Abstract
We report an unusual presentation of primary biliary cirrhosis. We present the case of a 31-year-old Indian woman who presented to the hospital with non specific complaints of gastritis, reduced appetite and marked weight loss and no complaints of pruritus. Serum liver enzymes were elevated. Cytoplasmic pattern of antinuclear antibodies was found on immunofluorescence microscopy accompanied by positive anti smooth muscle antibody. Endoscopy revealed esophageal varices. Following a liver biopsy, the diagnosis of primary biliary cirrhosis was made. It is important to consider the diagnosis of hepatic cirrhosis when patient presents with gastritis, reduced appetite and marked weight loss in both the presence and absence of ascites.
Keywords: PBC, Primary biliary cirrhosis, Pruritus, ANA, ASMA, AMA
Introduction
Patients with primary biliary cirrhosis (PBC) suffer irritation and swelling of the bile ducts of the liver, blocking the flow of bile, which normally aids digestion. The obstruction damages liver cells and leads to scarring, known as cirrhosis. The specific biological pathways underlying primary biliary cirrhosis are poorly understood. As there are no proven treatments available, the majority of patients require a liver transplant. Clinical awareness of PBC among clinicians and laboratory doctors is essential for early diagnosis and early initiation of treatment. Effective medical therapy with ursodeoxycholic acid, especially begun early in the course of the disease can slow disease progression and extend survival, free of liver transplant in patients who respond to therapy.
Case Report
A 31-year-old woman presented to our hospital for evaluation of gastritis, reduced appetite and marked weight loss. A complete physical examination of systems yielded no relevant findings. The patient’s medical history was unremarkable except for intermittent headache for which she took analgesics. She had no history of liver disease or risk factors for chronic liver disease (blood transfusions, intravenous drug use, high-risk sexual behavior, or current or past alcohol use or smoking history). Two family members from her maternal side had surgery for gallstones.
Physical examination revealed a thin female, 35 kg weight, in no distress. Slight scleral icterus, was observed. The patient’s abdomen was nondistended and nontender; a fluid wave test showed no ascites. The patient’s liver was palpable 2 cm below the right costal margin. Findings on the remainder of her examination were unremarkable.
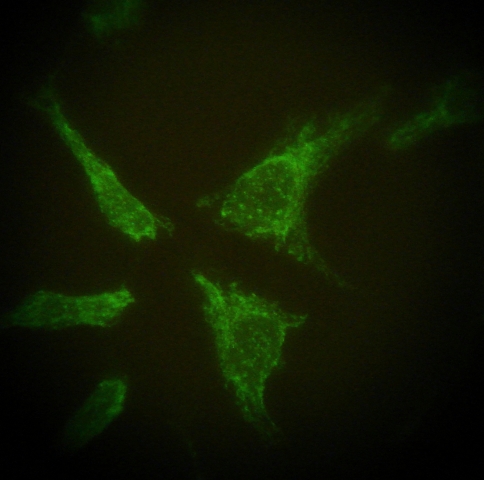
Laboratory tests yielded the following results (reference ranges provided parenthetically): complete blood cell count, within normal limits except for hemoglobin 11.2 g/dl (13–17 g/dl), total red blood cell count 3.90 million/cu mm (4.5–5.5 million/cumm) and ESR 123 mm 1st hour (5–15 mm 1st hour). PT INR was within reference range. Fasting plasma glucose 81 mg/dl (70–110 mg/dl); alkaline phosphatase, 632U/l (30–279 U/l); aspartate aminotransferase, 67 U/l (0–35 U/l); alanine aminotransferase, 51 U/l (0–35 U/l); total bilirubin 2.1 mg/dl (0.1–1.0 mg/dl); albumin, 2.9 g/dl (3.5–5.0 g/dl) Gamma glutamyltransferase 139 U/l (1–94 U/l); total cholesterol 224 mg/dl (<200 mg/dl); triglycerides 155 mg/dl (<150 mg/dl); high-density lipoprotein cholesterol, 62 mg/dl (>60 mg/dl); low-density lipoprotein cholesterol, 141 mg/dl (<100 mg/dl); urea,creatinine and electrolytes were within reference range; serum calcium was 7.2 mg/dl (8.5–10.1 mg/dl); thyroid stimulating hormone, 0.1 