Abstract
Background
The approach of choice for open reduction internal fixation of displaced fractures involving the scapula neck or body is from posterior. We describe a new approach that minimizes the surgical insult to the soft tissues but preserves the ability to restore alignment and stability to the fracture.
Description of Technique
Based on the fracture pattern, incisions are made along the anatomic bony perimeter to access the scapula borders for reduction and fixation. Since the incisions are centered over sites of “perimeter” fracture displacement of this relatively flat bone, minimal soft tissue retraction and less muscular stripping are necessary, while indirect reduction of the intervening scapula body is accomplished to restore anatomic alignment.
Patients and Methods
We retrospectively reviewed seven men with a mean age of 39 years (range, 19–75 years) who underwent open reduction internal fixation of a displaced scapula body or neck fracture using this minimally invasive approach. The minimum followup was 12 months (mean, 16 months; range, 12–23 months).
Results
Six of the seven patients returned to their original occupation/activities. The mean Disabilities of the Arm, Shoulder and Hand score at followup was 8.1 (range, 0–52; normative mean, 10.1). For all parameters, the mean SF-36 scores of the study patients were comparable to those of the normal population. Both strength and motion returned to equivalency with the uninjured shoulder. There were no intraoperative or postoperative complications.
Conclusions
This novel surgical approach to the scapula allows visualization of fracture reduction without an extensile incision or muscular or subcutaneous flaps and was associated with high functional scores.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Up to 98% of scapula fractures will involve the scapula body and neck [1, 14, 21, 22]. Due to the multitude of fracture types amenable to a posterior approach, it is the operative approach of choice for the majority of cases. A recent systematic review of operative scapula fractures revealed a posterior approach was used in 78.1% of the cases [18]. Fittingly, there has been considerably more interest in variations of the original approach described by Judet [17]. Exposure of the scapula through this approach involves either elevating a muscular flap consisting of the infraspinatus, teres minor, and deltoid [5, 17] or working through the interval between the infraspinatus and teres minor [5, 8, 16, 25].
Each approach has its advantages and disadvantages. The Judet approach allows access to the entire posterior aspect of the scapula body but requires a large skin incision and extensive muscular disruption [5, 17]. Furthermore, the large muscular flap impedes intra-articular visualization of fractures involving the posterior glenoid, and retraction of the flap can create tension on the suprascapular nerve as it curves around the spinoglenoid notch [5, 25]. The primary drawback of the modified Judet approach is the large skin incision with creation of a subcutaneous flap increasing the risk of a postoperative seroma, while its main advantages are less muscular dissection and the ability to fix posterior glenoid fractures with no tension placed on the suprascapular nerve [8, 16, 25].
Our purposes were to (1) describe a new, less invasive surgical technique with minimal muscular dissection that still allows open reduction and internal fixation (ORIF) of complex scapula body/neck fractures and posterior intra-articular glenoid fractures, (2) outline the advantages and disadvantages of our surgical technique compared to other published posterior approaches, and (3) report the clinical outcomes, including return to work/activities, ROM and strength, and patient-based function (Disabilities of the Arm, Shoulder and Hand [DASH] and SF-36) with this technique in seven patients.
Surgical Technique
The patients were placed in the lateral decubitus position utilizing a beanbag and an axillary roll. The body was positioned leaning slightly anteriorly, which aided in exposure of the scapula and intraoperative manipulation of the injured upper extremity. The entire forequarter was prepared, draped, and placed approximately 90° forward flexed over specialized, soft-positioning pillows that protect the contralateral arm under the wedge and allow a working surface for the injured arm on top of the wedge. Depending on the fracture pattern, approximately 6-cm straight incisions were made, oriented over the glenoid neck or lateral border and over the location at the vertebral border or spine where the fracture exits (Fig. 1). Laterally, the dissection was taken down to the deltoid fascia, which was divided in line with the deltoid fibers at its inferior edge. The deltoid was retracted cephalad, revealing the fascia overlying the external rotators. The fascia overlying the infraspinatus and teres minor was then divided in line with the muscular fibers exposing these muscles. Blunt dissection was used down to the lateral border between infraspinatus and teres minor, exposing the fracture site (Fig. 2). Care was taken while retraction of the infraspinatus was performed at the lateral window so as not to tether or injure the suprascapular nerve that exits at the base of the acromion in the spinoglenoid notch. Furthermore, the ascending branch of the circumflex scapular artery was encountered at the lateral border of the scapula approximately 5 to 6 cm below the glenoid rim [31]. This vessel was cauterized as necessary.
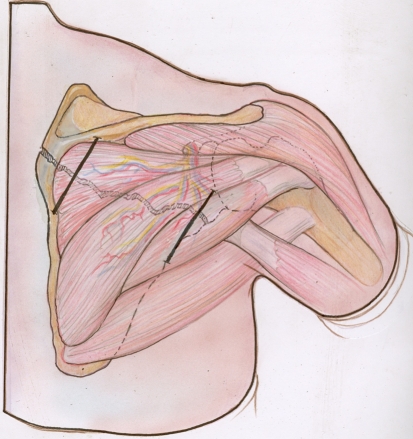
Fig. 1.
