic destruction of the ductal wall, leads to cystic dilatation. However, the theory of malformation of the pancreatobiliary ductal junction does not explain the occurrence of choledochal cysts in the presence of a normal pancreatobiliary ductal union, as in our cases1,10-12. An alternative hypothesis is that choledochal cysts represent a spectrum of embryonic malformation of the pancreatobiliary system, one of which may be an anomalous junction1,11,13,14.
A widely accepted classification of choledochal cysts based on anatomical location and cholangiographic morphology of the choledochal cysts was developed by Todani, who expanded the work of Along-Lej et al8. Todani and colleagues described 5 types of choledochal cysts: Type I is the most common type (80-90%). It is subdivided into type IA (cystic dilatation of the common bile duct), type IB (segmental dilatation of the common bile duct) and type IC (fusiform dilatation extending to common hepatic duct). Type II is rare (2%) and is a true diverticulum anywhere in the extrahepatic duct. Type III cyst, also referred as choledochocele, is also rare (1,4-5%) and confined to the common bile duct within the duodenal wall. Type IV cyst is more common (19%) and may be further subdivided into type IVA, which involves both the intra- and extrahepatic bile ducts, and the less common type IVB, where only extrahepatic cysts are observed. Type V, or Caroli’s disease, includes single or multiple intrahepatic bile cysts. However, this classification leads to some confusion because it includes Caroli’s disease, which seems to be a distinct disease entity. Moreover, choledochocele seems to be an anatomic variation rather than a true dilatation of the common bile duct15. Choledochal cysts in our patients were classified as Todani type I, but the morphology of the cysts was unusual. A bicornal configuration of the choledochal cysts was demonstrated in our cases due to the dilatation of the proximal portion of the cystic duct (Figure 4B). This type of choledochal cyst has not been described previously and we classify this as a subtype of Todani type I, type ID.
Histopathologically, choledochal cysts have a fibrotic wall varying in thickness from a few millimeters up to 1cm. The cyst wall consists of dense collagenous connective tissue with occasional elastic fibers and smooth muscle bundles. A complete epithelial lining is usually absent. However, scattered columnal or cuboidal epithelium can be found. An inflammatory reaction is often present. An exception is type III (choledochocele) which is lined by either duodenal or bile duct mucosa7,16.
Usually, choledochal cysts appear clinically as abdominal pain, jaundice and a palpable abdominal mass. Intermittent jaundice and an abdominal mass are the most common findings in infants 17. Complications of choledochal cysts include cholecystitis, recurrent cholangitis, biliary stricture, choledocholithiasis, recurrent acute pancreatitis and malignant transformation into cholangiocarcinoma 1,18,19. The frequency of biliary malignancy increases with age. Adult patients should be evaluated cautiously. Although excision of the cyst eliminates a potential source of carcinoma, it does not exclude the possibility of cancer developing in the intrahepatic ducts20-22.
From a surgeon's standpoint, preoperative imaging evaluation is essential for planning the operative approach to choledochal cysts. Anatomic details on the pancreatico bile duct union and the exact morphology of the duct are important factors for the surgeon to consider when determining the appropriate surgical procedure. Surgeons are also concerned about the exact location of the pancreatic duct, the site of entry into the duodenum, and the length of the common channel. Since malignancy may develop in the remaining stump after resection, surgeons prefer to resect the cyst as low as possible without causing injury to the pancreatic duct and the common channel23.
In conclusion, we describe the imaging findings of a new variant of Todani type I choledochal cyst that has not been recognized previously and we propose the classification of this variant under Todani's system, as type ID.
The authors declare that they have no conflict of interest.
