Abstract
Background
The ideal management of fractures of the distal third of the clavicle remains a topic of debate. Locked plating is a new treatment method but is not yet widely studied.
Questions/purposes
We therefore determined union rates, function, and complications treated with locked plating.
Patients and Methods
We retrospectively reviewed 20 patients with Neer Type II distal clavicle fractures. All patients were treated with superior locked plating augmented with suture cerclage or screw fixation into the coracoid when there were concerns with screw purchase in the lateral fragment. Union was assessed radiographically and function was reported in terms of American Shoulder and Elbow Surgeons (ASES) scores and motion. Sixteen of 20 patients were followed for a minimum of 1 year; four of the patients with less than 1 year followup were included only for reporting of complications. The 16 patients were followed a minimum of 12 months (average, 30.7 months; range, 13–87 months).
Results
Union occurred in 15 of 16 (94%) patients. Average forward elevation and external rotation were 165.6° (range, 115°–180°) and 58.8° (range, 20°–90°), respectively. The average ASES score at the most recent followup was 79.0 (range, 33.3–100). Complications occurred in two patients. One patient developed an infected nonunion and a second patient sustained a peri-implant fracture.
Conclusions
Acute unstable distal clavicle fractures can be treated with superior locking plates with union rates, ASES scores, and ROM that are comparable to similar studies in the literature. The treatment method described allows supplemental fixation such as suture augmentation or a coracoclavicular screw.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Fractures of the distal clavicle make up approximately 21% of clavicular fractures [20]. The unique difficulties imposed by this specific fracture pattern were first described by Neer, who classified distal clavicular fractures into three types [19]. Type I is a fracture lateral to the coracoclavicular ligaments with typically minimal displacement. Type II fractures occur more medial to the coracoclavicular ligaments and often result in major displacement. In Type IIa fractures, both the conoid and trapezoid ligaments remain attached to the distal fragment. Type IIb fractures are believed to involve additional rupture of the conoid ligament, leaving the trapezoid intact (Fig. 1). Type III fractures extend intra-articularly to the acromioclavicular joint. Neer recognized that Type II distal clavicular fractures carry a higher risk of nonunion compared with other clavicular fracture types [18]. An additional classification scheme was proposed by Robinson [26] in 1998. He described distal clavicle fractures according to whether they were displaced and whether they were intra- or extra-articular. In his series, the incidence of delayed union or nonunion was 11.1% in displaced extra-articular fractures and 18.2% in displaced intra-articular fractures. Half of the nonunions were symptomatic.
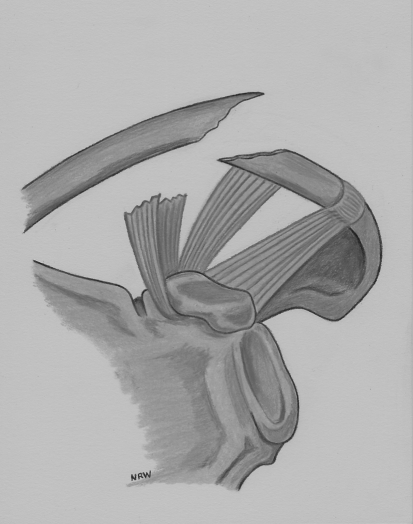
Fig. 1.
This depicts an illustration of a Neer Type IIb distal clavicle fracture showing a torn conoid ligament with an intact trapezoid ligament.
Historically, treatment of distal clavicle fractures was nonoperative, even with major fracture displacement. Displaced fractures had nonunion rates as high as 22% to 50% [21, 28, 29, 31]. A 14% rate of symptomatic nonunions [29] has led many to advocate surgical management of displaced fractures.
No consensus has been reached in the operative management of these fractures. Proposed treatments have included coracoclavicular screws [1, 17, 34], tension bands [2, 4, 13, 32], Kirschner wires [8, 16], hook plates [9, 14], and nonlocked [15] as well as locked superior plates [10, 12, 14, 22, 35]. Problems with internal fixation have included fixation failure, pin migration, fracture, nonunion, malunion, and the need to remove the hardware [3, 14, 15, 33]. There is a lack of high-quality, comparative studies to evaluate these techniques. Only a few small series exist in the literature.