mIU/l (0.3–5.0 mIU/l); and free thyroxine, 1.2 ng/dl (0.8–1.8 ng/dl). Serum α 1 antitrypsin level was 144.2 mg/dl (90–200 mg/dl). Cerruloplasmin levels were 62.8 mg/dl (15–60 mg/dl), copper in 24 h urine 57.6 μg/24 h (15–70 μg/24 h) and Kayser-Fleischer ring was not seen on slit lamp examination. Immunoglobulin G level was 1,584 mg/dl (700–1,600 mg/dl.) Serology for HCV, HbsAg, HIV were non reactive. In immunofluorescence microscopy, anti neutrophil cytoplasmic antibody was negative, Antimitochondrial antibodies were absent, cytoplasmic pattern of anti nuclear antibody was found in 1:80 titre and anti smooth muscle antibody positive in 1:20 titre (Fig. 1) autoimmune hepatitis panel for liver kidney microsomal antigen, cytosolic antigen type 1, soluble liver antigen were all negative. The titer of anti mitochondrial M2 (Pyruvate dehydrogenase complex) antibody was elevated. Radiological investigations revealed a normal ultrasound report of the whole abdomen ruling out biliary obstruction and portal vein thrombosis. Chest X-ray was also normal. Gastroduodenoscopy revealed early varices at lower end of esophagus (grade II).
Fig. 1.
Mitochondrial pattern ( HEp-2 cell line)
Liver biopsy was done to know the etiology. Microscopic study of biopsy material from liver revealed ill-defined granulomas centred on the bile ducts. Portal tracts were seen with dense inflammation by histiocytes, lymphocytes and plasma cells. No evidence of fibrosis was present. In correlation with clinical and other laboratory findings, the features were consistent with primary biliary cirrhosis.
The patient was treated symptomatically and ursodeoxycholic acid was started as treatment and the patient discharged. At 6 months follow-up, her liver enzymes has fallen alkaline phosphatase 181U/l. (30–279 U/l); aspartate aminotransferase, 27 U/l (0–35 U/l); alanine aminotransferase, 24 U/l (0–35 U/l); total bilirubin 1.1 mg/dl (0.1–1.0 mg/dl); albumin, 3.1 g/dl (3.5–5.0 g/dl).
Discussion
Primary biliary cirrhosis is a chronic cholestatic liver disease of presumed autoimmune etiology that affects predominantly middle-aged women. In the United States, approximately 3,500 new cases of PBC are diagnosed each year, with 47,000 prevalent cases among the white population [1]. The rarity of PBC in India is intriguing with only a few cases being reported from the subcontinent [2]. The low intensity of screening for anti mitochondrial antibody (AMA) and serum gamma globulins in patients with abnormal liver function may be responsible for the low prevalence of PBC reported from the developing countries [2].
Concordance rates in monozygotic twins, familial prevalence, and genetic associations underscore the importance of genetic factors, whereas findings of epidemiological studies and murine models suggest a possible role for exogenous chemicals and infectious agents through molecular mimicry. The incidence of primary biliary cirrhosis has increased over recent decades, possibly attributable to augmented testing of liver biochemistry rather than a rise in disease incidence [3].
Primary biliary cirrhosis (PBC) is an organ-specific autoimmune disease characterized by chronic, progressive destruction of small intrahepatic bile duct with portal inflammation and ultimately fibrosis. Current theories on the pathogenesis of PBC have favored the hypothesis that T lymphocytes played a pivotal role in the autoimmune response in PBC The liver-infiltrating T cells in PBC might be responsible for damaging the liver and causing chronic liver disease [4].
