Abstract
Traumatic brain injury (TBI) is a major public health problem and the leading cause of death and disability worldwide. Despite the modern diagnosis and treatment, the prognosis for patients with TBI remains poor. While severity of primary injury is the major factor determining the outcomes, the secondary injury caused by physiological insults such as hypotension, hypoxemia, hypercarbia, hypocarbia, hyperglycemia and hypoglycemia, etc. that develop over time after the onset of the initial injury, causes further damage to brain tissue, worsening the outcome in TBI. Perioperative period may be particularly important in the course of TBI management. While surgery and anesthesia may predispose the patients to new onset secondary injuries which may contribute adversely to outcomes, the perioperative period is also an opportunity to detect and correct the undiagnosed pre-existing secondary insults, to prevent against new secondary insults and is a potential window to initiate interventions that may improve outcome of TBI. For this review, extensive Pubmed and Medline search on various aspects of perioperative management of TBI was performed, followed by review of research focusing on intraoperative and perioperative period. While the research focusing specifically on the intraoperative and immediate perioperative TBI management is limited, clinical management continues to be based largely on physiological optimization and recommendations of Brain Trauma Foundation guidelines. This review is focused on the perioperative management of TBI, with particular emphasis on recent developments.
Keywords: Anesthesia, perioperative management, traumatic brain injury
INTRODUCTION
Traumatic brain injury (TBI) is a major public health problem and the leading cause of death and disability worldwide.[1] Approximately 1.7 million people sustain TBI every year in the United States, leading to 275,000 hospitalizations and 52,000 deaths.[1] TBI is a contributing factor in about 30.5% of all injury-related deaths in the United States.[1] TBI occurs most often in children aged 0–4 years, adolescents aged 15–19 years and elderly aged 65 years and more.[1] In all age groups, males have a higher rate of TBI than females.[1] Falls and motor vehicle-traffic injury are the leading causes of TBI in the United States.[1] In the recent years, prehospital and intensive care of patients with TBI has improved substantially and evidence-based guidelines for management have been developed.[2–13] However, despite the modern diagnosis and treatment, the prognosis for patients with TBI remains poor, emphasizing the need for further research and improvement in care. This review will focus on the perioperative management of TBI, with particular emphasis on recent developments, and is based on extensive Pubmed and Medline search on various aspects of perioperative management of TBI, followed by review of research focusing on intraoperative and perioperative period.
PATHOPHYSIOLOGY OF TRAUMATIC BRAIN INJURY
Pathophysiology of TBI involves primary and secondary injuries to the brain. Primary injury is the damage caused by the initial trauma involving mechanical impact to the brain tissue and skull due to acceleration–deceleration or rotational forces, resulting in skull fracture, brain contusion, expanding intracranial hematoma or diffuse axonal injury.[14] The primary injury then initiates inflammatory process, edema formation and excitotoxicity, resulting in further increase in intracranial pressure (ICP) and reduced cerebral perfusion pressure (CPP).[14,15] Severity of primary injury is the major factor determining the outcome of TBI patients. Secondary injury is a consequence of physiological insults that develop over time after the onset of the initial injury, causing further damage to the brain tissue and worsening the outcome in TBI patients.[14,15] Two major factors that cause secondary injury are hypotension [systolic blood pressure (SBP) < 90 mmHg] and hypoxemia (PaO2 < 60 mmHg).[16]
A study analyzing data from the Traumatic Coma Data Bank demonstrated that hypotension and hypoxemia were independently associated with increased morbidity and mortality from severe TBI.[17] A single episode of hypotension was associated with increased morbidity and mortality.[17] A meta-analysis of 8721 patients (IMPACT study) also suggested that hypotension and hypoxia were significantly associated with unfavorable 6-month outcome.[18] A study on the association between intraoperative hypotension and outcome demonstrated that patients who had intraoperative hypotension had over three times increased mortality than normotensive patients.[19] Moreover, the duration of intraoperative hypotension was also inversely associated with functional outcome.[19] Other factors implicated in secondary injury include hypoglycemia, hyperglycemia, hypercarbia and hypocarbia, and raised ICP.[20–25]
THE IMPORTANCE OF PERIOPERATIVE PERIOD
Given the poor outcomes of TBI and impact of secondary insults, current TBI management focuses on prevention of primary injury and avoidance of secondary injuries. Thus, the cornerstones of modern TBI management are field resuscitation, expeditious triage, emergent surgical evacuation of mass lesions, control of ICP, and support of CPP, multimodal monitoring and optimization of physiological environment. Perioperative period may be particularly important in the course of TBI management for numerous reasons. First, despite the aggressive interventions to rapidly correct hypoxemia, hypotension, hypo and hypercarbia, and hypo and hyperglycemia in the emergency department, it is not unusual for one or more of these complicating factors to persist or remain undetected as the patient is emergently transported to the operating room. Hence, perioperative period may provide an opportunity to either continue ongoing resuscitation or to correct the pre-existing secondary insults. Secondly, surgery and anesthesia may predispose the patient to new onset secondary injuries (such as intraoperative hypotension due to surgical blood loss or effect of anesthetic agents, new onset hyperglycemia due to stress response, etc.), which may contribute adversely to outcomes. Since secondary injury is largely preventable/treatable, the perioperative period may be a potential window to initiate interventions that may improve the outcome of TBI. Perioperative management involves rapid evaluation, continuation of resuscitation (cerebral and systemic), early surgical intervention, intensive monitoring and anesthetic planning.
Initial Assessment and Ongoing Resuscitation
The initial assessment and stabilization is usually achieved in the emergency department and resuscitation initiated before the patient is transported to Computed Tomography (CT) scanner and then to the operating room. Nevertheless, it is important for the anesthesia team to perform another rapid assessment as the patient is received in the operating room. The assessment should always begin with airway, breathing and circulation, followed by a rapid assessment of neurological status and associated extracranial injuries and attention to specific secondary injury mechanisms and ongoing treatment thereof. Information about time and mechanism of injury can be valuable. Brief neurological assessment is performed by using Glasgow Coma Scale (GCS)[26] score and pupillary responses. Associated thoracic, abdominal, spinal and long bone injuries may be stable or evolve during the perioperative period and must be considered in differential diagnosis of new onset hypotension, anemia, hemodynamic instability or hypoxemia during anesthesia and surgery. As the patient is transported to the operating room, all resuscitative measures should continue.
