Abstract
Objective
An alcohol-induced memory blackout represents an amnesia to recall events but does not involve a loss of consciousness. Memory blackouts are a common occurrence among college drinkers, but it is not clear if a history of memory blackouts is predictive of future alcohol-related injury above and beyond the risk associated with heavy drinking episodes. This analysis sought to determine if baseline memory blackouts can prospectively identify college students with alcohol-related injury in the next 24 months after controlling for heavy drinking days.
Methods
Data were analyzed from the College Health Intervention Project Study (CHIPS), a randomized controlled trial of screening and brief physician intervention for problem alcohol use among 796 undergraduate and 158 graduate students at four university sites in the US and one in Canada, conducted from 2004 to 2009. Multivariate analyses used generalized estimating equations (GEE) with the logit link.
Results
The overall 24-month alcohol-related injury rate was 25.6%, with no significant difference between males and females (p=.51). Alcohol-induced memory blackouts at baseline exhibited a significant dose-response on odds of alcohol-related injury during follow-up, increasing from 1.57 (95% CI: 1.13–2.19) for subjects reporting 1–2 memory blackouts at baseline to 2.64 (95% CI: 1.65–4.21) for students acknowledging 6+ memory blackouts at baseline. The link between memory blackouts and injury was mediated by younger age, prior alcohol-related injury, heavy drinking, and sensation-seeking disposition.
Conclusions
Memory blackouts are a significant predictor of future alcohol-related injury among college drinkers after adjusting for heavy drinking episodes.
Keywords: alcohol drinking, alcohol abuse, blackout, memory
INTRODUCTION
Hazardous drinking and its consequences are pervasive on college campuses.[1] An estimated 599,000 college students were injured in 2001 as a result of alcohol use.[2] Approximately 1,825 college students died from alcohol-related unintentional injury in 2005.[2]
Despite the burden of injuries, the predictors of future alcohol-induced bodily harm among college drinkers are not well understood.[3] Notably, it is not clear from research to date whether a history of alcohol-induced memory blackouts predicts future alcohol-related injury among college drinkers.
An alcohol-induced memory blackout represents amnesia to recall events but does not involve loss of consciousness.[4] Research suggests that alcohol use can affect memory formation by altering nerve–cell communication in the hippocampus region of the brain (Givens et al. 2000; Tomberg, 2010). A rapid rise in blood alcohol concentration has been linked to increased incidence of memory blackout (Rose and Grant, 2010).
Memory blackouts are common on college campuses, with nearly half of drinking students reporting at least one memory blackout in their lifetime and one third reporting a memory blackout in the past year.[5–6] Approximately 5% of drinking students experienced alcohol-related amnesia in the past 7 days.[7] On US college campuses women are as likely to have a memory blackout as men despite consuming lower quantities of alcohol.[5]
Cross-sectional studies consistently show an association between heavy alcohol consumption and injuries for college students. Students who engage in heavy episodic drinking (5+drinks for men or 4+drinks for women) on 3 or more occasions in the past month suffer 8 times greater injury rates than other students.[8] Frequent (6+ occasions in the past 2 weeks) and heavy drinkers together have an odds ratio of injury more than 11 times that of non-heavy drinkers.[9] For male college students, injuries increase 19% with each additional day consuming 8 or more drinks, and for female students, injuries increase 10% with each day consuming 5 or more drinks.[10] Unfortunately, injury prevention screening based on quantity-frequency of alcohol consumption lacks specificity. For example, 55% of college students are identified as at-risk for injury with a 5/4 alcohol drinking measure.[8]
It would be beneficial to find a prospective marker of alcohol-related injury that is more discriminating in identifying students at highest risk for injury. No prior studies have assessed memory blackouts as a marker for future injury after adjusting for alcohol intake. To fill this gap in the literature, the present study examines data from the College Health Improvement Projects (CHIPS), a randomized controlled trial of brief physician alcohol intervention for college students. Alcohol use, alcohol-induced memory blackouts and alcohol-related injury rates were collected at baseline, 6, 12, 18, and 24 month follow-ups. The objective of this analysis is to determine if baseline memory blackouts can prospectively identify college students with alcohol-related injuries in the next 24 months after adjusting for alcohol quantities. This will be the first large prospective study examining memory blackouts as a predictor of future alcohol-related injuries among college students.
