Abstract
Aim
To assess veterans’ experience and satisfaction in using the Surgeon General’s (SG) online family health history (FHH) tool, and determine the perceived facilitators and barriers to using the online SG-FHH tool.
Materials & methods
A mixed-method using both qualitative and quantitative approaches was employed in this study. A total of 35 veterans at the VA Medical Center in San Antonio, Texas, USA were invited to enter their FHH information using the online SG-FHH tool, complete the study’s satisfaction survey and participate in a short semi-structured interview. The goal of the semi-structured interviews was to assess participants perceived facilitators and barriers to using the online SG-FHH tool. All participants were also provided with a printed copy of their pedigree, which was generated by the SG-FHH tool and were encouraged to share it with their relatives and providers.
Results
The majority of participants (91%) said that they had access to a computer with internet capability and 77% reported that they knew how to use a computer. More than two-thirds of the participants felt that items on the SG-FHH tool were easy to read and felt that FHH categories were relevant to their family’s health. Approximately 94% of participants viewed the SG-FHH tool as useful, and the majority of participants (97%) indicated that they were likely to recommend the tool to others. Content analysis of the semi-structured interviews highlighted several barriers to veterans’ use of the SG-FHH tool and their FHH information. These included: lack of patients’ knowledge regarding their relatives’ FHH, and privacy and confidentiality concerns.
Conclusion
This study provides information on the performance and functionality of an inexpensive and widely accessible method for FHH collection. Furthermore, our findings highlight several opportunities and challenges facing the utilization of FHH information as a clinical and genomic tool at the Veterans Health Administration (VHA). The results suggest that strategies that improve veterans’ knowledge regarding the importance of their FHH information and that address their concerns about privacy and confidentiality may enhance the successful implementation of FHH information into VHA clinical practice.
Implications
identifying a locally accepted method for FHH collection and documentation which can be conducted outside of the patient visit will reduce time burdens for providers and patients and allow for a focus on other important topics during clinic visits. Improvement in familial risk screening and assessment will enable the VHA to be prepared for personalized medicine and focus their resources on promoting critically important health behaviors for populations with the highest risk of developing chronic diseases and their complications.
Keywords: family health history, genomic services, Surgeon General’s online tool
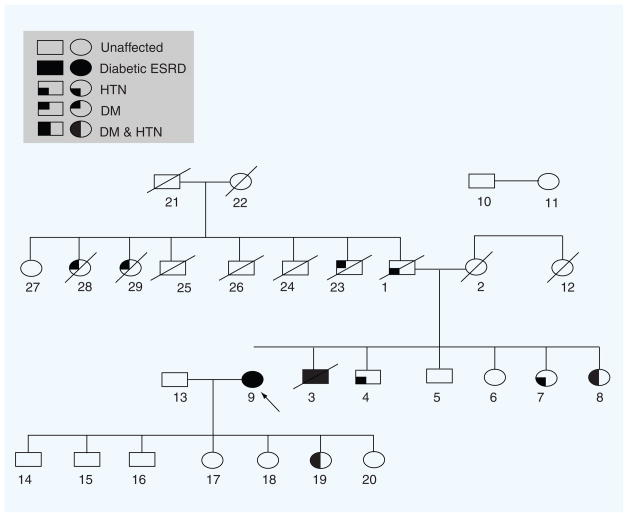
Comprehensive familial risk assessment represents a critical step towards the implementation of personalized medicine and will complement current/future genetic testing [1,2]. Using a systematic approach for collecting and documenting detailed family health history (FHH) information (Figure 1) will help in screening, identifying and tracking veterans at high risk of common chronic diseases so that they can be offered further genetic testing as appropriate and special preventive measures. Improvement in familial risk screening and assessment will enable the Veterans Health Administration (VHA) to be prepared for personalized medicine and focus resources on promoting critically important health behaviors for populations with the highest risk of developing chronic diseases and their complications.
Figure 1. Example of detailed family health history (pedigree).
Index case (proband) shown by arrow.
DM: Diabetes mellitus; ESRD: End-stage renal disease; HTN: Hypertension.
Despite increasing evidence supporting the importance and potential benefits of detailed FHH information in disease screening and risk assessment [3–5], its underutilization by patients and healthcare providers has been well documented [5–10]. A reason for this includes patients’ lack of awareness regarding the implications of FHH for disease risk and prevention [6,7]. Ethical concerns as a result of using FHH information, such as insurance discrimination, may also hinder use of FHH information by patients and providers [5,9,11]. Additional barriers commonly cited by providers include potential time constraints and increased workloads, compensation and reimbursement concerns and perceived lack of expertize in genomics and abilities to interpret FHH information [5,7–9].
