Abstract
Objective
To assess human papillomavirus (HPV) vaccination coverage after demonstration projects conducted in India, Peru, Uganda and Viet Nam by PATH and national governments and to explore the reasons for vaccine acceptance or refusal.
Methods
Vaccines were delivered through schools or health centres or in combination with other health interventions, and either monthly or through campaigns at fixed time points. Using a two-stage cluster sample design, the authors selected households in demonstration project areas and interviewed over 7000 parents or guardians of adolescent girls to assess coverage and acceptability. They defined full vaccination as the receipt of all three vaccine doses and used an open-ended question to explore acceptability.
Findings
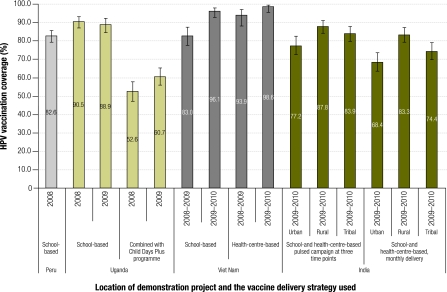
Vaccination coverage in school-based programmes was 82.6% (95% confidence interval, CI: 79.3–85.6) in Peru, 88.9% (95% CI: 84.7–92.4) in 2009 in Uganda and 96.1% (95% CI: 93.0–97.8) in 2009 in Viet Nam. In India, a campaign approach achieved 77.2% (95% CI: 72.4–81.6) to 87.8% (95% CI: 84.3–91.3) coverage, whereas monthly delivery achieved 68.4% (95% CI: 63.4–73.4) to 83.3% (95% CI: 79.3–87.3) coverage. More than two thirds of respondents gave as reasons for accepting the HPV vaccine that: (i) it protects against cervical cancer; (ii) it prevents disease, or (iii) vaccines are good. Refusal was more often driven by programmatic considerations (e.g. school absenteeism) than by opposition to the vaccine.
Conclusion
High coverage with HPV vaccine among young adolescent girls was achieved through various delivery strategies in the developing countries studied. Reinforcing positive motivators for vaccine acceptance is likely to facilitate uptake.
Résumé
Objectif
Évaluer la couverture vaccinale anti-papillomavirus humain (VPH) suite à des projets pilotes menés en Inde, au Pérou, en Ouganda et au Viet Nam par le PATH et par les gouvernements nationaux, et étudier les raisons de l’acceptation ou du refus de la vaccination.
Méthodes
Les vaccins étaient délivrés par des écoles ou des centres de soins ou conjointement à d'autres interventions sanitaires, et de façon mensuelle ou par des campagnes ponctuelles. En utilisant un échantillonnage en grappes à deux étapes, les auteurs ont sélectionné des ménages dans des zones de projet pilote et ont interrogé plus de 7 000 parents ou tuteurs d’adolescentes afin d'évaluer la couverture et l'acceptabilité du vaccin. Ils ont défini la vaccination complète comme étant la prise de l’ensemble des trois doses vaccinales et ont eu recours à des questions ouvertes pour étudier l‘acceptabilité.
Résultats
La couverture vaccinale, pour les programmes en milieu scolaire, était de 82,6% (intervalle de confiance de 95%, IC: 79,3–85,6) au Pérou, de 88,9% (IC de 95%: 84,7–92,4) en 2009 en Ouganda et de 96,1% (IC de 95%: 93.0–97,8) en 2009 au Viet Nam. En Inde, une approche de type campagne a permis de réaliser une couverture allant de 77,2% (IC de 95%: 72,4–81,6) à 87,8% (IC de 95%: 84,3–91,3), alors que la délivrance mensuelle a permis de réaliser une couverture allant de 68,4% (IC de 95%: 63,4–73,4) à 83,3% (IC de 95%: 79,3–87,3). Plus des deux tiers des personnes interrogées ont justifié l’acceptation du vaccin VPH pour les raisons suivantes: (i) il protège contre le cancer du col de l'utérus; (ii) il empêche la maladie, ou (iii) les vaccins sont bons. Le refus était plus souvent justifié par des considérations liées au programme (par ex. l’absentéisme scolaire) que par une opposition au vaccin.
Conclusion
Une couverture élevée du vaccin VPH parmi les jeunes filles a été obtenue par différentes stratégies de délivrance dans les pays en voie de développement à l’étude. Le renforcement des éléments de motivation positifs pour l’acceptation du vaccin est susceptible d'en faciliter la prise.
Resumen
Objetivo
Evaluar la cobertura de la vacunación del virus del papiloma humano (VPH) después de los proyectos de demostración llevados a cabo por PATH y los gobiernos nacionales en la India, Perú, Uganda y Vietnam, así como examinar las razones de aceptación o rechazo de la vacuna.
Métodos
Las vacunas se suministraron en colegios o centros de salud, o en combinación con otras intervenciones sanitarias, mensualmente o por medio de campañas realizadas en momentos específicos. Mediante el uso de un diseño de muestreo por conglomerados de dos fases, los autores seleccionaron hogares en áreas del proyecto de demostración y entrevistaron a más de 7000 padres o tutores de niñas adolescentes para evaluar su cobertura y aceptabilidad. Definieron la vacunación completa como el momento en el que se habían recibido las tres dosis de vacuna y utilizaron una pregunta de interpretación abierta para examinar la aceptabilidad.
Resultados
La cobertura de la vacunación en programas realizados en colegios fue del 82,6% (Intervalo de confianza del 95%, IC: 79,3–85,6) en Perú, 88,9% (IC del 95%: 84,7–92,4) en Uganda, en el año 2009, y del 96,1% (IC del 95%: 93,0–97,8) en Vietnam, también en el año 2009. En la India, un enfoque de campaña consiguió del 77,2% (IC del 95%: 72,4–81,6) al 87,8% (95% IC: 84,3–91,3) de cobertura, mientras que el suministro mensual consiguió una cobertura del 68,4% (IC del 95%: 63,4–73,4) al 83,3% (95% IC: 79,3–87,3). Más de dos tercios de los participantes indicaron como razones para la aceptación de la vacuna del VPH que: (i) protege del cáncer de cuello de útero; (ii) previene la enfermedad o (iii) las vacunas son buenas. El rechazo fue más habitual en base a consideraciones programáticas (p. ej., absentismo escolar) que por el rechazo a la vacuna.
Conclusión
Con la vacuna del VPH se consiguió una alta cobertura entre chicas adolescentes jóvenes mediante diversas estrategias de suministro en los países en desarrollo estudiados. Es probable que el refuerzo de las motivaciones positivas para la aceptación de facilite su aceptación.
ملخص
الغرض
قياس التغطية بالتلقيح المضاد لفيروسة الورم الحليمي البشري بعد مشاريع عملية توضيحية أجريت في الهند، وبيرو، وأوغندا، وفيتنام من قبل منظمة باث PATH والحكومات الوطنية لاستكشاف أسباب قبول أو رفض اللقاح.
الطريقة
جرى تقديم اللقاحات في المدارس والمراكز الصحية وعبر التدخلات الصحية الأخرى، سواء شهرياً أو من خلال حملات محددة التوقيت. وباستخدام تصميم لعينة عنقودية على مرحلتين، اختار الباحثون أسراً في مناطق المشروع التوضيحي، واجروا مقابلات مع أكثر من 7000 من الآباء أو الأوصياء على الفتيات المراهقات لقياس التغطية باللقاح والمقبولية له. وقد عَرَّفَ الباحثون التلقيح التام بأنه تلقي الجرعات الثلاث من اللقاح، واستخدموا أسئلة غير مقيدة الإجابات لاستكشاف المقبولية.
