Abstract
Background
Postoperative varus alignment has been associated with lower IKS scores and increased failure rates. Appropriate positioning of TKA components therefore is a key concern of surgeons. However, obtaining neutral alignment can be challenging in patients with substantial preoperative varus deformity and it is unclear whether residual deformity influences revision rates.
Questions/purposes
We asked: (1) in patients with preoperative varus deformities, does residual postoperative varus limb alignment lead to increased revision rates or lower IKS scores compared with correction to neutral alignment, (2) does placing the tibial component in varus alignment lead to increased revision rates and lower IKS scores, (3) does femoral component alignment affect revision rates and IKS scores, and (4) do these findings change in patients with at least 10° varus alignment preoperatively?
Patients and Methods
From a prospective database, we identified 553 patients undergoing TKAs for varus osteoarthritis. Patients were divided into those with residual postoperative varus and those with neutral postoperative alignment. Revision rates and International Knee Society (IKS) scores were compared between the two groups and assessed based on postoperative component alignment. Survival analysis was conducted with revision as the endpoint. The analysis was repeated in a subgroup of patients with at least 10° preoperative varus. Minimum followup was 2 years (median, 4.7 years; range, 2–19.8 years).
Results
The two groups had similar survival rates to 10 years and similar IKS scores. Varus tibial component alignment and valgus femoral component alignment were associated with lower mean scores. Revision rates and scores were similar in a subgroup of patients with substantial preoperative varus.
Conclusions
Our data suggest residual postoperative varus deformity after TKA does not increase survival rates at medium-term in patients with preoperative varus deformities, providing tibial component varus is avoided. Tibial component varus negatively influences IKS score.
Level of Evidence
Level III, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Appropriate positioning of TKA components is a key concern of arthroplasty surgeons. Numerous authors have suggested obtaining a femorotibial mechanical axis (FTMA) of 180° in the coronal plane is ideal [8, 10, 20, 23, 27]. Deviation greater than 2° or 3° from this alignment, particularly in varus, has been associated with lower IKS scores [6, 16, 18] and increased rates of aseptic loosening and failure [1, 3, 8, 10, 12, 15, 20, 23, 27].
However, obtaining neutral alignment can be challenging in patients with substantial preoperative deformity. More complex bone cuts and/or larger soft tissue releases [28] are required in these cases, which increase operative time [24]. Some authors suggest that despite these efforts, knees with substantial preoperative varus alignment are more likely to have varus alignment postoperatively [9, 15]. Additionally, some recent studies have cast doubt on the long-held belief that neutral alignment yields lower revision rates in all patients [21, 22].
The cited studies reporting increased revision rates and lower IKS scores in knees with postoperative varus alignment do not stratify their findings based on preoperative alignment. It is possible the ideal postoperative coronal plane alignment is determined in part by the extent and type of preoperative deformity and is not the same for every patient. Further, individual component alignment may influence revision rates and IKS scores, with tibial component alignment being particularly important.
We therefore addressed the following questions: (1) in patients with preoperative varus deformities, does residual postoperative varus limb alignment lead to increased revision rates or lower IKS scores compared with correction to neutral alignment? (2) Does placing the tibial component in varus alignment lead to increased revision rates and lower IKS scores? (3) Does femoral component alignment affect revision rates and IKS scores? (4) Do these findings change in patients with at least 10° varus alignment preoperatively?
Patients and Methods
We retrospectively reviewed 511 patients with primary varus tibiofemoral osteoarthritis (FTMA < 177°) treated with 553 TKAs between November 1987 and January 2008. During that time we treated a total of 1798 patients with 2216 primary TKAs. We excluded 1190 patients with neutral or valgus preoperative alignment, a history of surgery on the index knee other than meniscectomy, arthritis from other etiologies (posttraumatic, rheumatoid, or inflammatory arthritis), malignancies, or postoperative flexion contracture greater than 5°. Flexion contracture decreases the accuracy of measuring coronal plane limb alignment [5, 17]. These exclusions left 608 patients (703 TKAs). Radiographic and clinical followups of at least 2 years were available for 553 knees (79%). These knees form the study group. The minimum followup was 2 years (median, 4.7 years; range, 2–19.8 years).
