Abstract
Pulmonary rehabilitation is effective for improving exercise capacity in patients with interstitial lung disease (ILD), and most programs last about 8 weeks. A 43-year-old male patient with systemic sclerosis and oxygen saturation (SpO2) declining because of severe ILD was hospitalized for treatment of chronic skin ulcers. During admission, he completed a 27-week walking exercise program with SpO2 monitoring. Consequently, continuous walking distance without severe hypoxia (SpO2 > 90%) increased from 60 m to 300 m after the program, although his six-minute walking distance remained the same. This suggests that walking exercise for several months may reduce the risk of hypoxia in patients with ILD, even though exercise capacity does not improve.
Keywords: exercise, hypoxia, interstitial lung disease, systemic sclerosis, walking
Introduction
Systemic sclerosis is a multisystem disease with pulmonary involvement, which decreases exercise capacity and is related to survival.1,2 Medication and exercise training have recently been shown to improve dyspnea, six-minute walking distance, maximum heart rate, and quality of life.3 Most training studies4,5 have been performed using 8-week programs based on pulmonary rehabilitation used in the treatment of chronic obstructive pulmonary disease.6,7 This study was performed to evaluate the effects of a rehabilitation program including walking training over a 6-month period in a patient with systemic sclerosis and to determine any improvement in exercise capacity.
Case Report
A 43-year-old male patient with systemic sclerosis and ILD was admitted with chronic ulceration of his fingers. He had been treated for 4 years with corticosteroids, and at a dose of 10 mg for the 4 months prior to presentation. His lifestyle was sedentary and he had refused home oxygen therapy. He lived independently, including being able to drive. His Hugh-Jones grade was 3, ie, he was unable to keep up with healthy persons walking on the level, but was able to walk for one mile (1.6 km) or more at a slower speed.
On admission, forced vital capacity was 61.5% and carbon monoxide diffusion capacity (DLCO) was 29.8% of predicted. Blood gas analysis showed a PaO2 of 74 mmHg and PaCO2 of 39 mmHg. Right ventricular systolic pressure was 39 mmHg and mean pulmonary artery pressure was 18 mmHg. His six-minute walking distance was 521 m, with oxygen saturation (SpO2) declining from 96% at rest to 72% at completion, determined using a handheld pulse oximeter with a reflectance sensor on the forehead. Perceived exertion increased from 0 to 4 on the Borg 10 scale. Walking distance without rest was 60 m when SpO2 declined to 85%.
After admission to hospital, the corticosteroid dose was kept the same as before, but bosentan, sildenafil, and prostacyclin derivatives were added to treat the ulcers. The prostacyclin dose was increased during the first 8 weeks of admission, and then remained unchanged until discharge.
The rehabilitation program included walking training, training for leg muscle strengthening with a sand weight of 2.5 kg on the mat, and additional stretching exercise for the fingers because of sclerotic skin changes. The total time spent exercising was about one hour per day on 5 days per week. The patient gave informed consent to these rehabilitation treatments before starting the program. On the first day of walking training, 60 m walking in one minute was performed based on the first evaluation and was repeated with rest intervals of a few minutes. The total walking training time was 20 to 30 minutes per day. Training distance without rest increased when SpO2 was above 90% during training.
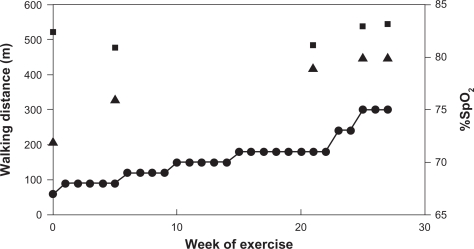
Figure 1 shows the training walking distance starting from 60 m, increasing gradually to 300 m after 27 weeks of training. The six-minute walking distance, evaluated five times, was about 500 m, and perceived exertion in the fifth test also increased from 0 to 4 on the Borg scale, while the end value of SpO2 was increased. At discharge, when the finger ulcers had resolved, forced vital capacity was 59.8% and DLCO was 24.2% of predicted. Right ventricular systolic pressure was 36 mmHg and mean pulmonary artery pressure was 19 mmHg, suggesting little change in cardiopulmonary function.
Figure 1.
Following walking exercise, training distance (•) increased during the intervention period. Six-minute walking test (▪) showed no marked changes, while end %SpO2 of the test (▴) improved.
Discussion
This patient showed no improvement in six-minute walking distance. In COPD patients, the minimal important difference for a six-minute walking distance test is 25 m,8 and was 22 m in this patient. One of the exclusion criteria for the six-minute walking test is an initial resting SpO2 < 90%.9 However, there are no clear criteria to discontinue the test in relation to low SpO2. The final SpO2 in this patient was 72%–80%, showing slight improvement, although these values were thought to be harmful to his circulation. Because this patient had no severe dyspnea during the six-minute walking test, it was recommended that he continue most of his daily activities despite the low oxygen saturation which might have been causing his finger ulcers.
During training in ILD, Holland et al3 set the lowest SpO2 to 85%. Progressive walking training was introduced by Nava10 in stepwise rehabilitation following acute respiratory failure. High-intensity interval exercise training for COPD is effective in inducing peripheral muscle adaptation, with less dyspnea compared with constant-load exercise.11 These studies are encouraging with regard to interval walking training (SpO2 > 90%) for ILD patients. Exercise training was beneficial to our patient in reducing the risk of hypoxia during walking up to 300 m. Thus, exercise training would be effective in improving safety, considering both hemodynamics and skin ulcer recurrence.