النتائج
بلغت نسبة التغطية في البرامج المدرسية 82.6% (فاصلة الثقة 95%: 79.3 – 85.6) في بيرو، و 88.9% (فاصلة الثقة 95%: 84.7 – 92.4) في عام 2009 في أوغندا، و 96.1% (فاصلة الثقة 95%: 93.0 – 97.8) في عام 2009 في فيتنام. وفي الهند، حقق أسلوب الحملة تغطية بلغت 77.2% (فاصلة الثقة 95%: 72.4 – 81.6) إلى 87.8% (فاصلة الثقة 95%: 84.3 -91.3)، بينما حقق التلقيح الشهري تغطية بلغت 68.4% (فاصلة الثقة 95%: 63.4 – 73.4 ) إلى 83.3% (فاصلة الثقة 95%: 79.3 – 87.3). أكثر من ثلثي المجيبين على الاستبيان ذكروا أن من أسباب قبولهم للقاح فيروسة الورم الحليمي: 1) أنه يحمي من سرطان عنق الرحم؛ 2) ويمنع الإصابة بالمرض؛ 3) ولأن اللقاحات مفيدة. وكان الرفض يعود غالباً لاعتبارات برنامجية (مثل تغيب التلاميذ في المدارس) وليس إلى المعارضة لإعطاء اللقاح.
الاستنتاج
أمكن تحقيق تغطية مرتفعة بلقاح فيروسة الورم الحليمي بين المراهقات الصغيرات باستراتيجيات مختلفة في البلدان النامية التي أجريت فيها الدراسة. ومن المتوقع أن يؤدي تعزيز الدوافع الإيجابية لقبول اللقاح إلى تيسير استخدامه.
摘要
目的
旨在评估美国帕斯适宜卫生科技组织(PATH)和各国政府在印度、秘鲁、乌干达和越南进行示范项目之后人乳头瘤病毒(HPV)疫苗覆盖率并探讨接受或拒绝疫苗的原因。
方法
疫苗通过学校、医疗站或连同其他健康干预措施一起每月或通过特定卫生日的重大活动提供。运用二阶段整群抽样设计,作者选择示范项目区域内的家庭并采访了7000多名青春期少女的父母或监护人以评估疫苗的覆盖率和可接受性。作者将充分接种定义为接受所有三次疫苗注射,还运用开放式问题探讨疫苗的可接受性。
结果
基于学校的项目疫苗接种覆盖率如下:秘鲁82.6%(95%可信区间:79.3-85.6),2009年乌干达为88.9%(95%可信区间:84.7-92.4),2009年越南为96.1%(95%可信区间:93.0-97.8)。在印度,开展重大活动方法取得了77.2%(95%可信区间:72.4-81.6)到87.8%(95%可信区间:84.3-91.3)的覆盖率,然而按月接种只取得了68.4%(95%可信区间:63.4-73.4)到83.3%(95%可信区间:79.3-87.3)的覆盖率。超过三分之二的调查对象给出的接受人乳头瘤病毒疫苗的原因为:(1)能够防止宫颈癌;(2)能够预防疾病;或(3)疫苗是好东西。拒绝疫苗接种往往是方案因素(如逃学)所致,而不是反对疫苗。
结论
青春期少女人乳头瘤病毒疫苗的高覆盖率是通过所研究的发展中国家的不同接种策略实现的。加强疫苗接受的积极激励因素有可能促进疫苗接种。
Резюме
Цель
Оценить охват вакцинацией против вируса папилломы человека (ВПЧ) после проведения демонстрационных проектов во Вьетнаме, Индии, Перу и Уганде некоммерческой организацией PATH («Программа оптимальных технологий в здравоохранении») и правительствами этих стран, и исследовать причины согласия на вакцинацию или отказа от нее.
Методы
Вакцинация проводилась в школах, медицинских центрах или в сочетании с другими медико-санитарными мерами вмешательства, ежемесячно либо, в рамках кампаний, через определенные промежутки времени. Используя план двухэтапной кластерной выборки, авторы провели отбор домохозяйств в районах проведения демонстрационного проекта и интервьюировали более семи тысяч родителей или опекунов девочек-подростков с целью оценки охвата и приемлемости вакцинации. Они определили полную вакцинацию как введение всех трех доз вакцины, а для исследования приемлемости использовали вопрос с открытым ответом.
Результаты
Охват вакцинацией в программах на базе школ составил: в Перу 82,6% (95% доверительный интервал, ДИ: 79,3–85,6); в Уганде в 2009 году – 88,9% (95% ДИ: 84,7–92,4); во Вьетнаме в 2009 году – 96,1% (95% ДИ: 93,0–97,8). В Индии концепция проведения вакцинации в форме кампании позволила обеспечить охват в пределах от 77,2 (95% ДИ: 72,4–81,6) до 87,8% (95% ДИ: 84,3–91,3), в то время как ежемесячный прием вакцины позволил добиться охвата в пределах от 68,4 (95% ДИ: 63,4–73,4) до 83,3% (95% ДИ: 79,3–87,3). Более 2/3 респондентов отметили, что согласились на вакцинацию против ВПЧ потому, что вакцина: (i) защищает от рака шейки матки; (ii) предотвращает заболевание, или (iii) является качественной. Отказ был чаще обусловлен программными соображениями (напр., пропуском занятий в школе), чем отрицательным отношением к вакцине.
Вывод
Широкий охват девочек-подростков вакцинацией против ВПЧ в обследованных развивающихся странах был достигнут благодаря использованию разнообразных стратегий вакцинации. Применение положительных стимулов, скорее всего, будет способствовать повышению числа обращений в медучреждения по поводу вакцинации.
Introduction
The global burden of cervical cancer is large and is increasing and it disproportionately affects low-resource countries.1 In 2008 there were approximately 529 000 new cases and over 270 000 deaths, of which nearly 85% occurred in developing countries,1 most often among women serving as caregivers and breadwinners in their communities.2 Cervical cancer prevention programmes in developed countries, which are based on regular Papanicolaou (Pap) smears and appropriate treatment of precancerous lesions, have succeeded in reducing disease incidence and mortality since the 1970s,3 but this expensive approach may prove difficult to implement and sustain in low-resource settings.4,5 However, the Expanded Programme on Immunization (EPI), which has helped to reduce infectious disease rates and infant and child mortality throughout the world, provides a tested and effective infrastructure that could be used to prevent cervical cancer by adding the human papillomavirus (HPV) vaccine to the schedule.6–8
The recent introduction of two highly efficacious vaccines against HPV – the necessary cause of cervical cancer – opens up new possibilities for disease prevention.9 These vaccines can reduce cervical cancer deaths by more than 60% and the largest effects have been reported in countries that have received subsidized vaccine through the GAVI Alliance.10 Vaccines against HPV are recommended by the World Health Organization (WHO) for girls aged 9 to 13 years before their sexual debut11 and are prequalified (i.e. evaluated for the quality, safety and efficacy) for United Nations purchase. Recently, the GAVI Alliance announced a price of 5 United States dollars (US$) per dose for HPV vaccine,12 a sum that approaches affordability for low-resource countries that are eligible for subsidized vaccine purchase and that increases the likelihood that the vaccine will be introduced.
