Abstract
Objective
To explore excess paediatric mortality after discharge from Kilifi District Hospital, Kenya, and its duration and risk factors.
Methods
Hospital and demographic data were used to describe post-discharge mortality and survival probability in children aged < 15 years, by age group and clinical syndrome. Cox regression models were developed to identify risk factors.
Findings
In 2004–2008, approximately 111 000 children were followed for 555 000 person–years. We analysed 14 971 discharges and 535 deaths occurring within 365 days of discharge. Mortality was higher in the post-discharge cohort than in the community cohort (age-adjusted rate ratio, RR: 7.7; 95% confidence interval, CI: 6.6–8.9) and declined little over time. An increased post-discharge mortality hazard was found in children aged < 5 years with the following: weight-for-age Z score < −4 (hazard ratio, HR: 6.5); weight-for-age Z score > −4 but < −3 (HR: 3.4); hypoxia (HR: 2.3); bacteraemia (HR: 1.8); hepatomegaly (HR: 2.3); jaundice (HR: 1.8); hospital stay > 13 days (HR: 1.8). Older age was protective (reference < 1 month): 6–23 months, HR: 0.8; 2–4 years, HR: 0.6. Children with at least one risk factor accounted for 545 (33%) of the 1655 annual discharges and for 39 (47%) of the 83 discharge-associated deaths.
Conclusion
Hospital admission selects vulnerable children with a sustained increased risk of dying. The risk factors identified provide an empiric basis for effective outpatient follow-up.
Résumé
Objectif
Explorer la surmortalité infantile après la sortie de l’Hôpital de District de Kilifi, au Kenya, ainsi que sa durée et ses facteurs de risque.
Méthodes
Des données médicales et démographiques ont été utilisées pour décrire la mortalité suite à une sortie de l’hôpital et la probabilité de survie parmi les enfants âgés de moins de 15 ans, par groupe d’âge et par syndrome clinique. Des modèles de régression de Cox ont été développés pour identifier les facteurs de risque.
Résultats
Entre 2004 et 2008, environ 111 000 enfants ont été suivis, pour 555 000 personnes-ans Nous avons analysé 14 971 sorties et 535 décès survenus dans les 365 jours suivant la sortie. La mortalité était plus élevée dans la cohorte ayant quitté l’hôpital que dans la cohorte communautaire (rapport du taux en fonction de l’âge, RA: 7,7; intervalle de confiance à 95%, lC: de 6,6 à 8,9) et n'a que peu décliné avec le temps. On a constaté un risque de mortalité suite à la sortie de l’hôpital accru chez les enfants âgés de moins de 5 ans, avec les données suivantes: z-score poids/âge < −4 (rapport de risque, RR: 6,5); z-score poids/âge > −4 mais < −3 (RR: 3,4); hypoxie (RR: 2,3); bactériémie (RR: 1,8); hépatomégalie (RR: 2,3) ; jaunisse (RR: 1,8); hospitalisation > 13 jours (RR: 1,8). Un âge plus élevé était protecteur (référence < 1 mois): de 6 à 23 mois, RR: 0,8; de 2 à 4 ans, RR : 0,6. Les enfants présentant au moins un facteur de risque représentaient 545 (33%) des 1655 sorties annuelles de l’hôpital et 39 (47%) des 83 décès associés à la sortie de l'hôpital.
Conclusion
L’admission hospitalière sélectionne les enfants fragiles présentant un risque de décès accru. Les facteurs de risques identifiés fournissent une base empirique pour un suivi efficace des patients non hospitalisés.
Resumen
Objetivo
Examinar la sobremortalidad pediátrica tras el alta hospitalaria en el Hospital del Distrito de Kilifi (Kenia), así como su duración y factores de riesgo.
Métodos
Se emplearon datos hospitalarios y demográficos para describir la mortalidad tras el alta hospitalaria y la probabilidad de supervivencia en niños menores de 15 años, por franja de edad y síndrome clínico. Se elaboraron modelos de regresión de Cox para identificar los factores de riesgo.
Resultados
En 2004-2008, se siguieron aproximadamente 111 000 niños hasta un total de 555 000 años-persona. Analizamos 14 971 altas hospitalarias y 535 fallecimientos ocurridos en los 365 días siguientes al alta hospitalaria. La mortalidad fue mayor en la cohorte post-alta que en la cohorte de la comunidad (razón de tasas ajustada según la edad, RT: 7,7; intervalo de confianza del 95%, IC: 6,6-8,9) y decreció ligeramente con el tiempo. En niños menores de 5 años se encontró un mayor riesgo de mortalidad post-alta, junto con los siguientes estadísticos: puntuación Z de peso para la edad < −4 (cociente de riesgos instantáneos [hazard ratio, HR]: 6,5); puntuación Z de peso para la edad > −4 pero < −3 (HR: 3,4); hipoxia (HR: 2,3); bacteriemia (HR: 1,8); hepatomegalia (HR: 2,3); ictericia (HR: 1,8); estancia en el hospital > 13 días (HR: 1,8). A mayor edad el riesgo era menor (referencia < 1 mes): 6-23 meses, HR: 0,8; 2-4 años, HR: 0,6). Los niños con al menos un factor de riesgo representaban 545 (33%) de las 1655 altas anuales y 39 (47%) de los 83 fallecimientos relacionados con el alta.
Conclusión
En el ingreso hospitalario se selecciona a los niños vulnerables con un mayor riesgo de muerte constante. Los factores de riesgo identificados proporcionan una base empírica para un seguimiento ambulatorio eficaz.
مخلص
الغرض
تحري زيادة وفيات الأطفال بعد تخريجهم من مستشفى مقاطعة كيليفي في كينيا، ومدتها وعوامل اختطارها.
الطريقة
استخدمت معطيات المستشفى والمعطيات الديموغرافية لوصف الوفيات التالية للتخريج من المستشفى واحتمال البقاء قيد الحياة بين الأطفال أقل من عمر 15 سنة، وفقاً للفئة العمرية، والمتلازمة الإكلينيكية. وأعدت نماذج تحوّف كوكس Cox لتحديد عوامل الاختطار.