A diagram illustrates minimally invasive incisions for fixation of extra-articular scapula body and neck fractures involving the medial and lateral borders. The suprascapular neurovascular bundle is visible coursing around the spinoglenoid notch.
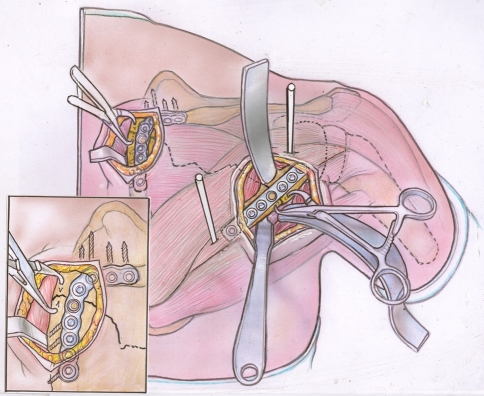
Fig. 2.
A diagram illustrates deep dissection and fixation. Lateral border dissection is through the interval between the teres minor and infraspinatus. The fracture along the medial border is exposed by localized elevation of the infraspinatus. Schanz pins are placed in the proximal and distal fragment (typically the neck and body) and used as joysticks to manipulate the fragments into the correct anatomic alignment. Pointed bone reduction forceps hold the fragments in the desired position until the plates are placed. The inset shows the screw vectors aimed into the area of the scapula with the best bone stock. Note the threaded screw hole overlying the fracture at the medial and lateral borders, indicating locking plates were employed for stable fixation.
At the medial angle at the base of the scapula spine, where most fractures exit medially, dissection was taken down to the fascia and then periosteum along the base of the spine and inferiorly on the vertebral border. A subperiosteal dissection was then performed to elevate the infraspinatus to the degree necessary to visualize the fracture and its reduction. These two small windows gave the surgeon direct access to the two sites of displacement at the scapular perimeter, allowing for reduction and plate fixation along the lateral border and superior angle at the vertebral border as necessary (Fig. 2).
A helpful reduction maneuver in scapula neck and body fractures is to place a Schanz pin (with T-handled chuck) in the glenoid neck, out of the way of eventual plate placement, and to use a pulling device such as a shoulder hook for the distal lateral border, so that the cephalad fragment is mobilized laterally while the caudad fragment is mobilized medially as necessary (Fig. 2). This helped to line up the lateral border, usually allowing for effective clamp application. A pointed bone reduction forceps could be used through small pilot holes on either side of the fracture at the vertebral border strategically placed out of the way of the plate placement.
Typically, we recommend a 2.7-mm dynamic compression plate for the lateral border and a 2.7-mm reconstruction plate for the medial border [5]. Locking plates are recommended, since longer plates are not possible through these small windows of access and since the points of purchase with each screw are only between 8 and 16 mm [26]. An accurate reduction with compression was necessary before plate application. Plate fixation of the lateral border fracture was typically performed first since this plate could be applied straight while the plate for the medial border required contouring. Therefore, the lateral border fixation facilitated maintenance of reduction while the medial border plate was placed. The fascia at the medial border was repaired with 0 braided absorbable suture, and at the lateral incision the fascia was repaired with running 0 braided absorbable suture. Subsequently, the subcutaneous tissue was approximated with 2-0 braided suture and the skin with a running 3-0 absorbable subcuticular stitch. Unlike with an open approach, we have not used drains below this surgical exposure.
Patients and Methods
We created a prospective scapula database in 2002 with approval of the Institutional Review Board to track the surgeon-based clinical observations and patient-based functional outcomes of patients with scapula fractures. From January 2002 to May 2010, 638 patients with a scapula fracture presented to our Level I trauma center or the outpatient clinic of the senior author (PAC). Of these 638 patients, 140 (22%) underwent ORIF for a displaced scapula fracture, of whom 73 were referred with highly displaced scapula fractures that met operative indications. From these 140, we identified and retrospectively reviewed seven patients who had minimally invasive plate osteosynthesis of the scapula as described above. The indications for this approach included (1) a fracture pattern amenable to a posterior approach and meeting relative indications for scapula ORIF (see below); (2) surgery occurring within 4 weeks of the date of injury; and (3) a simple fracture pattern not requiring long-length plates. The contraindications for this approach were (1) fracture of the anterior glenoid, coracoid, or acromion process; (2) scapula fractures greater than 30 days after injury; and (3) segmental fractures of the lateral border or multiple fractures exiting spine, medial, or lateral borders. All seven patients were men with a mean age of 39 years (range, 19–75 years). The mechanisms of injury were a snowmobiling accident in two patients, pedestrian versus motor vehicle in one, bicycle accident in two, fall from a height in one, and a motor vehicle collision in one (Table 1). No patients were lost to followup. No patients were recalled specifically for this study; all data were obtained from IRB-approved data collection forms, medical records, and radiographs. The minimum followup was 12 months (mean, 16 months; range, 12–23 months).
Table 1.