From 2006 to 2010, PATH, a global nongovernmental health organization, collaborated with the governments of India, Peru, Uganda and Viet Nam to gather evidence that would support decisions on whether and how to introduce HPV vaccines. Research was carried out in two phases: formative research and demonstration projects. During formative research, each country’s sociocultural environment and the capacity of its health system and policy pathways were investigated before introducing HPV vaccination.13 The results guided the development of the demonstration projects, which operated for 1 or 2 years in each country.14–17 For each country and each strategy within a country, the principal research question was what level of HPV vaccination coverage – successful receipt of all three doses by the target population – could be achieved.
This paper reports the HPV vaccination coverage achieved and the reasons that made individuals accept or decline vaccination. This information will assist government deliberations on the introduction of HPV vaccine programmes, particularly in low-resource settings. In-depth qualitative research on the acceptability of the HPV vaccine, the feasibility of different delivery strategies and the economic and programme costs of vaccine delivery were evaluated in separate studies and have been reported elsewhere.18
Methods
HPV vaccine demonstration projects
The HPV vaccine demonstration projects were designed in partnership with the ministry of health, subnational health and education sector organizations and other key stakeholders in each country. Project locations were selected on the basis of the cervical cancer disease burden, the size of the target population, the local performance of the EPI, the interests of local health authorities, socioeconomic status, ethnic or linguistic diversity and geographical area. One of three vaccine delivery strategies was followed: school-based vaccination, health-centre-based vaccination or vaccination combined with other health interventions. Eligible girls were selected either according to their grade in school or their age at the time of the first vaccine dose (Table 1). Programmes in India used a combination of school- and health-centre-based delivery, with delivery either at three fixed time points (i.e. a campaign approach) or once a month for the duration of the programme (i.e. a routine delivery approach). Although the programmes were implemented in limited geographical areas, these were large enough to cover complete administrative boundaries and be broadly representative of the programme’s capacities and the country’s population. This enabled the results to be used for scaling up future programmes.
Table 1. Human papillomavirus (HPV) vaccine delivery strategies in demonstration projects, India, Peru, Uganda and Viet Nam, 2008–2010.
| Country | Area | Delivery strategy | Vaccination year | No. of eligible girlsa |
|---|---|---|---|---|
| Peru | Piura region | School-based, selection by school grade, fifth grade selected | 2008 | 8092 |
| Uganda | Ibanda district | School-based, selection by school grade, primary five classb selected | 2008 | 3459 |
| 2009 | 2835c | |||
| Nakasongola district | Combined with Child Days Plus programme, selection by age, 10-year-olds selected | 2008–2009 | 2263d | |
| 2009 | 1923c | |||
| Viet Nam | Quan Hoa, Nong Cong and Ninh Kieu districts | School-based, selection by grade, sixth grade selected; supplemented by health-centre-based by age, 11-year-olds selectede | 2008–2009 | 2412 |
| 2009–2010 | 1890c | |||
| Quan Hoa, Nong Cong and Binh Thuy districts | Health-centre-based, selection by age, 11-year-olds selected | 2008–2009 | 1507 | |
| 2009–2010 | 1205c | |||
| India | Khamman district, Andhra Pradesh | School-based for girls in school and health-centre-based for girls out of school, pulsed campaign at three fixed time points, selection by age, 10- to 14-year-olds selected | 2009–2010 | 14 533 |
| Vadodara district, Gujarat | School-based for girls in school and health-centre-based for girls out of school, routine monthly vaccination, selection by age, 10- to 14-year-olds selected | 2009–2010 | 12 636 | |
| Total | – | – | – | 52 755 |
a The number of eligible girls was determined by enumerating and creating a list of those eligible according to the delivery strategy criteria in each country before administration of the first vaccine dose.
b The term ”class” is used in Uganda instead of “grade”, but has the same meaning.
c The number of eligible girls was lower in the second year than in the first because of population movements, primarily migration out of the area.
d This figure is the census estimate of the number of girls aged 10 years rather than that obtained by direct enumeration.
e Only for girls who were not enrolled in or attending school.
All vaccination programmes used existing EPI structures and staff and therefore reflected routine conditions. National and local steering groups were involved in programme planning and implementation, which followed typical microplanning for routine immunization.19 In accordance with WHO guidelines on the introduction of new vaccines,20 each demonstration project included: (i) comprehensive training on cervical cancer, HPV vaccines and programme logistics for health workers, teachers, community mobilizers and others involved in programme implementation; (ii) information, education and communication materials for girls, their parents and the wider community; (iii) prevaccination assessment of cold storage and transport; (iv) adverse event monitoring; and (v) supportive supervision.
Written parental consent or authorization was obtained in India and Peru and during the first year in Viet Nam; community consent was obtained in Uganda and during the second year in Viet Nam, in accordance with the recommendations of the respective ministries of health.
The HPV vaccines were donated to PATH by Merck & Co. Incorporated, United States of America, and GlaxoSmithKline, United Kingdom of Great Britain and Northern Ireland. All demonstration projects began after the vaccine had been licensed and registered in each country.
Study design
A cross-sectional study of HPV vaccination coverage and acceptability was performed in each country. This involved a population-based household survey that was adapted from WHO guidelines for infant immunization surveys.21
For surveys in India, Peru and Uganda and for the first year in Viet Nam, a two-stage cluster sample design was used.21 The primary sampling unit or cluster was the census district or census enumeration area within the prespecified geographical boundary of the vaccination programme. In rural areas, this comprised one or more contiguous villages; in urban areas, it comprised predefined urban blocks. The secondary sampling unit was the household within each cluster. Each country’s census department, with the exception of Peru’s, drew the sample using recent data and provided a list of clusters and locations to the research team. In Peru, the research team randomly selected clusters after each available cluster within the geographical boundary of the programme was enumerated and listed. The selection of households started at a central or randomly selected location in the cluster and progressed from house to house using the next-nearest-household approach.22 For the second-year survey in Viet Nam, systematic random sampling from a complete census of all eligible households was used.21 The sample was drawn for each of the two vaccination strategies from three geographical areas in which the programme was implemented (i.e. six separate samples). A random number generator determined the starting point and the sampling interval and was applied to each list of households that contained girls eligible for vaccination.
Households with eligible girls were visited up to three times if a parent or guardian was absent at the first or second visit. A respondent was any adult who could verify the girl’s HPV vaccination status and respond accurately to survey questions; parents were preferred. Surveys were carried out 1 to 3 months after administration of the third vaccine dose.
The size of each survey sample was determined from the expected or observed level of vaccination coverage for the delivery strategy employed, using a precision estimate of ± 5%, a design effect of 2 and a 95% confidence interval (CI).21 In total, 19 separate samples were drawn (Table 2, available at: http://www.who.int/bulletin/volumes/89/11/11-089862): one in Peru (one geographical area, 1 year); four in Uganda (two geographical areas, 2 years); six in India (three geographical areas in each of two districts); and eight in Viet Nam (one for each of the two strategies in the first year and six in the second year). The six samples from the second year in Viet Nam were aggregated into two samples for data analysis to reflect the two delivery strategies used.