الموجودات
في الفترة 2004-2008، جرى متابعة حوالي 111000 طفل أي 555000 فرد في تلك السنوات. وحلل الباحثون 14971 طفلاً تم تخريجهم و 535 وفاة حدثت خلال 365 يوماً من التخريج من المستشفى. وكانت الوفيات أعلى في الأتراب الذين أخرجوا من المستشفى عنها في الأتراب من سائر المجتمع (نسبة معدل العمر المُصَحّح: 7.7؛ وفاصلة الثقة 95%: 6.6-8.9)، وتراجعت الوفيات قليلاً مع مرور الوقت. ووجد زيادة في خطر الوفاة بعد التخريج من المستشفى في الأطفال أقل من عمر 5 سنوات ولديهم ما يلي: حرز Z للوزن لقاء العمر أقل من -4 (نسبة الخطر: 6.5)؛ وحرز z للوزن لقاء العمر أكبر من -4 ولكن أقل من -3 (نسبة الخطر: 3.4)؛ نقص التأكسج (نسبة الخطر: 2.3)؛ تجرثم الدم (نسبة الخطر: 1.8)؛ ضخامة الكبد (نسبة الخطر: 2.3)؛ اليرقان (نسبة الخطر: 1.8)؛ البقاء في المستشفى لأكثر من 13 يوماً (نسبة الخطر: 1.8). وكان لكبر العمر تأثير وقائي (المرجعية أقل من شهر واحد): 6-23 شهراً، نسبة الخطر: 0.8؛ 2-4 سنوات، نسبة الخطر: 0.6. وبلغ عدد الأطفال الذين لديهم عامل اختطار واحد على الأقل وجرى تخريجهم 545 طفلاً (33%) ممن جرى تخريجهم سنوياً وعددهم 1655، وبلغ عدد الوفيات بين هؤلاء الأطفال 39 وفاة (47%) من الوفيات التي ارتبطت بالتخريج من المستشفى وعددها 83 وفاة.
الاستنتاج
العلاج بالمستشفى ينتقي الأطفال الضعفاء ولديهم اختطار مرتفع ومستمر للتعرض للوفاة. وتعد عوامل الاختطار المكتشفة أساساً تجريبياً للمتابعة الفعّالة للمرضى بعد تخريجهم من المستشفى.
Резюме
Цель
Исследовать избыточную педиатрическую смертность после выписки из окружной больницы в Килифи (Кения), а также ее сроки и факторы риска.
Методы
Для описания смертности после выписки из больницы, а также вероятности выживания детей в возрасте до 15 лет, с разбивкой по возрастным группам и клиническим синдромам, использовались данные больницы и демографических исследований. Для выявления факторов риска разрабатывались модели регрессии Кокса.
Результаты
В 2004–2008 годах наблюдались около 111 тыс. детей, что составило 555 тыс. человеко-лет. Мы проанализировали 14 971 выписку и 535 случаев смерти, наступивших в течение 365 дней после выписки. Смертность была выше в когорте больных после выписки, чем в когорте, охватывавшей общину в целом (коэффициент показателя, скорректированный по возрасту, КСВ: 7,7; 95% доверительный интервал, ДИ: 6,6–8,9) и со временем незначительно снижалась. Повышенный риск смертности после выписки был отмечен у детей в возрасте до 5 лет со следующими параметрами: Z-счет по индексу масса тела–возраст меньше −4 (коэффициент риска, КР: 6,5); Z-счет по индексу масса тела–возраст больше −4, но меньше −3 (КР: 3,4); гипоксия (КР: 2,3); бактериемия (КР: 1,8); увеличение печени (КР: 2,3); инфекционный гепатит (КР: 1,8); пребывание в больнице более 13 дней (КР: 1,8). Дети более старшего возраста были лучше защищены (референтный период – до 1 месяца): 6–23 месяцев, КР: 0,8; 2–4 года, КР: 0,6. Дети с одним и более факторами риска составляли 545 (33%) из 1655 случаев выписки в год и 39 (47%) из 83 случаев смерти, связанных с выпиской.
Вывод
При поступлении в больницу отбираются уязвимые дети с устойчиво повышенным риском летального исхода. Выявленные факторы риска составляют эмпирическую базу для эффективного последующего амбулаторного наблюдения больных.
摘要
目的
旨在探索从肯尼亚基利菲地区医院出院后超额儿童死亡率及其持续时间和风险因素。
方法
医院和人口数据用来描述以年龄组和临床症状分类的15岁以下儿童出院后的死亡率和存活率。Cox回归模型用来确定风险因素。
结果
2004到2008年间,我们对约111 000名儿童进行了555 000人年的追踪调查。我们分析了14 971例出院病例,其中535例死亡发生在出院后365天内。与社区人群相比,出院后人群的死亡率较高(年龄调整率比:7.7;95%置信区间:6.6-8.9),并且随着时间的推移略有下降。具有下述特征且年龄小于5岁的儿童出院后死亡风险增加:年龄体重Z评分<−4(风险比:6.5);年龄体重Z评分>4但<3 (风险比:3.4);组织缺氧(风险比:2.3);菌血症(风险比:1.8);肝肿大(风险比:2.3);黄疸(风险比:1.8);住院超过13天(风险比:1.8)。年龄较大具有保护性(参考<1个月):6-23个月,风险比:0.8;2-4岁,风险比:0.6。最少具有一项风险因素的儿童占年度1655例出院病例的33%(545例),占与出院相关的死亡病例的47%(39/83)。
结论
住院对虚弱儿童有持续增加的死亡风险。所确立的风险因素为有效门诊随访提供了经验基础。
Introduction
The Integrated Management of Childhood Illness (IMCI) programme and inpatient guidelines of the World Health Organization (WHO) aim to standardize and improve the care of critically ill children at health facilities across Africa.1–4 While the IMCI may reduce in-hospital child mortality,5 its recommendations for the prevention and management of illness following discharge are based on limited evidence from the field and are rarely implemented. Several studies from developing countries have shown that children admitted to hospital and discharged alive are at increased risk of death for 12 months following discharge when compared with similar children in the community. Furthermore, malnutrition, anaemia, hypoxaemia, longer hospitalization and discharge against medical advice exacerbate this risk.6–12 Additional data are needed to guide the development of strategies for effective follow-up care that will reduce post-discharge mortality.
