Abstract
Malignant tumors of minor salivary glands are uncommon, representing only 2–4% of all head and neck malignancies. In the larynx, minor salivary gland tumors rarely occur and constitute less than 1% of laryngeal tumors. Most of the minor salivary gland tumors arise in the subglottis; however, they can also occur in the supraglottis in the false vocal cords, aryepiglottic folds, and caudal aspect of the epiglottis. The most common type of malignant minor salivary gland tumor is adenoid cystic carcinoma. In the last 20 years, only 40 cases of adenoid cystic carcinoma arising in variable locations of the larynx have been reported in the English language literature. We present a case of adenoid cystic carcinoma of the larynx arising in the inter-arytenoid and postcricoid region in a 54-year-old woman. To our knowledge, this is the first case of adenoid cystic carcinoma arising in this particular region of the larynx.
Keywords: Adenoid cystic carcinoma, Larynx, Minor salivary gland tumors
Introduction
Malignant tumors of minor salivary glands are uncommon, representing only 2–4% of all head and neck malignancies [1]. Minor salivary gland tumors most commonly arise in the oral cavity, particularly the hard palate, and less commonly in the nasal cavity, paranasal sinuses, pharynx, and larynx [2] owing to the distribution of minor salivary glands in these regions. In the larynx, minor salivary gland tumors rarely occur and constitute less than 1% of laryngeal tumors. They arise from submucosal minor salivary glands, which have a distinct anatomical distribution in the larynx [3]. The majority of these glands are concentrated in the subglottis but are also found in the supraglottis in the false vocal cords, aryepiglottic folds, and caudal aspect of the epiglottis [2]. The most common type of malignant minor salivary gland tumors is adenoid cystic carcinoma (AdCC) [2, 4]. In the last 20 years, only 40 cases of AdCC in variable locations of the larynx have been reported in the English language literature. To our knowledge, this is the first case of AdCC of the larynx arising in the inter-arytenoid, postcricoid region.
Case Presentation
A 54-year-old woman presented to the Department of Otolaryngology-Head and Neck Surgery at Uludag University School of Medicine complaining of difficulty swallowing solid foods over the past 4 months. Indirect laryngoscopy and office endoscopy revealed a submucosal bulging mass in the inter-arytenoid area that measured 3 × 3 × 2.5 cm. The mobility of the true vocal folds was restricted but there was no evidence of airway obstruction. No palpable lymph nodes were present in the neck.
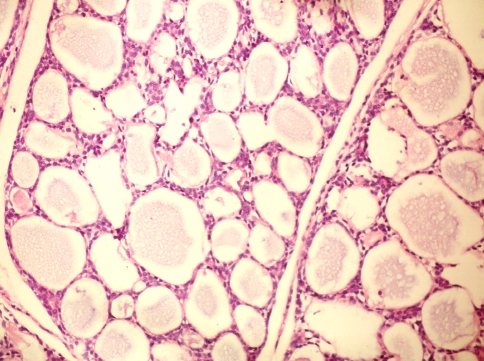
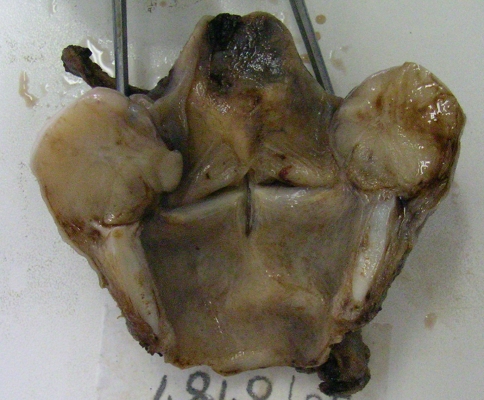
Biopsy of this mass revealed a cellular neoplasm characterized by a prominent cribriform architecture and comprised of small, bland hyperchromatic cells with high nuclear-to-cytoplasmic ratio and carrot- or peg-shaped nuclei with inconsipicous nucleoli (Fig. 3). These cells surrounded pseudoglandular spaces filled with basement membrane-like material and mucin. Scattered small true glandular lumina were also present, but perineural invasion was not identified. A diagnosis of AdCC was made and the patient subsequently underwent total laryngectomy (Figs. 1, 2) with bilateral selective neck dissections (levels 2–4). Histologic sections of the resected specimen showed similar histology, as well as perineural invasion. All the dissected neck lymph nodes were free of metastases. The patient did not receive any post-operative adjuvant therapy.
Fig. 3.
Microscopic appearance of AdCC shows classic cribriform architecture and small, bland hyperchromatic cells forming pseudoglandular spaces filled with a mucinous, pink to pale purple basement membrane-like material. Occasional small true glandular spaces are also seen. Perineural invasion (not shown) was identified only in the resected specimen
Fig. 1.