Mean (± SD) preoperative FTMA was 170.2° ± 4.4° (range, 151°–176°). Mean preoperative tibial mechanical angle (TMA) was 84.7° ± 3.7° (range, 69°–100°). Mean preoperative femoral mechanical angle (FMA) was 90.2° ± 2.7° (range, 77°–99°). Postoperatively, 181 patients (33%) remained in varus alignment and 352 patients (64%) had correction to within 3° of neutral alignment. Twenty patients (4%) were placed in valgus alignment and not included in data analysis. The age and gender distributions of patients in the residual varus and neutral alignment groups were not different, but the residual varus group had a higher mean body mass index (BMI), increased preoperative varus, and lower preoperative IKS scores (Table 1).
Table 1.
Preoperative demographic data for all patients by postoperative alignment
| Variable | Residual varus | Neutral alignment | Significance |
|---|---|---|---|
| Gender (males:females) | 53:128 | 113:223 | p = 0.36 |
| Age (years) | 71.9 ± 7.8 | 71.3 ± 7.0 | p = 0.40 |
| BMI (kg/m2) | 30.9 ± 5.8 | 29.2 ± 4.9 | p = 0.0004 |
| Preoperative FTMA (°) | 167.4 ± 4.9 | 171.5 ± 3.4 | p < 0.0001 |
| Preoperative TMA (°) | 83.8 ± 3.7 | 85.3 ± 3.6 | p < 0.0001 |
| Preoperative FMA (°) | 89.2 ± 2.8 | 90.6 ± 2.5 | p < 0.0001 |
| Preoperative IKS score (points) | 90.2 ± 31.6 | 104.0 ± 30.4 | p < 0.0001 |
Values are expressed as mean ± SD; BMI = body mass index; FTMA = femorotibial mechanical axis; FMA = femoral mechanical angle; TMA = tibial mechanical angle; IKS = International Knee Society.
A subgroup of 266 patients (48%) had at least 10° varus preoperatively. Mean preoperative FTMA in this group was 166.5° ± 3.6° (range, 151°–170°). Mean preoperative TMA was 83.2° ± 4.1° (range, 69°–100°) and mean preoperative FMA was 89.5° ± 2.6° (range, 79°–99°) among these patients. Postoperatively, 131 patients (49%) remained in varus alignment and 131 patients (49%) had correction to neutral alignment. Four patients (2%) were placed in valgus alignment and are not included in the data analysis. In this subgroup, the age and gender distributions of the residual varus and neutral alignment groups were not different, but the residual varus group had a higher mean BMI, increased preoperative varus, and lower preoperative IKS scores (Table 2).
Table 2.
Preoperative demographic data for patients with at least 10° preoperative varus by postoperative alignment
| Variable | Residual varus | Neutral alignment | Significance |
|---|---|---|---|
| Gender (males:females) | 41:90 | 52:79 | p = 0.20 |
| Age (years) | 72.2 ± 7.5 | 72.8 ± 6.3 | p = 0.51 |
| BMI (kg/m2) | 31.0 ± 5.9 | 28.8 ± 5.2 | p = 0.0019 |
| Preoperative FTMA (°) | 165.2 ± 3.9 | 167.8 ± 2.4 | p < 0.0001 |
| Preoperative TMA (°) | 82.8 ± 3.6 | 83.8 ± 4.2 | p = 0.058 |
| Preoperative FMA (°) | 88.9 ± 2.8 | 90.0 ± 2.2 | p = 0.0009 |
| Preoperative IKS score (points) | 86.6 ± 30.9 | 96.9 ± 29.5 | p = 0.0064 |
Values are expressed as mean ± SD; BMI = body mass index; FTMA = femorotibial mechanical axis; FMA = femoral mechanical angle; TMA = tibial mechanical angle; IKS = International Knee Society.
Exposure was obtained through a standard medial parapatellar approach in all cases. The tibial cut was made perpendicular to the tibial mechanical axis using an extramedullary guide. The distal femoral cut was made using an intramedullary guide. The cut was made in 7° valgus (8° for HLS2® prostheses [Tornier, St. Ismier, France]) relative to the anatomic axis of the femur. Components were cemented in all cases and the patella was resurfaced. Posterior-stabilized components were used in all cases. The implants included seven HLS1®, 50 HLS2®, 151 HLS Evolution®, and 345 Noetos HLS® (Tornier).
Patients began a supervised postoperative rehabilitation regimen on postoperative Day 1. Immediate weightbearing was allowed in all patients with a brace locked in extension and a walker for support. Patients progressed to ambulation without a brace or walker at the discretion of the therapist. The brace was removed and full range of motion was allowed when patients were not ambulating. No continuous passive motion devices were used.