In Kilifi district, Kenya, infant and child mortality have dropped sharply in recent years, yet only one third of child deaths occur in hospital and access to hospital care for severely ill children is poor.13 Previous data suggest that children who are discharged from hospital have a higher risk of dying during the 12-month period following discharge than comparable children in the community and that diarrhoea is a significant predictor of excess mortality.6 In this study we sought to determine whether hospital admission could be characterized as an acute event with an impact on short-term mortality or as a marker of chronic frailty associated with an increased risk of dying over the longer term. We analysed 5 years of linked demographic and paediatric hospital surveillance data in a rolling cohort of approximately 111 000 children aged less than 15 years at any one time, with detailed clinical and laboratory information available for all admissions. To guide hospital discharge policies and focus outpatient follow-up on high-risk groups, we estimated the burden and duration of excess mortality associated with hospital discharge and identified demographic and clinical risk factors for death in the post-discharge period.
Methods
This study was conducted in Kilifi district, a poor, rural area on the Indian Ocean coast of Kenya. The KEMRI/Wellcome Trust Research Programme has conducted laboratory, clinical and epidemiologic research in Kilifi for two decades. Kilifi District Hospital (KDH) in Kilifi town provides primary care and inpatient referral services for the entire district, following national and WHO management guidelines. The Kilifi Health and Demographic Surveillance Study (KHDSS) collects information on births, deaths and migrations in a population of 240 000 people residing in an 891 km2 area around KDH. Beginning in April 2002, all patients hospitalized in the paediatric ward or paediatric high-dependency unit at the KDH had their hospital records, including standard clinical and laboratory data, linked to their demographic records with a unique personal identifier. The linked hospital and demographic databases enable us to monitor life events after hospital discharge for residents of the Health and Demographic Surveillance Study (HDSS) area.
This analysis included all children < 15 years of age who were residents of the KHDSS area at some point in 2004–2008. We included discharges from 1 January 2003 onwards with follow-up time left truncated at 1 January 2004 to obtain information on post-discharge status for children who resided in the area in 2003 and were followed into 2004. In a single-discharge analysis, we considered only the first discharge observed for each child. Children entered the community cohort at the latest of birth, in-migration or 1 January 2004, and they exited at the earliest of death, out-migration, first discharge from hospital or 31 December 2008. Children entered the post-discharge cohort at the latest of first discharge from hospital or 1 January 2004 and exited at the earliest of death, out-migration, 365-days post-discharge or 31 December 2008. We also performed a multiple-discharge analysis in which we created duplicate records to allow children who were admitted to hospital more than once to contribute person–time (and deaths) to several post-discharge periods simultaneously. Entry and exit criteria for the post-discharge and community cohorts were analogous to those applied in the single-discharge model.
We compared mortality rates in the community and post-discharge cohorts and calculated crude and age-adjusted mortality rate ratios (RRs). We included a continuous term for post-discharge category to test for trends in mortality RR over the post-discharge period. To estimate the rate and proportion of deaths associated with hospital discharge in the post-discharge cohort and for the entire population, we used a standardized mortality approach in which we compared the observed number of deaths in the post-discharge cohort with the number of deaths expected from age-specific community mortality rates.
We constructed Kaplan–Meier survival curves and built two proportional hazards models to identify predictors of mortality in discharged children. In Model A we examined the effects of age, calendar time, number of previous discharges, travel time to hospital14 and clinical signs and symptoms at admission; in Model B we examined the effects of the following hierarchical, mutually exclusive syndromes: sick young infant, meningitis/encephalopathy, severe malnutrition, very severe pneumonia, severe pneumonia, mild pneumonia and “other”.15 In the multiple-discharge analysis we used a spatial bootstrap method with 100 repetitions to account for intra-subject correlation. For this we randomly selected 40 sublocations (with replacement) and estimated the regression models on all data from these sublocations. We developed multivariable models by grouping variables by syndrome, adjusting for age and nutritional status to select those entering the final model (p-value < 0.10), and then removing the non-significant variables (P > 0.05) in a backward stepwise fashion.
For each clinical variable remaining in the final model we calculated the number needed to treat (NNT) by dividing the number of children discharged with a given characteristic by the number of discharge-associated deaths among these children.
Analyses were conducted in Stata 10.0 (StataCorp, College Station, United States of America) and MS Excel (Microsoft, Redmond, USA).
This study was conducted in compliance with the principles of the World Medical Association Declaration of Helsinki. Ethical approval was obtained from the Kenya Medical Research Institute Ethical Review Committee.
Results
Our data set included 199 598 children under follow-up at some point between 1 January 2004 and 31 December 2008 for a total of 554 515 person–years or an average of 2.8 years per child. The mean number of children at any given time was 110 903. During this period there were 2541 deaths (4.6/1000 child-years) and 12 894 hospitalizations (23.3/1000), and 10 277 children were admitted to hospital at least once: 8457 (82.3%) had one admission, 1336 (13.0%) two admissions and 484 (4.7%) three or more admissions. After removing children who died or were censored in hospital, Demographic Surveillance Study follow-up was available for 12 203 discharges from 2004 to 2008 and for an additional 2768 discharges from 2003.
In the single-discharge analysis (Table 1) we observed 2057 community deaths and 343 post-discharge deaths; 141 deaths that occurred more than 365 days after the first discharge were dropped from the analysis since they fell neither into the community nor into the post-discharge category. Cumulative mortality risk within one year of discharge was 3.3% (95% confidence interval, CI: 3.0–3.7). Children in the post-discharge cohort had substantially higher mortality rates than those in the community cohort, even after age adjustment. Though RRs decreased with increasing time since discharge, mortality remained elevated throughout the post-discharge period and beyond (12–23 months post-discharge, age-adjusted RR: 3.8; 95% CI: 3.1–4.8).