Macroscopic appearance of the tumor in the inter-arytenoid, postcricoid area. Note the large glistening, submucosal mass bulging into the laryngeal space and causing mass effect in the hypopharynx, which explains the patient’s history of dysphagia
Fig. 2.
Bisection reveals a tan-white glistening cut surface with minute focal hemorrhage (greater on the right)
Dıscussion
The most common malignancy of the larynx and hypopharynx is squamous cell carcinoma. Less commonly, other epithelial, neuroendocrine, and soft tissue tumors can also occur in these locations [5]. Minor salivary gland tumors of the larynx are rare [2, 4, 6–8]. These tumors are predominantly subglottic, in keeping with their origin from submucosal glands, which are more frequently found in this region of the larynx [2].
Minor salivary gland tumors are usually malignant and the most common type is AdCC [2, 4]. AdCC of the larynx more commonly occurs in middle-aged or older patients [10]. No significant difference exists in terms of the frequency between male and female patients [9]. Symptoms depend on the tumor’s location. For example, a subglottic lesion may result in dyspnea (due to airway obstruction) and a glottic or supraglottic lesion may cause hoarseness (due to vocal cord compromise). In cases of AdCC, neck pain is a characteristic symptom due to perineural invasion [9].
AdCC of the larynx appears to behave in a similar fashion to AdCC of other head and neck sites. It is a slowly growing but highly invasive cancer with a high recurrence rate. Hematogenous spread occurs often in the course of the disease [11, 12]. The prognostic factors of AdCC depend on tumor site, tumor stage, and microscopic tumor pattern. Tubular and cribriform subtypes have a better prognosis than solid subtypes [13, 14]. in our case, microscopic examination revealed the classic cribriform pattern, which is considered low-grade (Grade I/III). Moreover, the patient presented in clinical stage II (T2, N0, M0) due to tumor extension to the vocal cords with impaired mobility (T2), negative lymph nodes (N0), and no evidence of distant metastases (M0).
Surgical excision is recommended owing to the relative radioresistance of these tumors. Because of the propensity for submucosal spread, plus perineural and lymphovascular invasion, total laryngectomy is often required. Notably, in AdCC, regional recurrence is rare, but distant metastasis is common [2].
Postoperative radiation is advocated by some, since radiotherapy has been shown to result in tumor regression and symptomatic relief [15]. The use of chemotherapy in AdCC is controversial. Some investigators have reported positive responses to chemotherapy and recommended it as palliative therapy in advanced cases [16].
Previous case reports of AdCC in the larynx are listed in the table [2, 4, 6, 9, 17–22]. Of these cases, none is described as arising in the exact location as our patient’s tumor. Therefore, to our knowledge, this is the first case of AdCC arising in the inter-arytenoid, postcricoid region ever reported in the English language literature. After 4 years of post-operative follow-up, our patient remains free of loco-regional recurrence and/or distant metastases (Table 1).
Table 1.
Previous case reports of AdCC arising in the larynx reported in the English language literature over the last 20 years
| Author(s) | Case(s) | Year(s) |
|---|---|---|
| Maukarbel RV et al. | 15 | 1963–2007 |
| Del Negro A et al. | 1 | 2007 |
| Khan AR et al. | 1 | 2006 |
| Ganly I et al. | 12 | 1970–2003 |
| Lee LA et al. | 1 | 2003 |
| Mahlstedt K et al. | 6 | 2002 |
| Javadi M et al. | 1 | 2002 |
| Altaf FJ | 1 | 2001 |
| Hogg RP et al. | 1 | 1999 |
| de Kerviler E et al. | 1 | 1995 |
Contributor Information
Ozlem Saraydaroglu, Phone: +90-224-2953687, Email: osaraydaroglu@uludag.edu.tr.
Hakan Coskun, Email: hcoskun@uludag.edu.tr.
Mehtap Kasap, Email: kasapmehtap@hotmail.com.
