Abstract
Objectives:
This study aimed to estimate the prevalence of uncontrolled hypertension (HTN) among Omani hypertensive patients, on treatment and under primary health care (PHC) follow-up in Al Seeb Wilayat, Oman. Socio-demographic and clinical factors were explored for possible influence on blood pressure (BP) control.
Methods:
Based on an assumption of 50% prevalence of uncontrolled HTN, a retrospective data collection was conducted on the last three follow-up visits of 411 randomly selected Omani adults (≥18 years) from 3,459 hypertensive patients. Adequate BP control was defined using criteria from 7th Report of the Joint National Committee on Prevention Detection Evaluation & Treatment of High Blood Pressure (JNC-7). A P value of <0.05 and odds ratios with 95% confidence interval were used to assess for association.
Results:
The targets for adequate BP control were achieved in 39% of the studied patients (95% confidence interval [CI]: 34–44%). Lower BP control was found among hypertensives with diabetes (6.4%, P = <0.001) and renal disease (18.5%, P = 0.02); those with cardiovascular disease (CVD) showed relatively better control (58%). Age and gender had no impact on BP control. Most patients were only on one (24%) or two (47%) antihypertensive medications, the most frequently used being β-blockers (58.2%) and diuretics (56.3%).
Conclusion:
HTN is not adequately controlled in over 60% of treated patients; the presence of co-morbidity and less than aggressive treatment are significant contributors. Improving the quality of HTN care is a priority; effective efforts should be undertaken to improve BP control.
Keywords: Hypertension, Primary care, Oman
Advances in Knowledge
Control of hypertension (HTN) among Omani adult hypertensive patients on treatment was significantly suboptimal.
Hypertensive patients who were obese, diabetic or had renal disease were at higher risk for uncontrolled HTN.
It is likely that the treatment of most hypertensive patients was inadequate and should have been more aggressive.
It seems that our primary care physicians have insufficient knowledge and experience in treating HTN to achieve international targets.
Applications to Patient Care
Improving the quality of HTN care in primary health care settings is a priority and effective efforts need to be undertaken in this regard.
Hypertensive patient who are also obese or diabetic should be targeted for a greater attention to blood pressure control.
Primary care physicians should be encouraged to become familiar with updated evidence-based HTN management guidelines.
Hypertension (HTN) is a major medical problem affecting more than 1 billion individuals worldwide.1 It is sufficiently common to represent a public health concern in Oman as well. According to preliminary data from the World Health Survey is 2008 (currently in press), the community prevalence of HTN in the country was estimated to be 40% and a further 17% of the population had pre-HTN.2 Three quarters of this hypertensive population were found to be unaware of their HTN. Solid data on the number of hypertensive patients under follow-up at different health facilities is limited.
Across the globe, it is well established that high blood pressure (BP) is a leading modifiable risk factor for cardiovascular disease, cerebrovascular disease, heart failure and renal disease.3,4 Reviewed literature has shown a consistent, strong relationship between higher levels of both systolic and diastolic BP, as well as mortality from these diseases.5 Generally, the higher the BP, the greater is the risk. Cohort studies and randomised clinical trials have shown that the risks from raised HTN can be partially reversed if an optimal BP control is achieved.6,7
HTN has been considered to be a common reason for patients to be seen by primary care physicians.8 It is generally accepted that well organised healthcare can improve the outcome in hypertensive patients,9 and clinical trials have clearly demonstrated that adequate BP control can be achieved in most patients.10,11 Still, uncontrolled HTN is a challenge for primary health care (PHC) services all over the world. The direct reasons for this global epidemic of uncontrolled HTN are not well understood, but it seems that the barriers for adequate control of HTN are complex and arise from a combination of factors related to patients, physicians and health systems.12 Studies have shown the influence of socio-demographic factors, such as age, gender and co-morbidity, on HTN control was variable with contradictory findings.13–16 Similar findings have been shown for the influence on BP of the number of antihypertensive medications taken by patients.