Timing of fixation of these injuries is important as well. Klein et al. [14] found that delaying surgery results in a higher complication rate. There were more infections, hardware failures, and peri-implant fractures in the delayed-treatment group. In addition, the hook plate group had substantially more complications than the superior locked plating group regardless of timing. As a result, our preferred treatment for Neer II distal clavicle fractures is early (less than 6 weeks) superior locked plating. There are few published series evaluating treatment with precontoured locked plates meant specifically for the distal clavicle (Table 1), and we sought to confirm that early treatment with this method is associated with high union rates and low complications.
Table 1.
The demographics, surgical treatment, union rates, function, and complications are reported here
| Pt # | Gender | Age (years) | Locking plate (+/−) | Suture (+/−) | CC screw (+/−) | Followup (months) | Union | Complications | ROM at Latest F/U (FF/ER) | ASES score at latest F/U |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 45 | + | + | + | 13.7 | Yes | − | 115/90 | − |
| 2 | M | 58 | + | − | − | 57.0 | Yes | − | 160/45 | 100 |
| 3 | M | 53 | + | + | − | 26.8 | No | Infected nonunion | 170/60 | 41.7 |
| 4 | M | 49 | + | + | − | 21.2 | Yes | − | 160/45 | 75 |
| 5 | F | 44 | + | + | − | 20.3 | Yes | − | 160/45 | 90 |
| 6 | M | 20 | + | + | − | 3.4 | − | − | − | − |
| 7 | M | 27 | + | + | − | 39.0 | Yes | − | 180/90 | 98.3 |
| 8 | M | 39 | + | − | − | 87.0 | Yes | − | 180/90 | 100 |
| 9 | M | 23 | + | − | − | 12.8 | Yes | − | 180/70 | − |
| 10 | M | 28 | + | − | − | 47.1 | Yes | Peri-implant fracture | 170/60 | 33.3 |
| 11 | M | 53 | + | − | − | 14.5 | Yes | − | 170/60 | − |
| 12 | M | 34 | + | + | − | 84.0 | Yes | − | 170/40 | 85 |
| 13 | M | 56 | + | − | − | 13.2 | Yes | − | 140/20 | − |
| 14 | F | 57 | + | + | − | 14.2 | Yes | − | 175/45 | 85 |
| 15 | M | 66 | + | − | − | 14.0 | Yes | − | 180/60 | 73.7 |
| 16 | M | 37 | + | − | − | 13.5 | Yes | − | 180/80 | − |
| 17 | M | 16 | + | − | − | 3.2 | Yes | − | − | − |
| 18 | M | 18 | + | − | − | 3.5 | Yes | − | − | − |
| 19 | M | 62 | + | − | − | 3.6 | − | − | − | − |
| 20 | M | 61 | + | + | + | 13.0 | Yes | − | 160/40 | 86.7 |
Pt = Patient; CC = coracoclavicular; mos = months; ROM = range of motion; F/U = followup; FF = forward flexion; ER = external rotation; ASES = American Shoulder and Elbow Score; F = female; M = male.
We therefore determined (1) radiographic union rates; (2) function in terms of American Shoulder and Elbow Surgeons (ASES) scores and ROM at latest followup; and (3) complication rates.
Patients and Methods
We retrospectively reviewed 20 patients surgically treated for acute displaced fractures of the distal clavicle from 2002 to 2010. The indications for surgery were an adult patient with an acute fracture (less than 6 weeks old) of the distal clavicle consistent with Neer Type II. The contraindications for surgery were skeletal immaturity or the presence of one or more comorbidities that would elevate the risks of anesthesia and surgery. We included only patients with (1) acute surgical treatment (within 6 weeks of injury) with superior locked plating; (2) a Neer Type II fracture pattern; and (3) at least 1 year of followup. In practice, Neer Types IIa and IIb are clinically equivalent injuries [30] and it is difficult to distinguish them radiographically. Therefore, for the purposes of this study, no attempt was made to distinguish between Types IIa and IIb fractures. At the time of presentation, we obtained two orthogonal views (AP and Zanca) of the distal clavicle, which demonstrated displaced Type II fractures of the distal clavicle. Seventeen patients were males and three were females. The average time from injury to surgical fixation was 12.1 days (range, 3–36 days). Four of 20 patients were lost to followup at 3.4, 3.6, 3.2, and 3.5 months, respectively. Our attempts to call them back to clinic or obtain ASES scores over the phone were unsuccessful and we excluded from evaluation of union and function but included for reporting of complications. All data were obtained from medical records and radiographs. The average age of the 16 patients was 45.6 years (range, 23–66 years). The minimum followup for the 16 patients was 12.8 months (mean, 30.7 months; range, 12.8–87 months).