Table 1. Single-discharge and multiple-discharge analysis: mortality rates and rate ratios (RRs) for community and post-discharge cohort of children < 15 years of age in Kilifi Demographic Surveillance Study area, Kenya, 2004–2008.
| Cohort | Post-discharge period | Deaths | Person–years of observation (x 10−3) | Rate | Crude RR | 95% CI | Adjusted RR | 95% CI |
|---|---|---|---|---|---|---|---|---|
| Single-discharge | ||||||||
| Community cohort | – | 2057 | 524.04 | 3.9 | 1.0 | – | 1.0 | – |
| Post-discharge cohort | 0–14 d | 72 | 0.35 | 204.5 | 52.1 | 41.2–65.9 | 6.2 | 4.9–7.9 |
| 15–30 d | 33 | 0.40 | 82.3 | 21.0 | 14.9–29.6 | 4.9 | 3.4–6.9 | |
| 1–2 mo | 82 | 1.52 | 54.0 | 13.8 | 11.0–17.2 | 7.9 | 6.4–9.9 | |
| 3–5 mo | 75 | 2.28 | 32.9 | 8.4 | 6.7–10.6 | 5.6 | 4.5–7.1 | |
| 6–11 mo | 81 | 4.47 | 18.1 | 4.6 | 3.7–5.8 | 4.3 | 3.4–5.4 | |
| 0–11 mo | 343 | 9.02 | 38.0 | 9.7 | 8.6–10.9 | 5.6 | 5.0–6.3 | |
| Multiple discharge | ||||||||
| Community cohort | – | 2047 | 522.44 | 3.9 | 1.0 | – | 1.0 | – |
| Post-discharge cohort | 0–14 d | 93 | 0.46 | 202.7 | 51.7 | 38.7–69.3 | 8.0 | 6.1–10.4 |
| 15–30 d | 51 | 0.52 | 97.7 | 24.9 | 18.2–34.2 | 7.2 | 5.7–9.1 | |
| 1–2 mo | 135 | 1.97 | 68.5 | 17.5 | 13.9–22.0 | 11.2 | 8.8–14.4 | |
| 3–5 mo | 127 | 2.94 | 43.2 | 11.0 | 9.1–13.3 | 8.2 | 6.6–10.2 | |
| 6–11 mo | 129 | 5.70 | 22.6 | 5.8 | 4.5–7.4 | 5.7 | 4.3–7.5 | |
| 0–11 mo | 535 | 11.59 | 46.1 | 11.8 | 9.5–14.6 | 7.7 | 6.6–8.9 |
CI, confidence interval.
Note: Analysis based on 199 598 children < 15 years of age observed for 554 515 person–years between 1 January 2004 and 31 December 2008. Adjustment for age in the following categories: < 1 month, 1–5 months, 6–11 months, 1 year, 2 years, 3 years, 4 years, and 5–14 years old.
The multiple-discharge analysis included 2047 community deaths and 535 post-discharge deaths. Observations were duplicated if they were linked to more than one post-discharge period, thereby leading to a larger number of deaths and person–years than in the single-discharge approach. A few observations were dropped from the analysis because of missing sublocation data. Cumulative mortality risk within one year of discharge was 4.5% (95% CI: 4.1–4.8). Further detailed results are shown in Table 1.
For each age stratum we estimated the expected number of deaths in the post-discharge cohort based on the background community mortality rate using the multiple-discharge approach (Table 2). In the post-discharge cohort 464 deaths (40 per 1000) were in excess of those expected from community rates; they represented 35% of deaths in neonates and 89% in older children. The population-attributable risk percent for mortality associated with hospital discharge was 0.8% in neonates and 27% in older children.
Table 2. Deaths associated with hospital discharge for children < 15 years of age in Kilifi Demographic Surveillance Study area, Kenya, 2004–2008.
| Age | No. of observed deaths | No. of expected deaths | No. of excess deaths | AR (%) | PAR (%) |
|---|---|---|---|---|---|
| < 1 mo | 22 | 14.4 | 7.6 | 34.5 | 0.8 |
| 1–5 mo | 107 | 12.0 | 95.0 | 88.8 | 26.6 |
| 6–11 mo | 107 | 15.8 | 91.2 | 85.2 | 32.1 |
| 1 y | 111 | 17.5 | 93.5 | 84.2 | 29.3 |
| 2 y | 51 | 6.9 | 44.1 | 86.5 | 24.2 |
| 3 y | 26 | 2.4 | 23.6 | 90.8 | 23.9 |
| 4 y | 23 | 1.0 | 22.0 | 95.8 | 30.2 |
| 5–14 y | 88 | 1.6 | 86.4 | 98.2 | 23.4 |
| Total | 535 | 71.5 | 463.5 | 86.6 | 18.0 |
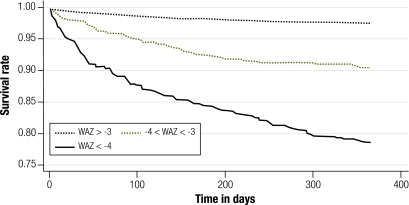
AR, attributable risk; PAR, populaton-attributable risk.
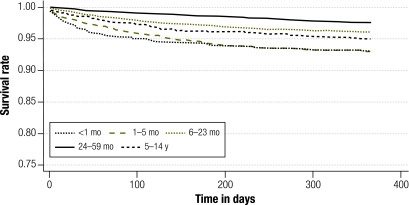
In univariate proportional hazards models (multiple-discharge approach), mortality decreased with age (Fig. 1) and calendar time (HR: 0.91 per year; P = 0.02), increased with distance to hospital (HR: 1.12 per ½ hour of vehicular travel time) and number of previous discharges (1 discharge, HR: 4.0; 2 discharges, HR: 9.5 and ≥ 3 discharges, HR: 32.4), and was unaffected by sex or season. We obtained unadjusted and age-, weight-for-age Z scores and syndrome-adjusted HRs for more than 40 clinical variables in children less than 5 years of age (Table 3, available at: http://www.who.int/bulletin/volumes/89/10/11-089235). Poor nutritional status was associated with an increased post-discharge mortality risk, irrespective of the measure chosen (Table 3 and Fig. 2). Finally, infection with the human immunodeficiency virus (HIV) was associated with mortality in the crude (HR: 3.3; P < 0.01) and age-adjusted (HR: 3.2; P < 0.01) models, but this association disappeared after adjustment for weight-for-age Z score (HR: 2.2; P = 0.19).