The prevalence of uncontrolled HTN in Oman and possible associated factors have not been adequately studied to date. Only a single small study was conducted between 1998 and 2002 in a tertiary hospital setting and it showed that BP control was 35% for Omani hypertensive patients examined, versus 53% for non-Omani.17
The current study aims to obtain an insight into the prevalence of uncontrolled HTN among Omani hypertensive patients on treatment and follow-up at the PHC settings in an urban town in Oman. Furthermore, certain socio-demographic and clinical factors will be explored for their possible influence on BP control.
Methods
The study was conducted using a retrospective data collection of hypertensive patients seen in the six PHC centres serving Al-Seeb Wilayat, an urban area belonging to the Muscat governorate of Oman. Al-Seeb is the most populated wilayat (district) in Oman with more than 225,000 residents.18 A total of 3,459 patients were registered as hypertensive patients and were under-follow up at HTN Clinics in these six PHC centres by 1 June 2009. A hypertensive patient usually attends the clinic every one to three months for follow-up and on monthly basis for a repeat prescription.
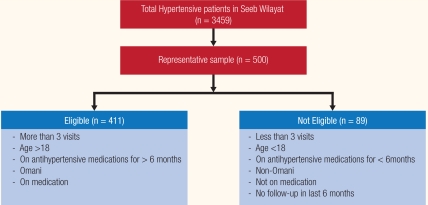
The sample size based on the assumption of a 50% prevalence of uncontrolled BP, α = 0.05, and permissible error of 5% on either side of the estimate to be around 400. To account for the inclusion criteria, a total of 500 patients were then selected randomly using computer-generated numbers. All adult Omani hypertensive patients aged ≥18 years, who had made at least three previous PHC visits and had been on antihypertensive medications for at least 6 months, were included. Newly diagnosed individuals, those having less than three previous BP readings and those without any follow-up in the previous 6 months were excluded from the study. Despite being at risk of inadequate BP control, hypertensive patients who were not on pharmacotherapy were also excluded as the majority of them were found to be either newly diagnosed, or not on the expected regular follow-up. A total of 411 patients (82.2%) met the inclusion criteria. Figure 1 summarises the selection process of the patients in the study.
Figure 1:
Selection of patients in the study.
The following information was collected from the electronic records of the patients’ last three visits: age, gender, duration of follow-up, three most recent BP readings, presence of co-existing diseases, current smoking status, body mass index (BMI), prescribed regular medications, frequency of attendance at the outpatient clinic (in the last 6 months) and presence or absence of care continuity. The traditional definition of ‘continuity of care’ is the patient’s experience of a “continuous caring relationship’ with an identified health care professional”.19 In this study continuity of care was defined as any included patient having been seen by same physician in the last three visits.
Uncontrolled HTN was defined based on guidelines from 7th Report of the Joint National Committee on Prevention Detection Evaluation & Treatment of High Blood Pressure (JNC-7) as a BP of >140/90 mm Hg or >130 mmHg systolic and >80 mmHg diastolic with coexisting diabetes or renal disease.1 Uncontrolled HTN was based on the average of the collected three BP readings and it could be either uncontrolled in systolic, diastolic or both.
Data were entered by authors 1 and 3, then analysed by author 2 using the Statistical Package for Social Sciences (SPSS, IBM, USA, Version 17.0). The chi-squire test was used to evaluate the association between qualitative variables (uncontrolled HTN and different independent variables). A P value of 0.05 or less was considered statistically significant. In addition, variables with a P value of less than 0.25 were included in a multivariate logistic regression model. Odds ratios (OR) with a 95% confidence interval for those variables was then estimated. Ethical approval was obtained from the Regional Research and Ethics Committee, Directorate General of Health Services, Governorate of Muscat.
Results
Data on a total of 411 subjects who met the inclusion criteria were analysed. The mean length of follow-up in the same clinic for the studied population was 5 ± 2 years. Their mean age ± standard deviation (SD) was 57 ± 12 years, and 68% (n = 281) were females. Only 39% (n = 160; 95% confidence interval [CI]: 34–44%) had a mean BP up to the goal. Table 1 describes the demographic and clinical characteristics of the patients with controlled and uncontrolled HTN. It can be observed that the age and gender of the subjects had no impact on BP control. Smoking was a measurable problem as 8% (n = 34) of subjects were documented as smokers; however, they were equally divided between the controlled and uncontrolled groups (P = 0.59).