All fractures were treated by one of two attending surgeons (MM and MF) fellowship-trained in shoulder and elbow surgery. Patients were treated at one of three institutions: (1) Florida Orthopedic Institute Surgery Center; (2) Tampa General Hospital; or (3) Saint Joseph’s Hospital. All surgeries were performed in the standard beach-chair position with the bed rotated 90° relative to the anesthesiologist. Before skin preparation and draping, fluoroscopy was brought to the head of the bed and positioned so that adequate views (AP and varying degrees of caudal tilt views) of the distal clavicle could be obtained. Once this was confirmed, the fluoroscopy was temporarily removed from the field for surgical preparation.
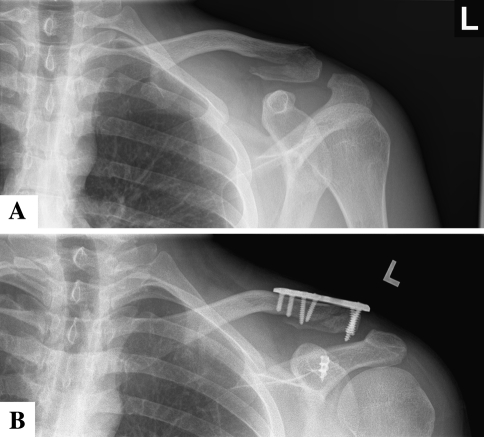
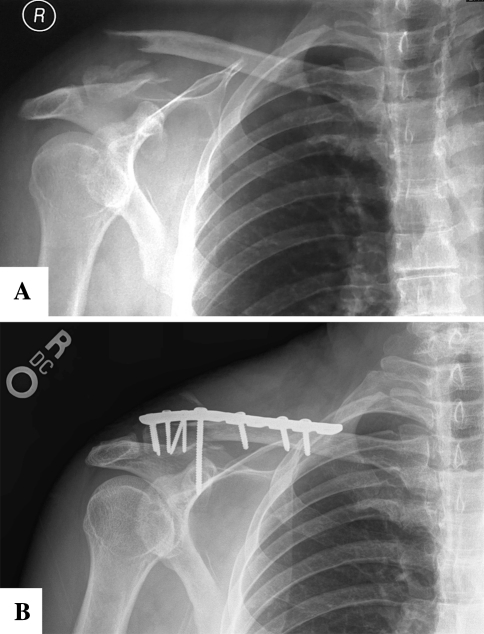
We used a standard anterosuperior approach to the clavicle. Electrocautery was used to control superficial bleeding and dissect directly to the clavicle. Care was taken to preserve the superior acromioclavicular joint ligaments. After identifying the fracture site, all hematoma and debris were curetted and removed. We then reduced the fracture reduced using a bone tenaculum. In most cases, 2.0-mm minifragment screws were used to lag the fracture fragments together. We countersunk the screws to avoid prominence and conflicts with plate positioning. In cases with considerable comminution, the fracture was reduced and held with Kirschner wires placed across the acromioclavicular joint. We directed the Kirschner wires from the smaller lateral fragment to the shaft of the clavicle. The plate was secured to the clavicle once the reduction was confirmed. Plate design has evolved to allow multiple 2.7- or 3.5-mm locking screws to be placed in a divergent pattern into the smaller lateral fragment. We filled the medial holes with both locked and nonlocked screws. The image intensifier confirmed proper hardware placement in that the plate did not cross over the acromioclavicular joint and that all screws remained extra-articular. The lateral fragment was often small and osteopenic, and the distal locking screws did not seem to achieve sufficient bony purchase. There were also times when, even after anatomic reduction and fixation with the locked plate, the acromioclavicular joint remained malreduced with the distal clavicle slightly high in relation to the acromion. When we had these concerns, we added one or more of the following techniques (Table 2) to improve fixation and maintain reduction. The first included suture augmentation with heavy nonabsorbable sutures, which were passed around the base of the coracoid and over the plate. The second technique consisted of anchor placement into the coracoid base with subsequent passing and tying of the sutures around the clavicle (Fig. 2A–B). The third technique included placing a small-fragment coracoclavicular screw and washer through the plate in nonlocking mode (Fig. 3A–B). When used, all of these additional techniques were able to provide anatomic reduction of the acromioclavicular joint. The Synthes LCP system (West Chester, PA) was used in 13 of 20 patients. The Acumed Congruent Locking System (Hillsboro, OR) was used in three of 20 and the Smith and Nephew PERI-LOC System (London, UK) in four of 20. Once we were satisfied with the reduction and hardware placement, the wound was closed in layers. Drains were not used. Average surgical time was 65 minutes (range, 45–110 minutes). Average blood loss was 100 cc (range, 50–225 cc).