Table 2. Survey samples used for assessing human papillomavirus (HPV) vaccination coverage in demonstration projects, India, Peru, Uganda and Viet Nam, 2008–2010.
| Country | Vaccine delivery strategy | Vaccination year | Estimated vaccination coverage (%) | No. of clusters × no. of girls | Sample size (n) |
||
|---|---|---|---|---|---|---|---|
| Expected | Final | Final for analysis | |||||
| Peru | School-based | 2008 | 80 | 70 × 8 | 560 | 580 | 575a |
| Uganda | School-based | 2008 | 85 | 40 × 10 | 400 | 400 | 400b |
| 2009 | 90 | 28 × 10 | 280 | 280 | 280 | ||
| Combined with Child Days Plus programme | 2008–2009 | 85 | 40 × 10 | 400 | 400 | 361c | |
| 2009 | 70 | 80 × 8 | 640 | 640 | 448d | ||
| Viet Nam | School-based | 2008–2009 | 80 | 20 × 25 | 500 | 500 | 500 |
| 2009–2010 | 95 | NAe | 285 | 285 | 285 | ||
| Health-centre-based | 2008–2009 | 90 | 20 × 14 | 280 | 280 | 280 | |
| 2009–2010 | 95 | NAe | 219 | 219 | 219 | ||
| India | School- and health-centre-based, pulsed campaign at three time points | 2009–2010 | 70 | 132 × 15 | 1980f | 1976 | 1948g |
| School- and health-centre-based, monthly delivery | 2009–2010 | 70 | 132 × 15 | 1980f | 1980 | 1973h | |
| Total | – | – | – | – | 7585 | 7540 | 7269 |
NA, not applicable.
a The analysis excluded five survey responses because the girls were not in the fifth school grade, as required by the vaccination strategy.
b School grades were missing for four girls but were assumed to be grade five.
c The analysis excluded 39 survey responses because the girls who were vaccinated were not 10 years old, as required by the vaccination strategy.
d The analysis excluded 192 survey responses because either the girls who were vaccinated were not 10 years old, as required by the vaccination strategy, or the girl was actually vaccinated in the first year of the programme rather than the second.
e Systematic random sampling from a complete census of all eligible households was used in the second year.
f There were 660 girls in each of three urban blocks.
g The analysis excluded 28 survey responses because the girls who were vaccinated were not aged between 10 and 14 years, as required by the vaccination strategy.
h The analysis excluded seven survey responses because the girls who were vaccinated were not aged between 10 and 14 years, as required by the vaccination strategy.
Outcomes of interest
The main outcome measure was the level of HPV vaccination coverage among eligible girls, which was defined as the percentage of households with eligible girls who had been fully vaccinated (i.e. had received all three doses of HPV vaccine). In addition, the level of partial vaccination coverage was defined as the percentage of households with eligible girls who had received only one or two vaccine doses. The percentage of households with eligible girls who received no vaccine was also calculated. Even though it was possible for a household to contain more than one girl eligible for HPV vaccination, this was a rare occurrence. Therefore, the descriptor households with eligible girls was used as a surrogate for the descriptor eligible girls in our coverage calculations. Reasons for accepting or not accepting vaccination were assessed using an open-ended question without prompting a response.
Outcomes were assessed in the same way in all four countries. The study was not designed to detect differences between countries or delivery strategies. Doing so would have been difficult because each country selected the delivery strategy best suited to its local circumstances. It was not possible to control for the magnitude of the variation in vaccine programme implementation within and between countries, such as the variation associated with differences in programme structure, human resources and infrastructure.
Data collection and analysis
Data were collected using a standardized structured questionnaire based on the WHO infant immunization survey.21 Also recorded were the basic demographic characteristics, age and school grade of the eligible girl; the dates of vaccination; the respondent’s exposure to information, education and communication materials and messages about vaccination; and the respondent’s beliefs about vaccines and the HPV vaccine. The questionnaires were developed in English, then translated into and administered in local languages.
Vaccination coverage estimates are reported with their 95% CIs. Responses to open-ended questions were translated into English, categorized according to theme and recoded into categorical or binary variables for analysis. All other variables were reported using descriptive statistics. Data were analysed using SAS v. 9.1.3 (SAS Institute, Cary, United States of America) or SPSS v. 10 (SPSS Inc., Chicago, USA).
Ethical considerations
Informed verbal consent to the survey was obtained from all respondents, who were free to withdraw at any time or to refuse to answer any question. Respondents in India, Peru and Uganda were not compensated financially; a small token of appreciation was given in Viet Nam, in accordance with local custom. The surveys were approved by institutional review boards in each country and in the United States.
Results
In total, 7540 respondents participated in the surveys. However, 271 records were excluded because the eligibility criteria for vaccination had not been met. Thus, the analysis was performed using 7269 records. One eligible household in Peru refused to respond to the survey, but there was no refusal in any other country. The majority of respondents (range across countries: 77.0–92.0%) were parents, mainly mothers (Table 3, available at: http://www.who.int/bulletin/volumes/89/11/11-089862). Overall, 537 schools and 672 health facilities in India, 264 schools and 161 health facilities in Peru, 417 schools and 69 health facilities in Uganda and 38 schools and 72 health facilities in Viet Nam participated in the demonstration projects. Most girls were attending school and were aged between 9 and 14 years (Table 3).
Table 3. Human papillomavirus vaccination coverage survey, survey respondents and girls eligible for vaccination, India, Peru, Uganda and Viet Nam, 2008–2010.
| Vaccine delivery strategy | Peru |
Uganda |
Viet Nam |
India |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| School-based |
School-based |
Combined with Child Days Plus programme |
School-based |
Health-centre-based |
School- and health-centre-based, pulsed campaign at three time points |
School- and health centre-based, monthly delivery |
||||||||||
| 2008 | 2008 | 2009 | 2008–2009 | 2009 | 2008–2009 | 2009–2010 | 2008–2009 | 2009–2010 | 2009–2010 | 2009–2010 | ||||||
| Respondents, no. | 575 | 400 | 280 | 361 | 448 | 500 | 285 | 280 | 219 | 1948 | 1973 | |||||
| Mother, no. (%) | 421 (74) | 243 (61) | 151(54) | 225 (63) | 272 (61) | 346 (69) | 177 (63) | 200 (71) | 123 (57) | 1246 (64) | 1147 (58) | |||||
| Father, no. (%) | 44 (8) | 89 (23) | 74 (26) | 52 (14) | 70 (16) | 65 (13) | 64 (23) | 58 (21) | 71 (33) | 437 (22) | 449 (23) | |||||
| Other adult relative, no. (%) | 105 (18) | 46 (12) | 36 (13) | 52 (14) | 84 (19) | 53 (11) | 29 (11) | 14 (5) | 15 (7) | 231 (12) | 374 (19) | |||||
| Other adult, no. (%) | 1 (< 1) | 18 (5) | 19 (7) | 30 (8) | 21 (5) | 36 (7) | 13 (5) | 8 (3) | 8 (4) | 34 (2) | 3 (< 1) | |||||
| Age of eligible girl,a,b no. (%) | ||||||||||||||||
| < 10 years | 16 (3) | 5 (1) | 3 (1) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| 10 years | 257 (45) | 18 (5) | 21 (8) | 361 (100) | 448 (100) | 22 (4) | 27 (9) | 29 (10) | 26 (12) | 123 (6) | 130 (6) | |||||
| 11 years | 198 (34) | 38 (10) | 42 (15) | 0 | 0 | 150 (30) | 126 (44) | 188 (67) | 137 (63) | 394 (20) | 350 (18) | |||||
| 12 years | 69 (12) | 79 (20) | 40 (14) | 0 | 0 | 2 (< 1) | 5 (2) | 0 | 0 | 538 (28) | 446 (23) | |||||
| 13 years | 20 (3) | 101 (25) | 63 (23) | 0 | 0 | 1 (< 1) | 0 | 0 | 0 | 495 (25) | 488 (25) | |||||
| 14 years | 9 (2) | 88 (22) | 55 (20) | 0 | 0 | 0 | 0 | 0 | 0 | 398 (20) | 559 (28) | |||||
| > 14 years | 6 (1) | 66 (17) | 30 (11) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| School grade of eligible girl,a,b,c no. (%) | ||||||||||||||||
| Not regularly attending school | 0 | 0 | 0 | 0 | 2 (< 1) | 0 | 0 | 0 | 0 | 179 (9) | 505 (26) | |||||
| Grade 1 or 2 | 0 | 0 | 0 | 70 (19) | 96 (21) | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| Grade 3 | 0 | 0 | 0 | 156 (43) | 162 (36) | 0 | 0 | 0 | 0 | 4 (< 1) | 8 (< 1) | |||||
| Grade 4 | 0 | 0 | 0 | 91 (25) | 120 (27) | 2 (< 1) | 1 (< 1) | 1 (< 1) | 1 (< 1) | 34 (2) | 45 (2) | |||||
| Grade 5 | 575 (100) | 400d (100) | 280 (100) | 33 (9) | 46 (10) | 10 (2) | 11 (4) | 12 (4) | 6 (3) | 173 (9) | 168 (9) | |||||
| Grade 6 | 0 | 0 | 0 | 7 (2) | 8 (2) | 472 (94) | 268 (94) | 256 (91) | 207 (95) | 369 (19) | 338 (17) | |||||
| Grade 7 | 0 | 0 | 0 | 0 | 0 | 1 (< 1) | 0 | 5 (2) | 0 | 412 (21) | 354 (18) | |||||
| Grade 8 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 338 (17) | 265 (13) | |||||
| Above grade 8 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 439 (23) | 289 (15) | |||||
a At administration of the first vaccine dose, as reported by survey respondents.