Increasing advancements in health information technology may provide opportunities to promote the use of the FHH information by addressing some aforementioned concerns. For instance, Fuller et al. examined providers’ perspectives on patient-generated pedigrees for FHH collection in their clinics [12]. The majority of respondents in the study favored patient- generated pedigrees compared with the usual/standard approach, with results indicating stronger support for computer-generated pedigrees over hand-drawn pedigrees. Most providers agreed that computer-generated pedigrees would improve upon their current methods (e.g., using paper-based forms to collect FHH information during patients’ visit) as they contain more FHH information and allow for easier identification of at-risk patients.
In additon, recent studies assessing patient satisfaction and experiences in using computerized or web-based health tools have demonstrated overall positive reactions. In a study examining satisfaction in using a secured web-site providing shared personal health records between patients and providers, Ralston et al. found that 94% of patients were satisfied with the program [13]. In another study, Atack et al. evaluated the usability of a website providing tailored health education to patients. In addition to general high levels of satisfaction with the online program, they discovered that patients favored the benefit of an online program’s 24-h access to health information and the ability to explore the tool at their own pace and time; this is especially true for those who may not be as proficient in using the computer [14]. These findings indicating patients’ high interest and satisfaction in using technology for health information suggest that computerized, web-based tools may facilitate the use of FHH information.
Several web-based tools have been developed to collect both general FHH information as well as disease-specific FHH information [8,15,16]. One such tool is ‘My Family Health Portrait’. a free, broad-based FHH tool developed by the Centers for Disease Control and Prevention and US Surgeon General’s (SG) Office [101]. The SG-FHH tool is designed to help users collect and organize data on their personal medical history as well as health information on their first-, second- and third-degree relatives. FHH information can be added and edited as needed. The SG-FHH tool generates a pedigree that can be saved for future reference, or printed to share with family members and healthcare providers [15,17]. The SG-FHH tool has been validated for accurate collection of FHH information for some common heritable conditions including diabetes [18].
A leader in the development and use of health information technology is the VHA. Along with their computerized patient record system, the VHA has developed My HealtheVet, a web-based personal health records portal, which features a FHH module and access to the SG-FHH tool. The SG-FHH tool includes additional detailed FHH information not available on My HealtheVet, including age at diagnosis of disease and a family pedigree diagram. To build upon the capacity of the FHH module, in our study we examined veterans’ experience and satisfaction in using the online SG-FHH tool and their views on facilitators and barriers to using the online SG-FHH tool.
Materials & methods
Invitation letters containing a postage-paid return envelope and response card were mailed to a random sample of 60 veterans, selected from a patient list of those seeking care at the VA Medical Center (VAMC) in San Antonio, Texas, USA. The study coordinator contacted veterans who expressed an interest in participating and scheduled an appointment at the VAMC to proceed with enrollment. We achieved a response rate of 58% (n = 35). We did not collect information on reasons for refusal. However, we speculate that time demands and concerns about privacy related to using online tools have affected veterans’ participation in this study. After a brief 5-min orientation to the online SG-FHH tool by the study coordinator, consented participants entered their FHH information into the SG-FHH tool. The study coordinator documented the length of time participants required to complete the forms on the SG-FHH tool. After completing the FHH forms, participants were asked to complete a survey and participate in a short semi- structured interview. At the end of the session, all participants were provided with a printed copy of their pedigree, which was generated from the SG-FHH tool and encouraged to share it with their relatives and healthcare providers. The study was approved by the Institutional Review Board at the University of Texas Health Science Center at San Antonio (TX, USA).
Survey instrument
The study used a modified version of the American Customer Satisfaction Survey (ACSS) [19,20]. The ACSS contained 11 questions that assessed drivers of satisfaction (i.e., accessibility, content, functionality, look and feel and performance) in using the SG-FHH tool. Questions related to basic demographic information (i.e., gender, age, race/ethnicity, marital status, level of education, employment status and income) were also included on the survey.
Semi-structured interview
The interview included four questions that focused on perceived facilitators and barriers to utilizing the online SG-FHH tool and FHH information in general. Examples of some open-ended questions include:
What are the key barriers you foresee to using SG-online tool for collecting FHH information?
How do you plan to address and overcome these barriers?
What are the key facilitators you foresee in using SG-online tool for collecting FHH information?