Table 2.
The retrospective series that used locking plates for fixation are compared
| Author | Number of patients | Average followup | Fixation method | Union rate | Complications | Functional result | Implant removal |
|---|---|---|---|---|---|---|---|
| Klein et al. [14] | 16 | 12 months | 1. Synthes LCP (13/16) 2. Acumed precontoured (3/16) 3. Suture cerclage (16/16) |
94% | Deep infection (1) | Average ASES 77 | 5 |
| Kalamaras et al. [13] | 8 | 10–19 months | 1. Synthes distal radius volar LCP (8/8) 2. Suture cerclage (6/8) |
100% | Superficial infection (1) Malreduction (1) |
Average Constant 96 | 0 |
| Herrmann et al. [10] | 7 | 8.3 months | 3.5 mm locking T-plate with suture cerclage | 100% | None | Average Constant 93.3 Average DASH 15.3 |
2 |
| Kaipel et al. [12] | 11 | 4 months | Synthes 2.4 mm LCP (2 per patient) | 100% | Screw loosening (2) | 10/11 patients with full ROM | 3 |
| Yu et al. [35] | 6 | 2–3 months | Synthes distal radius volar LCP | 100% | NR | Constant (95–100) | NR |
| Andersen et al. (present study) | 20 | 30.7 months | Locked plates ± suture cerclage, CC screw | 94% | Infected nonunion (1) Peri-implant fracture (1) |
Average ASES 79.0 | 4 |
NR = not reported; ASES = American Shoulder and Elbow Surgeons; DASH = Disabilities of the Arm, Shoulder and Hand.
Fig. 2A–B.
(A) This is a preoperative AP radiograph of Patient 7. (B) This is a postoperative AP radiograph of the same patient treated with superior locked plating and vertical suture sling from coracoid anchors.
Fig. 3A–B.
(A) This is a preoperative AP radiograph of Patient 20. (B) This is a postoperative AP radiograph of the same patient treated with superior locked plating supplemented with a coracoclavicular screw.
We placed all patients into a shoulder sling for 4 to 6 weeks. During this time, patients were allowed to remove the sling to bathe and perform pendulum exercises as well as elbow, wrist, and hand motion. From 6 to 12 weeks, active motion of the shoulder was encouraged with no lifting unless osseous union was evident on radiographs. After 12 weeks, unrestricted use of the upper extremity was encouraged. We did not generally recommend physical therapy. Patients were allowed to return to light office work as tolerated, but manual labor was restricted until osseous union was achieved.
All patients had clinical followup and radiographs. Patients returned to the clinic after surgery at 2 weeks, 6 weeks, 12 weeks, 6 months, 1 year, and then annually thereafter. Four of 20 patients did not return after the 12-week mark. At the 6- and 12-month time points, we determined function using the ASES score [25]. Seven of 20 patients did not complete ASES forms. Attempts to obtain them over the phone were unsuccessful, leaving 11 of 20 patients with scores. ROM in two planes (forward flexion and external rotation) was recorded at the patient’s latest followup. Complications were noted. Radiographs (AP and Zanca) were obtained at each visit. Two independent observers (JA and MW) evaluated all radiographs at each time point to determine the presence or absence of radiographic union. Although two orthogonal views were obtained at all clinical followup intervals, there were frequently cases in which the plate obscured visualization of the fracture line. Therefore, radiographic union was defined by obliteration of the fracture line or bridging bone seen in at least one view [5]. Clinical union was defined as no tenderness to palpation over the fracture site [5].