Fig. 1.
Kaplan–Meier graphs for survival in children recently discharged from Kilifi District Hospital, by age at discharge, Kenya, 2004–2008
Table 3. Crude and adjusteda mortality hazard ratios (HRs) for children < 5 years of age recently discharged from Kilifi District Hospital, by variable group, Kenya, 2004–2008.
| Clinical signs/symptoms | Crude HR | P | Adjusted HR | P |
|---|---|---|---|---|
| Fever/malaria | ||||
| Fever | 0.68 | < 0.01 | 0.91 | 0.46 |
| Temp. > 37.5 °C | 0.76 | < 0.01 | 1.15 | 0.35 |
| Temp. > 39 °C | 0.70 | 0.02 | 1.21 | 0.22 |
| Parasitaemia | 0.32 | < 0.01 | 0.46 | < 0.01 |
| Anaemia | 1.17 | 0.36 | 1.22 | 0.30 |
| Respiratory | ||||
| Cough | 1.14 | 0.30 | 1.00 | 0.99 |
| Difficulty breathing | 1.30 | < 0.01 | 0.82 | 0.16 |
| Tachypnea | 1.41 | < 0.01 | 1.05 | 0.75 |
| Indrawing | 1.57 | < 0.01 | 1.28 | 0.93 |
| Stridor | 0.99 | 0.99 | 0.83 | 0.99 |
| Hypoxia | 2.91 | < 0.01 | 2.07 | < 0.01 |
| Gastrointestinal | ||||
| Vomiting | 0.87 | 0.35 | 0.88 | 0.35 |
| Diarrhoea | 1.21 | 0.13 | 1.21 | 0.18 |
| Meningitis/sepsis | ||||
| Bacteraemia | 2.72 | < 0.01 | 1.95 | < 0.01 |
| Convulsions | 0.56 | < 0.01 | 0.72 | 0.13 |
| Prostration | 1.36 | 0.02 | 1.42 | 0.05 |
| Lethargy | 1.63 | < 0.01 | 1.59 | < 0.01 |
| Agitation | 1.39 | 0.21 | 1.22 | 0.64 |
| Bulging fontanelle | 3.66 | < 0.01 | 2.43 | 0.02 |
| Stiff neck | 3.29 | 0.01 | 2.01 | 0.92 |
| Shock | 1.39 | 0.05 | 0.79 | 0.17 |
| Nutritionalb | ||||
| −3 < WAZ < −2 | 2.11 | < 0.01 | Included in “baseline” group | |
| −4 < WAZ < −3 | 4.97 | < 0.01 | 2.41 | < 0.01 |
| WAZ < −4 | 12.15 | < 0.01 | 2.87 | 0.04 |
| −3 < WHZ < −2 | 2.33 | < 0.01 | 0.98 | 0.96 |
| −4 < WHZ < −3 | 4.43 | < 0.01 | 1.00 | 0.99 |
| WHZ < −4 | 7.41 | < 0.01 | 0.91 | 0.88 |
| −3 < HAZ < −2 | 1.65 | < 0.01 | 0.97 | 0.89 |
| −4 < HAZ < −3 | 3.02 | < 0.01 | 1.11 | 0.74 |
| HAZ < −4 | 5.91 | < 0.01 | 0.83 | 0.68 |
| −3 < MUAC-Z < −2 | 3.37 | < 0.01 | 2.32 | < 0.01 |
| −4 < MUAC-Z < −3 | 6.78 | < 0.01 | 2.92 | < 0.01 |
| MUAC-Z < −4 | 18.21 | < 0.01 | 7.59 | < 0.01 |
| Oedema | 2.96 | < 0.01 | Dropped due to collinearity | |
| Uncategorized variables | ||||
| Wheezing | 0.26 | 0.68 | 0.40 | 0.05 |
| Admission to KEMRI | 1.46 | 0.01 | 1.23 | 0.17 |
| Hospitalization > 13 d | 4.61 | < 0.01 | 2.07 | < 0.01 |
| Jaundice | 1.84 | 0.01 | 1.67 | 0.06 |
| HIV infection | 3.34 | < 0.01 | 2.22 | 0.19 |
| Enlarged spleen | 1.55 | 0.03 | 2.10 | < 0.01 |
| Hepatomegaly | 2.76 | < 0.01 | 2.32 | < 0.01 |
| High serum creatinine | 0.78 | 0.19 | 0.80 | 0.30 |
| Hyperglycaemia | 1.01 | 0.98 | 0.97 | 0.99 |
| Hypoglycaemia | 2.09 | < 0.01 | 1.24 | 0.40 |
| Transfusion | 1.66 | < 0.01 | 1.63 | < 0.01 |
| Absconded | 4.65 | < 0.01 | 2.06 | 0.95 |
HAZ, height-for-age Z score; HIV, human immunodeficiency virus; KEMRI, Kenya Medical Research Institute; MUAC-Z, mid-upper arm circumference Z score; WAZ, weight-for-age Z score; WHZ, weight-for-height Z score.
a Adjustment for age at discharge, weight-for-age Z score and covariates in same variable group.
b “Adjusted” model shown for children 2 to 59 months of age only (HAZ and WHZ unreliable in infants < 45 cm in length, MUAC-Z score not available for infants < 6 months of age). WAZ was used in the final multivariable models for all children < 5 years old.
Fig. 2.
Kaplan–Meier graphs for survival in children recently discharged from Kilifi District Hospital, by weight-for-age Z score (WAZ) on admission, Kenya, 2004–2008
The final Cox model for children 0–59 months of age included parasitaemia as a protective factor and young age, severe underweight, hypoxia, bacteraemia, jaundice, hepatomegaly, hospitalization > 13 days and number of previous discharges as risk factors for post-discharge mortality (Table 4). In the model investigating survival by disease syndrome, severe malnutrition was associated with the highest mortality, followed by very severe pneumonia, sick young infant, meningitis and mild or severe pneumonia compared with having none of these syndromes (Table 4).