Table 1:
Demographic and clinical characteristics of the study stratified by blood pressure (BP) goal attainment as per the 7th Report of the Joint National Committee on Prevention Detection Evaluation & Treatment of High Blood Pressure (JNC-7) recommendations
| Blood pressure Goal as per JNC-7 | PValue | |||
|---|---|---|---|---|
| No (n = 251, 61.1%) | Yes (n = 160, 38.9%) | |||
| Demographic data (n, % unless indicated otherwise) | ||||
| Age, mean ± SD, in years | 56.40 ± 12.17 | 57.43 ± 11.87 | 0.393 | |
| Female gender | 173 (68.9) | 108 (67.5) | 0.762 | |
| Male gender | 78 (31.1) | 52 (32.5) | 0.762 | |
| Smoking status | 21 (8.3) | 13 (8.1) | 0.593 | |
| Clinical data (n, % unless indicated otherwise) | ||||
| Dyslipidemia | 101(40) | 70 (44) | 0.570 | |
| CVD | 15 (6) | 21 (13) | 0.477 | |
| Diabetes mellitus | 88 (35.0) | 6 (4.0) | 0.001 | |
| Stroke | 5 (2.0) | 6 (2.4) | 0.416 | |
| Nephropathy | 22 (8.8) | 5 (3.1) | 0.024 | |
| Retinopathy | 1(0.4) | 0 (0) | 0.389 | |
| Thyroid disease | 9 (3.6) | 8 (5) | 0.703 | |
| Asthma | 11(4.4) | 11 (6.9) | 0.469 | |
| BMI | Normal | 55 (22) | 43 (26.9) | |
| Overweight | 60 (24) | 53 (33) | 0.021 | |
| Obese | 133 (53) | 59 (36.8) | ||
| Length of follow-up in the same clinic (mean ± SD) | 4.95 ± 2.18 | 5.01 ± 2.17 | 0.620 | |
| Non-adherence to scheduled follow-up appointments | 200 (80) | 76 (48) | 0.696 | |
| Continuity of care | 17 (7) | 12 (8) | 0.892 | |
Legend: SD = Standard deviation; CVD = cardiovascular disease; BMI = Body Mass Index; BP control was defined as casual BP of <140 (systolic) and <90 mmHg (diastolic) and <130 (systolic) and <80 mmHg (diastolic) for diabetic patients as per the JNC-7.
Around 23% of hypertensive patients in this study were diabetic; 47% were dyslipidemic; 9% had cardiovascular disease (CVD), and 6.5% were labelled as having kidney disease. The presence of diabetes mellitus or chronic kidney disease was associated with significantly poorer BP control, as more than 93% (n = 88/94) and 81% (n = 22/27) of these patients respectively had uncontrolled HTN. The presence of CVD, however, was associated with relatively better BP control, as 58% of hypertensive patients with CVD achieved their BP targets. The presence of dyslipidemia failed to show any association with the control of HTN. In addition, 74% (n = 305) of the total subjects were overweight (27%) or obese (47%). Of those who were obese, 69% failed to achieve their BP targets (P = 0.02). Being overweight was not a determinant of HTN control status, nor was normal weight.
Only 29 individuals (7%) of the total 411 analysed subjects experienced continuity of care in relation to their HTN management and follow-up. The statistical analysis did not show any association between continuity of care and HTN control (P = 0.89). Of 276 individuals with a history of non-adherence to scheduled HTN clinic follow-up appointments, 72% had inadequate BP control.
A total of 100 subjects (24%) were on a single anti-hypertensive medication, 193 subjects (47%) were on two medications, 96 subjects (23%) were on three medications, and only 18 subjects (4%) were on more than three anti-hypertensive drugs [Table 2]. Those on monotherapy were more likely to attain their BP control than those on two or more drugs (49% versus 37.8 and 31.3% respectively; P = 0.043). The most commonly prescribed antihypertensive agents were β-blockers and diuretics, 58% and 56% respectively. The class of antihypertensive agent had no influence on HTN control among those patients on monotherapy.
