Abstract
Background
Intramedullary clavicle fixation is a potential alternative to plate fixation. Previous studies documenting the complication rates of intramedullary clavicle fixation have demonstrated variable rates of soft tissue complications and fracture healing.
Questions/purposes
We asked the following questions: (1) Does use of the Rockwood Clavicle Pin (DePuy Orthopaedics Inc, Warsaw, IN) predispose patients to soft tissue complications requiring additional surgery or a high infection risk? (2) Does the Rockwood Clavicle Pin provide a truly minimally invasive insertion technique and reliable fracture fixation?
Patients and Methods
We retrospectively evaluated 18 patients (mean age, 31 years) who sustained a closed midshaft fracture of the clavicle treated with open intramedullary nailing with a Rockwood Clavicle Pin. We determined the incidence of complications and rate of fracture healing.
Results
Fourteen complications occurred in 10 patients. Five patients experienced a complication with fracture healing, including three nonunions. Nine patients experienced complications relating to soft tissue, including infection, skin necrosis, or posterior pain from pin prominence.
Conclusions
The Rockwood Clavicle Pin remains a historically relevant method of clavicle fixation. However, due to an unacceptably high rate of nonunion, repeat operation, and soft tissue complications, we do not recommend this device for treating middiaphyseal clavicle fractures.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
The acute midshaft clavicle fracture is one of the most common fractures treated by orthopaedic surgeons, representing 10% to 15% of all adult fractures [13, 15, 19]. Traditionally, this fracture has been managed with figure-of-eight sling immobilization. Early studies completed by Neer [12] and Rowe [18] demonstrated nonunion rates of less than 1% with nonoperative management of diaphyseal clavicle fractures. Based on these data, previous wisdom has dictated a nonoperative course of management for middle-third clavicle fractures.
Recent evidence suggests nonunion rates are higher than previously reported, with rates ranging from 20% to 47% for displaced and comminuted diaphyseal fractures [2, 3, 7, 14, 17]. The rate of nonunion is reportedly increased by the following factors: advanced age, female sex, fracture displacement, and comminution [2, 15]. However, initial displacement of the fracture is apparently the most accurate predictor of outcome, with shortening of more than 2 cm leading to a poor functional outcome [2, 7, 10, 11, 14]. Traditional indications for acute surgical fixation include open fracture, neurovascular compromise, skin tenting, impending open fracture, and severe displacement. These criteria do not take into consideration patient satisfaction, cosmetic considerations, return to previous level of function, and pain. McKee et al. [11] demonstrated surgeon-based methods of evaluating shoulder strength and endurance are not sensitive enough to detect residual deficits in patients treated nonoperatively.
The Rockwood Clavicle Pin (RCP) (DePuy Orthopaedics Inc, Warsaw, IN) is a modified Hagie pin developed by Dr. C. A. Rockwood in 1975. Boehme et al. [1] described utilizing the RCP and autologous bone grafting to achieve union in 20 of 21 patients with persistent nonunions of the clavicle shaft. Although the RCP “does not provide rigid fixation or control rotational forces” [1], they concluded the RCP provided advantages over standard plate fixation. One major drawback of the RCP is the mandatory removal of the implant.
Two small case series report on patients treated with the RCP [1, 20]. Strauss et al. [20] reported a high rate of complications with the RCP, with eight complications occurring in 16 patients. Boehme et al. [1] achieved union in 20 of 21 patients with persistent nonunions of the clavicle shaft with the RCP. These studies [1, 20] have shown contradictory results and no clear consensus can be drawn from this scant body of literature. Our case series provides additional information on the complication rates associated with the use of the RCP in midshaft clavicle fractures.
Therefore, we retrospectively analyzed the complication rate of patients after treatment with the RCP and specifically addressed the following questions: (1) Does the use of the RCP result in an unacceptably high rate of soft tissue complications? (2) Does the RCP provide stable fracture fixation in minimally comminuted midshaft clavicle fractures?
