Abstract
Six prospective, controlled trials have examined the effects of antiepileptic drugs (AEDs) given to prevent the occurrence of seizures following neurosurgery. Some studies have concentrated on specific reasons for the neurosurgery (brain tumor) while others have included people with a variety of indications for surgery. Phenytoin (PHT) has been studied most, but carbamazepine (CBZ) and phenobarbital (PB) have also been evaluated to some extent. Studies of people with traumatic brain injury (some of whom were operated on) provide some, but less direct, evidence of the prophylactic effects of AEDs after neurosurgery. Despite considerable variation in reasons for the neurosurgery, AEDs given, and study design, the overall conclusions are remarkably consistent. The seizure risk is reduced about 40%–50% for the first week after neurosurgery in those given the older AEDs compared with those given placebo or no treatment. After the first few weeks, none of the drugs has been proven to reduce the incidence of seizures and in most situations the best estimate is essentially no effect, but effects on the order of a 25%–50% reduction in late (epileptic) seizures cannot be ruled out. The new generation of AEDs have not been tested as prophylactic agents after neurosurgery. Although there are no guidelines for prophylaxis following neurosurgery in general, these results are consistent with the guidelines of professional organizations for subsets of neurosurgery cases. Those guidelines consider prophylaxis, especially using PHT, to be an option for the first week after surgery but that the routine use of prophylactic anticonvulsants after the first week is not warranted.
Introduction: The Need for Prophylaxis and the Studies Conducted
Craniotomies, especially supratentorial ones, are associated with a high risk of subsequent seizures. Depending on the reason for the surgery, about 20%–50% of patients have at least one seizure post-operatively(1,2). Several groups have evaluated whether prophylactic administration of antiepileptic drugs (AEDs) can reduce this high seizure rate. The strongest evidence comes from randomized clinical trials. Six prospective, controlled trials have been reported, two restricted to patients operated on for brain tumors 3, 4 and four including patients operated on for a variety of conditions 1, 2, 5, 6, 7. Phenytoin (PHT) has been evaluated most extensively; carbamazepine (CBZ), valproate (VPA), and phenobarbital (PB) have also been tested. Two of the studies 3, 6 considered only seizures occurring during the first week after surgery (early seizures, generally considered to be provoked), while the others considered both early and late seizures (after one week, generally considered to be unprovoked or epileptic seizures). Five of these studies have been included in meta-analyses 8, 9.
Additionally, studies looking at seizure prevention following traumatic brain injury include many patients who received a craniotomy as part of the treatment for their injuries. These studies provide some, less direct information about the effect of prophylactic AEDs after craniotomy. These studies have also been included in meta-analyses 9, 10.
Effect of Prophylactic AEDs on Early Seizures or the Combination of Early and Late Seizures
Overall, the five studies that evaluate the effect of PHT on preventing or suppressing early seizures indicate that PHT decreases the risk of seizures in the first week by 44%[95% CI (confidence interval): 16% reduction to 62% reduction]. This is based on the combined evidence from the five studies. Figure 1 depicts the estimates from the individual studies as well as their combination. Surprisingly, the masked, placebo controlled studies 1, 6, which are least likely to be affected by bias, showed the largest effects. Also surprisingly, the studies that showed the least effect started the assigned AED preoperatively 2, 4, 5 or intraoperatively 3, in addition to being unmasked. The traumatic brain injury studies are consistent with these craniotomy results—after traumatic brain injury, PHT decreased the rate of early seizures (best estimate: 67% reduction, 95% CI: 41% reduction to 81% reduction) 9.
FIGURE 1.