Table 4. Multivariable Cox models A and B: hazard ratios (HRs) for mortality in children < 5 years of age recently discharged from Kilifi District Hospital, 2004–2008, Kenya.
| HR | 95% CI | |
|---|---|---|
| Model A: by demographic and clinical characteristics | ||
| Age 1–5 mo | 1.34 | 0.93–1.92 |
| Age 6–11 mo | 0.82 | 0.57–1.18 |
| Age 2–5 y | 0.57 | 0.36–0.90 |
| WAZ < −3 | 3.42 | 2.50–4.68 |
| WAZ < −4 | 6.53 | 4.85–8.80 |
| Parasitaemia | 0.45 | 0.29–0.71 |
| Hypoxia | 2.30 | 1.64–3.23 |
| Bacteraemia | 1.77 | 1.15–2.74 |
| Jaundice | 1.77 | 1.08–2.91 |
| Hepatomegaly | 2.34 | 1.60–3.42 |
| Hospitalization > 13 d | 1.83 | 1.33–2.52 |
| 1 prior dischargea | 2.83 | 2.04–3.92 |
| 2 prior dischargesa | 7.06 | 4.09–12.21 |
| ≥ 3 prior dischargesa | 23.55 | 10.70–51.84 |
| Model B: by disease syndromeb | ||
| Mild pneumonia | 2.30 | 1.00–5.28 |
| Severe pneumonia | 1.37 | 1.05–1.79 |
| Very severe pneumonia | 4.09 | 2.25–7.46 |
| Severe malnutrition | 4.37 | 2.73–7.01 |
| Meningitis | 2.29 | 1.57–3.32 |
| Sick young infant | 2.67 | 1.98–3.58 |
CI, confidence interval; WAZ, weight-for-age Z score.
a Prior discharge occurring within 1 year of index discharge.
b This analysis was not adjusted for age at discharge because one of the syndromic groups is defined by age criteria.
In the NNT analysis, we found that one death could be identified by targeting 16 children or fewer with the following characteristics: weight-for-age Z score < −4 (NNT: 6.1); hospitalization > 13 days (NNT: 7.8); hypoxia (NNT: 11.5), bacteraemia (NNT: 12.6), hepatomegaly (NNT: 13.1), weight-for-age Z score > −4 but < −3 (NNT: 13.6) or jaundice (NNT: 16.2). An intervention focused on patients meeting one or more of these criteria would target approximately 545 children per year (33% of discharged patients) and 39 expected deaths (NNT: 13.9, 47% of discharge-associated deaths), whereas a programme focusing on severely underweight children alone would target 220 children per year (13% of discharged patients) and 24 potential deaths (NNT: 9.1, 29% of discharge-associated deaths).
Discussion
This is the largest study to date to investigate child mortality after hospital discharge in a developing country setting. It also presents the most comprehensive analysis of the risk factors for post-discharge mortality. We included 200 000 children who were followed for a period of 555 000 child–years during which they experienced more than 15 000 hospital discharges and 353 post-discharge deaths. The study had sufficient statistical power to estimate the increased risk of mortality during the 12 months following discharge and to explore demographic and clinical predictors of mortality in the post-discharge group. We found that child mortality was more than sevenfold higher among post-discharge children than among similarly-aged children in the community and that 4.5% of children who are discharged from hospital die within the subsequent year. Young age, poor nutritional status, hypoxia, bacteraemia, enlarged liver, jaundice, extended hospitalization and number of previous discharges were associated with increased mortality, whereas malaria parasitaemia was predictive of relatively decreased mortality.
The single- and multiple-discharge approaches yielded similar results, with slightly higher mortality seen in the multiple-discharge model. The single-discharge model is simple to implement and comprehend, but it assumes that the first discharge observed in the KDHSS was truly a child’s first discharge, and this could lead to misclassification if the child was hospitalized at another hospital. Additionally, it excludes any discharge that occurs after the initial one and excludes all deaths after the first post-discharge period. Since children with multiple hospitalizations are likely to be at highest risk of death, this will lead to an underestimation of post-discharge mortality. Despite the added complexity, the multiple-discharge model has several advantages. It avoids both of the problems described above but also allows us to investigate the contribution of previous discharges to mortality risk after any given discharge and to understand the relationship between post-discharge mortality and repeat admissions for chronic illness. Finally, it sheds light on mortality risk after “any” hospital discharge and is thus more useful from a clinical and programmatic perspective, as it does not require knowledge of a patient’s discharge history. This last aspect is particularly relevant in developing country settings, many of which have not established longitudinal follow-up of paediatric patients. Despite the differences between these modelling approaches, it is important to note that the two analyses yielded comparable results and therefore produce similar epidemiological and public health inferences.
In previous studies, age-adjusted mortality RRs for post-discharge versus community children ranged from 1.2 to 3.46,7,9 and decreased over the post-discharge period; in contrast, we estimated a rate ratio of 7.7 with little attenuation over time, even when the post-discharge period was extended for an additional year. Furthermore, our study may have underestimated the increased mortality risk associated with hospital discharge by potentially overestimating the baseline mortality risk, as children discharged from hospital before in-migration into KHDSS or treated at hospitals other than KDH while residents were classified in the community cohort. The increase in post-discharge mortality associated with hypoxaemia on admission was similar to that observed in the Gambia.8 Moderate and severe malnutrition produced stark reductions in post-discharge survival, as seen in Bangladesh.9 Unlike previous studies, ours did not support a relationship between severe anaemia,10 diarrhoea6 or absconding from hospital7 and mortality in the post-discharge cohort. Nevertheless, diarrhoea was significantly associated with mortality before adjustment for malnutrition, which suggests that the effect observed elsewhere may have been due to confounding by nutritional status. This observation is consistent with earlier findings from Kilifi indicating that in the absence of malnutrition, diarrhoeal disease is an acute illness that resolves rapidly and has a good prognosis.16 Finally, we identified previously unknown risk factors for post-discharge mortality, including bacteraemia, hepatomegaly, jaundice and repeated or prolonged hospitalization.