Demographics and fracture characteristics
| Patient | Age (years) | Sex | Mechanism of injury | Classification | Associated injuries | Fracture characteristics (preop/postop) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| AO/OTA | Mayo | Medial/lateral displacement (mm) | Angulation (°) | GPA (°) | Articular step-off (mm) | Articular gap (mm) | |||||
| 1 | 75 | Male | Snowmobile | C3 | Type IV | TBI, PTX, pulm cont, splenic lac, rib fx | 30/0 | 6/0 | 33/34 | 8/0 | 8/1 |
| 2 | 25 | Male | Snowmobile | A3.2 | NA | Femur fx | 21/0 | 26/0 | 24/36 | NA | NA |
| 3 | 52 | Male | Pedestrian vs MVC | A3.2 | NA | PTX, rib fx, facial lac | 21/0 | 3/0 | 39/40 | NA | NA |
| 4 | 19 | Male | Bicycle collision | C1.2 | NA | SSN injury | 11/0 | 10/0 | 16/28 | NA | NA |
| 5 | 26 | Male | Fall from height | A3.2 | NA | None | 23/0 | 22/0 | 33/48 | NA | NA |
| 6 | 47 | Male | MVC | A3.2 | NA | Ips distal radius/ulna fx, ips 2-5 metacarpal fx | 40/0 | 15/0 | 37/40 | NA | NA |
| 7 | 32 | Male | Bicycle collision | C1.1 | NA | None | 29/0 | 7/0 | 25/34 | NA | NA |
Preop = preoperative; postop = postoperative; GPA = glenopolar angle; MVC = motor vehicle collision; NA = not applicable; TBI = traumatic brain injury; PTX = pneumothorax; pulm cont = pulmonary contusion; lac = laceration; fx = fracture; SSN = suprascapular nerve; ips = ipsilateral.
Fractures were classified according to the revised AO/OTA [19] and Mayo [20] classifications and included four patients with comminuted body fractures (14-A3.2), one patient with an intra-articular glenoid fracture with extension into the body (14-C3, Mayo Type IV), one patient with an extra-articular comminuted scapula neck fracture (C1.2), and one patient with an extra-articular scapula neck fracture (C1.1). Five of the seven patients had associated injuries, including rib fractures (n = 2), ipsilateral distal radius fracture (n = 1), ipsilateral distal ulna fracture (n = 1), ipsilateral metacarpal fracture(s) (n = 1), pneumothorax (n = 2), pulmonary contusion (n = 1), complex facial laceration (n = 1), traumatic brain injury (n = 1), Grade I splenic laceration (n = 1), suprascapular nerve injury (n = 1), and left midshaft femur fracture (n = 1) (Table 1).
In six patients, medial/lateral displacement of the glenohumeral joint in relationship to the lateral border of more than 20 mm was the primary indication for surgery, with a mean displacement of 27 mm (range, 21–40 mm) (Fig. 3). A glenopolar angle (GPA) of 22° or less and an intra-articular step-off or gap of 4 mm or more were each operative indications in one patient (GPA = 16°, step-off = 8 mm, gap = 8 mm) (Table 1). The mean time elapsed from injury until the time of surgery was 11 days (range, 4–22 days) (Table 2). The senior author has previously published on the delayed treatment of scapula fractures [10]. After 3 weeks, osteoclasis and débridement to identify fracture lines were necessary, while after 6 weeks, osteoclasis combined with an osteotomy was required due to abundant mature callus formation. Therefore, the less invasive technique would be difficult for patients more than 3 weeks from the date of injury but not impossible. We believe a Judet approach would be more appropriate in such patients at this time. One patient had exploration and repair of a branch of the suprascapular nerve concomitantly with ORIF of the scapula. All seven patients had the lateral incision, with six requiring a medial incision. The patient with the comminuted glenoid neck fracture (C1.2) only required the lateral incision as the fracture did not exit out the medial border. Mean estimated blood loss was 250 mL (range, 150–300 mL).
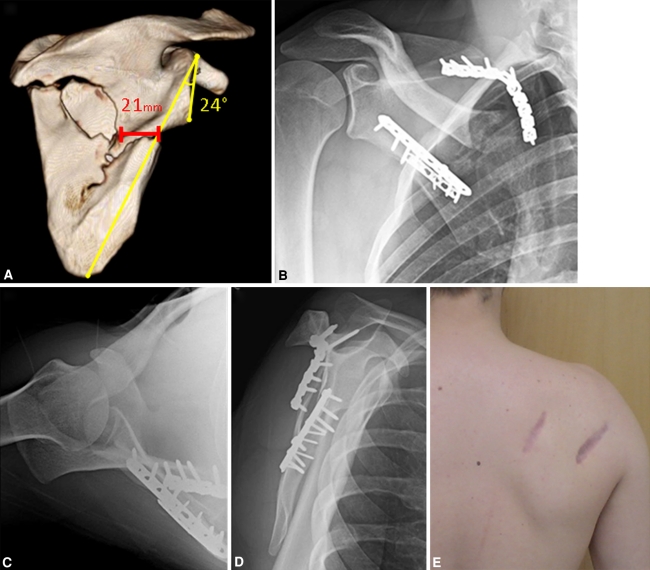
Fig. 3A–E.
