Abstract
Schwannomas are benign, encapsulated and slow-growing nerve sheath tumours arising from Schwann cells. The schwannoma arising from the cervical sympathetic chain (SCSC) is a very rare tumour. It usually presents as a slow growing, painless and asymptomatic neck mass, hence preoperative clinical diagnosis is difficult. Radiological investigation and fine needle aspiration cytology make only a small contribution to its preoperative diagnosis, histopathological examination being much more useful. We report here the first case report of SCSC from Oman. It occurred in a 45 year-old female and was successfully excised.
Keywords: Schwannoma, Cervical sympathetic chain, Excision, Case report, Oman
A schwannoma in the head and neck region may arise from any peripheral, cranial or autonomic nerve, except from the optic and olfactory nerve.1 This tumour arises from the Schwann cells, which are the precursor cells of the nerve sheath, and it occurs along the length of the nerves. These tumours are well encapsulated and nerve fibres often splay out on the surface so it never penetrates the capsule.2 In the head and neck region, schwannomas are categorised according the site of the origin nerve. The schwannoma arising from the cervical sympathetic chain (SCSC) is a very rare lesion and, until the time of this report, only 60 cases had been reported in English medical literature.3 The SCSC typically presents as painless, asymptomatic neck mass. This is due to the fact that the cervical sympathetic chain (CSC) runs in a relatively loose fascial compartment and compression is rare.
Radiological tests and fine needle aspiration cytology (FNAC) have only a small contribution in its preoperative diagnosis, histopathological examination being much more useful. On a computed tomography (CT) scan, these tumours show as a well circumscribed, solitary, round or oval shaped hypo-attenuated mass with poor contrast enhancement and are medial to carotid vessels.4 Imaging scans usually show anterolateral displacement of carotid vessels and the internal jugular vein. Because of lack of specific symptoms and the rarity of this lesion it can be mistaken preoperatively for a branchial cyst, lymphoma or metastatic node.5 The definitive diagnosis has to be made by histopathological examination of the excised specimen. The treatment of choice is surgical excision and recurrence is very rare. We report the first case report of SCSC from Oman which occurred in a female patient and was excised successfully. A review of the literature is also included.
Case Report
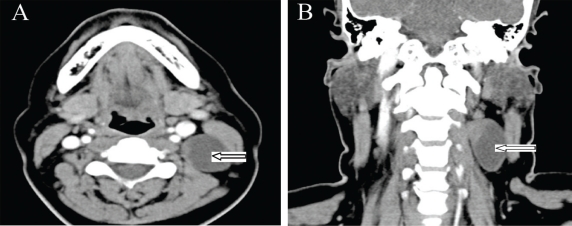
A forty-five year-old female patient presented to the outpatient department at Sultan Qaboos University Hospital, Oman, with a complaint of a painless mass on the left side of the upper lateral part of neck which had been slowly increasing in size for the previous nine months. On examination, there was a 2 x 2.5 cm firm mass in the left side of the upper part of neck under the sternocleidomastoid muscle. The overlying skin was normal and no visible pulsation was seen, nor was there any bruit on auscultation. A flexible nasopharyngolaryngoscopy showed normal nasopharynx, pharynx and larynx. A contrast enhanced CT scan of the neck showed a well encapsulated cystic mass posterior to the carotid vessel and internal jugular vein and was reported as a branchial cyst [Figure 1]. The FNAC from the swelling was inconclusive and so it was decided to excise the mass.
Figure 1.
A & B: Preoperative computed tomography scan of (A) axial and (B) coronal sections of the neck showing a well circumscribed cystic mass (arrows) posterior to carotid sheath in middle of neck.
The excision of the mass was done with a longitudinal incision along the posterior border of the sternocleidomastoid muscle. A sub-platysmal flap was elevated and the mass was found to be arising from the cervical sympathetic chain with some cystic consistency. It was carefully separated from the nerve and was excised completely. Postoperatively, the patient did well and did not develop Horner’s syndrome.
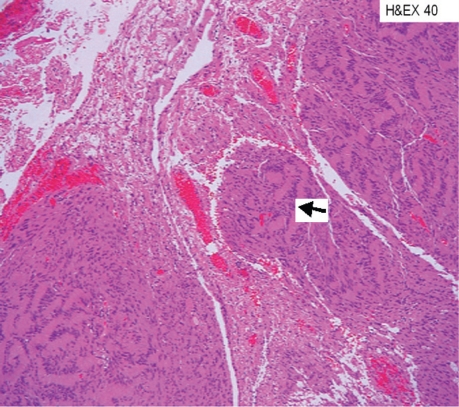
Histopathological examination of the resected specimen showed a cystic mass with some areas of solid encapsulations. Microscopy examinations showed characteristic Antoni A and B patterns suggesting the diagnosis of schwannoma [Figure 2]. The immunohistochemistry was positive for S-100 thus confirming the diagnosis. At the time of writing, the patient had been free from any locoregional recurrence for one and a half years.
Figure 2:
Histological microphotograph showing the typical Antoni type A and B pattern of schwannoma (haematoxylin and eosin stain x 40).