References
- 1.Lee HK, Park SJ, Yi BH, Lee AL, Moon JH, Chang YW. Imaging features of adult choledochal cysts: a pictorial review. Korean J Radiol. 2009;10:71–80. doi: 10.3348/kjr.2009.10.1.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wiseman K, Buczkowski AK, Chung SW, Francoeur J, Schaeffer D, Scudamore CH. Epidemiology, presentation, diagnosis, and outcomes of choledochal cysts in adults in an urban environment. Am J Surg. 2005;189:527–531. doi: 10.1016/j.amjsurg.2005.01.025. [DOI] [PubMed] [Google Scholar]
- 3.Visser BC, Suh I, Way LW, Kang SM. Congenital choledochal cysts in adults. Arch Surg. 2004;139:855–862. doi: 10.1001/archsurg.139.8.855. [DOI] [PubMed] [Google Scholar]
- 4.Alonso-Lej F, Rever WB, Pessango DJ. Congenital Choledochal cyst, with a report of two, and an analysis of 94 cases. Int Abstr Surg. 1959;108:1–10. [PubMed] [Google Scholar]
- 5.Flanigan DP. Biliary cysts. Ann Surg. 1975;182:635–643. doi: 10.1097/00000658-197511000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Powel CS, Sawyers JL, Reynolds VH. Management of adult choledochal cysts. Ann Surg. 1981;193:666–667. doi: 10.1097/00000658-198105000-00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crittenden S, Mckinley M. Choledochal cyst-clinical features and classification. Am J Gastroenterol. 1985;80:643–647. [PubMed] [Google Scholar]
- 8.Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K. Congenital bile duct cysts: Classification, operative procedures, and review thirty-seven cases including cancer arising from choledochal cyst. Am J Surg. 1977;134:263–269. doi: 10.1016/0002-9610(77)90359-2. [DOI] [PubMed] [Google Scholar]
- 9.Babbit D, Starshak R, Clemett A. Choledochal cyst: a concept of etiology. AJR. 1973;119:57–62. doi: 10.2214/ajr.119.1.57. [DOI] [PubMed] [Google Scholar]
- 10.Ok Hwa Kim, Hong Jun Chung, Bying Gil Choi. Imaging of the choledochal cyst. RadioGraphics. 1995;15:69–88. doi: 10.1148/radiographics.15.1.7899614. [DOI] [PubMed] [Google Scholar]
- 11.Komi N, Takehara H, Kunitomo K, Miyoshi Y, Yagi T. Does the type of anomalous arrangement of pancreaticobiliary ducts influence the surgery and prognosis of choledochal cyst? J Pediat Surg. 1992;27:728–731. doi: 10.1016/s0022-3468(05)80102-2. [DOI] [PubMed] [Google Scholar]
- 12.Iwai N, Yanagihara J, Tokiwa K, Shimotake T, Nakamura K. Congenital Choledochal Dilatation with emphasis on pathophysiology of the biliary three. Ann Surg. 1992;215:27–30. doi: 10.1097/00000658-199201000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Akhan O, Demirkazik FB, Ozmen MN, Ariyurek MO. Choledochal cysts: Ultrasonographic findings and correlation with other imaging modalities. Abdom Imaging. 1994;19:243–247. doi: 10.1007/BF00203517. [DOI] [PubMed] [Google Scholar]
- 14.Matos C, Nicaise N, Devière J, Cassart M, Metens T, Struyven J. Choledochal cysts : comparison of findings at MR cholangiopancreatography and Endoscopic Retrograde Cholangiopancreatography in eight patients. Radiology. 1998;209:443–448. doi: 10.1148/radiology.209.2.9807571. [DOI] [PubMed] [Google Scholar]
- 15.Arenas-Jimenez J, Gomez-Fernandez-Montes J, Mas-Estelle's F, Cortina-Orts H. Large choledochocoele: difficulties in radiological diagnosis. Pediatr Radiol. 1999;29:807–810. doi: 10.1007/s002470050700. [DOI] [PubMed] [Google Scholar]
- 16.O'Neill JA., Jr Choledochal cyst. Current Problems in Surgery. 1992;29:361–410. doi: 10.1016/0011-3840(92)90025-x. [DOI] [PubMed] [Google Scholar]
- 17.Oldham KT, Hart MJ, White TT. Choledochal Cysts presenting in late childhood and adulthood. Am Surg. 1981;141:568–571. doi: 10.1016/0002-9610(81)90050-7. [DOI] [PubMed] [Google Scholar]
- 18.Irie H, Honda H, Jimi M, Yokohata K. Value of MR Cholangiopancreatography in evaluating choledochal cysts. AJR. 1998 ;171:1381–1385. doi: 10.2214/ajr.171.5.9798883. [DOI] [PubMed] [Google Scholar]
- 19.Sugiyama M, Atomi Y. Anomalous pancreatobiliary junction without congenital choledochal cyst. Br J Surg. 1998;85:911–916. doi: 10.1046/j.1365-2168.1998.00744.x. [DOI] [PubMed] [Google Scholar]
- 20.Todani T, Tabuchi K, Watanabe Y, Kobayashi T. Carcinoma arising in the wall of congenital bile duct cysts. Cancer. 1979;44:1134–1141. doi: 10.1002/1097-0142(197909)44:3<1134::aid-cncr2820440350>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 21.Bloustein PA. Association of carcinoma with congenital cystic conditions of the liver and bile ducts. Am J Gastroenterol. 1977;67:40–46. [PubMed] [Google Scholar]
- 22.Yoshida H, Hai Y, Minami M, Kokudo T, Ohtomo K, Kuroda A. Biliary malignancies occurring in choledochal cysts. Radiology. 1989;173:389–392. doi: 10.1148/radiology.173.2.2678253. [DOI] [PubMed] [Google Scholar]
- 23.Lam W, Lam T, Saing H, Chan Fu-Luk, Chan K-L. MR Cholangiography and CT cholangiography of pediatric patients with choledochal cysts. AJR. 1999;173:401–405. doi: 10.2214/ajr.173.2.10430145. [DOI] [PubMed] [Google Scholar]