Some of the differences among studies may reflect true variations in epidemiology across populations or over time. Most of the studies cited here were conducted in the 1990s. Since then major changes in malaria epidemiology have occurred in Kilifi District,17,18 HIV infection has emerged as an important underlying cause of childhood illness, and socioeconomic conditions have improved. These factors are likely to change patterns of disease, hospitalization and mortality. For example, higher hospital utilization among chronically ill children would lead to higher relative mortality among discharged versus community children. In addition to true epidemiological differences, our findings may also reflect methodological differences among studies: the large sample size available and the breadth of clinical variables collected on admission to KDH allowed us to conduct a more detailed analysis compared with earlier research.
Routine HIV testing on admission was incorporated into clinical case management in KDH in late 2006. We found a significant relationship between HIV positivity and post-discharge survival in crude and age-adjusted models for 2007–2008, but the association disappeared after controlling for nutritional status, possibly owing to insufficient statistical power. Alternately, this finding may reveal a true lack of association between positivity for HIV antibodies – which has limited specificity for HIV infection in young infants – and mortality, in the absence of wasting. HIV infection prevalence was 2% in well nourished children versus 14% in severely malnourished children. We therefore suspect that the observed effect of malnutrition on mortality is partly explained by an overlap between severe underweight and HIV infection (due to high rates of diarrhoea in HIV-positive children), although malnutrition affects mortality independently as well. Additional data are needed to disentangle the independent effects of HIV infection and malnutrition in the post-discharge period. While the protective effect of malaria parasitaemia may seem paradoxical on first inspection, it suggests that children who are admitted to hospital with mild malaria recover quickly and have a lower mortality risk than discharged children who were hospitalized with more severe illness. In contrast, when compared with children in the community, children admitted with malaria parasitaemia have a higher mortality risk.
The high and sustained increase in mortality rates after discharge indicates that hospitalization is seldom merely the expression of an acute disease episode with a short-term impact on mortality risk. Rather, it is often the manifestation of underlying frailty, with many hospitalized children having chronic illnesses such as malnutrition, HIV infection or sickle cell anaemia. Hospital admission is therefore an opportunity to identify a group of children at higher risk of death than their peers and to select them for inclusion in targeted health interventions. Owing to significant improvements in malaria treatment and control measures and in access to existing and new vaccines, childhood mortality is declining widely in Africa.19 The deaths that remain are harder to identify and harder to prevent; vulnerable children with chronic illness who seek care at district hospitals represent a pragmatic target group for mortality prevention measures.
At a population level the potential impact of post-discharge follow-up interventions on child mortality is limited by poor access to hospital care in the study area, which reduces the opportunity to identify high-risk children. This is reflected in the relatively low population attributable risk of 27% (after the neonatal period). Nevertheless, targeting approximately 545 children aged under 5 per year in the KHDSS area would enable us to manage a high-risk group in whom we currently observe approximately 40 deaths per year, which represents 8% of annual resident deaths and 47% of the post-discharge deaths in this age group. This rests on the assumption that interventions are available to provide appropriate counselling and care to the families of high-risk children. For severely malnourished children these may include complementary feeding, micronutrient supplementation, targeted antibiotic prophylaxis and socio-educational strategies to improve nutrition.20 Among children with HIV infection, antiretroviral treatment is now widely available and antibiotic prophylaxis has a proven role in reducing mortality;21,22 both were in limited use in Kilifi during the study period. The outcome for patients with sickle cell anaemia could be improved with penicillin and malaria prophylaxis and with parental education for the identification of severe symptoms and malarial crises.23 Even if such interventions have an aggregate effectiveness of 50%, the number of preventable deaths, 20 per year (24% of post-discharge deaths), suggests that targeting the segment of the population in which a large fraction of deaths is associated with hospital discharge might prove cost-effective.
This study highlights the value of linking hospital admission and demographic surveillance data to enable follow-up of sick children after their discharge from hospital. These children bear a substantially higher risk of death than their peers in the community throughout the post-discharge period and targeting a subset of them with effective outpatient interventions could prevent a significant proportion of child mortality in the KHDSS area. In particular, severely underweight children sustain the greatest increase in mortality risk and should constitute the primary target group.
Acknowledgements
The authors thank the DSS field workers and Kilifi District Hospital clinical team for their involvement in data collection and the KEMRI/Wellcome Trust ICT staff for their diligent work on data entry and data management. This study is published with the permission of the director of KEMRI.
Funding:
This work was supported by the Wellcome Trust (UK). JAGS (grant number 081835), JAB (083579) and TNW (076934) are supported by research fellowships from the Wellcome Trust. The authors declare that they had full control over all primary data and did not enter into any agreement with the study sponsor that may have limited their ability to complete the research as planned.
Competing interests:
None declared.
References
- 1.Gove S, The WHO Working Group on Guidelines for Integrated Management of the Sick Child Integrated management of childhood illness by outpatient health workers: technical basis and overview. Bull World Health Organ. 1997;75(Suppl 1):7–24. [PMC free article] [PubMed] [Google Scholar]
- 2.Handbook: IMCI integrated management of childhood illness. Geneva: World Health Organization & United Nations Children’s Fund; 2005. [Google Scholar]
- 3.Gove S, Tamburlini G, Molyneux E, Whitesell P, Campbell H. Development and technical basis of simplified guidelines for emergency triage assessment and treatment in developing countries. Arch Dis Child. 1999;81:473–7. doi: 10.1136/adc.81.6.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pneumococcal vaccines Geneva: World Health Organization; 2003. Available from: http://www.who.int/vaccines/en/pneumococcus.shtml [accessed 4 July 2011].