Preoperatively and at each followup, any subsequent surgical procedures on the index knee were documented. Postoperative visits were scheduled at 2, 6, and 12 months postoperatively, and then at 2-year intervals. Physical examination included evaluation of knee ROM, stability to varus and valgus stress, and wound healing, and the IKS knee and function scores were calculated [11]. We grouped perioperative complications as major (those threatening life or requiring reoperation) and minor (those resolving with antibiotics, anticoagulation, or without specific treatment) as described previously [4, 25].
Radiographic assessment was performed on all patients preoperatively and postoperatively at each followup until maximum followup. Radiographs included standing AP and lateral views of the operative knee, a 30° axial patellar view, and standing full-leg films. As part of the prospective data collection for our arthroplasty database, the FTMA, TMA, and FMA were measured manually by various clinicians on full-leg films using a goniometer. The TMA refers to the alignment of the tibial articular surface preoperatively and tibial component postoperatively relative to the mechanical axis of the tibia. The FMA refers to alignment of the femoral articular surface preoperatively and femoral component postoperatively relative to the mechanical axis of the femur. Intraclass coefficients (ICC) for interrater reliability of this method of assessing mechanical axis are reportedly between 0.88 to 0.94 [19].
Patients were divided into three groups based on postoperative FTMA: residual varus (postoperative FTMA < 177°), neutral alignment (postoperative FTMA between 177° and 183°), and overcorrection (postoperative FTMA > 183°). A power analysis determined a minimum sample size of 87 patients in each group was required to identify a difference of 10 points in the IKS score between the residual varus and neutral alignment groups with α = 0.05 and a statistical power of 80%. Revision rate and IKS scores in patients not having revision were compared between the residual varus group and the neutral alignment group. Revision rates and IKS scores also were compared based on alignment of the tibial component relative to the mechanical axis of the tibia: varus alignment (TMA < 87°), neutral alignment (TMA between 87° and 93°), and valgus alignment (TMA > 93°). The same analysis was performed based on alignment of the femoral component relative to the mechanical axis of the femur: varus alignment (FMA < 87°), neutral alignment (FMA between 87° and 93°), and valgus alignment (FMA > 93°). Finally, the analysis described above was repeated on a subgroup of patients with preoperative genu varum of at least 10° (FTMA < 171°). Comparison of revision rates was performed using Kaplan-Meier survival analysis using revision as an endpoint [14]. We compared IKS scores based on overall limb alignment, tibial component alignment, and femoral component alignment using ANOVA and post hoc testing with the Bonferroni-Dunn method. A power analysis determined that a minimum sample size of 87 patients in each group was required to identify a clinically significant difference of 10 points in the IKS score between the residual varus and neutral alignment groups with α = 0.05 and a statistical power of 80%.
Results
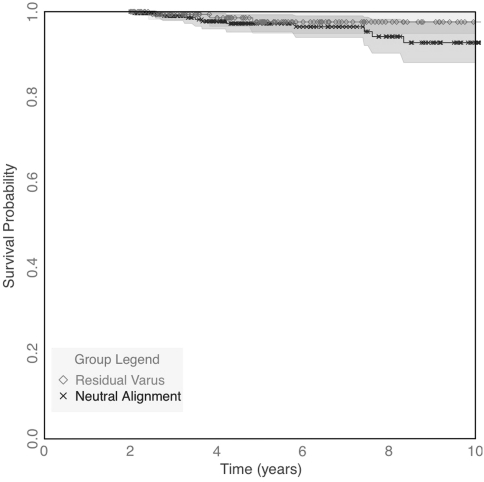
Revision was performed in a similar percentage of patients (p = 0.15) with residual varus alignment and neutral alignment: three of 181 knees (1.6%) and 13 of 352 knees (3.7%), respectively (Fig. 1). We noted no differences between the groups regarding the reason for the revisions (Table 3). Among the 537 implants still in place, the mean IKS score improved from 99.7 ± 31.8 preoperatively to 170.0 ± 27.3 at final followup. The mean IKS scores were similar (p = 0.12) in patients with residual varus (172.5) and those with neutral alignment (168.5).
Fig. 1.
A Kaplan-Meier survival curve with revision as an endpoint shows the influence of postoperative limb alignment on implant survival rates in patients with varus osteoarthritis preoperatively. We found no difference (p = 0.8) between patients with residual varus deformity and patients with neutral postoperative alignment.
Table 3.
Etiology of revisions
| Etiology | Varus alignment | Neutral alignment | Significance |
|---|---|---|---|
| Aseptic loosening | 2 | p = 0.61 | |
| Infection | 1 | 3 | |
| Laxity | 3 | ||
| Patellar complication | 1 | 2 | |
| Other | 1 | 3 | |
| Total number of revisions | 3 | 13 |
Varus = less than 177°; neutral = 177° to 183°.