Patients and Methods
Eighteen patients were identified as having undergone open reduction and fixation of a midshaft clavicle fracture using the RCP between 2004 through 2007 (Table 1). The RCP is a modified Hagie pin with course threads on the medial tip and fine threads on the lateral tip to accommodate a locking nut, securing the pin on the posterior lateral cortex of the clavicle. During this 3-year period, 50 acute midshaft clavicle fractures were treated: 28 were treated nonoperatively (56%), 18 received a RCP (36%), and four underwent plate fixation (8%). Patients with minimal to moderate displacement were treated nonoperatively. The indications for fixation with the RCP included (1) complete lack of cortical apposition with minimal comminution, (2) one large butterfly fragment, or (3) estimated shortening of at least 2 cm. Fractures with substantial comminution were treated primarily with plate fixation. There were 14 men and four women. The mean patient age was 31 years (range, 18–47 years). The affected clavicle was divided equally with nine fractures each of the right and left sides. Mechanisms of injury included motor vehicle collision (four), athletic activity (three), fall (three), motorcycle crash (two), all-terrain vehicle crash (two), bicycle accident (two), and skiing accident (two). All fractures were closed and no patients suffered neurovascular injuries. The fractures were classified by the Orthopaedic Trauma Association (OTA) system [5] as four OTA 15-B1 and 14 OTA 15-B2. Only two cases were associated with additional injuries: Patient 4 fractured the contralateral distal radius and scaphoid in an all-terrain vehicle accident and Patient 8 suffered a contralateral elbow dislocation in a motor vehicle collision. None of the patients had any serious medical comorbidities before injury.
Table 1.
Patient characteristics
| Patient | Sex | Age (years) | Mechanism of injury | Side of injury | Associated injuries | OTA grade | Time to surgery (days) | Bone graft placement | Cerclage of fragment | Time to pin removal (weeks) | Tobacco use |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Female | 18 | Athletics | Right | None | 15-B1 | 6 | No | − | 5 | − |
| 2 | Male | 21 | Athletics | Right | None | 15-B2 | 18 | DBM | + | 9 | − |
| 3 | Male | 22 | Motorcycle | Right | None | 15-B2 | 3 | No | + | 10 | + |
| 4 | Male | 24 | All-terrain vehicle | Right | Left distal radius and scaphoid fracture | 15-B1 | 11 | No | − | 7 | − |
| 5 | Male | 27 | Automobile | Left | None | 15-B1 | 55 | No | + | 18 | − |
| 6 | Male | 27 | All-terrain vehicle | Left | None | 15-B2 | 17 | DBM | + | 11 | + |
| 7 | Male | 28 | Fall | Left | None | 15-B2 | 3 | DBM | − | 9 | + |
| 8 | Male | 29 | Automobile | Left | Right elbow dislocation | 15-B2 | 38 | No | − | 12 | − |
| 9 | Male | 30 | Athletics | Left | None | 15-B2 | 7 | DBM, PDGF | + | 17 | − |
| 10 | Male | 32 | Fall | Left | None | 15-B2 | 9 | DBM | + | 18 | − |
| 11 | Male | 32 | Bicycle | Right | None | 15-B2 | 3 | DBM | + | 8 | − |
| 12 | Female | 32 | Bicycle | Left | None | 15-B1 | 3 | DBM | + | 11 | − |
| 13 | Male | 32 | Motorcycle | Right | None | 15-B2 | 11 | DBM | − | 10 | − |
| 14 | Female | 33 | Automobile | Left | None | 15-B2 | 16 | BMP | + | 18 | − |
| 15 | Male | 41 | Fall | Right | None | 15-B2 | 4 | No | − | 8 | + |
| 16 | Male | 44 | Skiing | Right | None | 15-B2 | 24 | No | − | 8 | − |
| 17 | Male | 47 | Skiing | Left | None | 15-B2 | 7 | No | + | 11 | − |
| 18 | Female | 47 | Automobile | Right | None | 15-B2 | 19 | DBM | + | 11 | − |
OTA = Orthopaedic Trauma Association; DBM = demineralized bone matrix; BMP = bone morphogenetic protein; PDGF = platelet-derived growth factor.