Antinuclear antibodies (ANA), the most common autoantibodies assessed, are nonspecific serologic markers of autoimmunity in acute and chronic liver disease. These antibodies are found in approximately 50% of patients with PBC [5]. In our patient, the diagnosis of PBC was confirmed on the basis of laboratory findings like predominant elevation of serum alkaline phosphatase, relative to aminotransferase suggesting bile flow impairment, positive anti mitochondrial antibody and histopathological findings compatible with PBC on liver biopsy. The best screening tool for PBC is an assay for AMAs, which are characteristic of PBC and are present in at least 95% of cases [5]. The combination of antimitochondrial antibodies on immunofluorescence (or anti-M2 antibodies on an enzyme-linked immunosorbent assay) and cholestatic liver function tests is 95% sensitive and specific for the diagnosis of PBC [6].
Lipoprotein X, an atypical lipoprotein found in PBC, can account for a major fraction of the total serum cholesterol [7]. It interferes with routine lipid panel measurements, falsely increasing the laboratory measurement of direct and calculated LDL Cholesterol and HDL.
PBC has been reported to frequently accompany various autoimmune diseases, including a report of ulcerative colitis, diagnosed by colonoscopy. The patient received mesalazine, following which his symptoms improved [8].
Our case report highlights the importance for clinicians to consider the differential diagnosis of PBC in young females who present with apparently innocuous symptoms of gastritis and marked weight loss. Early diagnosis and effective medical therapy begun early in the course of the disease can slow disease progression and extend survival, free of liver transplant in patients who respond to therapy.
References
- 1.Silveria MG, Lindor KD. 38-year-old woman with abnormal liver enzymes and hyperlipidemia. Mayo Clin Proc. June 2009;84(6):551–554. [DOI] [PMC free article] [PubMed]
- 2.Sarin SK, Monga R, Sandhu BS, Sharma BC, Sakhuja P, Malhotra V. Primary biliary cirrhosis in India. Hepatobiliary Pancreat Dis Int. 2006;5(1):105–109. [PubMed] [Google Scholar]
- 3.Selmi C, Bowlus CL, Gershwin ME, Coppel RL. Primary biliary cirrhosis. The Lancet. 2011;377(9777):1600–1609. [DOI] [PubMed]
- 4.Wen Z, Yunyun F, Jinming G, Bin L, Fengchun Z. The Role of CXCR3 in the induction of primary biliary cirrhosis. Clin Dev Immunol. 2011;2011:Article ID 564062, doi:10.1155/2011/564062. [DOI] [PMC free article] [PubMed]
- 5.Kaplan MM, Gershwin ME. Primary biliary cirrhosis [published correction appears in N Engl J Med. 2006;354(3):313]. N Engl J Med. 2005;353(12):1261–1273. [DOI] [PubMed]
- 6.Hirschfield GM, Liu X, Han Y, Gorlov IP, Lu Y, Xu C, et al. The Genetics of primary biliary cirrhosis: The revolution moves on;variants at IRF5-TNPO3, 17q12-21 and MMEL1are associated with primary biliary cirrhosis. Nat Genet. 2010;42:655–657. reprinted in Hepatology 2011;53(1):362–364. [DOI] [PMC free article] [PubMed]
- 7.Siedel D, Alaupovic P, Furman RH. A lipoprotein characterizing obstructive jaundice, I: method for quantitative separation and identification of lipoproteins in jaundiced subjects. J Clin Invest. 1969;48(7):1211–1223. doi: 10.1172/JCI106085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arai O, Ikeda H, Mouri H, Notohara K, Matsueda K. Two cases of inflammatory bowel disease diagnosed in the course of primary biliary cirrhosis. Nippon Shokakibyo Gakkai Zasshi. 2010;107(6):900–908. [PubMed] [Google Scholar]