b The totals may not add up to 100% of all respondents because some data on age, date of birth, school enrolment or school grade were missing.
c The term “grade” has been adopted generically even though India uses the term “standard”, Peru and Viet Nam use the term ”grade” and Uganda uses the term ”class”, all which have the same meaning.
d School grades were missing for four girls but were assumed to be grade five.
Vaccination coverage
High HPV vaccination coverage was achieved with all delivery strategies except for the Child Days Plus programme in Uganda (Fig. 1). The coverage achieved through school-based programmes was 82.6% (95% CI: 79.3–85.6) in Peru and 88.9% (95% CI: 84.7–92.4) in 2009 in Uganda, and it increased between the first and second years in Viet Nam, from 83.0% (95% CI: 77.6–87.3) to 96.1% (95% CI: 93.0–97.8). In India, where a combination of school- and health-centre-based delivery was used, the coverage achieved by the campaign approach at three fixed time points ranged from 77.2% (95% CI: 72.4–81.6) to 87.8% (95% CI: 84.3–91.3) depending on the type of geographical area (i.e. urban, rural or tribal); similar findings were observed with the routine delivery approach, in which vaccine was offered once per month. The highest coverage was achieved with the health-centre-based programme in Viet Nam: 98.6% (95% CI: 95.7–99.6) in the second year; the lowest coverage was found with the Child Days Plus programme in Uganda, in which girls were vaccinated on the basis of age: coverage was 52.6% (95% CI: 47.3–57.9) in the first year.
Fig. 1.
Human papillomavirus (HPV) vaccination coveragea in demonstration projects, India, Peru, Uganda and Viet Nam, 2008–2010b
a Full vaccination was defined as the receipt of all three vaccine doses.
b The error bars represent 95% confidence intervals.
The percentage of eligible girls who were either partially vaccinated or not vaccinated at all varied between countries and by delivery strategy. In the school-based programme in Uganda, about 6.0% were partially vaccinated and 4.0% were not vaccinated in each of the two years. In the Child Days Plus programme in Uganda, over 25.0% of 10-year-old girls did not receive any dose of HPV vaccine, while 21.0% and 13.0% received fewer than three doses in the first and second years, respectively. These findings contrast with those in the other countries where a girl who received a first dose was highly likely to complete the three-dose series: only 1.3% were partially vaccinated in Peru, compared with less than 1.0% in Viet Nam and with 2.0% and 3.0% in India with the campaign approach and with routine delivery, respectively.
Reasons for accepting or declining vaccination
More than two thirds of all respondents indicated that they had their daughters vaccinated primarily to protect them against cervical cancer, to prevent disease in general or because they believed that vaccines are good for health (Table 4). Reasons linked to the vaccination programme itself were mentioned less frequently, although “following the advice of others” was a common reason in all countries. That the vaccine was free of charge was often mentioned in Peru and that the government was providing the vaccine was a reason commonly given in Uganda and Viet Nam. Most parents or guardians surveyed stated at least two reasons for having their daughters vaccinated.
Table 4. Parents’ and guardians’ reasons for accepting or not accepting human papillomavirus (HPV) vaccination, India, Peru, Uganda and Viet Nam, 2008–2010.
| Vaccine delivery strategy | Peru |
Uganda |
Viet Nam |
India |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| School-based |
School-based |
Combined with Child Days Plus programme |
School-based |
Health-centre-based |
School- and health-centre-based, pulsed campaign at three time points |
School- and health-centre-based, monthly delivery |
||||||||||
| 2008 | 2008 | 2009 | 2008–2009 | 2009 | 2008–2009 | 2009–2010 | 2008–2009 | 2009–2010 | 2009–2010 | 2009–2010 | ||||||
| Survey respondents, no. | 575 | 400 | 280 | 361 | 448 | 500 | 285 | 280 | 219 | 1948 | 1973 | |||||
|
Reason for accepting full vaccinationa,b |
||||||||||||||||
| Responses, no. | 475 | 362 | 249 | 190 | 272 | 415 | 274 | 263 | 216 | 1617 | 1487 | |||||
| Protection against cervical cancer, no. (%) | 369 (78) | 248 (69) | 152 (61) | 104 (55) | 143 (53) | 203 (49) | 118 (43) | 116 (44) | 111 (51) | 859 (53) | 649 (44) | |||||
| Prevention of disease or infection, no. (%) | 13 (3) | 203 (56) | 109 (44) | 107 (56) | 144 (53) | 217 (52) | 208 (76) | 137 (52) | 144 (67) | 307 (19) | 176 (12) | |||||
| Vaccines thought good for health or wanted girl to be healthy, no. (%) | 20 (4) | 218 (60) | 138 (55) | 124 (65) | 154 (57) | 199 (48) | 117 (43) | 111 (42) | 96 (44) | 696 (43) | 520 (35) | |||||
| Any of the three reasons above, no. (%) | 388 (82) | 294 (81) | 210 (84) | 180 (95) | 228 (84) | 380 (92) | 253 (92) | 241 (92) | 203 (94) | 1530 (95) | 1010 (68) | |||||
| Other reasons for accepting full vaccination, no. (%) | ||||||||||||||||
| Government programme | 3 (< 1) | 66 (18) | 51 (21) | 13 (7) | 56 (21) | 81 (20) | 79 (29) | 31 (12) | 69 (32) | 11 (< 1) | 97 (7) | |||||
| Vaccine is free | 129 (27) | 8 (2) | 7 (3) | 22 (12) | 19 (7) | 53 (13) | 38 (14) | 36 (14) | 31 (14) | 59 (4) | 163 (11) | |||||
| Followed others’ advice | 81 (17) | 85 (23) | 15 (6) | 43 (23) | 81 (30) | 151 (36) | 77 (28) | 8 (3) | 41 (19) | 273 (17) | 772 (52) | |||||
| Information was convincing | 85 (18) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| School was providing it to every child | 11 (2) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 28 (2) | 348 (23) | |||||
| Fear of cancer | NA | NA | 61 (24) | NA | 80 (29) | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| Knows someone who had cervical cancer | 0 | 18 (5) | 26 (10) | 10 (5) | 12 (4) | 16 (4) | 0 | 10 (4) | 0 | 0 | 5 (< 1) | |||||
| Reason for partial or non-vaccinationa | ||||||||||||||||
| Responses, no. | 100 | 38 | 31 | 171 | 176 | 85 | 11 | 17 | 3 | 331 | 486 | |||||
| School absenteeism, no. (%) | 21 (21) | 23 (61) | 29 (94) | 64 (37) | 73 (41) | 14 (17) | 3 (27) | 2 (12) | 1 (33) | 60 (18) | 86 (18) | |||||
| Programme-related issues, no. (%) | ||||||||||||||||
| Was not aware of the programme | 9 (9) | 3 (8) | 3 (10) | 50 (29) | 41 (23) | 5 (6) | 0 | 2 (12) | 0 | 99 (30) | 195 (40) | |||||
| Eligibility was difficult to determine | 4 (4) | 0 | 0 | 59 (35) | 30 (17) | 2 (2) | 0 | 5 (29) | 0 | 7 (2) | 16 (3) | |||||
| Vaccine-related issues, no. (%) | ||||||||||||||||
| Concerns about safety | 7 (7) | 0 | 1 (3) | 3 (2) | 10 (6) | 28 (33) | 5 (45) | 1 (6) | 0 | 23 (7) | 17 (3) | |||||
| Vaccine is new | 0 | 0 | 0 | 0 | 0 | 13 (15) | 0 | 2 (12) | 0 | 0 | 0 | |||||
| Vaccine is experimental | 26 (26) | 1 (3) | 0 | 0 | 0 | 4 (5) | 0 | 3 (18) | 0 | 0 | 0 | |||||
| Impact on fertility | 1 (1) | 0 | 1 (3) | 1 (< 1) | 1 (< 1) | 10 (12) | 0 | 0 | 0 | 0 | 1 (< 1) | |||||
| Insufficient information about the vaccine | 5 (5) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| Fear of injections | 8 (8) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 7 (2) | 52 (11) | |||||
| Do not believe vaccine is good for health | 0 | 0 | 0 | 0 | 0 | 27 (32) | 2 (18) | 1 (6) | 0 | 12 (4) | 4 (1) | |||||
| Allergic to vaccines | 23 (23) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| Followed the advice of others | 20 (20) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| Vaccine encourages early sexual activity | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||||
NA, not available.
a More than one response was allowed. Only the most frequently reported responses are presented and non-responses are not included. As a result, totals may not add to 100% of all responses.