Images illustrate the case of Patient 2. (A) A preoperative three-dimensional CT posterior-anterior view shows a comminuted scapula body fracture with 21 mm of medial/lateral displacement and a GPA of 24º. (B) A postoperative AP radiograph demonstrates restoration of normal scapular anatomy with 0 mm of medial/lateral displacement and a normal GPA of 36º. In addition, postoperative (C) axillary and (D) scapula Y views demonstrate 0° of translation and angulation at the initial fracture site. (E) A postoperative photograph shows the operated shoulder. The combined length of the incisions was 14 cm.
Table 2.
Operative information and fracture fixation
| Patient | Time to surgery (days) | EBL (mL) | Operative time (minutes) | Fracture fixation (number of holes) | |||
|---|---|---|---|---|---|---|---|
| Lateral border | SMA | Neck | Glenoid | ||||
| 1 | 6 | 200 | 290 | T-plate (8) | 2.7-mm recon (9) | L-plate (3) | 2-mm LCP (3) 3.5-mm lag screw × 2 |
| 2 | 22 | 300 | 172 | 2.7-mm DC (9) 2-mm LCP (6) |
2.7-mm recon (10) | ||
| 3 | 4 | 200 | 155 | 2.7-mm DC (7) | 2.7-mm recon (8) | ||
| 4 | 8 | 300 | 185 | 2.7-mm DC (7) | 2.7-mm DC (3) T-plate (8) 2.7-mm lag screw × 2 |
||
| 5 | 12 | 300 | 146 | 2.7-mm DC (8) 2.4-mm LCP (6) |
2.7-mm recon (8) | ||
| 6 | 13 | 150 | 174 | 2.7-mm DC (12) 2-mm LCP (7) |
2.7-mm recon (7) | ||
| 7 | 12 | 300 | 157 | 2.7-mm DC (5) | 2.7-mm recon (8) | 2-mm LCP (3) | |
EBL = estimated blood loss; SMA = superior medial angle; DC = dynamic compression plate; LCP = locking compression plate; recon = reconstruction plate.
Immediately postoperatively, patients were given a sling for comfort and physical therapy was initiated. Patients were allowed to do full passive and active ROM and utilized pulleys, therapist-assisted stretching, and push-pull sticks to regain ROM. After 4 weeks, the focus was placed on regaining full active ROM, with strengthening using 3- to 5-pound weights, therapy bands, and proprioceptive exercises. Formal physical therapy concluded by 12 weeks, with all restrictions lifted at 3 months.
The postoperative followup protocol consisted of appointments at 1 to 2 and 6 weeks after surgery and at 3, 6, 12, 18, and 24 months. Postoperative radiographs included an AP, scapula Y, and axillary lateral at 2 and 6 weeks, with only an AP view at subsequent clinic appointments. All seven patients underwent clinical ROM testing by a single examiner (PAC) using a 14-inch goniometer and strength testing using a handheld dynamometer [9, 11] (MicroFET™ 2; Hoggan Health Industries, Draper, UT) and completed DASH [12] and SF-36 [27] questionnaires; we typically obtain the questionnaires beginning at 6 months but obtained them at 3 months in two patients and one at 6 weeks due to accelerated return to full work and activities. Our clinical criteria for fracture healing included painless ROM and no tenderness to palpation overlying the fracture lines. The surgical scars were measured and compared to five consecutive patients in whom a Judet incision was used for similar fracture patterns. We recorded complications from the medical records. We also recorded time to return to full work.
Both authors (PAC, EMG) independently evaluated all postoperative radiographs to determine the presence of nonunion or malunion. There is no radiographic or clinical consensus on the definition of fracture union [6]. Whelan et al. [29] studied the interobserver reliability on determination of tibial fracture healing and found a kappa value of 0.60 for a radiographic union scale and 0.67 for a general impression of fracture healing. This indicates there is a substantial amount of agreement between observers in determination of fracture union. We found no studies describing interobserver variability of assessing union of scapular fractures. We defined nonunion as a persistent fracture line on any radiographic view after 8 weeks or a painful shoulder with associated fixation failure including broken hardware or screw pull-out. Malunion was determined by meeting at least one of four parameters: displacement of greater than 0.5 cm on the AP radiograph, displacement of greater than 0.5 cm on the scapula Y radiograph, persistent angular deformity on scapula Y radiographs of greater than 10°, or a difference in GPA of 10° or more from the contralateral shoulder.
Results
At last followup, all fractures demonstrated clinical and radiographic evidence of union. There were no malunions (Table 1). The mean combined length for the medial and lateral incisions in the minimally invasive group was 14.8 cm (range, 12–20 cm) whereas the group operated on through the Judet incision had a mean scar length of 29.2 cm (range, 28–30 cm). The mean postoperative ROM for the injured/uninjured arm was 161°/162° of forward flexion, 117°/115° of abduction, and 74°/78° of external rotation with the arm by the patient’s side and the elbow flexed to 90° (Table 3). The mean postoperative strength for the injured/uninjured arm was 21/22 pounds of force for forward flexion, 17/18 pounds of force for abduction, and 23/26 pounds of force for external rotation (Table 3). The mean DASH score at followup was 8.1 (range, 0–52; normative mean, 10.1) [13]. The mean SF-36 score of the study patients was 55 (range, 38–59) and comparable to the normative mean of 50 [27, 28]. There were no intraoperative or postoperative complications.