The mean time from injury to surgery was 14.1 days (range, 3–55 days). Two patients underwent delayed primary fixation due to persistent pain and no evidence of radiographic healing. The patient population in this study is derived from a suburban private practice sports medicine group with high rates of patient compliance and access to physical therapy. The minimum followup was 4 months (mean, 6 months; range, 4–12 months). No patients were lost to followup. No patients were recalled specifically for this study; all data were obtained from medical records and radiographs. We had prior Institutional Review Board approval.
All patients were seen on an outpatient basis and scheduled for surgery electively. All surgical procedures were performed by one of three orthopaedic surgeons (LBG, GAP, MDM) with specific interest in shoulder surgery. The surgical procedure utilized has previously been described by Boehme et al. [1].
At the surgeon’s discretion in 11 patients, the butterfly fragment was reduced and secured with FiberWire® (Arthrex, Inc, Naples, FL) cerclage, and demineralized bone matrix (DBM) was used to fill substantial fracture voids. The periosteum and platysma were then repaired before skin closure. Ten patients underwent biologic augmentation of the fracture at the initial surgery: eight received DBM, one received bone morphogenetic protein paste, and one had both DBM and autologous platelet-derived growth factor placed in the fracture. The decision to use DBM was made by the attending surgeon based upon the degree of comminution. Autologous bone grafting was not utilized due to the increased morbidity of the harvesting procedure.
Postoperatively, the patients were placed into a sling and discharged to home on the same day. Patients were instructed to remain in a sling for 2 weeks postoperatively. After 2 weeks, physical therapy was started and patients were allowed to perform activities below shoulder level with less than 5 pounds until Week 6. After 6 weeks, patients were permitted activity above shoulder level and weightbearing activities were progressed as tolerated by the patient.
Patients were routinely seen in the clinic at 2, 4, 6, 9, and 12 weeks postoperatively. At each clinic visit, AP and cephalic tilt radiographs were obtained of the injured clavicle. Patients were followed longer if complications arose or union was not achieved. After the fracture was healed clinically and radiographically, the pin was removed in a second surgical procedure. For clinical purposes, union was defined as lack of tenderness to palpation of the fracture site. Radiographic union was defined as bridging callus on both radiographic views. Patients were seen 2 weeks after RCP removal to evaluate the incision and confirm fracture stability clinically and radiographically (ie, no change in clavicle length). Patients were allowed to follow up as needed if the following criteria were met: radiographic stability, absence of pain, and full active ROM. Time to removal of the RCP was dictated by both fracture healing and the patient’s ability to tolerate any complications secondary to the RCP.
From the medical records, we recorded the mechanism of injury, age, sex, time from injury to surgery, associated injuries, medical history, tobacco use, wound condition, pain at the fracture site, and time to pin removal. Specific attention was paid to the occurrence of soft tissue and fracture-healing complications. These included persistent pain at the insertion site, skin breakdown, infection, and persistent nonunion.
Two of us (CDM, KJQ) independently reviewed all radiographs. The radiographs were assessed for final union of fracture after the removal of the RCP. Radiographic union was defined as bridging bone on two or more cortices on orthogonal views, and trabeculae crossing the fracture site [4].
Descriptive statistics were utilized to analyze ultimate fracture union, time to pin removal, and incidence of soft tissue and osseous complications.