b Full vaccination was defined as the receipt of all three vaccine doses.
The parents and guardians of girls who were partially vaccinated or not vaccinated at all gave similar reasons for non-acceptance, which were often directly related to the vaccine delivery strategy (Table 4). In Peru, the the most frequently cited reasons were the belief that the HPV vaccine was “experimental”, “allergies” and “following the advice of others”. With the Child Days Plus delivery strategy in Uganda, in which girls were selected by age, the most frequently cited reasons for non-vaccination were a lack of awareness of the programme and difficulty in determining the girl’s eligibility. In India, a lack of programme awareness and, in India, Peru and Uganda, school absenteeism were also commonly given as reasons for non-vaccination. Concerns about the safety of the vaccine and its possible experimental nature were mentioned in Viet Nam, mostly in one urban location.
Discussion
Some policy-makers and researchers have pointed out the potential difficulties of implementing HPV vaccination in developing countries. They attribute them to the fact that the vaccine targets older girls, protects against a sexually transmitted virus, requires three doses, confers its benefit later in life and may be unaffordable.9,23–26 However, this study clearly shows that a range of HPV vaccine delivery strategies can be successful in low-resource settings. The coverage levels achieved resemble those obtained with vaccination programmes in high-income countries: 65.1% uptake of the first dose in British Columbia, Canada;27 68.5% uptake of two doses in Manchester, United Kingdom;28 and 26.7% and 55.0% coverage with three doses in the United States29 and southern Australia,30 respectively. Although our study involved demonstration projects, admittedly not reflective of routine field conditions, HPV vaccination was conducted in large, geographically distinct areas using only the infrastructure already in place for the EPI. Consequently, our findings could well provide evidence of what could be achieved should these strategies be adopted nationally.
In the demonstration projects, the criteria for selecting the eligible population seemed to be as important as the location where the girls were vaccinated. In Uganda, for example, the coverage achieved by the school-based programme, in which eligible girls were selected by school grade, differed from the coverage achieved by the Child Days Plus programme, which was also school-based but selected eligible girls by age (Fig. 1). Keeping accurate track of a person’s age is generally not perceived as important in Ugandan culture; hence birth certificates and other proof of age are not routinely available.The low vaccination coverage attained in Uganda may therefore have resulted from the eligibility criteria used to select vaccine recipients rather than from the Child Days Plus strategy itself. By contrast, selection by age posed no challenge in either India or Viet Nam, where age documentation was readily available.
Although concerns have arisen regarding the level of school attendance in developing countries,9,11,23,25,31 we found the rates to be very high in all areas. Moreover, the high vaccination coverage achieved in school-based programmes suggests that schools can be used to reach young adolescent girls. Nevertheless, ways of reaching girls who are out of school or absent on vaccination days must be considered in any delivery strategy.
A particular strength of our study was its assessment of parents’ reasons for having had their daughters vaccinated after vaccine was offered. Most published studies of HPV vaccine acceptability have been based on hypothetical vaccination offers rather than actual vaccination.32–34 Although some studies suggest that knowing about cervical cancer, HPV and HPV vaccines is necessary for vaccine acceptance,35,36 others report that this knowledge correlates poorly with acceptance32 and does not predict behaviour.36 Our data also indicate that parents’ primary motivation for having their daughters vaccinated was their perception that the HPV vaccine was good for health, prevented cancer and prevented disease in general, rather than specific knowledge of cervical cancer or HPV. A recent study of hypothetical vaccine acceptability in India found that the HPV vaccine was accepted even by people who knew relatively little about HPV or cervical cancer.33 Support for immunization in general was the driving factor behind vaccine acceptance.33 In our study, responses across countries, cultures and religions were strikingly and unexpectedly consistent, which suggests that parents worldwide are motivated by similar factors when making decisions about their children’s health. Framing community awareness messages in terms of “cancer prevention” could also have had an influence.37
Finally, parents whose daughters were only partially vaccinated or not vaccinated at all cited reasons that were primarily associated with the vaccination programme, whose schedule can be modified, rather than opposition to the vaccine itself. The main barriers to vaccination were girls being absent from school on the vaccination day, limited awareness of the vaccination programme, insufficient information about cervical cancer, the HPV vaccine or the HPV vaccination programme, and difficulty in determining a girl’s eligibility. Insufficient information has also been found to contribute to vaccine refusal in developed countries.27,28 Future HPV vaccination programmes could overcome these barriers by more attentive planning and community sensitization. Contrary to some study findings,38,39 not a single parent in our study mentioned the fear of sexual disinhibition or early sexual activity as a reason for not accepting HPV vaccination. This is consistent with findings elsewhere.28,40
Study limitations
Adaptation of the population-based survey of parents recommended by WHO for assessing infant immunization may not be reliable for determining the immunization status of older populations. In addition, the households surveyed may have contained more than one eligible girl and our estimates of vaccine coverage may not be precise. However, since most programmes vaccinated only a single cohort, the probability that there was more than one eligible girl in a household was very low. Moreover, some households with eligible girls may have been excluded because data collection was difficult in remote areas. Any inferences about HPV vaccine delivery strategies in low-resource settings based on our study findings are limited by the fact that the study did not directly compare strategies across or within countries. Nevertheless, since the demonstration projects made use of the infrastructure and human resources that were already in place for the routine EPI and covered large areas within each country, the lessons learned about the coverage achievable with different delivery strategies may be highly relevant for deciding how best to introduce vaccination nationally. Another limitation is that the responses given by guardians may have been less accurate than those given by parents. However, guardians were very few. There is potential for recall bias because surveys were administered 1 to 3 months after the vaccination programme. Since the reasons for vaccination or non-vaccination were explored using an open-ended question, responses may have been misclassified by survey administrators. However, this risk was reduced by training and quality assurance checks during response coding. Finally, although in each country we used a representative sample of the parents of girls who were eligible for HPV vaccination, our findings may not be generalizable to other countries.