Results
Osseous union was achieved in 15 of 16 (94%) patients. The mean ASES score was 79.0 (range, 33.3–100). Mean forward flexion and external rotation were 165.6° (range, 115°–180°) and 58.8° (range, 20°–90°), respectively.
Two of the 20 patients experienced complications. The first patient sustained a fracture medial to the plate and was treated nonoperatively until union at 7.0 months postfracture. The second patient was diagnosed with a deep infection 62 days after the index procedure and was subsequently treated with irrigation, débridement, and hardware removal. A symptomatic nonunion then developed and was treated with a distal clavicle excision. Four of 20 plates were removed at an average of 276 days after surgery (range, 62–425 days). Three were electively removed for hardware prominence approximately 1 year after surgery; the other removal was for the patient who developed the deep infection.
Discussion
The ideal surgical management of displaced distal clavicle fractures continues to be controversial. We sought to evaluate (1) union rates; (2) function; and (3) complications in our consecutive series of 18 patients treated with superior locked plating. Comparisons were then made to similar series in the literature (Table 1).
Our study is subject to a number of limitations. First, it was a retrospective review that lacked a control group. We attempted to mitigate this by comparing our study with similar series of a variety of surgical treatment methods (Tables 1, 3). Second, the study took place over a long time range (8 years), which resulted in variations in surgical technique. In addition, three different plate vendors were used. Although the common link between all patients was use of a superior locked plate, many had augmented fixation at the surgeons’ discretion in the form of coracoclavicular screw fixation or suturing techniques (Table 2). As discussed earlier, the decision to add fixation followed a specific thought process. However, it is difficult to interpret from this study whether the additional fixation had any added benefit to the patient. Third, four patients were excluded from the analysis of union and function as a result of inadequate followup.
Table 3.
The retrospective series that used a variety of non-plate fixation techniques are reported
| Author | Number of patients | Average followup | Fixation method | Union rate | Complications | Functional result |
|---|---|---|---|---|---|---|
| Ballmer et al. [1] | 5 | 12 months (8–21) | Coracoclavicular screw | 100% | None | 100% with full ROM |
| Bezer et al. [2] | 10 | 24 months (12–36) | 1. k-wires 2. suture anchor to coracoid |
100% | NR | Average Constant 96.6 (9 excellent, 1 good) |
| Chen et al. [4] | 11 | 18 months minimum (18–48) | 1. mersilene tape 2. primary ligament repair 3. k-wires |
100% | NR | Excellent/good in 10/11 |
| Levy et al. [16] | 12 | 2–6 years | Figure of eight sutures | 100% | None | Average Constant 97 (91–100) |
| Jou et al. [11] | 12 | 15.2 months (6–24) | Knowles intramedullary pin | 100% | Skin irritation from pin hub (3) | Average UCLA 33.9 (good) |
| Shin et al. [32] | 19 | 25 months | 1. 2 coracoclavicular anchors 2. 2 suture tension bands clavicular fragments |
1. 84% (16/19) union 2. 10% (2/19) delayed union |
Clavicular erosion (2) Malunion (1) |
Average Constant 94 |
| Robinson et al. [27] | 16 | 12 months | twin coracoid buttons with sutures around clavicle | 94% (15/16) | Capsulitis (1) Fibrous union (1) |
(1) Average Constant 87.1 (2) DASH 3.3 |
NR = not reported; ASES = American Shoulder and Elbow Surgeons; DASH = Disabilities of the Arm, Shoulder and Hand.
Klein et al. [14] described the use of precontoured plates designed specifically for the distal clavicle. Most studies reported in the peer-reviewed literature are small (Level IV) and, given the limited number of patients, the results are difficult to interpret. We reviewed several recent studies, all of which used some form of locked plating of the distal clavicle (Table 1). The study group had a high union rate (near 100% overall) and relatively few complications. Of 64 total patients, there were five reported complications, including two infections, two occurrences of screw loosening, and one malunion. Our results compare favorably with these studies in terms of union rates, function, and complications.