Table 2:
Patient and health care related factors and pharmaceutical characteristics of the study stratified by blood pressure (BP) goal attainment as per the 7th Report of the Joint National Committee on Prevention Detection Evaluation & Treatment of High Blood Pressure recommendations
| Blood pressure Goal as per JNC7 | PValue | ||
|---|---|---|---|
| No (n = 251 (61.1%) | Yes (n = 160 (38.9%) | ||
| Level of Antihypertensive Therapy | |||
| Mono therapy | 51 (20%) | 49 (30%) | 0.043 |
| Dual therapy | 113 (45%) | 80 (50%) | |
| Triple therapy | 61 (24%) | 35 (22%) | |
| More than three medications | 10 (4%) | 8 (5%) | |
Discussion
Inadequate control of HTN appears to be a significantly prevalent problem challenging the PHC system in Oman, as is the case globally. In this practice-based study, the majority (61%) of hypertensive patients failed to reach the targeted BP goals. This can potentially make a significant impact on the morbidity and mortality associated with cardiovascular disease, stroke and other HTN-related diseases. Almost 20% of the national total hospital deaths in adults aged ≥45 yrs are collectively due to HTN-related diseases (ischaemic heart disease 9.7%, cerebrovascular disease 6.8%, and heart failure 3.1%), while direct hypertensive diseases are estimated to account for 3.6% of total deaths.20 Inadequate control of HTN not only has significant consequences in terms of patient morbidity and mortality, but also in terms of health care costs.21
The high prevalence of uncontrolled HTN suggests that a substantial number of cardiovascular events can be prevented by improving BP control. Using data from the Third National Health & Nutrition Examination Survey (NHANES III), Wong et al. estimated that control of HTN to levels recommended by the JNC could prevent 19–56% of coronary heart disease events in men and 31–57% of coronary heart disease events in women, depending on the BP achieved.22
The level of HTN control found in our study (39%) was similar to that reported in a smaller hospital-based study conducted 8 years earlier in Oman (41%).17 The situation of HTN control in the Arabian Gulf region is no better. Reports from Saudi Arabia and Bahrain showed a control rate of 25% and 16.5% respectively.23,24 Globally, HTN control rates vary from one country to another, from as low as 5.4% in Korea to as high as 58% in Barbados, with a worldwide average of around 30%,9 which clearly demonstrates the worldwide difficulty in achieving satisfactory BP control.
As shown in Table 1, only half of those 24% who were on a single antihypertensive medication achieved their BP targets. Research has demonstrated that BP targets will be reached in only 40–50% of patients taking any single antihypertensive agent.25 The HTN management and control guideline by JNC-71 has recommended that most patients with HTN will require two or more antihypertensive medications to achieve goal BP (<140/90 mmHg, or <130/80 mmHg for patients with diabetes or chronic kidney disease). Several previous studies26,27 have shown that primary care physicians may not be managing HTN aggressively enough, and the majority was satisfied with the existing BP values.
On the other hand and despite the fact that three quarters of our patients were on two or more antihypertensive medications (the majority taking two drugs), the control of HTN in this group was relatively worse than in those taking a single drug. Similar findings were reported in a neighbouring country.23 These findings contradict what is concluded by major clinical trials that effective BP control is better achieved with two or more antihypertensive drugs for most patients.28–30 The association between BP control and level of management is not so self-evident. Patient characteristics may contribute a significant influence. Our patients who were on monotherapy were likely to have been diagnosed more recently and have less complications and co-morbidities, be younger in age and more involved in their care, and hence probably complied better with the recommended lifestyle adjustments.
The current study has also shown that diabetes, dyslipidemia and obesity were common co-morbidities among hypertensive patients. The relatively low prevalence (23%) of diabetes among the study population is likely not a representative figure of diabetics with co-existing HTN. This is due to the fact that in those PHC centres involved in the study most diabetic patients with HTN were seen and followed-up in the Diabetic Clinic rather than in the HTN Clinic.