Conclusion
This is the first population-based survey of the parents and guardians of girls who are eligible for HPV vaccination in developing countries. It shows that high vaccination coverage can be achieved through a variety of strategies for reaching young adolescent girls. In low-resource settings, the vaccine can be effectively administered in schools or health centres or incorporated into the existing community-based delivery of other health interventions. Setting appropriate selection criteria for the eligible population using either age or school grade is critical. Reinforcing positive motivators – cancer prevention, good health and well-being and the perception of vaccines as hugely beneficial public health interventions – could enhance acceptability in communities and increase vaccination coverage.
The next step is replicating or scaling-up the programme in our project countries and ensuring its sustainability. Uganda and Viet Nam are continuing to provide HPV vaccine in the communities involved in the demonstration projects as part of government immunization programmes. Further lessons on sustainability will be learned. However, all eyes are on Peru, which began to provide HPV vaccination to all 10-year-old girls in April 2011.41 Success there will depend to some extent on the lessons learned from this study when scaling up vaccination. With the financial commitment of the GAVI Alliance and the technical support of WHO, areas with large burdens of cervical cancer may soon be able to introduce the HPV vaccine and substantially reduce mortality from the disease.
Acknowledgements
The authors are grateful to those who assisted with the study: Martha Jacob, Satish Kaipilyawar, Irfan Khan, Sanjeev Singh, Uma Shankar, Seema Narwekar and Kishore Chaudry in India; Rosario Bartolini, Maria Ana Mendoza and Irma Ramos in Peru; Rachel Seruyange, Irene Mwenyango, Patrick Isingoma and Possy Mugyenyi in Uganda; and Nguyen Tran Hien, Dang Thi Thanh Huyen, Nguyen Van Cuong, Ngo Thi Kim Hoa and Nguyen Thi Ngoc Diep in Viet Nam; as well as Robin Biellik, Jenny Winkler, Allison Bingham and Vivien Tsu. They also thank national, subnational, provincial, regional, district, sub-centre and commune immunization and education programmes and staff; national stakeholders; research staff; all institutions involved in the HPV vaccine demonstration projects; research institutions that carried out the coverage surveys; staff based at PATH headquarters; their partners at GlaxoSmithKline and Merck & Co. Inc.; the Bill & Melinda Gates Foundation; and all study participants, especially the young girls in India, Peru, Uganda and Viet Nam. Amynah Janmohamed, Aisha Jumaan and Nghi Quy Nguyen were employed by PATH during the study.
Funding:
This study was funded by a grant to PATH from the Bill & Melinda Gates Foundation. PATH did not enter into an agreement with the funding organization that limited its ability to complete the research as planned and had full control of all primary data.
Competing interests:
None declared.
References
- 1.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 2.Wittet S, Tsu V. Cervical cancer prevention and the Millennium Development Goals. Bull World Health Organ. 2008;86:488–90. doi: 10.2471/BLT.07.050450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mathew A, George PS. Trends in incidence and mortality rates of squamous cell carcinoma and adenocarcinoma of cervix – worldwide. Asian Pac J Cancer Prev. 2009;10:645–50. [PubMed] [Google Scholar]
- 4.Brown RE, Breugelmans JG, Theodoratou D, Bénard S. Costs of detection and treatment of cervical cancer, cervical dysplasia and genital warts in the UK. Curr Med Res Opin. 2006;22:663–70. doi: 10.1185/030079906X99972. [DOI] [PubMed] [Google Scholar]
- 5.Insinga RP, Dasbach EJ, Elbasha EH. Assessing the annual economic burden of preventing and treating anogenital human papillomavirus-related disease in the US: analytic framework and review of the literature. Pharmacoeconomics. 2005;23:1107–22. doi: 10.2165/00019053-200523110-00004. [DOI] [PubMed] [Google Scholar]
- 6.State of the world’s vaccines and immunization. 3rd ed. Geneva: World Health Organization; 2009. [Google Scholar]
- 7.Lim SS, Stein DB, Charrow A, Murray CJ. Tracking progress towards universal childhood immunisation and the impact of global initiatives: a systematic analysis of three-dose diphtheria, tetanus, and pertussis immunisation coverage. Lancet. 2008;372:2031–46. doi: 10.1016/S0140-6736(08)61869-3. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention Global routine vaccination coverage, 2009. MMWR Morb Mortal Wkly Rep. 2010;59:1367–71. [PubMed] [Google Scholar]
- 9.Luciani S, Jauregui B, Kieny C, Andrus JK. Human papillomavirus vaccines: new tools for accelerating cervical cancer prevention in developing countries. Immunotherapy. 2009;1:795–807. doi: 10.2217/imt.09.48. [DOI] [PubMed] [Google Scholar]
- 10.Goldie SJ, O’Shea M, Campos NG, Diaz M, Sweet S, Kim SY. Health and exonomic outcomes of HPV 16, 18 vaccination in 72 GAVI-eligible countries. Vaccine. 2008;26:4080–93. doi: 10.1016/j.vaccine.2008.04.053. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization Human papillomavirus vaccines, WHO position paper. Wkly Epidemiol Rec. 2009;15:117–32. [PubMed] [Google Scholar]
- 12.GAVI welcomes lower prices for life-saving vaccines. Geneva: GAVI Alliance; 2011. Available from: http://www.gavialliance.org/library/news/press-releases/2011/gavi-welcomes-lower-prices-for-life-saving-vaccines/ [accessed 8 August 2011].