Table 3.
Patient followup results, including strength, ROM, and DASH scores
| Patient | Followup (months) | DASH | ROM (°) (injured/noninjured) | Strength (pounds of force) (injured/noninjured) | Return to work/ activities | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| FF | ABD | ER | IR (vertebra) | FF | ABD | ER | ||||
| 1 | 12 | 0 | 133/145 | 86/88 | 66/74 | T5/T4 | 15/16 | 13/13 | 16/17 | Yes |
| 2 | 23 | 0 | 170/170 | 95/95 | 76/76 | T10/T10 | 27/29 | 26/24 | 30/34 | Yes |
| 3 | 13 | 0 | 170/170 | 120/115 | 70/78 | T10/L1 | 27/28 | 18/19 | 27/30 | Yes |
| 4 | 23 | 3 | 158/158 | 127/127 | 55/63 | T4/T3 | 10/11 | 13/18 | 11/14 | Yes |
| 5 | 19 | 0 | 178/178 | 152/152 | 98/97 | T3/T3 | 25/24 | 16/18 | 29/29 | Yes |
| 6* | 12 | 52 | 142/142 | 102/105 | 66/68 | T8/T5 | 21/24 | 14/18 | 29/34 | No |
| 7 | 12 | 2 | 174/174 | 134/122 | 90/90 | T1/T1 | 21/22 | 16/18 | 20/24 | Yes |
* Patient specifically stated upper-extremity disability is due to ipsilateral forearm and hand injuries; DASH = Disabilities of the Arm, Shoulder, and Hand; FF = forward flexion; ABD = abduction; ER = external rotation; IR = internal rotation.
Discussion
Scapula fractures have distinctive patterns with predictable zones where the fracture exits the scapula [3]. Knowledge of the common patterns, along with accurate determination of the specific scapula fracture, is necessary in choosing a surgical approach. Since 62% to 98% of scapula fractures involve the scapula body/neck, the posterior approach is the most common approach for ORIF of scapula fractures [1, 14, 21, 22]. Our purpose was to describe a novel, less invasive surgical technique with minimal muscular dissection that still allows ORIF of complex scapula fractures involving the body, neck, and posterior glenoid; outline the advantages and disadvantages of our surgical technique compared to other published posterior approaches; and report the clinical and functional outcome with this technique in a small case series.
We acknowledge limitations to our study. First, we recognize our cohort is too small to provide statistical evidence that our patients have better ROM or function when compared to patients who underwent fixation using the Judet or modified Judet approach. However, this initial evidence for quicker return of strength, ROM, and function mimics the experience of long-bone fractures treated with so-called minimally invasive approaches [2]. We intend to conduct a larger study comparing the rate of improvement after reconstruction of scapula fractures utilizing different surgical techniques. Second, the senior author gained a substantial amount of experience on scapula fracture reduction and fixation through the Judet and modified Judet approaches before developing this less invasive approach, so it remains to be seen whether patient outcomes and low complication rate can be extrapolated to surgeons with lower volume.
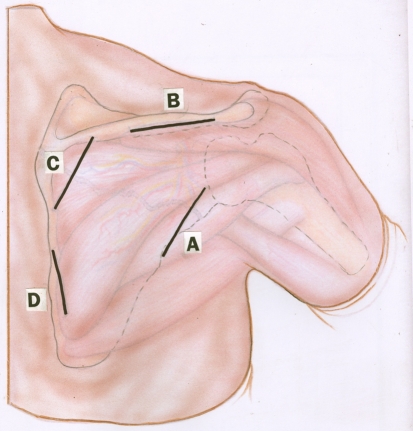
Our surgical approach strategically places small incisions over the perimeter of the scapula to allow fracture fixation (Fig. 4). The authors believe the fractures best indicated for this approach are simple patterns in which the fracture has a single exit point through the lateral border and a single exit point through the vertebral border and in which surgery is performed within a week of the injury when the fractures are very mobile. However, as with many other areas in orthopaedic surgery, the more familiar surgeons are with an approach, the more they can accomplish through that approach. Accordingly, we have extended the use of the minimally invasive approach to body fractures associated with posterior glenoid fractures and fractures that have also emanated through the acromial spine or have a segmental fracture through the vertebral border.
Fig. 4.
A diagram illustrates the possible scapula incisions. In our study, all seven patients had the lateral border incision (Incision A), with four patients requiring the incision overlying the medial border (Incision C). One major advantage over the Judet incision is the different combinations of incisions depending on the fracture pattern instead of a single incision regardless of the fracture type. Incision B is used for fractures extending through the scapular spine and Incision D for fractures exiting the inferior medial border.