The management of unstable distal clavicle fractures continues to be controversial. Despite reports of nonunions in the range of 22% to 50% [21, 28, 29, 31], many surgeons are in favor of initial nonoperative management of these fractures, especially in the case of advanced age and low activity levels [6, 15, 21, 29, 31]. In patients treated nonoperatively, the incidence of symptomatic nonunions requiring surgery is reportedly as low as 14% [29]. Functional outcome is acceptable in most cases of nonunion [22]. Rokito et al. [31] found that all seven nonunions in his group were asymptomatic with normal function. Robinson and Cairns [28] demonstrated that although the large majority of patients with these fractures were middle-aged or elderly, the group of younger patients typically having surgery for symptomatic nonunion. In younger, more active patients, early surgical intervention may be beneficial because of concerns regarding high nonunion rates and inherent difficulties with delayed management [7, 18, 19]. A 14% incidence of symptomatic nonunion in an active patient population may be regarded as an unacceptable risk of nonoperative care. Several authors have observed union rates of 95% to 100% after surgical fixation [10, 12–14, 22, 35]. Although the present study did not include patients treated nonoperatively, the union rate of 94% after surgery compares favorably with prior observations. In addition, our series generally consisted of younger, more active patients who would likely benefit from surgery (average age, 45.1 years).
Several techniques other than plate fixation have been described to treat displaced distal clavicle fractures, all with varying results. These techniques include Kirschner wires [8], tension band fixation with either wires or sutures [4, 16], coracoclavicular fixation with either screws, button, or suture anchors [1, 2, 17, 27, 32], and intramedullary pin fixation [11]. Despite the numerous techniques available for distal clavicle fractures, no single one has proven superior (Table 3). Our series appears comparable with these nonplate forms of fixation.
The recent introduction of precontoured locked-plate technology has proven beneficial in treating fractures with poor bone quality as well as fractures with short metaphyseal segments [23, 24]. The use of multiple, divergent, fixed-angle screws in the distal fragment would seem to increase pullout strength, especially when the distal fragment is small and osteopenic. In addition, by avoiding the need to bridge across the clavicle to the acromion, motion at the acromioclavicular joint is preserved. In our series, using intraoperative judgment of screw purchase in the lateral fragment as well judgment of appropriate acromioclavicular joint reduction, we determined that nine of 20 patients needed some form of additional fixation. We noted the use of multiple, divergent locking screws in the distal fragment appeared to provide stable enough fixation in most cases such that additional fixation was not needed. When additional fixation was used, those patients generally did well and went on to bony union. Using this treatment strategy, we observed no cases of fixation failure or complications related to hardware as well as a high union rate (94%).
Patients with acute distal clavicle fractures managed with superior locked plating demonstrated high union rates, good function, and low complication rates. This treatment method allows for the use of supplemental fixation in the form of suture augmentation or a coracoclavicular screw when necessary.
Acknowledgments
We thank Jordan Brooks, BS, Christopher David Williams, BS, and Mark Frankle, MD, for their hard work in collecting data and evaluating radiographs.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
This work was performed at Florida Orthopaedic Institute, Temple Terrance, FL, USA.