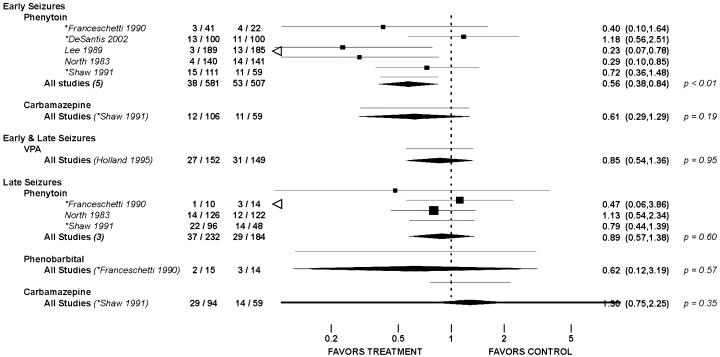
Meta-analysis results for seizure prophylaxis clinical trials following craniotomy. The relative risk for each study is marked by a square on a line that indicates the 95% confidence interval (CI) for that relative risk. Meta-analysis results for a time period and drug are marked by a diamond with the center at the overall relative risk estimate and the points extending to the ends of the 95% CI. The author's name is preceded by an asterisk (*) if the study did not use a placebo control. The seizure rate for the active treatment and control arms, the relative risk estimate and its confidence interval, and, for the meta-analyses the p-value, accompany each study or combination of studies. A relative risk of one, representing no treatment effect, is marked by the dashed vertical line. Adapted from Temkin NR. Antiepileptogenesis and seizure prevention trials with antiepileptic drugs: Meta-analysis of controlled trials. Epilepsia 2001;42:515–524, 2001 with permission of Blackwell Publishing, Inc.
Only a single study 2, 5 evaluated the effect of CBZ on early seizures following craniotomy. The best estimate is that CBZ is associated with a 39% reduction in early seizures, but that reduction is not statistically significant (95% CI: 71% reduction to 29% increase). The single study of CBZ following traumatic brain injury 11 found a significant 61% reduction in early seizures (95% CI: 18% reduction to 83% reduction). PB was evaluated in one study 4, but only the combined results for the PHT and PB arms were given. The results from both treatments are included in the PHT analysis above. The effect of valproate (VPA) on seizures after craniotomy was investigated in one study 7. The results presented early and late seizures combined and showed a nonsignificant 15% reduction with VPA (95% CI: 46% reduction to 36% increase).
Effect of Prophylactic AEDs on Late Seizures
Three studies assessed the effect of PHT on the prevention or suppression of late or epileptic seizures. Overall, the best estimate is that PHT following craniotomy is associated with a nonsignificant 11% reduction in epileptic seizures (95% CI: 43% reduction to 38% increase. Fig. 1). This is consistent with the results for traumatic brain injury 9, where the best overall estimate is a 30% reduction (95% CI: 67% reduction to 50% increase). The traumatic brain injury studies show significant variation in the results among studies, with one unmasked study having substantially more favorable results than the masked studies.
The single study 2, 5 looking at CBZ to prevent or suppress epileptic seizure after craniotomy found CBZ associated with a nonsignificant 30% increase in late seizures (95% CI: 25% reduction to 125% increase). The study of CBZ following traumatic brain injury 11 showed a compatible nonsignificant 20% reduction in seizures (95% CI: 58% reduction to 49% increase). PB was assessed in a single small study 4 of craniotomy for supratentorial brain tumors. The best estimate is that PB is associated with a nonsignificant 38% reduction in post-operative epileptic seizures (95% CI: 88% reduction to 219% increase). Traumatic brain injury studies 9 showed essentially no effect (best estimate: 2% reduction, 95% CI: 52% reduction to 104% increase).
Summary of Findings
Despite considerable variation in reasons for the neurosurgery, AEDs given, and study design, the overall conclusions are remarkably consistent. The seizure risk is reduced about 40%–50% for the first week after neurosurgery in those given the older AEDs compared to those given placebo or no treatment. After the first few weeks none of the drugs has been proven to reduce the incidence of seizures and in most situations the best estimate is essentially no effect, but effects on the order of a 25%–50% reduction in late (epileptic) seizures cannot be ruled out.
Future Research Directions
Only PHT has been reasonably well-studied. CBZ, PB, and VPA have each been assessed in one clinical trial after craniotomy and do not look especially encouraging, especially for prophylaxis of late seizures. Newer AEDs have not been evaluated at all, despite encouraging suggestions on some from preclinical work. Another important question is whether there are differences in specific subgroups of patients with respect to the need for or effectiveness of seizure prophylaxis. Subgroups based on the type of surgery as well as the location and reason for neurosurgery should be considered.