Results
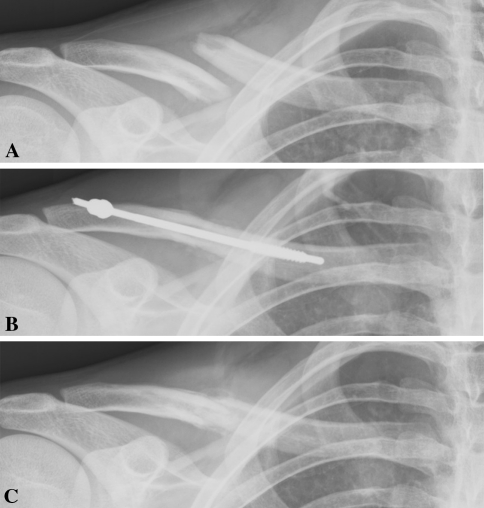
Overall, 14 complications occurred in 10 patients (Table 2). Nine patients sustained a soft tissue-related complication. Two patients required antibiotic treatment for infection. One patient required multiple irrigations and débridements for a deep Staphylococcus aureus infection, with revision to plate fixation and ultimate healing at 22 weeks. Six patients experienced posterior pain or skin necrosis requiring premature removal of the implant (Fig. 1).
Table 2.
Soft tissue and osseous complications
| Patient | Age (years) | Sex | Soft tissue complications | Osseous complications |
|---|---|---|---|---|
| 1 | 18 | Female | Posterior skin necrosis requiring operative débridement | None |
| 2 | 21 | Male | Posterior pin prominence with pain, transient axillary sensory neuropathy | None |
| 3 | 22 | Male | Posterior pain necessitating premature pin removal | Secondary alteration in reduction after pin removal |
| 4 | 24 | Male | None | None |
| 5 | 27 | Male | None | None |
| 6 | 27 | Male | None | None |
| 7 | 28 | Male | None | Atrophic nonunion, posterior pin migration with loss of reduction, reoperation with bone grafting and PDGF |
| 8 | 29 | Male | None | None |
| 9 | 30 | Male | None | None |
| 10 | 32 | Male | Anterior medial skin necrosis | Medial pin migration, reoperation, chronic fibrous nonunion |
| 11 | 32 | Male | Posterior skin necrosis with exposed pin requiring débridement | Secondary alteration in reduction after pin removal |
| 12 | 32 | Female | Anterior wound infection requiring premature pin removal | Secondary alteration in reduction after pin removal |
| 13 | 32 | Male | None | None |
| 14 | 33 | Female | Posterior pain | Delayed union |
| 15 | 41 | Male | Staphylococcus aureus wound infection requiring premature pin removal | Secondary alteration in reduction after pin removal, infected nonunion, ORIF × 2 |
| 16 | 44 | Male | Posterior pain necessitating premature pin removal | None |
| 17 | 47 | Male | None | None |
| 18 | 47 | Female | None | None |
PDGF = platelet-derived growth factor; ORIF = open reduction and internal fixation.
Fig. 1A–C.
Images illustrate the case of Patient 1, an 18-year-old woman injured while playing softball. (A) A preoperative radiograph shows a displaced midshaft clavicle fracture. (B) A postoperative radiograph shows reduction with RCP application. (C) Despite undergoing posterior skin débridement, the overall alignment of the fracture is excellent after pin removal at 5 weeks.
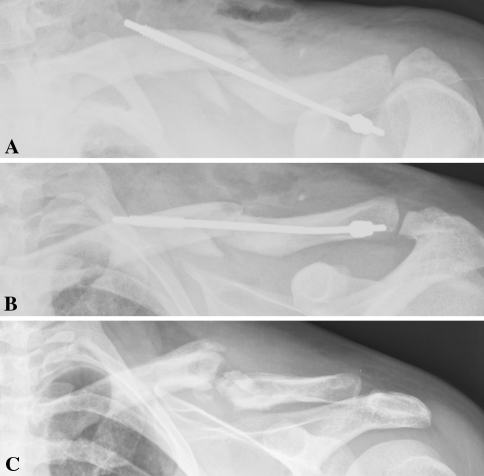
Five patients experienced a complication directly related to fracture healing. Ultimately, 16 patients achieved union after implantation of the RCP. Three nonunions (one infected, one atrophic, one persistent fibrous) and one delayed union occurred. The delayed union (Patient 14) united with the use of an electronic bone stimulator. Both the infected and atrophic nonunions required revision surgery to achieve fracture union. Patient 10 developed medial migration of the pin immediately postoperatively with loss of fracture reduction. He returned to the operating room on the following day for removal of the pin, rereduction, and insertion of a second RCP leading to a persistent fibrous nonunion (Fig. 2).