Data analysis
Data from the veterans’ surveys was assessed by descriptive statistics such as frequencies for categorical variables (e.g., level of education) and means, medians and quartiles for continuous variables (e.g., age and beliefs). All quantitative data analyses were performed using SAS 9.1 (SAS Institute, NC, USA). Qualitative analysis was performed to examine veterans’ views regarding barriers or facilitators to using the SG-FHH tool. Content analysis of veterans’ responses to the semi-structured interviews was conducted in three steps. First, for each participant, we built an initial matrix which consisted of cells presenting veterans’ responses extracted from the interviews. The text of the cells was either direct quotations or summations of responses. Second, we examined the initial matrices in order to identify patterns across cases. Patterns recognized in this analysis formed the basis of additional categorization to construct higher-level matrices [21,22]. All interview materials were checked and evaluated in order to assure consistency in coding and classification procedures. The analysis was conducted primarily by one experienced (in qualitative methods) researcher, while another research assistant independently read half of the transcripts to confirm the integrity of the emerging themes and concepts. Inter-coder reliability was assured by a coding comparison method. Once development of the coding tree was advanced, the researchers and the assistants involved in this project recoded 20% of the transcribed materials selected at random. Agreement was acceptable (Kappa coefficients = 0.75). We used the software NVivo (QSR International Pty Ltd, CA, USA) to perform the content analysis [102].
Results
Demographic characteristics of study participants
Participants’ average age was 60.6 ± 13.3 years (range: 29–88 years). Over 50% of the participants (66%) were male, and 71% of participants described themselves as non-Hispanic white. Nearly all participants (97%) indicated that they had attended and completed at least some college or technical school. In addition, 23% of patients who could not use the computer were found to be over 60 years of age (Table 1).
Table 1.
Demographic characteristics of study participants (n = 35).
| Characteristic | Value (%) |
|---|---|
|
Age
| |
| Mean ± SD | 60.6 ± 13.3 |
|
| |
|
Gender
| |
| Male | 23 (66) |
| Female | 12 (34) |
|
| |
|
Race/ethnicity
| |
| Non-Hispanic white | 16 (46) |
| Hispanic or latino | 10 (29) |
| Black or African–American | 7 (20) |
| White and American–Indian/Alaska native | 1 (3) |
| No response | 1 (3) |
|
| |
|
Marital status
| |
| Single, never married | 3 (9) |
| Married | 22 (63) |
| Separated | 2 (6) |
| Divorced | 4 (11) |
| Widowed | 3 (9) |
| Other | 1 (3) |
|
| |
|
Education
| |
| Some high school | 1 (3) |
| Some college/technical school | 19 (54) |
| College graduate | 15 (43) |
|
| |
|
Income
| |
| <$25,000 | 4 (11) |
| $25,001–35,000 | 4 (11) |
| $35,001–50,000 | 6 (17) |
| $50,001–75,000 | 9 (26) |
| >$75,000 | 5 (14) |
| Do not wish to provide information | 7 (20) |
SD: Standard deviation.
Overall assessment of the SG-FHH tool
On average, participants spent 25 min completing the forms on the SG-FHH tool, with recorded times ranging between 15 and 40 min. The participants rated their overall experience using the online SG-FHH tool as positive. Many participants stated the tool had a user-friendly format and instructions; those who had a working knowledge of computers navigated the tool with ease. Participants praised the tool as a novel way to view one’s FHH information. One participant commented: “I think it’s wonderful – with a click of a button, you can see everything”. Participants also enjoyed the convenience of the tool in maintaining updated FHH information and in sharing FHH information with various providers. In addition, one individual stated: “The mere fact of seeing a bigger picture of my and my family’s health is a big motivator (to facilitate use of FHH information)”. Another participant remarked that the SG-FHH tool can “make you take a hard look at your own health and inspire you to improve your health”. Finally, several participants noted the increased advantage of early utilization of the SG-FHH tool, as one participant stated: “I think this will potentially be a valuable tool in the future, especially if it is begun when a person is young”. In addition, some felt that this tool provided a means for older generations to impart FHH knowledge to younger generations; one person added: “It will help us to encourage our children to know how important it is (to use FHH tool)”. Even those who felt that the tool did not offer any personal benefits still accepted the potential benefits for the health of their children and other younger relatives. For instance, a participant stated: “I already know my personal FHH, but it would be good and helpful for my nieces and nephews”.
Satisfaction in using the SG-FHH tool
The majority of participants (91%) reported having access to a computer with internet and 77% claimed that they knew how to use a computer, while 23% indicated that they are unable to use a computer (Table 2). More than two thirds of the participants felt that items on the SG-FHH tool were easy to understand and felt that FHH categories were relevant to their family’s health. Approximately 94% of participants viewed the SG-FHH tool as being useful (Table 3), and the majority of participants (97%) indicated that they would likely to recommend the tool to others (Table 4).
Table 2.
Veterans’ reported access to a computer and internet (n = 35).
| Participants responses | Frequency (%) |
|---|---|
|
Access to computer with internet to complete SG-FHH tool
| |
| Poor access | 3 (9) |
| Moderate access | 13 (37) |
| Excellent access | 19(54) |
|
| |
|
Ability to use computer
| |
| Not able | 8 (23) |
| Moderately able | 12 (34) |
| Very able | 15 (43) |
SG-FHH: Surgeon General’s family health history.