Implications for Practice
There are no formal guidelines for seizure prophylaxis after neurosurgery in general. The Brain Trauma Foundation, American Association of Neurological Surgeons, Joints Section on Neurotrauma and Critical Care, have guidelines 12 on the role of seizure prophylaxis following head injury (traumatic brain injury). They include a treatment option of giving PHT or CBZ to prevent seizures in high risk patients during the first week after injury. They have a standard that routine use of anticonvulsants later than 1 week following head injury is not recommended for preventing late posttraumatic seizures. The American Academy of Neurology has a practice parameter 13 on anticonvulsant prophylaxis in patients with newly diagnosed brain tumors. Their standard is that prophylactic anticonvulsants should not be used routinely in patients with newly-diagnosed brain tumors. Their guideline that tapering and discontinuing anticonvulsants after the first postoperative week is appropriate in patients who have not had a seizure. The studies reviewed here on prophylaxis for seizures following neurosurgery are consistent with the above guidelines and suggest similar practices are appropriate for seizure prophylaxis after supratentorial craniotomy for a variety of reasons.
Acknowledgment
This work was supported by NIH/NINDS grant R01 NS 19643.
References
- 1.North JB, Penhall RK, Hanieh A, Frewin DB, Taylor WB. Phenytoin and postoperative epilepsy: A double-blind study. J Neurosurg 1983;58: 672–677. [DOI] [PubMed] [Google Scholar]
- 2.Shaw MD, Foy PM. Epilepsy after craniotomy and the place of prophylactic anticonvulsant drugs: discussion paper. J R Soc Med 1991;84: 221–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.De Santis A, Villani R, Sinisi M, Stocchetti N, Perucca E. Add-on phenytoin fails to prevent early seizures after surgery for supratentorial brain tumors: a randomized controlled study. Epilepsia 2002;43: 175–182. 10.1046/j.1528-1157.2002.24801.x [DOI] [PubMed] [Google Scholar]
- 4.Franceschetti S, Binelli S, Casazza M, Lodrini S, Panzica F, Pluchino F, Solero CL, Avanzini G. Influence of surgery and antiepileptic drugs on seizures symptomatic of cerebral tumours. Acta Neurochir 1990;103: 47–51. [DOI] [PubMed] [Google Scholar]
- 5.Foy P, Chadwick D, Rajgopalan N, Johnson A, Shaw M. Do prophylactic anticonvulsant drugs alter the pattern of seizures after craniotomy? J Neurol Neurosurg Psychiatry 1992;55: 753–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee ST, Lui TN, Chang CN, Cheng WC, Wang DJ, Heimburger RF, Lin CG. Prophylactic anticonvulsants for prevention of immediate and early postcraniotomy seizures. Surg Neurol 1989;31: 361–364. [DOI] [PubMed] [Google Scholar]
- 7.Holland JP, Stapleton SR, Moore AJ, Marsh HT, Uttley D, Bell BA. A randomized double blind study of sodium valproate for the prevention of seizures in neurosurgical patients. J Neurol Neurosurg Psychiatry 1995;58: 116. [Google Scholar]
- 8.Kuijlen JM, Teernstra OP, Kessels AG, Herpers MJ, Beuls EA. Effectiveness of antiepileptic prophylaxis used with supratentorial craniotomies: a meta-analysis. Seizure 1996;5: 291–298. [DOI] [PubMed] [Google Scholar]
- 9.Temkin NR. Antiepileptogenesis and seizure prevention trials with antiepileptic drugs: meta-analysis of controlled trials. Epilepsia 2001;42: 515–524. 10.1046/j.1528-1157.2001.28900.x [DOI] [PubMed] [Google Scholar]
- 10.Schierhout G, Roberts I. Prophylactic antiepileptic agents after head injury: a systematic review. J Neurol Neurosurg Psychiatry 1998;64: 108–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Glötzner FL, Haubitz I, Miltner F, Kapp G, Pflughaupt KW. Anfallsprophylaxe mit Carbamazepin nach schweren Schadelhirnverletzungen. Neurochirurgia (Stuttg.) 1983;26: 66–79. [DOI] [PubMed] [Google Scholar]
- 12.The Brain Trauma Foundation. The American Association of Neurological Surgeons. The Joint Section on Neurotrauma and Critical Care. Role of antiseizure prophylaxis following head injury. J Neurotrauma 2000;17: 549–553. [DOI] [PubMed] [Google Scholar]
- 13.Glantz MJ, Cole BF, Forsyth PA, Recht LD, Wen PY, Chamberlain MC, Grossman SA, Cairncross JG. Practice parameter: anticonvulsant prophylaxis in patients with newly diagnosed brain tumors: report of the quality standards subcommittee of the American Academy of Neurology. Neurology 2000;54: 1886–1893. [DOI] [PubMed] [Google Scholar]