Some medications for pulmonary arterial hypertension were added to treat the ulcers. Bosentan is reported to have no effect on the six-minute walking distance in idiopathic pulmonary fibrosis,12 whereas prostacyclin derivatives improved six-minute walking distance test in systemic sclerosis with pulmonary arterial hypertension.12 These medications for pulmonary arterial hypertension did not improve cardiopulmonary function nor exercise capacity in our patient.
Conclusion
Generally, exercise training for lung disease is known to increase exercise capacity over 8 weeks. Although the six-minute walking distance in this patient was about 500 m and did not change after exercise training, the risk of hypoxia was remarkably reduced up to 300 m of walking. This case report suggests a benefit of exercise training to ameliorate hypoxia in addition to improving exercise capacity.
Acknowledgments
This study was supported by a Grant-in-Aid for Scientific Research.
Footnotes
Disclosures
Author(s) have provided signed confirmations to the publisher of their compliance with all applicable legal and ethical obligations in respect to declaration of conflicts of interest, funding, authorship and contributorship, and compliance with ethical requirements in respect to treatment of human and animal test subjects. If this article contains identifiable human subject(s) author(s) were required to supply signed patient consent prior to publication. Author(s) have confirmed that the published article is unique and not under consideration nor published by any other publication and that they have consent to reproduce any copyrighted material. The peer reviewers declared no conflicts of interest.
References
- 1.Koh ET, Lee P, Gladman DD, Abu-Shakra M. Pulmonary hypertension in systemic sclerosis: An analysis of 17 patients. Br J Rheumatol. 1996;35:989–93. doi: 10.1093/rheumatology/35.10.989. [DOI] [PubMed] [Google Scholar]
- 2.Goh NSL, Desai SR, Veeraraghavan S, et al. Interstitial lung disease in systemic sclerosis. Am J Respir Crit Care Med. 2008;177:1248–54. doi: 10.1164/rccm.200706-877OC. [DOI] [PubMed] [Google Scholar]
- 3.Holland AE, Hill CJ, Conron M, Munro P, McDonald CF. Short term improvement in exercise capacity and symptoms following exercise training in interstitial lung disease. Thorax. 2008;63:549–54. doi: 10.1136/thx.2007.088070. [DOI] [PubMed] [Google Scholar]
- 4.Nishiyama O, Kondoh Y, Kimura T, et al. Effects of pulmonary rehabilitation in patients with idiopathic pulmonary fibrosis. Respirology. 2008;13:394–9. doi: 10.1111/j.1440-1843.2007.01205.x. [DOI] [PubMed] [Google Scholar]
- 5.Ferreira A, Garvey C, Connors GL, et al. Pulmonary rehabilitation in interstitial lung disease. Chest. 2009;135:442–7. doi: 10.1378/chest.08-1458. [DOI] [PubMed] [Google Scholar]
- 6.Garrod R, Lasserson T. Role of physiotherapy in the management of chronic lung diseases: An overview of systematic reviews. Respir Med. 2007;101:2429–36. doi: 10.1016/j.rmed.2007.06.007. [DOI] [PubMed] [Google Scholar]
- 7.Foglio K, Bianchi L, Bruletti G, et al. Seven-year time course of lung function, symptoms, health-related quality of life, and exercise tolerance in COPD patients undergoing pulmonary rehabilitation programs. Respir Med. 2007;101:1961–70. doi: 10.1016/j.rmed.2007.04.007. [DOI] [PubMed] [Google Scholar]
- 8.Holland AE, Hill CJ, Rasekaba T, Lee A, Naughton MT, McDonald CF. Updating the minimal important difference for six-minute walk distance in patients with chronic obstructive pulmonary disease. Arch Phys Med Rehabil. 2010;91:221–5. doi: 10.1016/j.apmr.2009.10.017. [DOI] [PubMed] [Google Scholar]
- 9.Enright PL, McBurnie MA, Bittner V, et al. The 6-min walk test: a quick measure of functional status in elderly adults. Chest. 2003;123:387–98. doi: 10.1378/chest.123.2.387. [DOI] [PubMed] [Google Scholar]
- 10.Nava S. Rehabilitation of patients admitted to a respiratory intensive care unit. Arch Phys Med Rehabil. 1998;79:849–54. doi: 10.1016/s0003-9993(98)90369-0. [DOI] [PubMed] [Google Scholar]
- 11.Vogiatzis I, Terzis G, Nanas S, et al. Skeletal muscle adaptations to interval training in patients with advanced COPD. Chest. 2005;128:3838–45. doi: 10.1378/chest.128.6.3838. [DOI] [PubMed] [Google Scholar]
- 12.King TE, Jr, Behr J, Brown KK, et al. BUILD-1: a randomized placebo-controlled trial of bosentan in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2008;177:75–81. doi: 10.1164/rccm.200705-732OC. [DOI] [PubMed] [Google Scholar]
- 13.Badesch DB, Tapson VF, McGoon MD, et al. Continuous intravenous epoprostenol for pulmonary hypertension due to the scleroderma spectrum of disease. A randomized, controlled trial. Ann Intern Med. 2000;132:425–34. doi: 10.7326/0003-4819-132-6-200003210-00002. [DOI] [PubMed] [Google Scholar]