Fig. 2A–C.
Images illustrate the case of Patient 10, a 32-year-old man injured due to a fall. (A) A postoperative radiograph demonstrates medial pin migration with loss of posterior lateral fixation. (B) A radiograph is shown after immediate removal of the migrated pin with reapplication of the RCP. (C) This patient subsequently developed a chronic fibrous nonunion 8 months postoperatively.
We routinely removed the RCP in all patients at a mean of 11 weeks (range, 7–18 weeks). Four patients had radiographic changes of fracture shortening of 4 to 7 mm after premature removal (5 to 11 weeks) of the RCP due to soft tissue complications (Fig. 3).
Fig. 3A–D.
Images illustrate the case of Patient 15, a 41-year-old man injured due to a fall. (A) A postoperative radiograph demonstrates RCP placement. (B) Premature removal of the pin after 7 weeks due to posterior necrosis allowed the fracture to displace. (C) This necessitated open reduction and internal fixation with a reconstruction plate at 10 weeks, which subsequently failed due to Staphylococcus aureus infection. (D) Reapplication of a precontoured clavicle plate after multiple débridements promoted healing at 22 weeks.
Discussion
The orthopaedic community has recently begun to more closely evaluate the functional disability caused by clavicle fractures. Current publications suggest nonunion of the clavicle and functional disability caused by displaced midshaft clavicle fractures are more common problems than once thought [2, 7, 9–11, 17]. These new data have encouraged surgeons to expand the relative indications for operative fixation of clavicle fractures to include athletes and active patients with displaced or shortened diaphyseal clavicle fractures. The RCP was developed with the intention of providing a less invasive alternative to plate fixation. However, we noted a high rate of complications in patients treated with the RCP. Due to the paucity of published data on the RCP, we sought answers to the following questions: (1) Does the RCP cause an unacceptably high rate of soft tissue complications? (2) Does the RCP provide stable fracture fixation in minimally comminuted midshaft clavicle fractures?
There are several limitations to this study. First, this study has a small patient population. However, the published data on the RCP involve only small case series, ranging from 16 to 21 patients [1, 20]. Second, the retrospective nature of this study did not provide standardization of protocol and functional outcome data collection. Third, the lack of clearly defined indications for the use of DBM and FiberWire® cerclage augmentation may have influenced the biology of fracture healing. A major flaw of the RCP is the inability to allow for lag fixation of a free butterfly fragment. The application of a cerclage may improve fracture reduction and increase stability. However, this practice could potentially strangulate the periosteum. Fourth, the application of DBM into the fracture is also a potentially confounding factor in fracture healing. Finally, the lack of a control group for comparison of an alternative method of treatment does not allow us to establish superiority or inferiority compared to other methods.
The interval from injury to surgery in our patient population was 14.1 days. This interval was increased due to several patients who initially elected nonoperative treatment and later desired to undergo operative fixation. Neither of the two patients with delayed primary fixation developed a nonunion.