Airway Management
Patients with TBI requiring surgery will invariably require tracheal intubation. In fact, most patients are likely to arrive in the operating room already intubated. However, some patients, particularly those with extradural hematoma, may be conscious and breathing spontaneously. The indwelling tracheal tube can possibly migrate during transport, leading to endobronchial intubation or even dislodgement, and hence, adequate position of the tube must always be confirmed. In the select patients who may not be already intubated, airway management is complicated by a number of factors, including urgency of situation (because of pre-existing/worsening hypoxia), uncertainty of cervical spine status, uncertainty of airway (due to presence of blood, vomitus, debris in the oral cavity or due to laryngo-pharyngeal injury or skull base fracture), full stomach, intracranial hypertension and uncertain volume status. All TBI patients requiring urgent surgery must be considered to have full stomach and airway management must account for possible underlying cervical spine injury. Although it has been reported that patients with craniocerebral trauma had an incidence of cervical spine injury (CSI) similar to that of the general trauma population,[27] emerging evidence suggests a higher incidence of cervical injury in patients who have experienced craniocerebral trauma, especially among those with increasing severity of craniocerebral injury as determined by low GCS score and unconsciousness.[28,29]
The choice of technique for tracheal intubation is determined by urgency, individual expertise/skills and available resources and generally incorporates rapid sequence intubation with cricoid pressure and manual in-line stabilization.[27] The anterior portion or cervical collar may be removed when manual in-line stabilization is established to allow greater mouth opening and facilitate laryngoscopy. Newer airway devises, particularly Glidescope videolaryngoscope, have gained popularity in recent years for use in trauma victims and may be useful in difficult airway scenarios. However, the intubation time using Glidescope may be longer due to difficulty in passing the tracheal tube through the glottis despite easier visualization.[30] Nasal intubation should be avoided in patients with base of skull fracture, severe facial fractures or bleeding diathesis. In any case, it is advisable to have a back-up plan ready in case of difficult intubation, given the significant risk of intracranial hypertension resulting from increased cerebral blood volume (CBV) because of hypoxemia and hypercarbia.
Choice of induction agents and muscle relaxants is important for successful uncomplicated airway management. Sodium thiopental, etomidate and propofol are commonly used to induce anesthesia before intubation. All these agents decrease the systemic hemodynamic response to intubation, blunt increases in ICP, and decrease the cerebral metabolic rate for oxygen (CMRO2). However, propofol and thiopental may cause cardiovascular depression leading to hypotension, especially in the presence of uncorrected hypovolemia. Etomidate may be advantageous due to little change in blood pressure during induction despite reduction of CMRO2.[31] However, it may lead to adrenal insufficiency causing delayed hypotension and requiring vasopressor use.[32] Ketamine, which causes limited cardiovascular compromise, has been associated with increased cerebral blood flow (CBF) and increased ICP, and as such, may be relatively contraindicated for intubating patients with risk for or pre-existing increased ICP.[33] The choice of muscle relaxant for rapid sequence induction is between succinylcholine and rocuronium.[34] Succinylcholine may contribute to increased ICP[35,36] which can be blunted by administration of an adequate dose of an induction agent such as thiopental.[37] While the clinical significance of the effect of succinylcholine on ICP is questionable,[37,38] increases in ICP secondary to hypoxia and hypercarbia are well documented and much more likely to be clinically important. Hence, in patients with TBI, clinicians may not avoid using succinylcholine.[38]
Anesthetic Management
The major goals of anesthetic management of TBI are to
maintain CPP;
treat increased ICP;
provide optimal surgical conditions;
avoid secondary insults such as hypoxemia, hyper and hypocarbia, hypo and hyperglycemia; and
provide adequate analgesia and amnesia.
Anesthetic technique
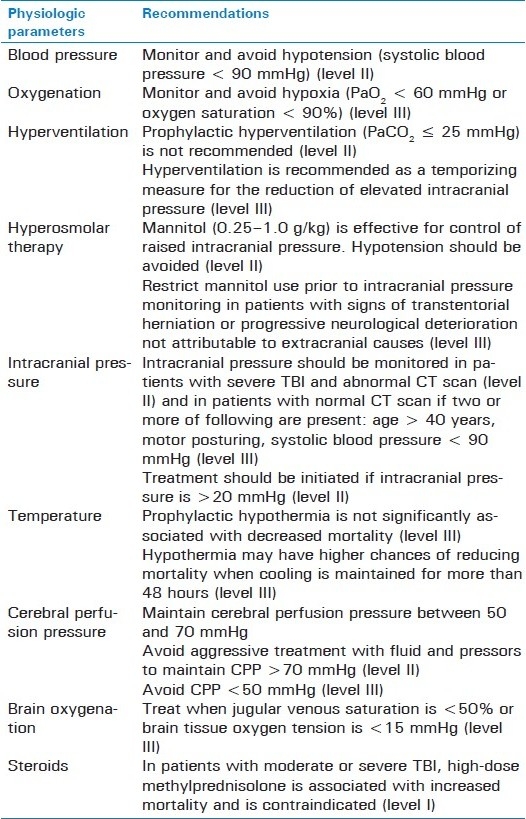
Important pharmacodynamic and pharmacokinetic differences exist between intravenous and volatile anesthetic agents. Intravenous agents including thiopental, propofol and etomidate cause cerebral vasoconstriction and reduce CBF, CBV, CMRO2and ICP.[39] Opioids have no direct effects on cerebral hemodynamics in the presence of controlled ventilation.[40] All volatile anesthetic agents (isoflurane, sevoflurane, desflurane) decrease CMRO2 and may cause cerebral vasodilation, resulting in increasing CBF and ICP. But at concentration less than 1 minimum alveolar concentration (MAC), the cerebral vasodilatory effects are minimal and hence they may be used in low concentrations in patients with TBI.[41] Nitrous oxide can increase CMRO2 and cause cerebral vasodialation and increased ICP and should be avoided.[42] Importantly, the effects of anesthetic agents (inhalation vs. total intravenous anesthesia) on outcome of TBI have not been demonstrated. In the absence of conclusive evidence, either anesthetic technique may be employed judiciously. However, more importantly, the principles of anesthetic management should adhere to the current guidelines for the management of severe TBI [Table 1].[2–13]
Table 1.