There are several advantages to our surgical approach. First and foremost, these limited surgical windows minimize creation of subcutaneous flaps and disruption of the posterior scapula musculature. A commonly accepted strategy for long-bone fractures is to obtain a closed reduction of the fracture (metaphyseal or diaphyseal) and use small incisions remote from the fracture site to apply implants for fixation. We employ the same concept here for the fixation of scapula fractures. The scapula is a triangular-shaped flat bone, so instead of the incisions being distant from the fracture site, they are at each end of the fracture. This approach thus allows the luxury of direct reduction of the fracture, without exposing the majority of the fracture line across the body. It is likely a wide range of scapula fractures can be surgically reconstructed using this method. We report on patients with scapula body, neck, and posterior glenoid fractures. The placement of the incisions allows them to be extended if increased exposure is required for more complex patterns or occult fractures creating segmental fragments at the scapula borders. The medial incision can be extended distally toward the inferior angle and laterally along the scapular spine as much as necessary to access a fracture line exiting lateral to the base of the spine. The lateral incision can also be extended distally toward the inferior angle and proximally over the glenoid and acromioclavicular joint and even anteriorly for coracoid fixation. Lastly, the shorter length of these incisions (4–10 cm) results in improved cosmetic outcomes for patients, though this must not be the primary basis for choosing this approach.
There have been several descriptions in the literature of posterior approaches to scapula fractures (Table 4). Obremskey and Lyman [25] described a modified Judet approach employing the Judet skin incision and fixation of the lateral border through the teres minor/infraspinatus interval and the medial border through localized dissection of the infraspinatus. This approach has recently been employed with the exclusive use of 2.7-mm plates for fixation [16]. A similar technique combines the Judet skin incision and variably placed “windows” [5] or “portals” [4] at the scapular spine, medial, or lateral borders. All of these approaches have the advantage of limiting the amount of deep muscular dissection and allowing for elevation of a muscular flap if increased posterior exposure is necessary. Differences between our approach and the preceding techniques include the dissection of the posterior deltoid from its origin on the scapular spine and the resultant scar from the extensile Judet incision. Furthermore, our approach does not yield a large subcutaneous flap, which would theoretically be more vulnerable to hematoma accumulation and/or scarring. Wiedemann [30] described an oblique incision starting slightly inferior to the medial 1/3 of the scapular spine and extending laterally into the axilla. This approach allows access to the lateral border and inferior glenoid but is inadequate for addressing neck and body variants, scapula spine, and vertebral border. Furthermore, exposure cannot be extended, if needed, for more complex variants. The elevation of a large muscular flap restricts the Judet approach from being used for intra-articular inspection of glenoid fractures. Therefore, several approaches have been described for posterior glenoid fractures [7, 15, 24, 32]. Disadvantages of these approaches include lack of exposure of the scapula neck/body and the increase in injury to the axillary nerve by splitting the deltoid. The modified Judet approach [25] can be used for a variety of intra-articular glenoid fractures. Nork et al. [23] employed this approach specifically for displaced glenoid fractures with extension medially into the scapula body. An impetus for the publication of this new surgical technique and the outcomes of a relatively small cohort was comments from patients regarding how quickly they were able to return to their activities after surgery. There were several instances of patients using the injured arm well ahead of the recommended course of progression of physical therapy. Patient 1, a 75-year-old man with an intra-articular glenoid fracture, admitted to playing a full round of golf the week before his 3-month followup and claimed to have no pain or limitation. Two of the patients had full active ROM at their first postoperative visit. Corroboration of faster recovery will be necessary in future studies.
Table 4.
Comparison of posterior approaches reported in the literature
| Study | Fracture types amenable to fixation | Incision | SubQ flap | Infraspinatus flap | Deltoid reflection or split | Clinical experience | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Body | Neck | Posterior glenoid | Patients (% followup) | Mean followup | Outcome measurements/comments | |||||
| Hardegger et al. [8] (1984) | No | Yes | Yes | Starts at acromion and extends medially along scapular spine curving to inferior scapula angle | Yes | Optional | NR | 37 (89%) | 6.5 years (18 months to 15 years) | ROM: 21 full; pain: 25 pain free; strength grade: 22 patients 5/5; unclear what % patients underwent posterior approach |
| Norwood et al. [24] (1985) | No | No | Yes | Starts midscapular spine curving anteriorly at posterior edge of acromion | No | No | Yes | 42 (100%) | NR | No infection; no deltoid weakness; good strength; only 1 patient had a scapula fracture |
| Wirth et al. [32] (1993) | No | Yes | Yes | 8-cm straight incision from lateral acromion to posterior axillary crease | Yes | No | Yes | 35 (86%) | 20 months (1 month to 11.4 years) | No weakness; only 1 patient had a scapula fracture |
| Ebraheim et al. [7] (1997) | No | Yes | Yes | Starts at medial 1/3 scapular spine and extends laterally curving distally along lateral border | Yes | Optional | Yes | 2 (100%) | NR | No complications; neurovascularly intact |
| Jerosch et al. [15] (2001) | No | Yes | Yes | Oblique incision immediately inferior and in line with deltoid fibers | No | No | No | 12 (100%) | NR | No complications; no signs/symptoms of sensory or motor dysfunction; no patients were treated for a scapula fracture |
| Obremskey and Lyman [25] (2004) | Yes | Yes | Yes | Starts inferiorly to the acromion and extends medially to the superomedial angle, curving inferiorly to inferior angle | Yes | No | Yes | 10 (NR) | NR | No complications; 100% union; nearly full ROM and strength |
| Wiedemann [30] (2004) | No | Yes | Yes | Oblique incision starting slightly inferior to the medial 1/3 of the scapular spine and extending laterally into the axilla | No | No | No | None | NA | NA |
| Braun et al. [4] (2005) | No | Yes | Yes | Starts at acromion and extends medially along scapular spine curving to inferior scapula angle | Yes | No | Yes | 19 (100%) | 26 months (6–39 months) | Constant-Murley score: 79.9/100 |
| Nork et al. [23] (2008) | Yes | Yes | Yes | Starts inferiorly to the acromion and extends medially to the superomedial angle, curving inferiorly to inferior angle | Yes | No | Yes | 17 (100%) | NR | No postoperative neurologic deficits; no wound infections; 100% union |
| Gauger and Cole (2011) | Yes | Yes | Yes | ~6-cm incisions along the scapula bony perimeter to access fracture exit sites | No | No | No | 7 (100%) | 16 months (12–23 months) | Clinical: ROM, strength, return to work/activities; functional: DASH, SF-36 |
SubQ = subcutaneous; NR = not reported; NA = not applicable.