METHODS
This study analyzes data from the College Health Intervention Project Study (CHIPS), a randomized controlled trial of screening and brief physician intervention for problem alcohol use conducted at four university sites in the US and one in Canada. A more detailed study description is presented in Fleming et al.[11] The study was approved by the Institutional Review Boards for the Protection of Human Subjects in Research at the participating sites.
Study Sample
Study enrollment was limited to full-time students aged 18 years or older. At four sites, students were administered a Health Screening Survey (HSS) upon arrival for a regularly scheduled appointment with their primary care clinician. At a fifth site, recruitment was conducted at a college health class. The HSS embeds alcohol screening questions with questions on smoking, exercise, and weight control. Participation at all sites was voluntary.
A total of 12,900 students completed the HSS, with 4,532 screening positive for at-risk drinking, defined as 15+ drinks per week for men or 12+ drinks per week for women. Students screening positive were invited to participate in a face-to-face baseline eligibility interview for the intervention phase of the study.
A total of 2,090 students completed the face-to-face baseline interview for the randomized clinical trial. Eligibility criteria for entry into the randomized trial were 50 drinks or 8 or more heavy drinking days (5+ standard 14-g drinks) in the previous 28 days for male students and 40 drinks or 6 heavy drinking days (4+ standard 14-g drinks) in the previous 28 days for female students.
Overall, 986 high risk drinkers met the study inclusion criteria, provided informed consent, and were randomized into the study: 493 to the brief alcohol intervention group and 493 to the control group. Brief intervention subjects received personalized feedback focused on the adverse consequences of alcohol and development of risk reduction skills. Control group subjects were given a general health education booklet with advice on diet, exercise, tobacco, and alcohol use.
Telephone follow-ups were conducted by a trained researcher with all randomized subjects at 6, 12, 18, and 24 months post-randomization. Of the 986 subjects enrolled in the trial, 97% (n=955) took part in one or more follow-up interviews. One subject did not complete the baseline memory blackout question and was excluded from the analysis. The resulting sample size for the analysis reported here was 954 students.
Alcohol Consumption Measures
Students completed a 28-day Alcohol Timeline Follow-Back (TLFB).[12–13] Participants identified the days they drank alcohol and the number of standard drinks they consumed each day. The interviewer verified that the subject understood the definition of standard drink sizes in relation to drinks served in a bar setting. The standard drink size was defined as 14g of alcohol, corresponding to 12 ounces of beer, 5 ounces of wine, or 1.5 ounces of 80 proof liquor.
Alcohol-Related Injury Measure
The variable of interest in the analysis was bodily harm as a direct result of alcohol use. Students were asked the following questions at baseline and follow-up: ‘In the past 6 months, how many accidents or injuries have you had?’ and ‘Was alcohol a factor in any of your injuries?’ A positive response to both questions was defined as the affirmative for alcohol-related injury. The interviewer clarified for respondents that the intent of the former question was motor vehicle collisions or injuries requiring medical treatment.
Memory Blackout Measure
Memory blackout frequency was collected at baseline as part of the Rutgers Alcohol Problem Index (RAPI).[14] Respondents were prompted with the sentence ‘How many times has this happened to you while you were drinking or because of your drinking during the last year?’ Students were then asked to reply to the memory blackout item, which read ‘Suddenly found yourself in a place that you could not remember getting to.’ Responses were given on a 4-point scale (never, 1–2 times, 3–5 times, more than 5 times). The RAPI has been extensively used with college students and has been validated for identifying alcohol-related problems.[15–18]
Sensation Seeking Measure
Sensation-seeking has been shown to be associated with alcohol use disorders among college students (Sher et al., 2000). Sensation-seeking was assessed with the 8-item Brief Sensation-Seeking Scale (BSSS) developed by Hoyle et al.[19] The items were measured on a 7-point scale with values ranging from “strongly disagree” to “strongly agree”.