Ventilation
Ventilation should be adjusted to ensure adequate oxygenation and gas exchange. Inspired oxygen concentration is adjusted to maintain PaO2 >60 mmHg.2Monitoring arterial PCO2 is recommended since end-tidal CO2 may not be reliable. Hypercarbia should be avoided but hypocarbia must not be used indiscriminately.[12] Excessive hyperventilation may cause cerebral vasoconstriction leading to ischemia.[12] Hence, hyperventilation should be used judiciously for short-term control of ICP and to facilitate surgical exposure during craniotomy. Normocarbia should be restored before dural closure to avoid development of tension pneumocephalus. Monitoring cerebral oxygenation is recommended when utilizing hyperventilation for prolonged periods. In the intraoperative period, this may be accomplished by jugular venous oximetry[9,43] and in the postoperative period by brain tissue oxygenation (PbtO2) or CBF monitoring (e.g. using Transcranial Doppler ultrasonography).[9]
Monitoring
In additional to standard American Society of Anesthesiology (ASA) monitors, arterial catheterization is recommended for beat-to-beat blood pressure monitoring and for blood gas analysis and blood glucose monitoring during craniotomy. Central venous pressure (CVP) may be useful, particularly for resuscitation and when vasopressors are administered. However, it is advisable not to delay surgical evacuation of expanding intracranial hematoma because of institution of invasive monitoring. According to the current guidelines, ICP monitoring is recommended in all salvageable patients with a severe TBI (GCS < 9) and an abnormal CT scan (hematomas, contusions, swelling, herniation or compressed basal cistern), and in patients with severe TBI with a normal CT scan if two or more of the following features are noted at the admission: age > 40 years, unilateral or bilateral motor posturing, or SBP < 90 mmHg.[5] The use of multimodal monitoring for postoperative and intensive care of patients with TBI is increasing and monitoring cerebral oxygenation (global or focal) or CBF and metabolism parameters may be helpful in making important treatment decisions.[9]
Intravenous Fluids, Blood Pressure Management and Vasopressor Use
Hypotension following TBI can compromise cerebral hemodynamics and cause cerebral ischemia. Therefore, blood pressure management, including choice of fluids and vasopressors, is of paramount importance. Brain Trauma Foundation guidelines for the management of TBI recommend avoiding hypotension (SBP < 90 mmHg) and maintaining CPP between 50 and 70 mmHg.[2,8] Warm, non-glucose containing isotonic crystalloid solution is preferable for TBI patients. The role of colloid is controversial. A post-hoc analysis of the Saline versus Albumin Fluid Evaluation (SAFE) study demonstrated that resuscitation with albumin was associated with higher mortality rate and unfavorable neurological outcome at 24 months.[44] Hypertonic saline may be beneficial resuscitation fluid for TBI patients because it increases intravascular fluid and decreases ICP. Prehospital hypertonic saline resuscitation has been shown to be associated with a reduction in serum biomarker levels (S100B, Neuron Specific Enolase and Membrane Basic Protein) which correlated with better outcome.[45] However, a double-blind randomized controlled trial comparing prehospital resuscitation of hypotensive TBI patients with hypertonic saline with standard fluid resuscitation protocols found no difference in neurological outcome at 6 months.[46]
Vasopressors are commonly administered to treat hypotension or to augment CPP. However, there are only a few studies comparing the effectiveness of commonly used vasopressors in TBI and results of these studies are conflicting. Human data explicitly comparing vasopressors are limited to three small prospective, randomized, crossover trials comparing sequential effectiveness between norepinephrine and dopamine. Despite there being no differences in mean cerebral flow velocity[47,48] and cerebral oxygenation or metabolism[49] between the two vasopressors, norepinephrine had more predictable and consistent effect[48] while dopamine use led to higher ICP.[47] A recent single-center retrospective study of patients with severe TBI who received phenylephrine, norepinephrine or dopamine reported maximum increase in MAP and CPP from baseline with phenypephrine use.[50] There was no difference in ICP between the treatment groups after initiating the vasopressor although it was unclear whether improved MAP/CPP with vasopressor use translated into improved CBF or oxygenation.[50] Current evidence does not support preference of one vasopressor over the other.
Blood Transfusion
Anemia is associated with increased in-hospital mortality[51] and poor outcome in TBI.[52,53] Yet, there is little evidence to support packed red blood cell (PRBC) transfusion practice standards to correct anemia in TBI. While some have suggested that patients with TBI may not benefit from a higher transfusion threshold than other critically ill patients,[52] others have cautioned against the liberal use of blood transfusion in TBI.[53] Potential mechanisms of cerebral injury due to anemia include tissue hypoxia, injury caused by reactive oxygen species, inflammation, disruption of blood-brain barrier (BBB) function, vascular thrombosis and anemic cerebral hyperemia.[54] However, a number of cerebroprotective physiological mechanisms become effective with anemia which include aortic chemoreceptor activation, increased sympathetic activity leading to increased heart rate, stroke volume and cardiac index, reduced systemic vascular resistance, and enhanced oxygen extraction. Moreover, a number of cellular mechanisms of cerebral protection become effective in acute anemia. These include Hypoxia Inducible Factor (HIF), increased nitric oxide synthetase and nitric oxide in the brain (nNOS/NO), erythropoietin and vascular endothelial growth factor (VEGF) mediated angiogenesis and vascular repair.[54] Although increase in CBF during acute anemia can improve oxygen delivery, high hematocrit after PRBC transfusion may potentially decrease CBF and increase the risk of cerebral ischemia.[55] However, anemia due to hemodilution may impair cerebral autoregulation.[56] The overall effects of anemia on the brain might, therefore, depend on the relative balance between these competing protective and harmful factors of anemia and PRBC transfusion, and it is unclear whether transfusion trigger in patients with TBI should be any different from other critically ill patients and whether the injured brain is more susceptible to deleterious effects of anemia.
In the absence of defined optimal hemoglobin (Hb) levels, it has been suggested that neurophysiologic criteria for RBC transfusion may be more rational and may progressively replace arbitrary Hb-based transfusion triggers in neurocritical care.[57] RBC transfusion may influence cerebral oxygenation through a number of potential mechanisms in patients with TBI. Besides increasing the oxygen-carrier capacity of blood, RBC transfusion increases the circulating volume and can increase CBF in patients with impaired cerebral autoregulation secondary to the TBI. Transfusion also increases the blood viscosity to which the circulatory network responds with the release of nitric oxide, leading to vasodilatation and increasing functional capillary density (which quantifies capillary perfusion).[58] In recent years, there has been growing interest in the effect of RBC transfusion on brain tissue oxygenation (PbtO2) in patients with TBI and it seems an interesting possibility that PbtO2 values may be developed into potential transfusion triggers. However, most studies evaluating the effect of transfusion on PbtO2 in neurosurgical patients are limited by small sample size and have failed to demonstrate a consistent response to transfusion or elucidate predictors of PbtO2 response to transfusion.[59,60] The potential role of brain tissue oxygenation in deciding transfusion thresholds has been discussed elsewhere.[61,62]