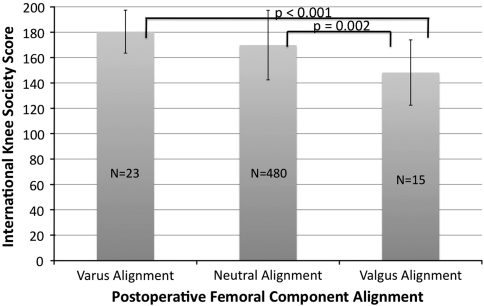
Postoperative TMA was varus in 35 knees, neutral in 514, and valgus in four. All 16 revisions occurred in the neutral TMA group. Among patients with implants still in place, mean IKS scores were different (p = 0.008) between the three groups: post hoc testing revealed lower IKS scores when the tibial component was placed in varus compared with neutral alignment (p = 0.002). The mean IKS scores were similar in patients with valgus alignment and those with either varus (p = 0.42) or neutral positions (p = 0.81) (Fig. 2).
Fig. 2.
A graph shows the influence of postoperative TMA on IKS score in patients with varus osteoarthritis preoperatively. Patients with varus alignment of the tibial component had lower (p = 0.002) mean scores compared with those with neutral alignment. We observed no differences in patients with valgus alignment and either varus or neutral component alignment. Values are shown as mean with SD (error bar).
Postoperative FMA was varus in 24 knees, neutral in 513, and valgus in 16. All 16 revisions occurred in the neutral FMA group. Among patients with implants still in place, mean IKS scores differed (p = 0.002) among the three groups. We observed lower mean IKS scores when the femoral component was placed in valgus compared with varus (p < 0.001) or neutral (p = 0.002) positions. The mean IKS scores were similar (p = 0.06) in patients with varus and neutral positions (Fig. 3).
Fig. 3.
A graph shows the influence of postoperative FMA on IKS score in patients with varus osteoarthritis preoperatively. We observed lower mean scores in patients with valgus alignment of the femoral component compared with those with varus (p < 0.001) and neutral alignment (p = 0.002). We found no differences in patients with varus and neutral component alignment. Values are shown as mean with SD (error bar).
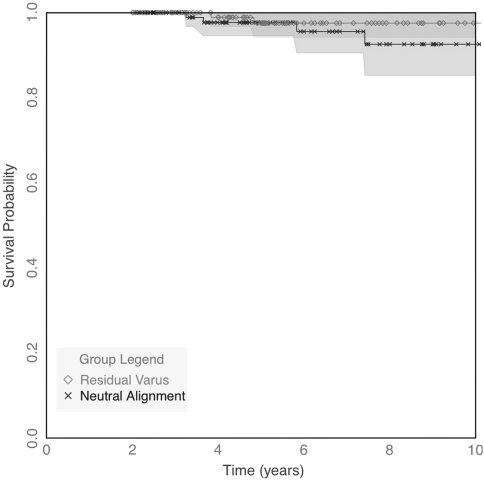
Among patients with at least 10° preoperative varus, revision was performed in a similar percentage of knees (p = 0.16) with residual varus alignment and neutral alignment: two of 131 knees (1.5%) and five of 131 knees (3.8%), respectively (Fig. 4). Among the 255 knees with implants still in place, the mean IKS score improved from 91.6 ± 30.9 preoperatively to 172.7 ± 24.6 at final followup. IKS scores were higher (p = 0.03) in patients with residual varus (176.4) than in those with neutral alignment (169.8); we had insufficient data to evaluate the effect of valgus alignment.
Fig. 4.
A Kaplan-Meier survival curve shows the influence of postoperative limb alignment on implant survival rates in patients with varus osteoarthritis and a preoperative deformity of at least 10°. We found no differences (p = 0.6) in patients with residual varus deformity and patients with neutral postoperative alignment.
For the subgroup of patients with at least 10° preoperative varus, postoperative TMA was varus in 21 knees, neutral in 244, and valgus in one. All seven revisions occurred in the neutral TMA group. Among knees with implants still in place, mean IKS scores were lower (p = 0.015) when the tibial component was placed in varus (159.8) compared with neutral alignment (173.7). Insufficient data were available to evaluate the effect of valgus positioning of the tibial component. For the subgroup of patients with at least 10° preoperative varus, postoperative FMA was varus in 24 knees, neutral in 230, and valgus in 12. All seven revisions occurred in the neutral FMA group. Among knees with implants still in place, mean IKS scores differed among the three groups: we observed lower mean IKS scores when the femoral component was placed in valgus compared with varus (p < 0.001) or neutral (p < 0.001) positions. We observed no difference (p = 0.18) in mean IKS scores in patients with varus and neutral positions (Fig. 5).