In conclusion, we describe a minimally invasive surgical approach to the scapula body, neck, and posterior glenoid that allows visualization of fracture reduction without an extensive Judet incision or creation of muscular flaps and was associated with DASH and SF-36 scores comparable to a normal (uninjured) population without any complications.
Footnotes
One or more of the authors (PAC) have received funding from Synthes, Inc (West Chester, PA). The funding source for this study did not play a role in the investigation.
Each author certifies that his institution has approved the human protocol for this investigation as required, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Ada JR, Miller ME. Scapular fractures: analysis of 113 cases. Clin Orthop Relat Res. 1991;269:174–180. [PubMed] [Google Scholar]
- 2.An Z, Zeng B, He X, Chen Q, Hu S. Plating osteosynthesis of mid-distal humeral shaft fractures: minimally invasive versus conventional open reduction technique. Int Orthop. 2010;34:131–135. doi: 10.1007/s00264-009-0753-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Armitage BM, Wijdicks CA, Tarkin IS, Schroder LK, Marek DJ, Zlowodzki M, Cole PA. Mapping of scapular fractures with three-dimensional computed tomography. J Bone Joint Surg Am. 2009;91:2222–2228. doi: 10.2106/JBJS.H.00881. [DOI] [PubMed] [Google Scholar]
- 4.Braun C, Wirbel R, Mutschler W. The two-portal approach for internal fixation of scapular fractures. Eur J Trauma. 2005;31:186–193. doi: 10.1007/s00068-005-6205-4. [DOI] [Google Scholar]
- 5.Cole PA. Scapula fractures: open reduction internal fixation. In: Wiss DA, ed. Fractures. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006:15–36.
- 6.Corrales LA, Morshed S, Bhandari M, Miclau T., 3rd Variability in the assessment of fracture-healing in orthopaedic trauma studies. J Bone Joint Surg Am. 2008;90:1862–1868. doi: 10.2106/JBJS.G.01580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ebraheim NA, Mekhail AO, Padanilum TG, Yeasting RA. Anatomic considerations for a modified posterior approach to the scapula. Clin Orthop Relat Res. 1997;334:136–143. [PubMed] [Google Scholar]
- 8.Hardegger FH, Simpson LA, Weber BG. The operative treatment of scapular fractures. J Bone Joint Surg Br. 1984;66:725–731. doi: 10.1302/0301-620X.66B5.6501369. [DOI] [PubMed] [Google Scholar]
- 9.Hayes K, Walton JR, Szomor ZL, Murrell GA. Reliability of 3 methods for assessing shoulder strength. J Shoulder Elbow Surg. 2002;11:33–39. doi: 10.1067/mse.2002.119852. [DOI] [PubMed] [Google Scholar]
- 10.Herrera DA, Anavian J, Tarkin IS, Armitage BA, Schroder LK, Cole PA. Delayed operative management of fractures of the scapula. J Bone Joint Surg Br. 2009;91:619–626. doi: 10.1302/0301-620X.91B5.22158. [DOI] [PubMed] [Google Scholar]
- 11.Hsieh CY, Phillips RB. Reliability of manual muscle testing with a computerized dynamometer. J Manipulative Physiol Ther. 1990;13:72–82. [PubMed] [Google Scholar]
- 12.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: The DASH (Disabilities of the Arm, Shoulder and Hand) [corrected]. The Upper Extremity Collaborative Group (UECG) Am J Ind Med. 1996;29:602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 13.Hunsaker FG, Cioffi DA, Amadio PC, Wright JG, Caughlin B. The American Academy of Orthopaedic Surgeons Outcomes Instruments: normative values from the general population. J Bone Joint Surg Am. 2002;84:208–215. doi: 10.2106/00004623-200202000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Imatani RJ. Fractures of the scapula: a review of 53 fractures. J Trauma. 1975;15:473–478. doi: 10.1097/00005373-197506000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Jerosch J, Greig M, Peuker ET, Filler TJ. The posterior subdeltoid approach: a modified access to the posterior glenohumeral joint. J Shoulder Elbow Surg. 2001;10:265–268. doi: 10.1067/mse.2001.112885. [DOI] [PubMed] [Google Scholar]