References
- 1.Sadeghi A, Tran LM, Mark R, et al. Minor salivary gland tumors of the head and neck: treatment strategies and prognosis. Am J Clin Oncol. 1993;16(1):3–8. doi: 10.1097/00000421-199302000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Ganly I, Patel SG, Coleman M, et al. Malignant minor salivary gland tumors of the larynx. Arch Otolaryngol Head Neck Surg. 2006;132(7):767–770. doi: 10.1001/archotol.132.7.767. [DOI] [PubMed] [Google Scholar]
- 3.Bak-Pedersen K, Nielsen KO. Subepithelial mucous glands in the adult human larynx. Studies on number, distribution and density. Acta Otolaryngol. 1986;102(3–4):341–352. doi: 10.3109/00016488609108685. [DOI] [PubMed] [Google Scholar]
- 4.Mahlstedt K, Ussmüller J, Donath K. Malignant sialogenic tumours of the larynx. J Laryngol Otol. 2002;116(2):119–122. doi: 10.1258/0022215021910078. [DOI] [PubMed] [Google Scholar]
- 5.Barnes L, Eveson JW, Reichart P, et al. World health organization classification of tumours. Pathology and genetics of head and neck tumours. Lyon: IARC Press; 2005. [Google Scholar]
- 6.Messaoudi C, Larouk R, Baili S, et al. Adenoid cystic carcinoma of the larynx. A case report and review of the literature. Rev Laryngol Otol Rhinol. 2007;128(1–2):97–100. [PubMed] [Google Scholar]
- 7.Khan AR, Jan A, Nawaz G, et al. Adenoid cystic carcinoma of larynx. J Coll Physicians Surg Pak. 2006;16(10):669–670. doi: 10.2006/JCPSP.669670. [DOI] [PubMed] [Google Scholar]
- 8.Kufeld M, Junker K, Sudhoff H, et al. Collision tumor of a hypopharyngeal adenoidcystic carcinoma and a laryngeal squamous cell carcinoma. Laryngorhinootologie. 2004;83(1):51–54. doi: 10.1055/s-2004-814109. [DOI] [PubMed] [Google Scholar]
- 9.Lee LA, Fang TJ, Li HY, et al. Adenoid cystic carcinoma of the supraglottis mimicking a laryngeal cyst. Otolaryngol Head Neck Surg. 2003;129(1):157–158. doi: 10.1016/S0194-5998(03)00490-X. [DOI] [PubMed] [Google Scholar]
- 10.Tewfik TL, Novick WH, Schipper HM. Adenoid cystic carcinoma of the larynx. J Otolaryngol. 1983;12(3):151–154. [PubMed] [Google Scholar]
- 11.Abdul-Hussein A, Morris PA, Markova T. An unusual presentation of adenoid cystic carcinoma of the minor salivary glands with cranial nerve palsy: a case study. BMC Cancer. 2007;13(7):157. doi: 10.1186/1471-2407-7-157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huang M, Ma D, Sun K, et al. Factors influencing survival rate in adenoid cystic carcinoma of the salivary glands. Int J Oral Maxillofac Surg. 1997;26(6):435–439. doi: 10.1016/S0901-5027(97)80008-2. [DOI] [PubMed] [Google Scholar]
- 13.Norberg-Spaak L, Dardick I, Ledin T. Adenoid cystic carcinoma: use of cell proliferation, BCL-2 expression, histologic grade, and clinical stage as predictors of clinical outcome. Head Neck. 2000;22(5):489–497. doi: 10.1002/1097-0347(200008)22:5<489::AID-HED8>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 14.Khan AJ, DiGiovanna MP, Ross DA, et al. Adenoid cystic carcinoma: a retrospective clinical review. Int J Cancer. 2001;96(3):149–158. doi: 10.1002/ijc.1013. [DOI] [PubMed] [Google Scholar]
- 15.Kokemueller H, Eckardt A, Brachvogel P, et al. Adenoid cystic carcinoma of the head and neck—a 20 years experience. Int J Oral Maxillofac Surg. 2004;33(1):25–31. doi: 10.1054/ijom.2003.0448. [DOI] [PubMed] [Google Scholar]
- 16.Hill ME, Constenla DO, A’Hern RP, et al. Cisplatin and 5-fluorouracil for symptom control in advanced salivary adenoid cystic carcinoma. Oral Oncol. 1997;33(4):275–278. doi: 10.1016/S0964-1955(97)00026-2. [DOI] [PubMed] [Google Scholar]
- 17.Moukarbel RV, Goldstein DP, O’Sullivan B, et al. Adenoid cystic carcinoma of the larynx: a 40-year experience. Head Neck. 2008;30(7):919–924. doi: 10.1002/hed.20802. [DOI] [PubMed] [Google Scholar]
- 18.Del Negro A, Ichihara E, Tincani AJ, et al. Laryngeal adenoid cystic carcinoma: case report. Sao Paulo Med J. 2007;125(5):295–296. doi: 10.1590/S1516-31802007000500010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Javadi M, Bafrouee FM, Mohseni M, et al. Laryngeal adenoid cystic carcinoma in a child: a case report. Ear Nose Throat J. 2002;81(1):34–35. [PubMed] [Google Scholar]
- 20.Altaf FJ. Histopathology of adenoid cystic carcinoma of the larynx and adenocarcinoma hybrid. Saudi Med J. 2001;22(10):920–923. [PubMed] [Google Scholar]
- 21.Hogg RP, Kuo MJ, Olliff J, et al. Invasion of the recurrent laryngeal nerve by adenoid cystic carcinoma. An unusual cause of true vocal fold paralysis. J Laryngol Otol. 1999;113(3):260–262. doi: 10.1017/S0022215100143737. [DOI] [PubMed] [Google Scholar]
- 22.Kerviler E, Bely N, Laccourreye O, et al. The aryepiglottic fold as a rare location of adenoid cystic carcinoma. AJNR Am J Neuroradiol. 1995;16(6):1375–1377. [PMC free article] [PubMed] [Google Scholar]