- 13.Bingham A, Janmohamed A, Bartolini R, Creed-Kanashiro HM, Katahoire AR, Khan I, et al. An approach to formative research in HPV vaccine introduction planning in low-resource settings. Open Vaccine J. 2009;2:1–16. doi: 10.2174/1875035400902010001. [DOI] [Google Scholar]
- 14.Katahoire RA, Jitta J, Kivumbi G, Murokora D, Arube WJ, Siu G, et al. An assessment of the readiness for introduction of the HPV vaccine in Uganda. Afr J Reprod Health. 2008;12:159–72. [PubMed] [Google Scholar]
- 15.Bartolini RM, Drake JK, Creed-Kanashiro HM, Díaz-Otoya MM, Mosqueira-Lovón NR, Penny ME, et al. Formative research to shape HPV vaccine introduction strategies in Peru. Salud Publica Mex. 2010;52:226–33. doi: 10.1590/S0036-36342010000300007. [DOI] [PubMed] [Google Scholar]
- 16.Nghi NQ, LaMontagne DS, Bingham A, Rafiq M, Phuong Mai LT, Phuong Lien NT, et al. Human papillomavirus vaccine introduction in Vietnam: formative research findings. Sex Health. 2010;7:262–70. doi: 10.1071/SH09123. [DOI] [PubMed] [Google Scholar]
- 17.Jacob M, Mawar N, Menezes L, Kaipilyawar S, Gandhi S, Khan I, et al. Assessing the environment for introduction of human papillomavirus vaccine in India. Open Vaccine J. 2010;3:96–107. doi: 10.2174/1875035401003010096. [DOI] [Google Scholar]
- 18.Penny M, Bartolini R, Mosqueira NR, Lamontagne DS, Mendoza MA, Ramos I, et al. Strategies to vaccinate against cancer of the cervix: feasibility of a school-based HPV vaccination program in Peru. Vaccine. 2011;29:5022–30. doi: 10.1016/j.vaccine.2011.04.078. [DOI] [PubMed] [Google Scholar]
- 19.Microplanning for immunization service delivery using the reaching every district (RED) strategy Geneva: World Health Organization, Department of Immunization, Vaccines and Biologicals; 2009. [Google Scholar]
- 20.Vaccine introduction guidelines: adding a vaccine to a national immunization program – decision and implementation (WHO/IVB/05.18). Geneva: World Health Organization, Department of Immunization, Vaccines and Biologicals; 2005. [Google Scholar]
- 21.Immunization coverage cluster survey – reference manual (WHO/IVB/04.23). Geneva: World Health Organization, Department of Immunization, Vaccines and Biologicals; 2005. [Google Scholar]
- 22.Module 7. The EPI coverage survey: training for mid-level managers (MLM) Geneva: World Health Organization, Department of Immunization, Vaccines and Biologicals; 2008. [Google Scholar]
- 23.Preparing for the introduction of HPV vaccines: policy and programme guidance for countries Geneva: World Health Organization, Department of Reproductive Health and Research; 2006. [Google Scholar]
- 24.Kaufmann AM, Schneider A. New paradigm for prevention of cervical cancer. Eur J Obstet Gynecol Reprod Biol. 2007;130:25–9. doi: 10.1016/j.ejogrb.2006.07.048. [DOI] [PubMed] [Google Scholar]
- 25.Brabin L, Greenberg DP, Hessel L, Hyer R, Ivanoff B, Van Damme P. Current issues in adolescent immunization. Vaccine. 2008;26:4120–34. doi: 10.1016/j.vaccine.2008.04.055. [DOI] [PubMed] [Google Scholar]
- 26.Das BC, Hussain S, Nasare V, Bharadwaj M. Prospects and prejudices of human papillomavirus vaccines in India. Vaccine. 2008;26:2669–79. doi: 10.1016/j.vaccine.2008.03.056. [DOI] [PubMed] [Google Scholar]
- 27.Ogilvie G, Anderson M, Marra F, McNeil S, Pielak K, Dawar M, et al. A population-based evaluation of a publicly-funded school-based HPV vaccine program in British Columbia, Canada: parental factors associated with HPV vaccine receipt. PLoS Med. 2010;7:e1000270. doi: 10.1371/journal.pmed.1000270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brabin L, Roberts SA, Stretch R, Baxter D, Chambers G, Kitchener H, et al. Uptake of first two doses of human papillomavirus vaccine by adolescent schoolgirls in Manchester: prospective cohort study. BMJ. 2008;336:1056–8. doi: 10.1136/bmj.39541.534109.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention National, state, and local area vaccination coverage among adolescents aged 13–17 years–United States, 2008. MMWR Morb Mortal Wkly Rep. 2010;59:1018–23. [PubMed] [Google Scholar]
- 30.Watson M, Shaw D, Molchanoff L, McInnes C. Challenges, lessons learned and results following the implementation of a human papilloma virus school vaccination program in South Australia. Aust N Z J Public Health. 2009;33:365–70. doi: 10.1111/j.1753-6405.2009.00409.x. [DOI] [PubMed] [Google Scholar]
- 31.Human papillomavirus and HPV vaccines: technical information for policy-makers and health professionals Geneva: World Health Organization, Department of Immunization, Vaccines and Biologicals; 2007. [Google Scholar]
- 32.Allen JD, Coronado GD, Williams RS, Glenn B, Escoffery C, Fernandez M, et al. A systematic review of measures used in studies of human papillomavirus (HPV) vaccine acceptability. Vaccine. 2010;28:4027–37. doi: 10.1016/j.vaccine.2010.03.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Madhivanan P, Krupp K, Yashodha MN, Marlow L, Klausner JD, Reingold AL. Attitudes toward HPV vaccination among parents of adolescent girls in Mysore, India. Vaccine. 2009;27:5203–8. doi: 10.1016/j.vaccine.2009.06.073. [DOI] [PubMed] [Google Scholar]
- 34.Becker-Dreps S, Otieno WA, Brewer NT, Agot K, Smith JS. HPV vaccine acceptability among Kenyan women. Vaccine. 2010;28:4864–7. doi: 10.1016/j.vaccine.2010.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zimet GD, Liddon N, Rosenthal SL, Lazcano-Ponce E, Allen B. Chapter 24: Psychological aspects of vaccine acceptability. Vaccine. 2006;24(Suppl. 3):S201–9. doi: 10.1016/j.vaccine.2006.06.017. [DOI] [PubMed] [Google Scholar]
- 36.Lenselink CH, Gerrits MJ, Massuger L, van Hamont D, Bekkers R. Parental acceptance of human papillomavirus vaccines. Eur J Obstet Gynecol Reprod Biol. 2008;137:103–7. doi: 10.1016/j.ejogrb.2007.02.012. [DOI] [PubMed] [Google Scholar]
- 37.Leader AE, Weiner JL, Kelly BJ, Hornik RC, Cappella JN. Effects of information framing on human papillomavirus vaccination. J Womens Health (Larchmt) 2009;18:225–33. doi: 10.1089/jwh.2007.0711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zimet GD, Mays RM, Sturm LA, Ravert AA, Perkins SM, Juliar BE. Parental attitudes about sexually transmitted infection vaccination for their adolescent children. Arch Pediatr Adolesc Med. 2005;159:132–7. doi: 10.1001/archpedi.159.2.132. [DOI] [PubMed] [Google Scholar]
- 39.Bharadwaj M, Hussain S, Nasare V, Das BC. HPV & HPV vaccination: issues in developing countries. Indian J Med Res. 2009;130:327–33. [PubMed] [Google Scholar]
- 40.Ferris DG, Cromwell L, Waller JL, Horn L. Most parents do not think receiving human papillomavirus vaccine would encourage sexual activity in their children. J Low Genit Tract Dis. 2010;14:179–84. doi: 10.1097/LGT.0b013e3181d41806. [DOI] [PubMed] [Google Scholar]
- 41.Ministerio de Salud. Peru. Resolución Ministerial No. 070-2011. El peruano 2011 2 February. Spanish. Available from: http://www.tvperu.gob.pe/noticias/politica/presidente/18244-presidente-lanza-campana-de-vacunacion.html [accessed 24 August 2011].