Existing evidence suggests that both anemia and RBC transfusion are associated with poor neurological outcome in TBI.[52,53] While anemia is associated with increased in-hospital mortality[51] and lower hospital discharge GCS score, discharge Glasgow outcome score and Ranchos Los Amigos scores,[52] RBC transfusion is associated with acute lung injury, longer intensive care unit and hospital stay, and mortality.[63–65] The optimal Hb level in TBI patients is still unclear but there is no benefit of a liberal transfusion strategy (transfusion when Hb <10 g/dl) in moderate to severe TBI patients and it is not recommended.[53]
Coagulopathy and Factor VII
Coagulation disorder is a common problem after TBI. Coagulation disorder could result from TBI and cause secondary brain injury. A recent review reported that the overall prevalence of coagulopathy was 32.7% after TBI and more than 60% in severe TBI and that the presence of coagulopathy was associated with an increased mortality and poor outcome.[66] According to a recent prospective study, the independent risk factors for coagulopathy in TBI are GCS ≤ 8, Injury Severity Score (ISS) ≥ 16, presence of cerebral edema, subarachnoid hemorrhage and midline shift.[67] When brain is injured, tissue factor (TF) is released. Subsequently, pro-coagulant factors are activated resulting in thrombin formation and conversion of fibrinogen to fibrin. Normally, antithrombotic mechanisms are also activated to counter fibrin formation. Disseminated intravascular coagulation (DIC) inhibits the antithrombotic mechanism, causing imbalance of coagulation and fibrinolysis. Currently, there are no guidelines for management of coagulopathy in TBI. Hemostatic drugs including antifibrinolytic agents such as tranexamic acid and pro-coagulant drugs such as recombinant activated factor VII (rFVIIa) are sometimes used in treatment of coagulopathy after TBI. A Cochrane review found two randomized controlled trials that evaluated the effects of rFVIIa, but both the trails were too small to draw a conclusion regarding the effectiveness of rFVIIa for TBI patients.[68] The Clinical Randomization of Antifibrinolytics in Significant Hemorrhage (CRASH-2) trial, a large international placebo-controlled trial evaluating the effect of tranexamic acid on death, vascular occlusion events and blood transfusion in adult trauma patients, demonstrated that tranexamic acid was associated with a reduction of mortality (RR: 0.91, 95% CI: 0.85-097, P = 0.0035).[69] The risk of death from bleeding was also lower in tranexamic acid group (RR: 0.85, 95% CI: 0.76–0.96, P = 0.0077).[69]
Hyperosmolar Therapy
Mannitol is the standard agent used in hyperosmolar therapy. The recommended dose of mannitol is 0.25–1 g/kg body weight. Due to osmotic diuresis which can result in hypovolemia and hypotension, mannitol is recommended only when there are signs of transtentorial herniation or progressive neurological deterioration not attributable to extracranial causes.[3] In patients with severe TBI and elevated ICP refractory to mannitol treatment, 7.5% hypertonic saline administered as second tier therapy can increase cerebral oxygenation and improve cerebral and systemic hemodynamics.[70]
Glycemic Control
Hyperglycemia after TBI is associated with increased morbidity and mortality.[71–73] It may reflect the extent of injury severity,[74] reflecting a normal response to stress due to a rise in circulating counter-regulatory hormones or may worsen outcome after TBI.[74,75] Secondary brain injury from hyperglycemia can ensue, leading to an increase in glycolytic rates as shown by increased lactate/pyruvate ratio, resulting in metabolic acidosis within brain parenchyma, overproduction of reactive oxygen species, and ultimately neuronal cell death.[74–77] In 2001, Van den Berghe et al. reported that intensive insulin therapy (target blood glucose 80–110 mg/dl) in critically ill patients was associated with lower mortality.[78] However, more recent studies not only failed to demonstrate the mortality benefit of intensive insulin therapy but also found an increased risk of hypoglycemia.[79,80] Billotta et al. randomized 97 severe TBI patients to intensive insulin therapy group targeting blood glucose at 80-120 mg/dl or conventional insulin therapy group targeting blood glucose below 220 mg/dl and found that both the groups had similar mortality and neurological outcome at 6 months.[80] Although the intensive insulin therapy group had shorter ICU stay, infection rates were similar between both the groups and episodes of hypoglycemia (glucose < 80 mg/dl) were significantly higher in the intensive insulin therapy group.[80]
Hence, tight glucose control with intensive insulin therapy remains controversial. While a number of studies have investigated hyperglycemia in adult TBI in different contexts (admission vs. ICU, transient vs. persistent, early vs. late, etc.), none has specifically addressed the intraoperative period and the prevalence of intraoperative hyperglycemia, and its relation to preoperative glycemic patterns in adult TBI is not known. Since hyperglycemia is attributed to a stress response from the initial injury[74,75] and blood glucose levels are known to increase under anesthesia even in non-diabetic patients,[81] it is possible that added stress during general anesthesia and surgery may worsen hyperglycemia and contribute to poor outcome. Moreover, individual anesthetic agents have been shown to have differential effects on blood and brain glucose levels.[82,83] The only perioperative study in children with TBI demonstrated that intraoperative hyperglycemia is common, hypoglycemia in the absence of insulin treatment is not rare, and TBI severity and the presence of subdural hematoma (SDH) predict intraoperative hyperglycemia.[73] In the author's experience in adult patients undergoing craniotomy for TBI, intraoperative hyperglycemia (glucose > 200 mg/dl) was common (15%) and hypoglycemia (glucose < 60 mg/dl) was not observed (unpublished data). We also found that the independent risk factors for intraoperative hyperglycemia were severe TBI, SDH, preoperative hyperglycemia, and age ≥65 years, and the in-hospital mortality was higher in patients with intraoperative hyperglycemia. Given the current evidence for glucose control for TBI in perioperative period, a target glucose range of 80–180 mg/dl seems reasonable.
Therapeutic Hypothermia and Steroids
Hypothermia reduces cerebral metabolism during stress, reduces excitatory neurotransmitters release, attenuates BBB permeability, and has been used for brain protection in TBI patients for decades. However, clinical evidence in terms of mortality and functional outcomes is still inconclusive. A recent meta-analysis reported statistically insignificant reduction in mortality and increased favorable neurological outcome with hypothermia in TBI.[84] The benefits of hypothermia were greater when cooling was maintained for more than 48 hours, but the potential benefits of hypothermia may likely be offset by a significant increase in the risk of pneumonia.[84] These observations support previous findings that hypothermic therapy constitutes a beneficial treatment of TBI in specific circumstances. Accordingly, the BTF/AANS guidelines task force has issued a Level III recommendation for optional and cautious use of hypothermia for adults with TBI.[4]
Steroids have not been shown to improve outcomes or lower ICP in TBI.[13] In fact, findings from a randomized multicenter study on the effect of corticosteroids (MRC CRASH trail) showed that administration of methylprednisolone within 8 hours of TBI was associated with higher risk of death, and the risk of death or severe disability was more compared to placebo.[85] Therefore, the use of high-dose methylprednisolone is contraindicated in patients with moderate or severe TBI.[13]
SUMMARY
Perioperative period may be important in TBI management. While it may predispose the patient to new onset secondary injuries which may contribute adversely to outcomes, it is also an opportunity to detect and correct the undiagnosed pre-existing secondary insults. It may also be a potential window to initiate interventions that may improve the outcome of TBI. While research focused specifically on the intraoperative and perioperative TBI management is awaited, clinical management will continue to be based on physiological optimization.