References
- 1.Ballmer FT, Gerber C. Coracoclavicular screw fixation for unstable fractures of the distal clavicle. A report of five cases. J Bone Joint Surg Br. 1991;73:291–294. doi: 10.1302/0301-620X.73B2.2005158. [DOI] [PubMed] [Google Scholar]
- 2.Bezer M, Aydin N, Guven O. The treatment of distal clavicle fractures with coracoclavicular ligament disruption: a report of 10 cases. J Orthop Trauma. 2005;19:524–528. doi: 10.1097/01.bot.0000164593.04348.e5. [DOI] [PubMed] [Google Scholar]
- 3.Brouwer KM, Wright TC, Ring DC. Failure of superior locking clavicle plate by axial pull-out of the lateral screws: a report of four cases. J Shoulder Elbow Surg. 2009;18:e22–e25. doi: 10.1016/j.jse.2008.05.042. [DOI] [PubMed] [Google Scholar]
- 4.Chen CH, Chen WJ, Shih CH. Surgical treatment for distal clavicle fracture with coracoclavicular ligament disruption. J Trauma. 2002;52:72–78. doi: 10.1097/00005373-200201000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Corrales LA, Morshed S, Bhandari M, Miclau T., III Variability in the assessment of fracture healing in orthopedic trauma studies. J Bone Joint Surg Am. 2008;90:1862–1868. doi: 10.2106/JBJS.G.01580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Deafenbaugh MK, Dugdale TW, Staeheli JW, Nielsen R. Nonoperative treatment of Neer type II distal clavicle fractures: a prospective study. Contemp Orthop. 1990;20:405–413. [PubMed] [Google Scholar]
- 7.Edwards DJ, Kavanagh TG, Flannery MC. Fractures of the distal clavicle: a case for fixation. Injury. 1992;23:44–46. doi: 10.1016/0020-1383(92)90125-C. [DOI] [PubMed] [Google Scholar]
- 8.Goldberg JA, Bruce WJ, Sonnabend DH, Walsh WR. Type 2 fractures of the distal clavicle: a new surgical technique. J Shoulder Elbow Surg. 1997;6:380–382. doi: 10.1016/S1058-2746(97)90006-9. [DOI] [PubMed] [Google Scholar]
- 9.Haidar SG, Krishnan KM, Deshmukh SC. Hook plate fixation for type II fractures of the lateral end of the clavicle. J Shoulder Elbow Surg. 2006;15:419–423. doi: 10.1016/j.jse.2005.11.012. [DOI] [PubMed] [Google Scholar]
- 10.Herrmann S, Schmidmaier G, Greiner S. Stabilisation of vertical unstable distal clavicular fractures (Neer 2b) using locking T-plates and suture anchors. Injury. 2009;40:236–239. doi: 10.1016/j.injury.2008.07.021. [DOI] [PubMed] [Google Scholar]
- 11.Jou IM, Chiang EP, Lin CJ, Lin CL, Wang PH, Su WR. Treatment of unstable distal clavicle fractures with Knowles pin. J Shoulder Elbow Surg. 2011;20:414–419. doi: 10.1016/j.jse.2010.08.009. [DOI] [PubMed] [Google Scholar]
- 12.Kaipel M, Majewski M, Regazzoni P. Double-plate fixation in lateral clavicle fractures—a new strategy. J Trauma. 2010;69:896–900. doi: 10.1097/TA.0b013e3181bedf28. [DOI] [PubMed] [Google Scholar]
- 13.Kalamaras M, Cutbush K, Robinson M. A method for internal fixation of unstable distal clavicle fractures: early observations using a new technique. J Shoulder Elbow Surg. 2008;17:60–62. doi: 10.1016/j.jse.2007.04.012. [DOI] [PubMed] [Google Scholar]
- 14.Klein SM, Badman BL, Keating CJ, Devinney DS, Frankle MA, Mighell MA. Results of surgical treatment for unstable distal clavicular fractures. J Shoulder Elbow Surg. 2010;19:1049–1055. doi: 10.1016/j.jse.2009.11.056. [DOI] [PubMed] [Google Scholar]
- 15.Kona J, Bosse MJ, Staeheli JW, Rosseau RL. Type II distal clavicle fractures: a retrospective review of surgical treatment. J Orthop Trauma. 1990;4:115–120. doi: 10.1097/00005131-199004020-00002. [DOI] [PubMed] [Google Scholar]
- 16.Levy O. Simple, minimally invasive surgical technique for treatment of type 2 fractures of the distal clavicle. J Shoulder Elbow Surg. 2003;12:24–28. doi: 10.1067/mse.2003.128564. [DOI] [PubMed] [Google Scholar]