Table 3.
Veterans satisfaction in using the online Surgeon General’s family health history tool (n = 35).
| Participants responses | Frequency (%) |
|---|---|
|
Definition of FHH categories in SG-FHH tool
| |
| Not clear | 2 (6) |
| Moderately clear | 11 (33) |
| Very clear | 21 (61) |
|
| |
|
Relevance of FHH categories in SG-FHH tool to own family
| |
| Not relevant | 2 (6) |
| Moderately relevant | 13 (37) |
| Very relevant | 20 (57) |
|
| |
|
Ability to complete SG-FHH tool
| |
| Not able | 6 (17) |
| Moderately able | 12 (34 |
| Very able | 17 (49) |
|
| |
|
Usefulness of SG-FHH tool
| |
| Not useful | 2 (6) |
| Useful | 11 (31) |
| Very useful | 22 (63) |
|
| |
|
Ease of reading items in SG-FHH tool
| |
| Not easy | 1 (3) |
| Easy | 12 (35) |
| Very easy | 22 (62) |
|
| |
|
Speed of loading pages in SG-FHH tool
| |
| Very poor | 0 |
| Poor | 8 (24) |
| Excellent | 26 (76) |
FHH: Family health history; SG-FHH: Surgeon General’s family health history.
Table 4.
Veterans’ response to recommend the Surgeon General’s family health history tool (n = 35).
| Participants responses | Frequency (%) |
|---|---|
|
Likelihood to recommend SG-FHH tool
| |
| Not likely | 1 (3) |
| Modestly likely | 12 (23) |
| Very likely | 26 (74) |
|
| |
|
Likelihood to recommend linking SG-FHH tool to My HealtheVet (n = 26†)
| |
| Not likely | 1 (4) |
| Modestly likely | 8 (30) |
| Very likely | 17 (66) |
|
| |
|
Likelihood to recommend linking SG-FHH tool to CPRS
| |
| Not likely | 4 (1) |
| Modestly likely | 9 (26) |
| Very likely | 22 (63) |
Only 26 participants responded to the question on the likelihood to recommend linking SG-FHH tool to My HealtheVet.
CPRS: Computerized patients records; SG-FHH: Surgeon General’s family health history.
Barriers to using the SG-FHH tool
Content analysis of the semi-structured interviews highlighted several barriers to veterans’ use of the SG-FHH tool and their FHH information. These included: lack of patients’ knowledge regarding their relatives’ FHH and privacy and confidentiality concerns.
Lack of FHH knowledge
Approximately two thirds of the participants (69%) cited their lack or limited knowledge concerning their FHH information as a barrier to using the SG-FHH tool. One common reason was a minimal communication between family members; one participant explicitly stated: “Communication is key to knowing FHH information”, and another participant identified a “lack of family closeness” as a barrier. Factors that may contribute to this limited communication between relatives may be due to having family members who prefer not to share personal health information or who live in far proximity from relatives and infrequent interaction between families. For instance, one participant commented: “My sisters are pretty private”, referring to a lack of sibling FHH information. Some participants (26%) had minimal or no FHH knowledge of their extended family and only knew the health history of their immediate family. Furthermore, some participants (20%), especially those who were older in age, revealed that many of their family members had already passed away and thus they had no way of obtaining past relatives’ FHH information.
Limited computer/internet access or ability
Participants over 60 years of age had limited or no access to a computer with internet capability; highlighting computer and internet issues as an obstacle inherent in using a computerized or web-based tool. One participant stated: “What will hinder my use of this tool would be the lack of knowledge/operation of using the computer”. Another participant asserted that despite the SG-FHH tool’s potential, “many will be/are incapable of filling it out, especially postworld war II generation veterans … they can’t use the computer”. Furthermore, an additional concern was that the distinct features offered in the SG-FHH tool would be lost to users without the assistance of an informed and trained person, as in the case of the research coordinator in this study; this may particularly be an issue among those with limited computer abilities. One participant stated: “It would be helpful to have someone who knows the tool to show you how to use it”, and another participant suggested: “It would be helpful to have someone explaining everything (because) it may not be easy for all users, especially older people”.
Privacy & confidentiality concerns
Approximately half of the participants (46%) raised concerns about the privacy and confidentiality of their FHH information. Related to these concerns were fears regarding insurance discrimination, including service-connected disability benefits at the VHA (29%). Participants feared that using such a tool in the future and presenting their FHH information to providers could potentially affect their and their family members’ veteran-related healthcare benefits if FHH information were disclosed. For instance, one participant stated: “This (tool) is great as long as the healthcare agencies don’t get access to it … because they can deny policies or increase cost according to this information”. Participants feared that if their FHH information revealed that a condition for which they are currently receiving veteran-related care were to be attributed to FHH rather than service-connected circumstances, it may no longer be covered by veteran benefits.