Fig. 5.
A graph shows the influence of postoperative FMA on IKS score in patients with substantial varus osteoarthritis (at least 10° varus) preoperatively. We found lower mean scores in patients with valgus alignment of the femoral component compared with those with varus (p < 0.001) and neutral alignment (p = 0.002). No differences in mean scores occurred in patients with varus or neutral component alignment. Values are shown as mean with SD (error bar).
The major complication rate was 3.6% and included one patient with septicemia, four with pulmonary emboli, two with patellar dislocations, one with an intraarticular drain requiring operative removal, two with pseudarthroses of the tibial tubercle osteotomy sites, five with infections, two with femur fractures, two with patellar clunk who underwent arthroscopic débridement, and one with algodystrophy who had manipulation for stiffness. The minor complication rate was 6.1% and included one case of patellar subluxation not requiring surgery, 12 cases of postoperative stiffness, two superficial wound infections, four hematomas, three patella fractures treated nonoperatively, and three cases of algodystrophy treated nonoperatively.
Discussion
Appropriate positioning of TKA components is a key concern of surgeons. Postoperative varus alignment has been associated with lower IKS scores and increased failure rates. However, obtaining neutral alignment can be challenging in patients with substantial preoperative varus deformity. We therefore addressed the following questions: (1) In patients with preoperative varus deformities, does residual postoperative varus limb alignment lead to increased revision rates or lower IKS scores compared with correction to neutral alignment? (2) Does placing the tibial component in varus alignment lead to increased revision rates and lower IKS scores? (3) Does femoral component alignment affect revision rates and IKS scores? (4) Do these findings change in patients with at least 10° varus alignment preoperatively?
This study has several limitations. First, and perhaps the most important was a relatively short median followup of 4.7 years. The relatively low failure rate expected after this length of followup leaves the study relatively underpowered to detect differences in failure rate based on alignment. The study is well powered to detect differences in IKS scores and we did not find lower scores with residual varus alignment. Second is the retrospective nature of the study, although data were collected prospectively as part of a joint registry at our institution. The use of such a registry results in a relatively complete data set but data collection was performed by various people, possibly leading to some inconsistency in measurement of radiographs in particular. We do not anticipate the introduction of substantial bias with this limitation. The retrospective design did not allow matching of preoperative characteristics of the two groups, resulting in increased BMI and varus deformity and decreased preoperative IKS scores in the residual varus group. The postoperative IKS scores and revision rates in this group compare favorably with those of the neutral group despite these differences. Third, the retrospective nature of the study also led to the inclusion of patients with several different, albeit similar, implants. Fourth, we did not explore or analyze the etiology of preoperative deformities. Patients with large intraarticular deformities might be easier to correct to neutral alignment than those with large degrees of varus in the tibia, potentially affecting outcome. Fifth, manual goniometer measurements of limb alignment reportedly are accurate to between 2° and 3° [7, 29]. The use of digital radiography and computers for angle measurements might improve the accuracy of these measurements [26]. Sixth, we excluded patients with a postoperative flexion deformity from our analysis as this condition can alter measures of FTMA radiographically [5, 17]. Seventh, we used the IKS score to compare knees of the residual varus group and the neutral alignment group; however, the IKS score awards more points to knees with neutral alignment. This fact would effectively lower the scores of knees in the residual varus group [11]. Eight, the study was performed with components from only one manufacturer. We believe the findings applicable to all TKA prostheses, but additional studies are needed to confirm this assertion. Finally, we lack sufficient patient numbers to further analyze the interactions between femoral and tibial component alignment and overall limb alignment. For example, we are unable to determine whether the lower IKS scores in patients with tibial component varus or femoral component valgus are worsened by overall limb alignment other than neutral.