Level I recommendations are based on the strongest evidence for effectiveness, and represent principles of patient management that reflect high degree of clinical certainty. Level II recommendations reflect a moderate degree of clinical certainty. For level III recommendations, the degree of clinical certainty is not established.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Faul M, Xu L, Wald MM, Coronado VG. Traumatic brain injury in the United States: Emergency department visits, hospitalizations, and deaths. Atlanta (GA): Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2010. [Google Scholar]
- 2.Bratton SL, Chestnut RM, Ghajar J, McConnell Hammond FF, Harris OA, Hartle R, et al. Brain Trauma Foundation; American Association of Neurological Surgeons; Congress of Neurological Surgeons; Joint Section on Neurotrauma and Critical Care, AANS/CNS. Guidelines for the management of severe traumatic brain injury Blood pressure and oxygenation. J Neurotrauma. 2007;24:S7–13. doi: 10.1089/neu.2007.9995. [DOI] [PubMed] [Google Scholar]
- 3.Bratton SL, Chestnut RM, Ghajar J, McConnell Hammond FF, Harris OA, Hartle R, et al. Brain Trauma Foundation; American Association of Neurological Surgeons; Congress of Neurological Surgeons; Joint Section on Neurotrauma and Critical Care, AANS/CNS. Guidelines for the management of severe traumatic brain injury II. Hyperosmolar therapy. J Neurotrauma. 2007;24:S14–20. doi: 10.1089/neu.2007.9994. [DOI] [PubMed] [Google Scholar]
- 4.Bratton SL, Chestnut RM, Ghajar J, McConnell Hammond FF, Harris OA, Hartl R, et al. Brain Trauma Foundation; American Association of Neurological Surgeons; Congress of Neurological Surgeons; Joint Section on Neurotrauma and Critical Care, AANS/CNS. Guidelines for the management of severe traumatic brain injury III Prophylactic hypothermia. J Neurotrauma. 2007;24:S21–5. doi: 10.1089/neu.2007.9993. [DOI] [PubMed] [Google Scholar]
- 5.Bratton SL, Chestnut RM, Ghajar J, McConnell Hammond FF, Harris OA, Hartl R, et al. Brain Trauma Foundation; American Association of Neurological Surgeons; Congress of Neurological Surgeons; Joint Section on Neurotrauma and Critical Care, AANS/CNS. Guidelines for the management of severe traumatic brain injury. VI. Indications for intracranial pressure monitoring. J Neurotrauma. 2007;24:S37–44. doi: 10.1089/neu.2007.9990. [DOI] [PubMed] [Google Scholar]
- 6.Bratton SL, Chestnut RM, Ghajar J, McConnell Hammond FF, Harris OA, Hartl R, et al. Brain Trauma Foundation; American Association of Neurological Surgeons; Congress of Neurological Surgeons; Joint Section on Neurotrauma and Critical Care, AANS/CNS. Guidelines for the management of severe traumatic brain injury. VII. Intracranial pressure monitoring technology. J Neurotrauma. 2007;24:S45–54. doi: 10.1089/neu.2007.9989. [DOI] [PubMed] [Google Scholar]
- 7.Bratton SL, Chestnut RM, Ghajar J, McConnell Hammond FF, Harris OA, Hartl R, et al. Brain Trauma Foundation; American Association of Neurological Surgeons; Congress of Neurological Surgeons; Joint Section on Neurotrauma and Critical Care, AANS/CNS. Guidelines for the management of severe traumatic brain injury. VIII. Intracranial pressure thresholds. J Neurotrauma. 2007;24:S55–8. doi: 10.1089/neu.2007.9988. [DOI] [PubMed] [Google Scholar]
- 8.Bratton SL, Chestnut RM, Ghajar J, McConnell Hammond FF, Harris OA, Hartl R, et al. Brain Trauma Foundation; American Association of Neurological Surgeons; Congress of Neurological Surgeons; Joint Section on Neurotrauma and Critical Care, AANS/CNS. Guidelines for the management of severe traumatic brain injury. IX. Cerebral perfusion thresholds. J Neurotrauma. 2007;24:S59–64. doi: 10.1089/neu.2007.9987. [DOI] [PubMed] [Google Scholar]
- 9.Bratton SL, Chestnut RM, Ghajar J, McConnell Hammond FF, Harris OA, Hartl R, et al. Brain Trauma Foundation; American Association of Neurological Surgeons; Congress of Neurological Surgeons; Joint Section on Neurotrauma and Critical Care, AANS/CNS. Guidelines for the management of severe traumatic brain injury. X. Brain oxygen monitoring and thresholds. J Neurotrauma. 2007;24:S65–70. doi: 10.1089/neu.2007.9986. [DOI] [PubMed] [Google Scholar]
- 10.Bratton SL, Chestnut RM, Ghajar J, McConnell Hammond FF, Harris OA, Hartl R, et al. Brain Trauma Foundation; American Association of Neurological Surgeons; Congress of Neurological Surgeons; Joint Section on Neurotrauma and Critical Care, AANS/CNS. Guidelines for the management of severe traumatic brain injury. XI. Anesthetics, analgesics, and sedatives. J Neurotrauma. 2007;24:S71–6. doi: 10.1089/neu.2007.9985. [DOI] [PubMed] [Google Scholar]
- 11.Bratton SL, Chestnut RM, Ghajar J, McConnell Hammond FF, Harris OA, Hartl R, et al. Brain Trauma Foundation; American Association of Neurological Surgeons; Congress of Neurological Surgeons; Joint Section on Neurotrauma and Critical Care, AANS/CNS. Guidelines for the management of severe traumatic brain injury. XIII. Antiseizure prophylaxis. J Neurotrauma. 2007;24:S83–6. doi: 10.1089/neu.2007.9983. [DOI] [PubMed] [Google Scholar]
- 12.Bratton SL, Chestnut RM, Ghajar J, McConnell Hammond FF, Harris OA, Hartl R, et al. Brain Trauma Foundation; American Association of Neurological Surgeons; Congress of Neurological Surgeons; Joint Section on Neurotrauma and Critical Care, AANS/CNS. Guidelines for the management of severe traumatic brain injury. XIV. Hyperventilation. J Neurotrauma. 2007;24:S87–90. doi: 10.1089/neu.2007.9982. [DOI] [PubMed] [Google Scholar]
- 13.Bratton SL, Chestnut RM, Ghajar J, McConnell Hammond FF, Harris OA, Hartl R, et al. Brain Trauma Foundation; American Association of Neurological Surgeons; Congress of Neurological Surgeons; Joint Section on Neurotrauma and Critical Care, AANS/CNS. Guidelines for the management of severe traumatic brain injury. XV. Steroids. J Neurotrauma. 2007;24:S91–5. doi: 10.1089/neu.2007.9981. [DOI] [PubMed] [Google Scholar]
- 14.Greve MW, Zink BJ. Pathophysiology of traumatic brain injury. Mt Sinai J Med. 2009;76:97–104. doi: 10.1002/msj.20104. [DOI] [PubMed] [Google Scholar]