Discussion
Collecting and documenting detailed FHH information (Figure 1) is essential for accurate familial risk assessment. Genetic heritage is only one component of disease etiology for complex conditions within families and increased inflammation linked to pedigrees relating to environmental, occupational and lifestyle exposures could be critical in understanding disease patterns. By identifying patterns of diseases among relatives, healthcare providers can decide whether individuals or other family members may be at an increased risk of developing a particular condition [1–3]. In addition, healthcare providers may recommend more frequent screening (such as a mammography or colonoscopy) starting at an earlier age for people at an increased risk of certain cancers [12]. Healthcare providers may encourage regular checkups or testing for people with a medical condition that runs in their family [13]. Besides, knowing FHH allows a person to make lifestyle changes such as adopting a healthier diet, getting regular exercise and quitting smoking to reduce the chances of developing heart disease and other common illnesses [14]. Using detailed FHH information (Figure 1) will be increasingly important for accurate personalized familial risk assessments and will complement any current or future genetic screening tools [13,15,101]. Despite mounting evidence regarding the importance of FHH information and risk assessment in health-care, to date, promising approaches in screening and identifying at-risk individuals have not been broadly applied [16]. This is mainly owing to barriers related to collecting and documenting FHH information in busy primary care settings [17–19]. This study provides information on the performance and functionality of an inexpensive and widely-accessible method for the collection of FHH information that can be integrated into clinical practice to aid providers in identifying individuals most in need of genetic testing, screening and other preventive measures. Participants spent, on average, 25 min to complete the forms on the SG-FHH tool. While the length of time needed to complete the tool has been estimated to be 15 min [103], we have found that most participants in our study needed more time, sometimes as long as 40 min. As those with a high level of computer skills required at least 15 min to complete the tool, those with a minimal level of computer skills may require even more time.
Most participants responded positively to the SG-FHH tool, and found that it was a useful instrument to effectively organize and share their FHH information with their healthcare providers and relatives. Several participants also felt that this tool enabled individuals to share FHH information with their younger family members and recognized the benefit of FHH information for their children and relatives’ health. These results are consistent with recent findings by Simon et al. who also reported that respondents expressed interest in using a computerized tool for cancer family history [23].
Despite veterans’ overall satisfaction in using the SG-FHH tool, the results also demonstrate that a lack of or having minimal knowledge about one’s FHH is a significant barrier to collecting FHH. Current literature similarly corresponds with this finding related to patients’ limited knowledge of their FHH information [5,6]. For instance, a study by Walter et al. found that patients’ perception of factors that constitute having a FHH of illness varied significantly [10], and Sifri et al. found that even among patients who may be aware of some FHH information, very few reported knowing pertinent details, such as the age at diagnosis [24]. Furthermore, studies have demonstrated that the public not only lacks knowledge about FHH, but genetics and genomics as a whole. In a recent study by Hahn et al., focus group findings demonstrated that many community members have a limited understanding of genomic medicine and revealed misconceptions related to genomic medicine [25]. Similarly, 57% of respondents from a study by Henneman et al. reported perceiving a lack of genetic knowledge. In addition, computer and/or internet challenges were revealed to potentially deter individuals from utilizing the SG-FHH tool [26]. As many new healthcare innovations are becoming increasingly technologically based and as the current trend of computer users is moving to younger individuals, this suggests that computerized, web-based tools may potentially be better and more advantageously utilized in younger populations [23,27,104]. Participants in our study concurred with this sentiment, stating that the tool may encourage younger generations, such as their children and grandchildren, to take preventive measures and show them the importance of FHH information. Furthermore, for individuals to utilize their FHH information, measures will need to be taken to ensure privacy and confidentiality and to alleviate the insurance concerns many have expressed. Similar concerns regarding genetic discrimination have been well-documented in previous studies [23,25,28–30]. While several state and federal laws have already been enacted to prohibit genetic discrimination by insurance providers [31,32], many individuals may be unaware of these protections [28,33]. It is important to point out that the Genetic Information Non-Discrimination Act (GINA) has been in place since 2008 [105]. This law prohibits genetic discrimination by employers and health insurers based on family history. Patients should be educated about this and other state laws that may protect them.