- 16.Jones CB, Cornelius JP, Sietsema DL, Ringler JR, Endres TJ. Modified Judet approach and minifragment fixation of scapular body and glenoid neck fractures. J Orthop Trauma. 2009;23:558–564. doi: 10.1097/BOT.0b013e3181a18216. [DOI] [PubMed] [Google Scholar]
- 17.Judet R. Surgical treatment of scapular fractures. Acta Orthop Belg. 1964;30:673–678. [PubMed] [Google Scholar]
- 18.Lantry JM, Roberts CS, Giannoudis PV. Operative treatment of scapular fractures: a systematic review. Injury. 2008;39:271–283. doi: 10.1016/j.injury.2007.06.018. [DOI] [PubMed] [Google Scholar]
- 19.Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, Prokuski L, Sirkin MS, Ziran B, Henley B, Audige L. Fracture and Dislocation Classification Compendium - 2007: Orthopaedic Trauma Association Classification, Database and Outcomes Committee. J Orthop Trauma. 2007;10(Suppl):S1–S133. doi: 10.1097/00005131-200711101-00001. [DOI] [PubMed] [Google Scholar]
- 20.Mayo KA, Benirschke SK, Mast JW. Displaced fractures of the glenoid fossa: results of open reduction and internal fixation. Clin Orthop Relat Res. 1998;347:122–130. doi: 10.1097/00003086-199802000-00015. [DOI] [PubMed] [Google Scholar]
- 21.McGahan JP, Rab GT, Dublin A. Fractures of the scapula. J Trauma. 1980;20:880–883. doi: 10.1097/00005373-198010000-00011. [DOI] [PubMed] [Google Scholar]
- 22.McGinnis M, Denton JR. Fractures of the scapula: a retrospective study of 40 fractured scapulae. J Trauma. 1989;29:1488–1493. doi: 10.1097/00005373-198911000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Nork SE, Barei DP, Gardner MJ, Schildhauer TA, Mayo KA, Benirschke SK. Surgical exposure, fixation of displaced Type IV V, and VI glenoid fractures. J Orthop Trauma. 2008;22:487–493. doi: 10.1097/BOT.0b013e31817d5356. [DOI] [PubMed] [Google Scholar]
- 24.Norwood LA, Matiko JA, Terry GC. Posterior shoulder approach. Clin Orthop Relat Res. 1985;201:167–172. [PubMed] [Google Scholar]
- 25.Obremskey WT, Lyman JR. A modified Judet approach to the scapula. J Orthop Trauma. 2004;18:696–699. doi: 10.1097/00005131-200411000-00007. [DOI] [PubMed] [Google Scholar]
- 26.Schroeder HP, Kuiper SD, Botte MJ. Osseous anatomy of the scapula. Clin Orthop Relat Res. 2001;383:131–139. doi: 10.1097/00003086-200102000-00015. [DOI] [PubMed] [Google Scholar]
- 27.Ware JE, Kosinski M, Keller SD. SF-36 Physical and Mental Health Summary Scales: A User’s Manual. Boston, MA: New England Medical Center, Health Assessment Lab; 1994. [Google Scholar]
- 28.Ware JE, Jr, Sherbourne CD. The MOS 36-item Short-form Health Survey (SF-36) I. Conceptual framework and item selection. Med Care. 1992;30:473–483. doi: 10.1097/00005650-199206000-00002. [DOI] [PubMed] [Google Scholar]
- 29.Whelan DB, Bhandari M, McKee MD, Guyatt GH, Kreder HJ, Stephen D, Schemitsch EH. Interobserver and intraobserver variation in the assessment of the healing of tibial fractures after intramedullary fixation. J Bone Joint Surg Br. 2002;84:15–18. doi: 10.1302/0301-620X.84B1.11347. [DOI] [PubMed] [Google Scholar]
- 30.Wiedemann E. Fractures of the scapula] [in German. Unfallchirurg. 2004;107:1124–1133. doi: 10.1007/s00113-004-0892-x. [DOI] [PubMed] [Google Scholar]
- 31.Wijdicks CA, Armitage BM, Anavian J, Schroder LK, Cole PA. Vulnerable neurovasculature with a posterior approach to the scapula. Clin Orthop Relat Res. 2009;467:2011–2017. doi: 10.1007/s11999-008-0635-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wirth MA, Butters KP, Rockwood CA., Jr The posterior deltoid-splitting approach to the shoulder. Clin Orthop Relat Res. 1993;296:92–98. [PubMed] [Google Scholar]