It is well accepted that patients who have both diabetes and HTN are at a greater risk for cardiovascular events compared to non-diabetic hypertensive patients.31 Despite this, research by Abbott et al. has shown poor BP control in diabetic patients with only 11% of the diabetic patients treated for HTN reported as having achieved the systolic BP goal of <130 mmHg.32 A similar percentage was found in a national study where the BP control in diabetics was (10%).17 Our study demonstrated remarkably poor control of HTN among hypertensive patients with diabetes mellitus (6%, P = 0.001) as well as those with renal insufficiency (18%, P = 0.02). These findings could be related to the strict definition of controlled BP in diabetic and kidney disease patients (i.e. <130/80 mmHg) used in this study. It is likely that such a target might not yet be fully employed or accepted in routine practice.
In this study, CVD was found to be relatively associated with better BP control. Such a positive effect was observed by other studies as well.15,33 The mechanism of this effect is not clear, but it might be a result of improved compliance in these patients or more aggressive treatment by a specialist rather than by a PHC physician.
Another potentially important observation was the relationship between poor BP control and the presence of obesity (P = 0.02), in addition to the high prevalence of obesity (47%) among the studied population. These remarkable figures make it necessary for the health care providers in PHC settings to be aware of the importance of emphasising the treatment of obesity as part of the management of HTN, if better HTN control is to be achieved.
Although this study failed to show any statistically significant association between the control of HTN and continuity of care (as defined in this study), the importance of this aspect in the long term management of chronic diseases like HTN is beyond doubt. The absence of such an aspect from the care provided for hypertensive patients in all PHC centres in this study was a significant defect which needs to be addressed.
Several limitations of this study deserve mention. As this is a retrospective study, no information was available on how BP was measured and recorded which might question the accuracy of the BP readings obtained. The absence of some data from patients’ electronic records could also have affected the findings and their ability to be generalised. A possible bias in this study is related to hypertensive patients who were also diabetics and whose HTN was followed-up in the diabetic clinic; they were thus not registered as hypertensive and so not included in the study. Another possible bias might also arise from the exclusion of hypertensive patients who were not on anti-hypertensive medication. However, such biases, if true, could contribute to further supporting our findings of poor HTN control since the excluded group could be expected to have even worse BP control. This study was conducted in PHC centres where family physicians were available, which is not the case in other PHC centres in rural parts of Oman. This limits the generalisation of the results to the whole of Oman. The lack of a global assessment of cardiovascular risk for each patient was another limitation.
Conclusion
The present study concluded that HTN is not adequately controlled in over 60% of treated patients, and that is explained by different factors including co-existing conditions like diabetes and obesity, as well as insufficient pharmacological treatment in many patients. Moreover, it seems that our primary care physicians have little training and experience in treating to target, as we have observed with the results of hypertensive patients with diabetes and renal disease. Improving the quality of HTN care is a priority and effective efforts need to be taken in order to improve BP control among hypertensive patients. Clinical experience affords sufficient reason not to delay aggressive treatment in patients with uncontrolled HTN. Obese patients and diabetics should be targeted for even greater attention to BP control. Any effort to decrease any degree of BP which is above the normal range is beneficial.
Further improvements in HTN control will require changes in physician behaviour which should be associated with more awareness of and familiarity with updated evidence-based practice guidelines. Further research is needed to explore in depth different underlying factors influencing the appropriate HTN control.
Acknowledgments
The authors also would like to thank Dr. Abdullah Al-Muniri for his generous help with the statistical part of the study.
Footnotes
CONFLICT OF INTEREST
The authors reported no conflict of interest.