Therefore, although most participants viewed the SG-FHH tool favorably, it will be imperative to address reported barriers in order to enhance the utilization of FHH information. Specifically, future interventions should focus on educating patients about the importance of FHH information and activating them to engage in the collection and documentation of their FHH. Furthermore, efforts should be made to increase awareness about existing laws protecting patients from genetic discrimination so as to address any concerns related to the disclosure of FHH information and to promote the future use of genomic services.
Study limitations
While our study findings highlighted several opportunities and challenges related to the utilization of FHH information as a clinical and genomic tool at the VHA, limitations include the small sample size, the high percentage of male participants and potential response bias, as veterans who are more interested in computers/the internet or in FHH information may have been more likely to participate in the study. The main goal of this study was to gain an in depth understanding of veterans’ responses to using online tools in order to collect and document their FHH information. The sample size of 35 subjects is appropriate for collecting observation/qualitative data; however, this sample size will not provide sufficient statistical power for testing the study hypotheses. A follow-up study that includes a larger and representative sample of the general population is justified.
In addition, while this study assessed veterans’ ability and satisfaction in using the SG-FHH tool, it does not report on actual behaviors regarding whether or not they shared their FHH information with their family or healthcare providers. Future research should include a larger sample of veterans, including returning OEF/OIF (‘Operation Enduring Freedom’ and ‘Operation Iraqi Freedom’) veterans, to analyze this study’s barriers with a more diverse population.
Our work contributes to ongoing efforts of integrating and translating genomic research findings into clinical practice. The findings from our study suggest that promoting the use of a web-based FHH tool, such as the SG-FHH tool, has implications for primary-care providers and their patients. The utilization of FHH information as a clinical and genomic tool has the potential to reduce healthcare costs by improving familial risk screening and assessment and enabling healthcare organizations to focus their resources on populations with the highest risk of developing chronic diseases or disease complications.
Future perspective
Family health history information represents a critical step towards the implementation of personalized medicine and will complement current/future genetic testing. FHH information captures the interactions of genetic susceptibility and the shared environment, and therefore has the potential to maximize screening through the identification of individuals at increased risk of common diseases such as diabetes and cancer. Despite mounting evidence regarding the importance of FHH information and risk assessments in healthcare, to date, promising approaches in screening and identifying at-risk individuals have not been broadly applied. Using detailed FHH information will be increasingly important and will complement any current or future genetic screening tools. Future research will be geared towards developing and implementing system-based interventions that will improve the delivery and adoption of personalized familial risk assessment, thereby improving healthcare for veterans at risk of, or with, common chronic diseases. Despite of many opportunities exisiting, several important challenges related to the delivery of personalized familial risk assessment will not be resolved. Just two challenges are the lack of patients’ knowledge regarding their relatives’ FHH, and privacy and confidentiality concerns. Altogether, these challenges will lead to a fundamental paradigm shift in current healthcare practices that, in turn, may lead to changes in the business and regulatory models.
Executive summary.
Aim
We assessed veterans’ experience and satisfaction in using the Surgeon General’s (SG) online family health history (FHH) tool, and perceived facilitators and barriers to using the online SG-FHH tool.
Results
Most participants had access to a computer with internet capability and reported that they know how to use a computer.
More than two thirds of the participants felt that items in the SG-FHH tool were easy to read and felt that FHH categories were relevant to their family’s health.
Almost all participants viewed the SG-FHH tool as useful, and the majority of participants indicated that they were likely to recommend the tool to others.
Content analysis of the semi-structured interviews highlighted several barriers to veterans’ use of the SG-FHH tool and their FHH information. These included: lack of patients’ knowledge regarding their relatives’ FHH, and privacy and confidentiality concerns.
Conclusion
Our findings highlighted several opportunities and challenges facing the utilization of FHH information as a clinical and genomic tool at the Veterans Health Administration.
The results suggest that strategies to improve veterans’ knowledge regarding the importance of their FHH information and address their concerns about privacy and confidentiality may enhance successful implementation of FHH information into Veterans Health Administration clinical practice.
The utilization of FHH information as a clinical and genomic tool has the potential to reduce healthcare costs by improving familial risk screening and assessment and enabling healthcare organizations to focus their resources on populations with the highest risk of developing chronic diseases or disease complications.
Footnotes
For reprint orders, please contact: reprints@futuremedicine.com
Author disclosure
The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Ethical conduct of research
The authors state that they have obtained appropriate institutional review board approval or have followed the principles outlined in the Declaration of Helsinki for all human or animal experimental investigations. In addition, for investigations involving human subjects, informed consent has been obtained from the participants involved.