- 15.Werner C, Engelhard K. Pathophysiology of traumatic brain injury. Br J Anaesth. 2007;99:4–9. doi: 10.1093/bja/aem131. [DOI] [PubMed] [Google Scholar]
- 16.Chesnut RM, Marshall LF, Klauber MR, Blunt BA, Baldwin N, Eisenberg HM, et al. The role of secondary brain injury in determining outcome from severe head injury. J Trauma. 1993;34:216–22. doi: 10.1097/00005373-199302000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Marshall LF, Becker DP, Bowers SA, Cayard C, Eisenberg H, Gross CR, et al. The National Traumatic Coma Data Bank. Part 1: Design, purpose, goals, and results. J Neurosurg. 1983;59:276–84. doi: 10.3171/jns.1983.59.2.0276. [DOI] [PubMed] [Google Scholar]
- 18.McHugh GS, Engel DC, Butcher I, Steyerberg EW, Lu J, Mushkudiani N, et al. Prognostic value of secondary insults in traumatic brain injury: Results from the IMPACT study. J Neurotrauma. 2007;24:287–93. doi: 10.1089/neu.2006.0031. [DOI] [PubMed] [Google Scholar]
- 19.Pietropaoli JA, Rogers FB, Shackford SR, Wald SL, Schmoker JD, Zhuang J. The deleterious effects of intraoperative hypotension on outcome in patients with severe head injuries. J Trauma. 1992;33:403–7. doi: 10.1097/00005373-199209000-00011. [DOI] [PubMed] [Google Scholar]
- 20.Liu-DeRyke X, Collingridge DS, Orme J, Roller D, Zurasky J, Rhoney DH. Clinical impact of early hyperglycemia during acute phase of traumatic brain injury. Neurocrit Care. 2009;11:151–7. doi: 10.1007/s12028-009-9228-6. [DOI] [PubMed] [Google Scholar]
- 21.Jeremitsky E, Omert LA, Dunham CM, Wilberger J, Rodriguez A. The impact of hyperglycemia on patients with severe brain injury. J Trauma. 2005;58:47–50. doi: 10.1097/01.ta.0000135158.42242.b1. [DOI] [PubMed] [Google Scholar]
- 22.Griesdale DE, Tremblay MH, McEwen J, Chittock DR. Glucose Control and Mortality in Patients with Severe Traumatic Brain Injury. Neurocrit Care. 2009;11:311–6. doi: 10.1007/s12028-009-9249-1. [DOI] [PubMed] [Google Scholar]
- 23.Sharma D, Jelacic J, Chennuri R, Chaiwat O, Chandler W, Vavilala MS. Incidence and risk factors for perioperative hyperglycemia in children with traumatic brain injury. Anesth Analg. 2009;108:81–9. doi: 10.1213/ane.0b013e31818a6f32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Warner KJ, Cuschieri J, Copass MK, Jurkovich GJ, Bulger EM. The impact of prehospital ventilation on outcome after severe traumatic brain injury. J Trauma. 2007;62:1330–6. doi: 10.1097/TA.0b013e31804a8032. [DOI] [PubMed] [Google Scholar]
- 25.Dumont TM, Visioni AJ, Rughani AI, Tranmer BI, Crookes B. Inappropriate prehospital ventilation in severe traumatic brain injury increases in-hospital mortality. J Neurotrauma. 2010;27:1233–41. doi: 10.1089/neu.2009.1216. [DOI] [PubMed] [Google Scholar]
- 26.Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2:81–4. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 27.Crosby ET. Airway management in adults after cervical spine trauma. Anesthesiology. 2006;104:1293–318. doi: 10.1097/00000542-200606000-00026. [DOI] [PubMed] [Google Scholar]
- 28.Holly LT, Kelly DF, Counelis GJ, Blinman T, McArthur DL, Cryer HG. Cervical spine trauma associated with moderate and severe head injury: Incidence, risk factors, and injury characteristics. J Neurosurg (Spine 3) 2002;69:285–291. doi: 10.3171/spi.2002.96.3.0285. [DOI] [PubMed] [Google Scholar]
- 29.Demetriades D, Charalambides K, Chahwan S, Hanpeter S, Alo K, Velmahos G, et al. Nonskeletal cervical spine injuries: Epidemiology and diagnostic pitfalls. J Trauma. 2000;48:724–7. doi: 10.1097/00005373-200004000-00022. [DOI] [PubMed] [Google Scholar]
- 30.Platts-Mills TF, Campagne D, Chinnock B, Snowden B, Glickman LT, Hendey GW. A comparison of GlideScope video laryngoscopy versus direct laryngoscopy intubation in the emergency department. Acad Emerg Med. 2009;16:866–71. doi: 10.1111/j.1553-2712.2009.00492.x. [DOI] [PubMed] [Google Scholar]
- 31.Dearden NM, McDowall DG. Comparison of etomidate and althesin in the reduction of increased intracranial pressure after head injury. Br J Anaesth. 1985;57:361–8. doi: 10.1093/bja/57.4.361. [DOI] [PubMed] [Google Scholar]
- 32.Cohan P, Wang C, McArthur DL, Cook SW, Dusick JR, Armin B, et al. Acute secondary adrenal insufficiency after traumatic brain injury: A prospective study. Crit Care Med. 2005;33:2358–66. doi: 10.1097/01.ccm.0000181735.51183.a7. [DOI] [PubMed] [Google Scholar]
- 33.Schulte am Esch J, Pfeifer G, Thiemig I, Entzian W. The influence of intravenous anaesthetic agents on primarily increased intracranial pressure. Acta Neurochir (Wien) 1978;45:15–25. doi: 10.1007/BF01774380. [DOI] [PubMed] [Google Scholar]
- 34.Perry JJ, Lee JS, Sillberg VA, Wells GA. Rocuronium versus succinylcholine for rapid sequence induction intubation. Cochrane Database Syst Rev. 2008;2:CD002788. doi: 10.1002/14651858.CD002788.pub2. [DOI] [PubMed] [Google Scholar]
- 35.Minton MD, Grosslight K, Stirt JA, Bedford RF. Increases in intracranial pressure from succinylcholine: Prevention by prior nondepolarizing blockade. Anesthesiology. 1986;65:165–9. doi: 10.1097/00000542-198608000-00006. [DOI] [PubMed] [Google Scholar]
- 36.Stirt JA, Grosslight KR, Bedford RF, Vollmer D. Defasciculation“ with metocurine prevents succinylcholine-induced increases in intracranial pressure. Anesthesiology. 1987;67:50–3. doi: 10.1097/00000542-198707000-00009. [DOI] [PubMed] [Google Scholar]
- 37.Kovarik WD, Mayberg TS, Lam AM, Mathisen TL, Winn HR. Succinylcholine does not change intracranial pressure, cerebral blood flow velocity, or the electroencephalogram in patients with neurologic injury. Anesth Analg. 1994;78:469–73. doi: 10.1213/00000539-199403000-00008. [DOI] [PubMed] [Google Scholar]
- 38.Clancy M, Halford S, Walls R, Murphy M. In patients with head injuries who undergo rapid sequence intubation using succinylcholine, does pretreatment with a competitive neuromuscular blocking agent improve outcome? A literature review. Emerg Med J. 2001;18:373–5. doi: 10.1136/emj.18.5.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Turner BK, Wakim JH, Secrest J, Zachary R. Neuroprotective effects of thiopental, propofol, and etomidate. AANA J. 2005;73:297–302. [PubMed] [Google Scholar]