References
- 1.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LE, Izzo JL, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 2.Preliminary data from World Health Survey . 2008 Used with permission from Non-Communicable Disease Department. Ministry of Health; Oman: 2010. (in press). [Google Scholar]
- 3.Berrios X, Kopnen T, Huiguang T, Khaltaev N, Puska P, Nissinen A. Distribution and prevalence of major risk factors of non-communicable diseases in selected countries: WHO Inter-Health Program. Bull World Health Organ. 1997;75:99–108. [PMC free article] [PubMed] [Google Scholar]
- 4.US Department of Health and Human Services . Screening for Hypertension: The Guide to Clinical Preventive Services: Task force. 2nd ed. 1996. pp. 39–53. [Google Scholar]
- 5.Al-Rukban MO, Al-Sughair AM, Al-Bader BO, Al-Tolaihi BA. Management of hypertensive patients in primary health care setting, auditing the practice, Saudi Arabia. Saudi Med J. 2007;28:85–90. [PubMed] [Google Scholar]
- 6.Konzem SL, Devore VS, Bauer DW. Controlling hypertension in patients with diabetes. Am Fam Physician. 2002;66:1209–14. [PubMed] [Google Scholar]
- 7.Padwal R, Straus SE, McAlister FA. Cardiovascular risk factors and their effects on the decision to treat hypertension: Evidence based review. BMJ. 2001;322:977–80. doi: 10.1136/bmj.322.7292.977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bernard DB, Townsend RR, Sylvestri MF. Health and disease management: What is it and where is it going? What is the role of health and disease management in hypertension? Am J Hypertens. 1998;11:103–11. doi: 10.1016/s0895-7061(98)00103-4. [DOI] [PubMed] [Google Scholar]
- 9.Kearney PM, Whelton M, Reynolds K, Whelton PK, He J. Worldwide prevalence of hypertension: A systematic review. J Hypertens. 2004;22:11–19. doi: 10.1097/00004872-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Cushman WC, Ford CE, Cutler JA, Marqolis KL, Davis BR, Grimm RH, et al. Success and predictors of blood pressure control in diverse North American settings: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) J Clin Hypertens. 2002;4:393–404. doi: 10.1111/j.1524-6175.2002.02045.x. [DOI] [PubMed] [Google Scholar]
- 11.Black HR, Elliott WJ, Neaton JD, Grandits G, Grambsch P, Grimm RH, Jr, et al. Baseline characteristics and elderly blood pressure control in the CONVINCE Trial. Hypertension. 2001;37:12–8. doi: 10.1161/01.hyp.37.1.12. [DOI] [PubMed] [Google Scholar]
- 12.Düsing R. Overcoming barriers to effective blood pressure control in patients with hypertension. Curr Med Res Opin. 2006;22:1545–53. doi: 10.1185/030079906X120995. [DOI] [PubMed] [Google Scholar]
- 13.Avanzini F, Alli C, Colombo F, Tognoni G. Control of hypertension in Italy: Results of the Study on Antihypertensive Treatment in General Practice (STAP) G Ital Cardiol. 1998;28:760–6. [PubMed] [Google Scholar]
- 14.Inkster M. Organizational factors in relation to control of blood pressure: An observational study. J Gen Pract. 2005;55:931–7. [PMC free article] [PubMed] [Google Scholar]
- 15.Deqli Esposti E, Di Martino M, Sturani A, Russo P, Dradi C, Falcinelli S, et al. Risk factors for uncontrolled hypertension in Italy. J Hum Hypertens. 2004;18:207–13. doi: 10.1038/sj.jhh.1001656. [DOI] [PubMed] [Google Scholar]
- 16.Llisterri Caro JL, Rodríguez Roca GC, Alonso Moreno FJ, Lou Arnol S, Divisón Garrote JA, Santos Rodríguez JA, et al. Blood pressure control in Spanish hypertensive patients in primary health care centers. PRESCAP 2002 Study. Med Clin (Barc) 2004;122:165–71. doi: 10.1016/s0025-7753(04)74183-4. [DOI] [PubMed] [Google Scholar]
- 17.Almahrezi A, Al-Zakwani I, Al-Aamri A, Al-Khaldi S, Al-Zadjali N, Al-Hatali M, et al. Control and management of hypertension at a university health centre in Oman. SQU Med J. 2006:179–84. [PMC free article] [PubMed] [Google Scholar]