Our most important finding is that residual varus limb alignment does not portend lower function or lower medium-term survival after TKA for patients with varus osteoarthritis. Additionally, we did not find an association between residual varus alignment and implant revision. Although two recent studies found little correlation between limb alignment and revision rates [21, 22], the majority of studies showed increased revision rates with malalignment, particularly in varus [3, 8, 12, 15, 23, 27] (Table 4). Several factors likely contribute to the different findings in our study. First, numerous studies cited above feature older implant designs [8, 12, 15, 23, 27]. Advances in implant design, polyethylene processing, and cementing technique might improve the tolerance of mild malalignment after TKA. Second, these studies do not stratify revision rates or IKS scores based on preoperative limb alignment. We believe this a critical point. Placing a knee that was in neutral alignment preoperatively into varus alignment is likely quite different from hypocorrecting a knee with substantial preoperative varus. Finally, there are many factors in component positioning affecting overall limb alignment. According to our data whether residual varus comes from tibial component malalignment or another source influences the revision rate and IKS score. Similarly, three prior studies evaluating the influence of limb alignment on IKS scores did have lower scores with alignment other than neutral (Table 5) [6, 13, 16]. The patients in these studies all had substantially shorter followups than our patients and the studies did not separately analyze patients with residual varus or consider the effect of preoperative alignment.
Table 4.
Outcome scores and revision rates based on postoperative limb alignment
| Study | Range of followup (years) | Revision rate | Significance | ||||
|---|---|---|---|---|---|---|---|
| Neutral | Varus | Valgus | Neutral versus varus | Neutral versus valgus | Varus versus valgus | ||
| Fang et al. [8] | 2 to 22.5 | 21/4029 (0.5%) | 18/1222 (1.8%) | 12/819 (1.5%) | p = 0.002 | p = 0.003 | NS |
| Jeffery et al. [12] | 1 to 12 | 2/78 (3%) | 9/37 (24%) | p < 0.001* | |||
| Lewallen et al. [15] | 6.5 to 12.5 | 46/166 (28%) | 12/18 (67%) | 13/25 (52%) | p < 0.001 | p < 0.001 | NS |
| Morgan et al. [21] | NR to 11 | 3/73 (4.1%) | 2/66 (3%) | 1/58 (1.7%) | NS | NS | NS |
| Parratte et al. [22] | 0.5 to 15 | 45/292 (15%) | 14/106 (13%) | p = 0.88* | |||
| Ritter et al. [23] | 0.2 to 13 | 5/35 (14%) | 3/234 (1.3%) | 0/82 (0%) | p = 0.04 | p = 0.28 | p = 0.03 |
| Tew & Waugh [27] | 1 to 9 | 45/192 (23%) | 44/127 (35%) | 33/109 (30%) | p < 0.001 | p < 0.001 | NS |
| Current study | 2 to 19.8 | 13/352 (3.7%) | 3/181 (1.7%) | p = 0.19 | |||
* Jeffery et al. and Parratte et al. compared knees with neutral alignment with those with varus or valgus; NR = not reported; NS = not significant.
Table 5.
Outcome scores based on postoperative limb alignment
| Study | Mean followup (years) | Clinical outcome score | Significance | |||||
|---|---|---|---|---|---|---|---|---|
| Score | Neutral | Varus | Valgus | Neutral versus varus | Neutral versus valgus | Varus versus valgus | ||
| Choong et al. [6] | 1 | IKS | 168 | 135 | p < 0.001* | |||
| Kamat et al. [13] | 3 | OKS | 29.5 | 23.3 | p = 0.035* | |||
| Longstaff et al. [16] | 1 | IKS | 154 | 137 | p = 0.013* | |||
| Current study | 5.8 | IKS | 168.5 | 172.5 | p = 0.12 | |||
* Choong et al., Kamat et al., and Longstaff et al. compared knees with neutral alignment with those with varus or valgus; varus = less than 177°; neutral = 177° to 183°; valgus = greater than 183°; IKS = International Knee Society; OKS = Oxford Knee Score.
Our findings should not be interpreted to suggest TKA component alignment does not influence long-term durability. Although we observed complete correction of preoperative varus alignment is unnecessary to obtain comparable revision rates and IKS scores, we also showed the critical importance of avoiding tibial component varus. Failure to completely correct tibial varus leads to lower IKS scores (Fig. 2). Numerous authors have reported an association between tibial component varus alignment and increased failure rates [1, 3, 8, 10, 18, 20, 27].
Similarly, placement of the femoral component in valgus yielded lower IKS scores when considering all knees with preoperative varus (Fig. 3) as well as only those with preoperative varus greater than 10° (Fig. 5). These lower IKS scores may be associated with the more oblique cut and subsequent more difficult ligament balancing required to achieve femoral valgus in many patients with a preoperative varus deformity. There are less data in the literature regarding the influence of femoral component alignment on failure rates. Berend et al. did note a reduction in the risk of revision in knees with the tibial component in varus if the femoral component was placed in “compensatory” valgus [3]. The tendency to associate a valgus femoral cut with a varus tibial cut may contribute to the lower IKS scores noted with femoral component valgus in our series.