- 40.Schregel W, Weyerer W, Cunitz G. Opioids, cerebral circulation and intracranial pressure. Anaesthesist. 1994;43:421–30. doi: 10.1007/s001010050074. [DOI] [PubMed] [Google Scholar]
- 41.Engelhard K, Werner C. Inhalational or intravenous anesthetics for craniotomies? Pro inhalational? Curr Opin Anaesthesiol. 2006;19:504–8. doi: 10.1097/01.aco.0000245275.76916.87. [DOI] [PubMed] [Google Scholar]
- 42.Schulte am Esch J, Thiemig I, Pfeifer G, Entzian W. The influence of some inhalation anaesthetics on the intracranial pressure with special reference to nitrous oxide. Anaesthesist. 1979;28:136–41. [PubMed] [Google Scholar]
- 43.Schaffranietz L, Heinke W. The effect of different ventilation regimes on jugular venous oxygen saturation in elective neurosurgical patients. Neurol Res. 1998;20:S66–70. doi: 10.1080/01616412.1998.11740613. [DOI] [PubMed] [Google Scholar]
- 44.Myburgh J, Cooper DJ, Finfer S, Bellomo R, Norton R, Bishop N, et al. SAFE Study Investigators; Australian and New Zealand Intensive Care Society Clinical Trials Group; Australian Red Cross Blood Service; George Institute for International Health. Saline or albumin for fluid resuscitation in patients with traumatic brain injury. N Engl J Med. 2007;357:874–84. doi: 10.1056/NEJMoa067514. [DOI] [PubMed] [Google Scholar]
- 45.Baker AJ, Rhind SG, Morrison LJ, Black S, Crnko NT, Shek PN, et al. Resuscitation with hypertonic saline-dextran reduces serum biomarker levels and correlates with outcome in severe traumatic brain injury patients. J Neurotrauma. 2009;26:1227–40. doi: 10.1089/neu.2008.0868. [DOI] [PubMed] [Google Scholar]
- 46.Cooper DJ, Myles PS, McDermott FT, Murray LJ, Laidlaw J, Cooper G, et al. Prehospital hypertonic saline resuscitation of patients with hypotension and severe traumatic brain injury: A randomized controlled trial. JAMA. 2004;291:1350–7. doi: 10.1001/jama.291.11.1350. [DOI] [PubMed] [Google Scholar]
- 47.Ract C, Vigué B. Comparison of the cerebral effects of dopamine and norepinephrine in severely head-injured patients. Intensive Care Med. 2001;27:101–6. doi: 10.1007/s001340000754. [DOI] [PubMed] [Google Scholar]
- 48.Steiner LA, Johnston AJ, Czosnyka M, Chatfield DA, Salvador R, Coles JP, et al. Direct comparison of cerebrovascular effects of norepinephrine and dopamine in head-injured patients. Crit Care Med. 2004;32:1049–54. doi: 10.1097/01.ccm.0000120054.32845.a6. [DOI] [PubMed] [Google Scholar]
- 49.Johnston AJ, Steiner LA, Chatfield DA, Coles JP, Hutchinson PJ, Al-Rawi PG, et al. Effect of cerebral perfusion pressure augmentation with dopamine and norepinephrine on global and focal brain oxygenation after traumatic brain injury. Intensive Care Med. 2004;30:791–7. doi: 10.1007/s00134-003-2155-7. [DOI] [PubMed] [Google Scholar]
- 50.Sookplung P, Siriussawakul A, Malakouti A, Sharma D, Wang J, Souter MJ, et al. Vasopressor Use and Effect on Blood Pressure After Severe Adult Traumatic Brain Injury. Neurocrit Care. 2010 doi: 10.1007/s12028-010-9448-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Alvarez M, Nava JM, Rué M, Quintana S. Mortality prediction in head trauma patients: Performance of Glasgow Coma Score and general severity systems. Crit Care Med. 1998;26:142–8. doi: 10.1097/00003246-199801000-00030. [DOI] [PubMed] [Google Scholar]
- 52.Carlson AP, Schermer CR, Lu SW. Retrospective evaluation of anemia and transfusion in traumatic brain injury. J Trauma. 2006;61:567–71. doi: 10.1097/01.ta.0000231768.44727.a2. [DOI] [PubMed] [Google Scholar]
- 53.Salim A, Hadjizacharia P, DuBose J, Brown C, Inaba K, Chan L, et al. Role of anemia in traumatic brain injury. J Am Coll Surg. 2008;207:398–406. doi: 10.1016/j.jamcollsurg.2008.03.013. [DOI] [PubMed] [Google Scholar]
- 54.Hare GM, Tsui AK, McLaren AT, Ragoonanan TE, Yu J, Mazer CD. Anemia and cerebral outcomes: Many questions, fewer answers. Anesth Analg. 2008;107:1356–70. doi: 10.1213/ane.0b013e318184cfe9. [DOI] [PubMed] [Google Scholar]
- 55.Pendem S, Rana S, Manno EM, Gajic O. A review of red cell transfusion in the neurological intensive care unit. Neurocrit Care. 2006;4:63–7. doi: 10.1385/NCC:4:1:063. [DOI] [PubMed] [Google Scholar]
- 56.Ogawa Y, Iwasaki K, Aoki K, Shibata S, Kato J, Ogawa S. Central hypervolemia with hemodilution impairs dynamic cerebral autoregulation. Anesth Analg. 2007;105:1389–96. doi: 10.1213/01.ane.0000281910.95740.e4. [DOI] [PubMed] [Google Scholar]
- 57.Leal-Noval SR, Múñoz-Gómez M, Murillo-Cabezas F. Optimal hemoglobin concentration in patients with subarachnoid hemorrhage, acute ischemic stroke and traumatic brain injury. Curr Opin Crit Care. 2008;14:156–62. doi: 10.1097/MCC.0b013e3282f57577. [DOI] [PubMed] [Google Scholar]
- 58.Martini J, Carpentier B, Chávez Negrete A, Cabrales P, Tsai AG, Intaglietta M. Beneficial effects due to increasing blood and plasma viscosity. Clin Hemorheol Microcirc. 2006;35:51–7. [PubMed] [Google Scholar]
- 59.Leal-Noval SR, Rincón-Ferrari MD, Marin-Niebla A, Cayuela A, Arellano-Orden V, Marín-Caballos A, et al. Transfusion of erythrocyte concentrates produces a variable increment on cerebral oxygenation in patients with severe traumatic brain injury: A preliminary study. Intensive Care Med. 2006;32:1733–40. doi: 10.1007/s00134-006-0376-2. [DOI] [PubMed] [Google Scholar]
- 60.Zygun DA, Nortje J, Hutchinson PJ, Timofeev I, Menon DK, Gupta AK. The effect of red blood cell transfusion on cerebral oxygenation and metabolism after severe traumatic brain injury. Crit Care Med. 2009;37:1074–8. doi: 10.1097/CCM.0b013e318194ad22. [DOI] [PubMed] [Google Scholar]
- 61.Sharma D, Vavilala MS. Transfusion improves cerebral oxygenation. but not always. Crit Care Med. 2009;37:1166–7. doi: 10.1097/CCM.0b013e31819a0085. [DOI] [PubMed] [Google Scholar]