- 5.Bryce J, Victora CG, Habicht JP, Black RE, Scherpbier RW, MCE-IMCI Technical Advisors Programmatic pathways to child survival: results of a multi-country evaluation of Integrated Management of Childhood Illness. Health Policy Plan. 2005;20(Suppl 1):i5–17. doi: 10.1093/heapol/czi055. [DOI] [PubMed] [Google Scholar]
- 6.Snow RW, Howard SC, Mung’Ala-Odera V, English M, Molyneux CS, Waruiru C, et al. Paediatric survival and re-admission risks following hospitalization on the Kenyan coast. Trop Med Int Health. 2000;5:377–83. doi: 10.1046/j.1365-3156.2000.00568.x. [DOI] [PubMed] [Google Scholar]
- 7.Veirum JE, Sodeman M, Biai S, Hedegård K, Aaby P. Increased mortality in the year following discharge from a paediatric ward in Bissau, Guinea-Bissau. Acta Paediatr. 2007;96:1832–8. doi: 10.1111/j.1651-2227.2007.00562.x. [DOI] [PubMed] [Google Scholar]
- 8.West TE, Goetghebuer T, Milligan P, Mulholland EK, Weber MW. Long-term morbidity and mortality following hypoxaemic lower respiratory tract infection in Gambian children. Bull World Health Organ. 1999;77:144–8. [PMC free article] [PubMed] [Google Scholar]
- 9.Roy SK, Chowdhury AK, Rahaman MM. Excess mortality among children discharged from hospital after treatment for diarrhoea in rural Bangladesh. Br Med J (Clin Res Ed) 1983;287:1097–9. doi: 10.1136/bmj.287.6399.1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zucker JR, Lackritz EM, Ruebush TK 2nd, Hightower AW, Adungosi JE, Were JB, et al. Childhood mortality during and after hospitalization in western Kenya: effect of malaria treatment regimens. Am J Trop Med Hyg. 1996;55:655–60. doi: 10.4269/ajtmh.1996.55.655. [DOI] [PubMed] [Google Scholar]
- 11.Phiri KS, Calis JC, Faragher B, Nkhoma E, Ng’oma K, Mangochi B, et al. Long term outcome of severe anaemia in Malawian children. PLoS ONE. 2008;3:e2903. doi: 10.1371/journal.pone.0002903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Islam MA, Rahman MM, Mahalanabis D, Rahman AK. Death in a diarrhoeal cohort of infants and young children soon after discharge from hospital: risk factors and causes by verbal autopsy. J Trop Pediatr. 1996;42:342–7. doi: 10.1093/tropej/42.6.342. [DOI] [PubMed] [Google Scholar]
- 13.Moïsi JC, Nokes DJ, Gatakaa H, Williams TN, Bauni E, Levine OS, et al. Sensitivity of hospital-based surveillance for severe disease: a geographic information system analysis of access to care in Kilifi district, Kenya. Bull World Health Organ. 2011;89:102–11. doi: 10.2471/BLT.10.080796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moïsi JC, Gatakaa H, Noor AM, Williams TN, Bauni E, Tsofa B, et al. Geographic access to care is not a determinant of child mortality in a rural Kenyan setting with high health facility density. BMC Public Health. 2010;10:142. doi: 10.1186/1471-2458-10-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Berkley JA, Maitland K, Mwangi I, Ngetsa C, Mwarumba S, Lowe BS, et al. Use of clinical syndromes to target antibiotic prescribing in seriously ill children in malaria endemic area: observational study. BMJ. 2005;330:995. doi: 10.1136/bmj.38408.471991.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nokes DJ, Abwao J, Pamba A, Peenze I, Dewar J, Maghenda JK, et al. Incidence and clinical characteristics of group A rotavirus infections among children admitted to hospital in Kilifi, Kenya. PLoS Med. 2008;5:e153. doi: 10.1371/journal.pmed.0050153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Okiro EA, Hay SI, Gikandi PW, Sharif SK, Noor AM, Peshu N, et al. The decline in paediatric malaria admissions on the coast of Kenya. Malar J. 2007;6:151. doi: 10.1186/1475-2875-6-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.O’Meara WP, Bejon P, Mwangi TW, Okiro EA, Peshu N, Snow RW, et al. Effect of a fall in malaria transmission on morbidity and mortality in Kilifi, Kenya. Lancet. 2008;372:1555–62. doi: 10.1016/S0140-6736(08)61655-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rajaratnam JK, Marcus JR, Flaxman AD, Wang H, Levin-Rector A, Dwyer L, et al. Neonatal, postneonatal, childhood, and under-5 mortality for 187 countries, 1970–2010: a systematic analysis of progress towards Millennium Development Goal 4. Lancet. 2010;375:1988–2008. doi: 10.1016/S0140-6736(10)60703-9. [DOI] [PubMed] [Google Scholar]
- 20.Bhutta ZA, Ahmed T, Black RE, Cousens S, Dewey K, Giugliani E, et al. Maternal and Child Undernutrition Study Group What works? Interventions for maternal and child undernutrition and survival. Lancet. 2008;371:417–40. doi: 10.1016/S0140-6736(07)61693-6. [DOI] [PubMed] [Google Scholar]
- 21.Sauvageot D, Schaefer M, Olson D, Pujades-Rodriguez M, O’Brien DP. Antiretroviral therapy outcomes in resource-limited settings for HIV-infected children <5 years of age. Pediatrics. 2010;125:e1039–47. doi: 10.1542/peds.2009-1062. [DOI] [PubMed] [Google Scholar]
- 22.Chintu C, Bhat GJ, Walker AS, Mulenga V, Sinyinza F, Lishimpi K, et al. CHAP trial team Co-trimoxazole as prophylaxis against opportunistic infections in HIV-infected Zambian children (CHAP): a double-blind randomised placebo-controlled trial. Lancet. 2004;364:1865–71. doi: 10.1016/S0140-6736(04)17442-4. [DOI] [PubMed] [Google Scholar]
- 23.Tshilolo L, Kafando E, Sawadogo M, Cotton F, Vertongen F, Ferster A, et al. Neonatal screening and clinical care programmes for sickle cell disorders in sub-Saharan Africa: lessons from pilot studies. Public Health. 2008;122:933–41. doi: 10.1016/j.puhe.2007.12.005. [DOI] [PubMed] [Google Scholar]