In cases of substantial varus (at least 10°), residual varus limb alignment was associated with improved IKS scores in our series. The most likely explanation for this finding is the difficulty associated with obtaining neutral alignment in patients with substantial varus. Sampath et al. [24] described the need for increased operative time to obtain neutral alignment in these difficult cases. This more difficult and time-consuming procedure requires more complex bone cuts and larger soft tissue releases, potentially increasing joint trauma. Additionally, medial soft tissue contracture has been noted in patients with at least 10° varus deformity [2], potentially leading to increased tension medially if alignment is corrected without sufficient release.
In patients with preoperative varus deformities, residual postoperative varus deformity after TKA is not associated with lower postoperative IKS scores or increased failure rates, provided tibial component varus is avoided. Ideal postoperative limb alignment is likely multifactorial and may not be the same for all patients undergoing TKA.
Acknowledgments
We thank Professor Philippe Neyret of the Department of Orthopaedic Surgery, Hôpital de la Croix-Rousse, Centre Albert Trillat, Lyon, France, for guidance and assistance with this project. We also thank Frédéric Marcelli and William H. Beasley for assistance with statistics and data management.
Footnotes
One or more authors (RAM, SL, ES) have received funding from Tornier, Inc. GD has received funding from Tornier, Inc. and DePuy, Inc. Each remaining author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This study was performed at Hôpital de la Croix-Rousse, Centre Albert Trillat, Lyon, France.
References
- 1.Bargren JH, Blaha JD, Freeman MA. Alignment in total knee arthroplasty: correlated biomechanical and clinical observations. Clin Orthop Relat Res. 1983;173:178–183. [PubMed] [Google Scholar]
- 2.Bellemans J, Vandenneucker H, Vanlauwe J, Victor J. The influence of coronal plane deformity on mediolateral ligament status: an observational study in varus knees. Knee Surg Sports Traumatol Arthrosc. 2010;18:152–156. doi: 10.1007/s00167-009-0903-0. [DOI] [PubMed] [Google Scholar]
- 3.Berend ME, Ritter MA, Meding JB, Faris PM, Keating EM, Redelman R, Faris GW, Davis KE. Tibial component failure mechanisms in total knee arthroplasty. Clin Orthop Relat Res. 2004;428:26–34. doi: 10.1097/01.blo.0000148578.22729.0e. [DOI] [PubMed] [Google Scholar]
- 4.Bonutti PM, Dethmers D, Ulrich SD, Seyler TM, Mont MA. Computer navigation-assisted versus minimally invasive TKA: benefits and drawbacks. Clin Orthop Relat Res. 2008;466:2756–2762. doi: 10.1007/s11999-008-0429-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brouwer RW, Jakma TS, Brouwer KH, Verhaar JA. Pitfalls in determining knee alignment: a radiographic cadaver study. J Knee Surg. 2007;20:210–215. doi: 10.1055/s-0030-1248045. [DOI] [PubMed] [Google Scholar]
- 6.Choong PF, Dowsey MM, Stoney JD. Does accurate anatomical alignment result in better function and quality of life? Comparing conventional and computer-assisted total knee arthroplasty. J Arthroplasty. 2009;24:560–569. doi: 10.1016/j.arth.2008.02.018. [DOI] [PubMed] [Google Scholar]
- 7.Cooke TD, Sled EA, Scudamore RA. Frontal plane knee alignment: a call for standardized measurement. J Rheumatol. 2007;34:1796–1801. [PubMed] [Google Scholar]
- 8.Fang DM, Ritter MA, Davis KE. Coronal alignment in total knee arthroplasty: just how important is it? J Arthroplasty. 2009;24:39–43. doi: 10.1016/j.arth.2009.04.034. [DOI] [PubMed] [Google Scholar]
- 9.Heyse TJ, Decking R, Davis J, Boettner F, Laskin RS. Varus gonarthrosis predisposes to varus malalignment in TKA. HSS J. 2009;5:143–148. doi: 10.1007/s11420-009-9118-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Insall JN, Binazzi R, Soudry M, Mestriner LA. Total knee arthroplasty. Clin Orthop Relat Res. 1985;192:13–22. [PubMed] [Google Scholar]