Discussion
SCSC is a benign nerve sheath tumour that occurs along the length of the nerves. These tumours are well encapsulated and nerve fibres often splay out on the surface, but never penetrate the capsule. A review of the literature disclosed fewer than 60 cases of schwannomas of the CSC to date.2 It is a solitary, slow growing tumour and generally seen in patients between 20 and 50 years of age. As this lesion is so often misdiagnosed, some non-diagnostic and unsuccessful surgical procedures are often performed before a definitive diagnosis is made. Frequency is the same in both sexes and malignant change is very rare.6
Schwannoma of the head and neck can be divided into those of cochleovestibular and non-vestibular nerve origins. The majority of these schwannomas are of non-vestibular origin and have been reported to arise from various sites including the middle ear, mastoid cavity, sinonasal region, orbit, neck, posterior pharynx, parapharyngeal space, and skull base.6,7 In the neck region, the vagus nerve is the most commonly involved nerve followed by the CSC.8
The cervical sympathetic ganglia are part of the sympathetic chain in the neck region and run longitudinally over the longus capitis and longus colli muscles, as far as the pre-vertebral fascia. They are comprised of three ganglia—the superior, middle, and the inferior ganglion. The superior ganglion is largest and most constant and lies at the level of the carotid sinus (C2–C4) .The middle ganglion lies at the level of C6 while the inferior ganglion is variable in position and may fuse with the first thoracic ganglion to form the stellate ganglion. In most cases reported in the literature, the SCSC arises from the superior or middle part of the sympathetic chain.
The differential diagnoses of SCSC include carotid body tumours, deep lobe parotid tumours, minor salivary gland tumours, lymphoma, branchial cleft cyst, vagal schwannoma, distant metastases, sympathicoblastoma, leiomyoma, teratoma, neurofibroma, aneurysm of the internal carotid artery, and rhabdomyoma.9
The presence of Horner’s syndrome is very rare before the surgery and, even when present, does not indicate the nerve of origin.10 Only in 10 cases of SCSC, did patients have Horner’s syndrome preoperatively.2 FNAC has a limited role and is not useful in diagnosis as it was seen in our case; the majority of studies do not recommend it preoperatively.5
Radiological examinations have a definite role in the preoperative diagnosis of this lesion. They help by assessing the extent of the tumour and its relationship with carotid vessels and the internal jugular vein. On a contrast enhanced CT scan, the mass appears as an isodense or hypoattenuated, well circumscribed, round to oval in shape lession with anterior displacement of carotid vessels. There can be heterogeneity due to cystic degeneration, xanthomatous change, or due to areas of relative hypocellularity adjacent to densely cellular or collagenous regions.4 In our case, the heterogeneity on the CT scan was due to cystic degeneration and such changes are very rarely seen. Angiography is indicated if the mass is contrast enhancing and if vessels appear to be compressed by the tumour. Surgical excision is the treatment of choice and should be done with careful extracapsular dissection or by intracapsular enucleation to preserve the nerve of origin.
Conclusion
SCSC, although rare, should be considered as a differential diagnosis in patients presenting with a lateral neck mass. FNAC is usually inconclusive, but radiological examination has a definite role in diagnosis. SCSC is mainly diagnosed by histopathology and the treatment of choice is surgical excision.
References
- 1.Malone JP, Lee WJ, Levin RJ. Clinical characteristics and treatment outcome for nonvestibular schwannomas of the head and neck. Am J Otolaryngol. 2005;26:108–112. doi: 10.1016/j.amjoto.2004.08.011. [DOI] [PubMed] [Google Scholar]
- 2.Sedat A, Arif S, Omer T, Aylin GE. Horner’s syndrome post excision of a huge cervical sympathetic chain schwannoma. Turk J Med Sci. 2007;37:185–190. [Google Scholar]
- 3.Bocciolini C, Dall’olio D, Cavazza S, Laudadio P. Schwannoma of cervical sympathetic chain: Assessment and management. Acta Otorhinolaryngol Ital. 2005;25:191–4. [PMC free article] [PubMed] [Google Scholar]
- 4.Anil G, Tan TY. Imaging characteristics of schwannoma of the cervical sympathetic chain: A review of 12 cases. Am J Neuroradiol. 2010;31:1408–12. doi: 10.3174/ajnr.A2212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ganesan S, Harar RPS, Owen RA, Dawkins RS, Prior AJ. Horner’s syndrome: A rare presentation of cervical sympathetic chain schwannoma. J Laryngol Otol. 1997;111:493–5. doi: 10.1017/s0022215100137740. [DOI] [PubMed] [Google Scholar]
- 6.Colreavy MP, Lacy PD, Hughes J, Bouchier-Hayes D, Brennan P, O’Dwyer AJ, et al. Head and neck schwannomas – a 10-year review. J Laryngol Otol. 2000;114:119–24. doi: 10.1258/0022215001905058. [DOI] [PubMed] [Google Scholar]
- 7.Yoo H, Jung H-W, Yang HJ. Jugular foramen schwannomas: Surgical approaches and outcome of treatment. Skull Base Surg. 1999;9:243–52. doi: 10.1055/s-2008-1058133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wanamaker JF, Wanamaker HH, Kotton B, Akers GD, Lavertu P, et al. Schwannomas of the nose and paranasal sinuses. Am J Rhinol. 1993;7:59–65. [Google Scholar]
- 9.Rosner M, Fisher W, Malligan L. Cervical sympathetic schwannoma: Case report. Neurosurgery. 2001;49:1452–4. doi: 10.1097/00006123-200112000-00027. [DOI] [PubMed] [Google Scholar]
- 10.Mikaelian DO, Holmes WF, Simonian SK. Parapharyngeal schwannomas. Otolaryngol Head Neck Surg. 1981;89:77–81. doi: 10.1177/019459988108900117. [DOI] [PubMed] [Google Scholar]
- 11.Furukawa M, Furukawa MK, Katoh K, Tsukuda M. Differentiation between schwannoma of vagus nerve and cervical sympathetic chain by imaging diagnosis. Laryngoscope. 1996;106:1548–52. doi: 10.1097/00005537-199612000-00021. [DOI] [PubMed] [Google Scholar]