Financial & competing interests disclosure
This work was supported by the VHA-HSR and D (DNA 08-129 and PPO 09-241, PI: Nedal Arar). This study was partly funded by the Clinical and Translational Science Award (CTSA) – NIH grant (UL1RR025767). The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
Bibliography
- 1.Yoon PW, Scheuner MT, Khoury MJ. Research priorities for evaluating family history in the prevention of common chronic diseases. Am J Prev Med. 2003;24(2):128–135. doi: 10.1016/s0749-3797(02)00585-8. [DOI] [PubMed] [Google Scholar]
- 2.Scheuner MT, Wang SJ, Raffel LJ, et al. Family history: a comprehensive genetic risk assessment method for the chronic conditions of adulthood. Am J Med. 1997;71(3):315–324. doi: 10.1002/(sici)1096-8628(19970822)71:3<315::aid-ajmg12>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (CDC) Awareness of family health history as a risk factor for disease. MMWR Morb Mortal Wkly Rep. 2004;53:1044–1047. [PubMed] [Google Scholar]
- 4.Hariri S, Yoon PW, Moonesinghe R, Valdez R, Khoury MJ. Evaluation of family history as a risk factor and screening tool for detecting undiagnosed diabetes in a nationally representative survey population. Genet Med. 2006;8(12):752–759. doi: 10.1097/01.gim.0000250205.73963.f3. [DOI] [PubMed] [Google Scholar]
- 5.Guttmacher AE, Collins FS, Carmona RH. The family history – more important than ever. N Engl J Med. 2004;351(22):2333–2336. doi: 10.1056/NEJMsb042979. [DOI] [PubMed] [Google Scholar]
- 6.Acheson LS, Wang C, Zyzanski SJ, et al. Family Healthware Impact Trial (FHITr) Group. Family history and perceptions about risk and prevention for chronic diseases in primary care: a report from the family healthware impact trial. Genet Med. 2010;12(4):212–218. doi: 10.1097/GIM.0b013e3181d56ae6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rich EC, Burke W, Heaton CJ, et al. Reconsidering the family history in primary care. J Gen Intern Med. 2004;19(3):273–280. doi: 10.1111/j.1525-1497.2004.30401.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yoon PW, Scheuner MT, Jorgensen C, Khoury MJ. Developing family healthware, a family history screening tool to prevent common chronic disease. Prev Chronic Dis. 2009;6(1):A33. [PMC free article] [PubMed] [Google Scholar]
- 9.Arar N, Seo J, Abboud HE, et al. Providers’ behavioral beliefs regarding the delivery of genomic medicine at the Veterans Health Administration. Personalized Medicine. 2010;7(5):485–494. doi: 10.2217/pme.10.47. [DOI] [PubMed] [Google Scholar]
- 10.Walter FM, Emery J. ‘Coming down the line’ – patients’ understanding of their family history of common chronic disease. Ann Fam Med. 2005;3(5):405–414. doi: 10.1370/afm.368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scheuner MT, Sieverding P, Shekelle PG. Delivery of genomic medicine for common chronic adult diseases: a systematic review. JAMA. 2008;299(11):1320–1334. doi: 10.1001/jama.299.11.1320. [DOI] [PubMed] [Google Scholar]
- 12.Fuller M, Myers M, Webb T, Tabangin M, Prows C. Primary care providers’ responses to patient-generated family history. J Genet Couns. 2010;19(1):84–96. doi: 10.1007/s10897-009-9264-6. [DOI] [PubMed] [Google Scholar]
- 13.Ralston JD, Carrell D, Reid R, Anderson M, Moran M, Hereford J. Patient web services integrated with a shared medical record: patient use and satisfaction. J Am Med Inform Assoc. 2007;14(6):798–806. doi: 10.1197/jamia.M2302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Atack L, Luke R, Chien E. Evaluation of patient satisfaction with tailored online patient education information. Comput Inform Nurs. 2008;26(5):258–264. doi: 10.1097/01.NCN.0000304838.52207.90. [DOI] [PubMed] [Google Scholar]
- 15.Feero WG, Bigley MB, Brinner KM. New standards and enhanced utility for family health history information in the electronic health record: an update from the American Health Information Community’s Family Health History Multi-Stakeholder Workgroup. J Am Med Inform Assoc. 2008;15(6):723–728. doi: 10.1197/jamia.M2793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Valdez R, Yoon PW, Qureshi N, Green RF, Khoury MJ. Family history in public health practice: a genomic tool for disease prevention and health promotion. Annu Rev Public Health. 2010;31:69–87. doi: 10.1146/annurev.publhealth.012809.103621. [DOI] [PubMed] [Google Scholar]
- 17.Giovanni MA, Murray MF. The application of computer-based tools in obtaining the genetic family history. Curr Protoc Hum Genet. 2010;Chapter 9(Unit 9.21) doi: 10.1002/0471142905.hg0921s66. [DOI] [PubMed] [Google Scholar]