The high number of soft tissue complications that occurred in our series deserves careful consideration. Six patients consistently complained of pain from the posterior locking nut. The subcutaneous position of the RCP contributed to the overlying skin necrosis in several patients. Skin breakdown over an implant is clearly a concern for bacterial seeding of the implant. Two patients in our series developed a documented infection and two others required skin débridement and closure with premature removal of the RCP due to necrosis. The results of similar series have largely agreed with those seen on our study. In a series similar to ours, Strauss et al. [20] reported a high rate of complications with the RCP. Eight complications occurred in 16 patients: three cases of posterior skin breakdown due to prominent hardware, two cases of hardware breakage, two cases of decreased sensation over insertion site, and one case of persistent pain. Grassi et al. [6] compared nonoperative treatment to open intramedullary fixation of midclavicular fractures and concluded nonoperative treatment was superior due to the much lower complication rate. The intramedullary fixation group experienced eight superficial infections, three refractures, two delayed unions with pin breakage, and two nonunions. Jubel et al. [8] reported one nonunion and no infections or pin migrations in 58 fractures treated with a medially inserted flexible titanium nail. The medial starting point they used appeared to decrease the incidence of implant prominence and skin breakdown. Thus, the ability of the soft tissues to tolerate the RCP for the duration of fracture healing must be considered when selecting this implant for fracture fixation.
In addition to a high rate of soft tissue complications, four patients experienced complications directly related to fracture healing. Three nonunions and one delayed union occurred. The delayed union healed with the use of a bone stimulator and two of the nonunions ultimately united with revision surgery. Four patients (Patients 3, 11, 12, 15) demonstrated radiographic alterations in fracture alignment secondary to premature implant removal due to either infection or soft tissue irritation. The inherent biomechanical stability of the RCP is another consideration in the potential development of nonunion. The RCP serves as an internal splint with load-sharing properties. The inability of the RCP to provide stabilized compression is another factor potentially leading to the generation of a nonunion. Renfree et al. [16] conducted a biomechanical study with synthetic clavicle bones comparing precontoured clavicle plates against the RCP. The results demonstrated the RCP group was unable to resist small torque associated with off-axis loading, failed at a lower maximum load, and was less stiff than the plate group. They concluded the RCP is inadequate in situations where rotational stiffness is required.
Additionally, patients must be rehabilitated in a more cautious manner than with plate fixation. Boehme et al. [1] describes limiting the ROM to less than 90° of forward flexion in the early postoperative period. The technical application of the pin by the surgeon plays a vital role in the overall stability of the fracture. Although the RCP was developed as a less invasive alternative, the technique of open intramedullary nailing through the fracture site appears more detrimental to the soft tissue envelope than plate application.
Although the RCP provides an alternative to plate fixation of displaced midshaft clavicle fractures, our case series of 18 patients yielded 14 complications, including three nonunions (one persistent) and one delayed union. Due to the excessive soft tissue- and fracture-related complications, the use of the RCP cannot be recommended for the treatment of midshaft clavicle fractures.
Acknowledgments
The authors thank George A. Paletta, MD, and Mark D. Miller, MD, for the contribution of clinical data.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at The Orthopedic Center of Saint Louis and Des Peres Hospital Saint Louis.
References