- 11.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed] [Google Scholar]
- 12.Jeffery RS, Morris RW, Denham RA. Coronal alignment after total knee replacement. J Bone Joint Surg Br. 1991;73:709–714. doi: 10.1302/0301-620X.73B5.1894655. [DOI] [PubMed] [Google Scholar]
- 13.Kamat YD, Aurakzai KM, Adhikari AR, Matthews D, Kalairajah Y, Field RE. Does computer navigation in total knee arthroplasty improve patient outcome at midterm follow-up? Int Orthop. 2009;33:1567–1570. doi: 10.1007/s00264-008-0690-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. doi: 10.2307/2281868. [DOI] [Google Scholar]
- 15.Lewallen DG, Bryan RS, Peterson LF. Polycentric total knee arthroplasty: a ten-year follow-up study. J Bone Joint Surg Am. 1984;66:1211–1218. [PubMed] [Google Scholar]
- 16.Longstaff LM, Sloan K, Stamp N, Scaddan M, Beaver R. Good alignment after total knee arthroplasty leads to faster rehabilitation and better function. J Arthroplasty. 2009;24:570–578. doi: 10.1016/j.arth.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 17.Lonner JH, Laird MT, Stuchin SA. Effect of rotation and knee flexion on radiographic alignment in total knee arthroplasties. Clin Orthop Relat Res. 1996;331:102–106. doi: 10.1097/00003086-199610000-00014. [DOI] [PubMed] [Google Scholar]
- 18.Lotke PA, Ecker ML. Influence of positioning of prosthesis in total knee replacement. J Bone Joint Surg Am. 1977;59:77–79. [PubMed] [Google Scholar]
- 19.Marx RG, Grimm P, Lillemoe KA, Robertson CM, Ayeni OR, Lyman S, Bogner EA, Pavlov H. Reliability of lower extremity alignment measurement using radiographs and PACS. Knee Surg Sports Traumatol Arthrosc. 2011 March 23. [Epub ahead of print] [DOI] [PubMed]
- 20.Moreland JR. Mechanisms of failure in total knee arthroplasty. Clin Orthop Relat Res. 1988;226:49–64. [PubMed] [Google Scholar]
- 21.Morgan SS, Bonshahi A, Pradhan N, Gregory A, Gambhir A, Porter ML. The influence of postoperative coronal alignment on revision surgery in total knee arthroplasty. Int Orthop. 2008;32:639–642. doi: 10.1007/s00264-007-0391-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Parratte S, Pagnano MW, Trousdale RT, Berry DJ. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am. 2010;92:2143–2149. doi: 10.2106/JBJS.I.01398. [DOI] [PubMed] [Google Scholar]
- 23.Ritter MA, Faris PM, Keating EM, Meding JB. Postoperative alignment of total knee replacement: its effect on survival. Clin Orthop Relat Res. 1994;299:153–156. [PubMed] [Google Scholar]
- 24.Sampath SA, Voon SH, Sangster M, Davies H. The statistical relationship between varus deformity, surgeon’s experience, BMI and tourniquet time for computer assisted total knee replacements. Knee. 2009;16:121–124. doi: 10.1016/j.knee.2008.09.008. [DOI] [PubMed] [Google Scholar]
- 25.Schroer WC, Calvert GT, Diesfeld PJ, Reedy ME, LeMarr AR. Effects of increased surgical volume on total knee arthroplasty complications. J Arthroplasty. 2008;23:61–67. doi: 10.1016/j.arth.2008.03.013. [DOI] [PubMed] [Google Scholar]
- 26.Siu D, Cooke TD, Broekhoven LD, Lam M, Fisher B, Saunders G, Challis TW. A standardized technique for lower limb radiography: practice, applications, and error analysis. Invest Radiol. 1991;26:71–77. doi: 10.1097/00004424-199101000-00013. [DOI] [PubMed] [Google Scholar]
- 27.Tew M, Waugh W. Tibiofemoral alignment and the results of knee replacement. J Bone Joint Surg Br. 1985;67:551–556. doi: 10.1302/0301-620X.67B4.4030849. [DOI] [PubMed] [Google Scholar]
- 28.Verdonk PC, Pernin J, Pinaroli A, Ait Si Selmi T, Neyret P. Soft tissue balancing in varus total knee arthroplasty: an algorithmic approach. Knee Surg Sports Traumatol Arthrosc. 2009;17:660–666. doi: 10.1007/s00167-009-0755-7. [DOI] [PubMed] [Google Scholar]
- 29.Yaffe MA, Koo SS, Stulberg SD. Radiographic and navigation measurements of TKA limb alignment do not correlate. Clin Orthop Relat Res. 2008;466:2736–2744. doi: 10.1007/s11999-008-0427-9. [DOI] [PMC free article] [PubMed] [Google Scholar]