- 18.Facio FM, Feero WG, Linn A, Oden N, Manickam K, Biesecker LG. Validation of My Family Helath Portrait for six common heritable conditions. Genet Med. 2010;12(6):370–375. doi: 10.1097/GIM.0b013e3181e15bd5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fornell C, Johnson MD, Anderson EW, Cha J, Bryant BE. The American Customer Satisfaction Index: nature, purpose, and findings. J Mark. 1996;60(4):7–18. [Google Scholar]
- 20.Arar NH, Hazuda HP, Steinbach R, Arar MY, Abboud HE. Ethical issues associated with conducting genetic family studies of complex disease. Ann Epidemiol. 2005;15(9):712–719. doi: 10.1016/j.annepidem.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 21.Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook. 2. Thousand Oaks; Sage Publications, CA, USA: 1994. [Google Scholar]
- 22.Bernard HR. Research Methods in Cultural Anthropology. Sage Publications; Newbury Park, CA, USA: 1988. [Google Scholar]
- 23.Simon C, Acheson L, Burant C, et al. Patient interest in recording family histories of cancer via the internet. Genet Med. 2008;10(12):895–902. doi: 10.1097/GIM.0b013e31818de708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sifri RD, Wender R, Paynter N. Cancer risk assessment from family history: gaps in primary care practice. J Fam Pract. 2002;51(10):856. [PubMed] [Google Scholar]
- 25.Hahn S, Letvak S, Powell K, et al. Genomedical Connection. A community’s awareness and perceptions of genomic medicine. Public Health Genomics. 2010;13(2):63–71. doi: 10.1159/000218712. [DOI] [PubMed] [Google Scholar]
- 26.Henneman L, Timmermans DRM, van der Wal G. Public experiences, knowledge and expectations about medical genetics and the use of genetic information. Community Genet. 2004;7(1):33–43. doi: 10.1159/000080302. [DOI] [PubMed] [Google Scholar]
- 27.Cho AH, Arar NH, Edelman DE, Hartwell PH, Oddone EZ, Yancy WS., Jr Do diabetic veterans use the internet? Self-reported usage, skills, and interest in using My HealtheVet web portal. Telemed J E Health. 2010;16(5):595–602. doi: 10.1089/tmj.2009.0164. [DOI] [PubMed] [Google Scholar]
- 28.Hall MA, Rich SS. Patients fear of genetic discrimination by health insurers: the impact of legal protections. Genet Med. 2000;2:213–221. doi: 10.1097/00125817-200007000-00003. [DOI] [PubMed] [Google Scholar]
- 29.Beene-Harris RY, Wang C, Bach JV. Barriers to access: results from focus groups to identify genetic service needs in the community. Community Genet. 2007;10:10–18. doi: 10.1159/000096275. [DOI] [PubMed] [Google Scholar]
- 30.Arar N, Seo J, Lee S, et al. Preferences regarding genetic research results: comparing veterans and nonveterans responses. Public Health Genomics. 2010;13(7–9):431–439. doi: 10.1159/000317099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ginsburg GS. Genomic medicine: ‘grand challenges’ in the translation of genomics to human health. Eur J Hum Genet. 2008;16:873–874. doi: 10.1038/ejhg.2008.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Epps PG. Policy before practice: genetic discrimination reviewed. Am J Pharmacogenomics. 2003;3:405–418. doi: 10.2165/00129785-200303060-00008. [DOI] [PubMed] [Google Scholar]
- 33.Hall MA, McEwen JE, Barton JC, et al. Concerns in a primary care population about genetic discrimination by insurers. Genet Med. 2005;7(5):311–316. doi: 10.1097/01.gim.0000162874.58370.c0. [DOI] [PubMed] [Google Scholar]
Websites
- 101.US Department of Health and Human Services. News release: Surgeon General’s New Family health history tool is released, ready for ‘21st century medicine’. [Accessed 21 February 2011];2009 www.hhs.gov/news/press/2009pres/01/20090113a.html.
- 102.QSR International Pty Ltd. www.qsrinternational.com/about-qsr_company-profile.aspx.
- 103.ACSI: ACSI Methodology. http://theacsi.org/index.php?option=com_content&task=view&id=48&Itemid=41.
- 104.Rideout V, Neuman T, Kitchman M, Brodie M. e-Health and the elderly: how seniors use the internet for health information. Key findings from a national survey of older Americans. Program for the Study of Media and Health. Kaiser Family Foundation. 2005 www.kff.org/entmediaupload/e-Health-and-the-Elderly-How-Seniors-Use-the-Internet-for-Health-Information-Key-Findings-From-a-National-Survey-of-Older-Americans-Survey-Report.pdf.
- 105.Genetic Information Non-Discrimination Act. www.eeoc.gov/laws/types/genetic.cfm.