- 18.Oman Census 2003 Report. Muscat: Oman Census Administration, Ministry of National Economy; 2004. [Google Scholar]
- 19.Gulliford M, Naithani S, Morgan M. What is ‘Continuity of Care’? J Health Serv Res Policy. 2006;11:248–50. doi: 10.1258/135581906778476490. [DOI] [PubMed] [Google Scholar]
- 20.Department of Health Information & Statistics, Directorate General of Planning, Ministry of Health, Oman Annual Health Report 2009. Muscat: Ministry of Health; 2010. [Google Scholar]
- 21.Kalantan KA, Mohamed AG, Al-Taweel AA, Abdulghani HM. Hypertension among attendants of primary health care centers in Al-Qassim Region, Saudi Arabia. Saudi Med J. 2001;22:960–3. [PubMed] [Google Scholar]
- 22.Wong ND, Thakral G, Franklin SS, L’Italien GJ, Jacobs MJ, Whyte JL, et al. Preventing heart disease by controlling hypertension: Impact of hypertensive subtype, stage, age, and sex. Am Heart J. 2003;145:888–95. doi: 10.1016/S0002-8703(02)94787-3. [DOI] [PubMed] [Google Scholar]
- 23.Al-Rukban MO, Al-Sughair AM, Al-Bader BO, Al-Tolaihi BA. Management of hypertensive patients in primary health care setting: Auditing the practice. Saudi Med J. 2007;28:85–90. [PubMed] [Google Scholar]
- 24.Al Khaja KA, Sequeira RP, Damanhori AH. Treatment of hypertension in Bahrain. Ann Pharmacother. 2003;37:1511–17. doi: 10.1345/aph.1C430. [DOI] [PubMed] [Google Scholar]
- 25.Materson BJ, Reda DJ, Cushman WC. Department of Veterans Affairs Cooperative Study Group on Antihypertensive Agents. Department of Veterans Affairs single-drug therapy of hypertension study. Revised figures and new data. Am J Hypertens. 1995;8:189–92. doi: 10.1016/0895-7061(94)00196-i. [DOI] [PubMed] [Google Scholar]
- 26.Oliveria SA, Lapuerta P, McCarthy BD, L’Italien GI, Berlowitz DR, Asch SM. Physician-related barriers to the effective management of uncontrolled hypertension. Arch Intern Med. 2002;162:413–20. doi: 10.1001/archinte.162.4.413. [DOI] [PubMed] [Google Scholar]
- 27.Sever PS. Blood pressure control for the hypertensive patient: What can we do better? Am J Hypertens. 1997;10:128–30. doi: 10.1016/s0895-7061(97)00100-3. [DOI] [PubMed] [Google Scholar]
- 28.Fox JC, Leight K, Sutradhar SC, Demopoulos LA, Gleim GW, Lewin AJ, et al. The JNC-7 Approach compared to conventional treatment in diabetic patients with hypertension: A double-blind trial of initial monotherapy vs. combination therapy. J Clin Hypertens (Greenwich) 2004;6:437–442. doi: 10.1111/j.1524-6175.2004.03488.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jamerson K, Bakris GL, Dahlof B, Pitt B, Velazquez E, Gupte J, et al. Exceptional early blood pressure control rates: The ACCOMPLISH Trial. Blood Press. 2007;16:80–86. doi: 10.1080/08037050701395571. [DOI] [PubMed] [Google Scholar]
- 30.Neutel JM, Smith DH, Weber MA, Schofield L, Purkayastha D, Gatlin M. Efficacy of combination therapy for systolic blood pressure in patients with severe systolic hypertension: The Systolic Evaluation of Lotrel Efficacy and Comparative Therapies (SELECT) study. J Clin Hypertens. 2005;7:641–6. doi: 10.1111/j.1524-6175.2005.04615.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Casiglia E, Zanette G, Mazza A, Donadon V, Donada C, Pizziol A, et al. Cardiovascular mortality in non-insulin dependent diabetes mellitus. A controlled study among 683 diabetics and 683 age- and sex-matched normal subjects. Eur J Epidemiol. 2000;16:677–84. doi: 10.1023/a:1007673123716. [DOI] [PubMed] [Google Scholar]
- 32.Abbott K, Basta E, Bakris GL. Blood pressure control and nephroprotection in diabetes. J Clin Pharmacol. 2004;44:431–8. doi: 10.1177/0091270004263046. [DOI] [PubMed] [Google Scholar]
- 33.Knight EL, Bohn RL, Wang PS, Glynn RJ, Mogun H, Avorn J. Predictors of uncontrolled hypertension in ambulatory patients. Hypertension. 2001;38:809–14. doi: 10.1161/hy0901.091681. [DOI] [PubMed] [Google Scholar]