- 62.Sharma D, Vavilala MS. Should brain tissue oxygenation be the transfusion trigger in traumatic brain injury? Pediatr Crit Care Med. 2010;11:420–1. doi: 10.1097/PCC.0b013e3181c315c4. [DOI] [PubMed] [Google Scholar]
- 63.Chaiwat O, Lang JD, Vavilala MS, Wang J, MacKenzie EJ, Jurkovich GJ, et al. Early packed red blood cell transfusion and acute respiratory distress syndrome after trauma. Anesthesiology. 2009;110:351–60. doi: 10.1097/ALN.0b013e3181948a97. [DOI] [PubMed] [Google Scholar]
- 64.Vincent JL, Baron JF, Reinhart K, Gattinoni L, Thijs L, Webb A, et al. ABC (Anemia and Blood Transfusion in Critical Care) Investigators. Anemia and blood transfusion in critically ill patients. JAMA. 2002;288:1499–507. doi: 10.1001/jama.288.12.1499. [DOI] [PubMed] [Google Scholar]
- 65.Malone DL, Dunne J, Tracy JK, Putnam AT, Scalea TM, Napolitano LM. Blood transfusion, independent of shock severity, is associated with worse outcome in trauma. J Trauma. 2003;54:898–905. doi: 10.1097/01.TA.0000060261.10597.5C. [DOI] [PubMed] [Google Scholar]
- 66.Harhangi BS, Kompanje EJ, Leebeek FW, Maas AI. Coagulation disorders after traumatic brain injury. Acta Neurochir (Wien) 2008;150:165–75. doi: 10.1007/s00701-007-1475-8. [DOI] [PubMed] [Google Scholar]
- 67.Talving P, Benfield R, Hadjizacharia P, Inaba K, Chan LS, Demetriades D. Coagulopathy in severe traumatic brain injury: A prospective study. J Trauma. 2009;66:55–61. doi: 10.1097/TA.0b013e318190c3c0. [DOI] [PubMed] [Google Scholar]
- 68.Perel P, Roberts I, Shakur H, Thinkhamrop B, Phuenpathom N, Yutthakasemsunt S. Haemostatic drugs for traumatic brain injury. Cochrane Database Syst Rev. 2010;1:CD007877. doi: 10.1002/14651858.CD007877.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.CRASH-2 trial collaborators, Shakur H, Roberts I, Bautista R, Caballero J, Coats T, Dewan Y, et al. Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): A randomised, placebo-controlled trial. Lancet. 2010;376:23–32. doi: 10.1016/S0140-6736(10)60835-5. [DOI] [PubMed] [Google Scholar]
- 70.Oddo M, Levine JM, Frangos S, Carrera E, Maloney-Wilensky E, Pascual JL, et al. Effect of mannitol and hypertonic saline on cerebral oxygenation in patients with severe traumatic brain injury and refractory intracranial hypertension. J Neurol Neurosurg Psychiatry. 2009;80:916–20. doi: 10.1136/jnnp.2008.156596. [DOI] [PubMed] [Google Scholar]
- 71.Liu-DeRyke X, Collingridge DS, Orme J, Roller D, Zurasky J, Rhoney DH. Clinical impact of early hyperglycemia during acute phase of traumatic brain injury. Neurocrti Care. 2009;11:151–7. doi: 10.1007/s12028-009-9228-6. [DOI] [PubMed] [Google Scholar]
- 72.Jeremitsky E, Omert LA, Dunham CM, Wilberger J, Rodriguez A. The impact of hyperglycemia on patients with severe brain injury. J Trauma. 2005;58:47–50. doi: 10.1097/01.ta.0000135158.42242.b1. [DOI] [PubMed] [Google Scholar]
- 73.Sharma D, Jelacic J, Chennuri R, Chaiwat O, Chandler W, Vavilala MS. Incidence and risk factors for perioperative hyperglycemia in children with traumatic brain injury. Anesth Analg. 2009;108:81–9. doi: 10.1213/ane.0b013e31818a6f32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Young B, Ott L, Dempsey R, Haack D, Tibbs P. Relationship between admission hyperglycemia and neurologic outcome of severely brain-injured patients. Ann Surg. 1989;210:466–72. doi: 10.1097/00000658-198910000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lipshutz AK, Gropper MA. Perioperative glycemic control: An evidence-based review. Anesthesiology. 2009;110:408–21. doi: 10.1097/ALN.0b013e3181948a80. [DOI] [PubMed] [Google Scholar]
- 76.Rovlias A, Kotsou S. The influence of hyperglycemia on neurological outcome in patients with severe head injury. Neurosurgery. 2000;46:335–42. doi: 10.1097/00006123-200002000-00015. [DOI] [PubMed] [Google Scholar]
- 77.Bilotta F, Caramia R, Cernak I, Paoloni FP, Doronzio A, Cuzzone V, et al. Intensive insulin therapy after severe traumatic brain injury: A randomized clinical trial. Neurocrit Care. 2008;9:159–66. doi: 10.1007/s12028-008-9084-9. [DOI] [PubMed] [Google Scholar]
- 78.van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, et al. Intensive insulin therapy in the critically ill patients. N Engl J Med. 2001;345:1359–67. doi: 10.1056/NEJMoa011300. [DOI] [PubMed] [Google Scholar]
- 79.Finfer S, Chittock DR, Su SY, Blair D, Foster D, Dhingra V, et al. NICE-SUGAR Study Investigators, Intensive versus conventional glucose control in critically ill patients. N Engl J Med. 2009;306:1283–97. doi: 10.1056/NEJMoa0810625. [DOI] [PubMed] [Google Scholar]
- 80.Billotta F, Caramia R, Cernak I, Paoloni FP, Doronzio A, Cuzzone V, et al. Intensive insulin therapy after severe traumatic brain injury: A randomized clinical trial. Neurocrit Care. 2008;9:159–66. doi: 10.1007/s12028-008-9084-9. [DOI] [PubMed] [Google Scholar]
- 81.Bower WF, Lee PY, Kong AP, Jiang JY, Underwood MJ, Chan JC, et al. Peri-operative hyperglycemia: A consideration for general surgery? Am J Surg. 2010;199:240–8. doi: 10.1016/j.amjsurg.2009.04.010. [DOI] [PubMed] [Google Scholar]
- 82.Diltoer M, Camu F. Glucose homeostasis and insulin secretion during isoflurane anesthesia in humans. Anesthesiology. 1988;68:880–6. doi: 10.1097/00000542-198806000-00008. [DOI] [PubMed] [Google Scholar]
- 83.Kitamura T, Ogawa M, Kawamura G, Sato K, Yamada Y. The effects of sevoflurane and propofol on glucose metabolism under aerobic conditions in fed rats. Anesth Analg. 2009;109:1479–85. doi: 10.1213/ANE.0b013e3181b8554a. [DOI] [PubMed] [Google Scholar]
- 84.Peterson K, Carson S, Carney N. Hypothermia treatment for traumatic brain injury: A systematic review and meta-analysis. J Neurotrauma. 2008;25:62–71. doi: 10.1089/neu.2007.0424. [DOI] [PubMed] [Google Scholar]
- 85.Edwards P, Arango M, Balica L, Cottingham R, El-Sayed H, Farrell B, et al. CRASH trial collaborators. Final results of MRC CRASH, a randomised placebo-controlled trial of intravenous corticosteroid in adults with head injury-outcomes at 6 months. Lancet. 2005;365:1957–9. doi: 10.1016/S0140-6736(05)66552-X. [DOI] [PubMed] [Google Scholar]