- 17.Macheras G, Kateros KT, Savvidou OD, Sofianos J, Fawzy EA, Papagelopoulos PJ. Coracoclavicular screw fixation for unstable distal clavicle fractures. Orthopedics. 2005;28:693–696. doi: 10.3928/0147-7447-20050701-18. [DOI] [PubMed] [Google Scholar]
- 18.Neer CS., II Fracture of the distal clavicle with detachment of the coracoclavicular ligaments in adults. J Trauma. 1963;3:99–110. doi: 10.1097/00005373-196303000-00001. [DOI] [PubMed] [Google Scholar]
- 19.Neer CS., II Fractures of the distal third of the clavicle. Clin Orthop Relat Res. 1968;58:43–50. [PubMed] [Google Scholar]
- 20.Nordqvist A, Petersson C. The incidence of fractures of the clavicle. Clin Orthop Relat Res. 1994;300:127–132. [PubMed] [Google Scholar]
- 21.Nordqvist A, Petersson C, Redlund-Johnell I. The natural course of lateral clavicle fracture. 15 (11–21) year follow-up of 110 cases. Acta Orthop Scand. 1993;64:87–91. doi: 10.3109/17453679308994539. [DOI] [PubMed] [Google Scholar]
- 22.Oh JH, Kim SH, Lee JH, Shin SH, Gong HS. Treatment of distal clavicle fracture: a systematic review of treatment modalities in 425 fractures. Arch Orthop Trauma Surg. 2010 Oct 22 [Epub ahead of print]. [DOI] [PubMed]
- 23.Perren S, Claes L. Biology and biomechanics in fracture management. In: Ruedi T, Murphy W, editors. AO Principles of Fracture Management. New York: Theime; 2000. pp. 7–31. [Google Scholar]
- 24.Renfree T, Conrad B, Wright T. Biomechanical comparison of contemporary clavicle fixation devices. J Hand Surg Am. 2010;35:639–644. doi: 10.1016/j.jhsa.2009.12.012. [DOI] [PubMed] [Google Scholar]
- 25.Richards RR, An K, Bigliani LU, Friedman RJ, Gartsman GM, Gristina AG, Iannotti JP, Mow VC, Sidles JA, Zuckerman JD. A standardized method for the assessment of Shoulder function. J Shoulder Elbow Surg. 1994;3:347–352. doi: 10.1016/S1058-2746(09)80019-0. [DOI] [PubMed] [Google Scholar]
- 26.Robinson CM. Fractures of the clavicle in the adult; Epidemiology and classification. J Bone Joint Surg Br. 1998;80:476–484. doi: 10.1302/0301-620X.80B3.8079. [DOI] [PubMed] [Google Scholar]
- 27.Robinson CM, Akhtar MA, Jenkins PJ, Sharpe T, Ray A, Olabi B. Open reduction and Endobutton fixation of displaced fractures of the lateral end of the clavicle in younger patients. J Bone Joint Surg Br. 2010;92:811–816. doi: 10.1302/0301-620X.92B6.23558. [DOI] [PubMed] [Google Scholar]
- 28.Robinson CM, Cairns DA. Primary nonoperative treatment of displaced lateral fractures of the clavicle. J Bone Joint Surg Am. 2004;86:778–782. doi: 10.2106/00004623-200404000-00016. [DOI] [PubMed] [Google Scholar]
- 29.Robinson CM, Court-Brown CM, McQueen MM, Wakefield AE. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Joint Surg Am. 2004;86:1359–1365. doi: 10.2106/00004623-200407000-00002. [DOI] [PubMed] [Google Scholar]
- 30.Rockwood CA. The Shoulder. Philadelphia: Saunders/Elsevier; 2009. [Google Scholar]
- 31.Rokito AS, Zuckerman JD, Shaari JM, Eisenberg DP, Cuomo F, Gallagher MA. A comparison of nonoperative and operative treatment of type II distal clavicle fractures. Bull Hosp Jt Dis. 2002;61:32–39. [PubMed] [Google Scholar]
- 32.Shin SJ, Roh KJ, Kim JO, Sohn HS. Treatment of unstable distal clavicle fractures using two suture anchors and suture tension bands. Injury. 2009;40:1308–1312. doi: 10.1016/j.injury.2009.03.013. [DOI] [PubMed] [Google Scholar]
- 33.Webber MC, Haines JF. The treatment of lateral clavicle fractures. Injury. 2000;31:175–179. doi: 10.1016/S0020-1383(99)00276-4. [DOI] [PubMed] [Google Scholar]
- 34.Yamaguchi H, Arakawa H, Kobayashi M. Results of the Bosworth method for unstable fractures of the distal clavicle. Int Orthop. 1998;22:366–368. doi: 10.1007/s002640050279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yu C, Sun YH, Zhao CQ, Shi DW, Wang Y. Treatment of distal clavicle fracture with distal radius volar locking compression plate. Chin J Traumatol. 2009;12:299–301. [PubMed] [Google Scholar]