- 1.Boehme D, Curtis RJ, Jr, DeHaan JT, Kay SP, Young DC, Rockwood CA., Jr Non-union of fractures of the mid-shaft of the clavicle: treatment with a modified Hagie intramedullary pin and autogenous bone grafting. J Bone Joint Surg Am. 1991;73:1219–1226. [PubMed] [Google Scholar]
- 2.Brinker MR, Edwards TB, O’Connor DP. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Joint Surg Am. 2005;87:676–677. doi: 10.2106/00004623-200503000-00034. [DOI] [PubMed] [Google Scholar]
- 3.Canadian Orthopaedic Trauma Society Nonoperative treatment compared with plate fixation of displaced midshaft clavicle fractures: a multicenter, randomized clinical trial. J Bone Joint Surg Am. 2007;89:1–10. doi: 10.2106/JBJS.F.00020. [DOI] [PubMed] [Google Scholar]
- 4.Corrales LA, Morshed S, Bhandari M. Variability in the assessment of fracture-healing in orthopaedic trauma studies. J Bone Joint Surg Am. 2008;90:1862–1868. doi: 10.2106/JBJS.G.01580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fracture and Dislocation Compendium: Orthopaedic Trauma Association for Coding and Classification. J Orthop Trauma. 1996:(10 Suppl 1):v–ix,1–154. [PubMed]
- 6.Grassi FA, Tajana MS, D’Angelo F. Management of midclavicular fractures: comparison between nonoperative treatment and open intramedullary fixation in 80 patients. J Trauma. 2001;50:1096–1100. doi: 10.1097/00005373-200106000-00019. [DOI] [PubMed] [Google Scholar]
- 7.Hill JM, McGwire MH, Crosby LA. Closed treatment of displaced middle-third clavicle fractures gives poor results. J Bone Joint Surg Br. 1997;79:537–539. doi: 10.1302/0301-620X.79B4.7529. [DOI] [PubMed] [Google Scholar]
- 8.Jubel A, Andermahr J, Bergmann H, Prokop A, Rehm KE. Elastic stable intramedullary nailing of midclavicular fractures in athletes. Br J Sports Med. 2003;37:480–484. doi: 10.1136/bjsm.37.6.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jupiter JB, Leffert RD. Non-unions of the clavicle. J Bone Joint Surg Am. 1987;69:753–760. [PubMed] [Google Scholar]
- 10.Lazarides S, Zafiropoulos G, Tydfil M. Conservative treatment of fractures of the middle third of the clavicle: the relevance of shortening and clinical outcome. J Shoulder Elbow Surg. 2006;15:191–194. doi: 10.1016/j.jse.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 11.McKee MD, Pedersen EM, Jones C, Stephen DJ, Kreder HJ, Schemitsch EH, Wild LM, Potter J. Deficits following nonoperative treatment of displaced midshaft clavicular fractures. J Bone Joint Surg Am. 2006;88:35–40. doi: 10.2106/JBJS.D.02795. [DOI] [PubMed] [Google Scholar]
- 12.Neer CS., 2nd Nonunion of the clavicle. J Am Med Assoc. 1960;172:1006–1011. doi: 10.1001/jama.1960.03020100014003. [DOI] [PubMed] [Google Scholar]
- 13.Nordqvist A, Peterson C. The incidence of fractures of the clavicle. Clin Orthop Relat Res. 1994;300:127–132. [PubMed] [Google Scholar]
- 14.Nowak J, Mallmin H, Larsson S. The aetiology and epidemiology of clavicular fractures: a prospective study during a two-year period in Uppsala, Sweden. Injury. 2000;31:353–358. doi: 10.1016/S0020-1383(99)00312-5. [DOI] [PubMed] [Google Scholar]
- 15.Postacchini F, Gumina S, Santis P, Albo F. Epidemiology of clavicle fractures. J Shoulder Elbow Surg. 2002;11:452–456. doi: 10.1067/mse.2002.126613. [DOI] [PubMed] [Google Scholar]
- 16.Renfree T, Conrad B, Wright T. Biomechanical comparison of contemporary clavicle fixation devices. J Hand Surg Am. 2010;35:639–644. doi: 10.1016/j.jhsa.2009.12.012. [DOI] [PubMed] [Google Scholar]
- 17.Robinson CM, Court-Brown CM, McQueen MM, Wakefield AE. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Joint Surg Am. 2004;86:1359–1365. doi: 10.2106/00004623-200407000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Rowe CR. An atlas of anatomy and treatment of midclavicular fractures. Clin Orthop Relat Res. 1968;58:29–42. doi: 10.1097/00003086-196805000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Sankarankutty M, Turner BW. Fractures of the clavicle. Injury. 1975;7:101–106. doi: 10.1016/0020-1383(75)90006-6. [DOI] [PubMed] [Google Scholar]
- 20.Strauss EJ, Egol KA, France MA, Koval KJ, Zuckerman JD. Complications of intramedullary Hagie pin fixation for acute midshaft clavicle fractures. J Shoulder Elbow Surg. 2007;16:280–284. doi: 10.1016/j.jse.2006.08.012. [DOI] [PubMed] [Google Scholar]