Statistical Analyses
Statistical analyses were based on alcohol-related injury rates during the 24-month follow-up period of the randomized controlled trial. Memory blackout frequencies were compared by chi-square analysis across covariates. Pearson correlations were calculated to assess unadjusted bivariate associations between follow-up alcohol-related injury and memory blackout frequency at baseline.
Multivariate analyses used generalized estimating equations (GEE) with the logit link [20–21]. A first GEE model included only alcohol-induced memory blackouts as a predictor of unadjusted alcohol-related injury risk. A full GEE model then controlled for subject intervention group status, gender, age, class level, weight, total number of drinks in the past 28 days, heavy drinking days (≥5 drinks male, ≥4 drinks female), sensation-seeking disposition, and alcohol-related injury prior to study enrollment. Separate indicator variables were created and entered into the model for the 1–2 blackout, 3–5 blackout, and 6+ blackout categories. The odds ratios obtained from the model represent odds of alcohol-related injury in the 24 months of follow-up relative to the no blackout group. All multivariate analyses were conducted in SAS version 9.1 (SAS Institute Inc, Cary, NC).
RESULTS
Table 1 provides descriptive information by gender on the 954 randomized subjects who completed at least one follow-up and answered the baseline RAPI. The participants were equally divided between males (49%) and females (51%). The sample was predominantly non-Hispanic white (91%), and represented a wide range of ages and class levels, including graduate students (16%).
Table 1.
Baseline Characteristics of High Risk College Drinkers in CHIPS, a Brief Alcohol Intervention Trial (n=954)
| Males (n=471) | Females (n=483) | |
|---|---|---|
| Intervention group status | ||
| Experimental, % | 49.7 | 48.7 |
| Control, % | 50.3 | 51.3 |
| Race/Ethnicity | ||
| Non-hispanic white, % | 89.4 | 92.5 |
| White hispanic, % | 4.3 | 2.7 |
| African American, % | 0.6 | 0.6 |
| Asian American, % | 3.0 | 2.7 |
| Other/refused, % | 2.7 | 1.5 |
| Age | ||
| 18–20 years, % | 44.2 | 46.2 |
| 21–23 years, % | 34.4 | 35.6 |
| 24 or older, % | 21.4 | 18.2 |
| Year in school | ||
| Freshman, % | 19.1 | 19.1 |
| Sophomore, % | 17.6 | 16.2 |
| Junior, % | 22.5 | 20.3 |
| Senior, % | 23.6 | 28.6 |
| Graduate student, % | 17.2 | 15.9 |
| Sensation-seekinga, mean (sd) | 3.60 (0.58)** | 3.31 (0.65)** |
| Weight (lbs), mean (sd) | 179 (28)** | 146 (28)** |
Table 2 gives alcohol use, memory blackout frequency, and injury rates for the study participants. Male subjects consumed 81.8 drinks on average in the past 28 days, while females consumed significantly less, averaging 58.7 drinks (p<.001). Men drank significantly more drinks on a typical drinking day than women (7.4 vs. 5.6, p<.001). Females in the study reported significantly fewer heavy drinking days, defined as 5+ drinks for men or 4+ drinks for women, than did males (p=.01). More than half of the subjects experienced one or more memory blackouts in the 12 months prior to the study. Seven percent reported 6 or more past year memory blackout episodes prior to study entry. Despite significant differences in amounts of alcohol consumed, males and females in the study reported similar frequencies of memory blackouts (p=.94). In addition, there were no significant differences in alcohol-related injuries by gender at baseline (p=.48) or during 24-month follow-up (p=.51). The overall 24-month alcohol-related injury rate was 25.6%.
Table 2.
Alcohol Consumption, Memory Blackout Frequency, and Alcohol-Related Injury Among High-Risk College Drinkers (n=954)
| Males (n=471) | Females (n=483) | |
|---|---|---|
| Baseline alcohol use | ||
| Days drinking, past 28 days (sd) | 12.0 (5.0) | 11.5 (4.9) |
| Drinks per drinking day (sd) | 7.4 (2.9)** | 5.6 (2.4)** |
| Total drinks, past 28 days (sd) | 81.8 (35.4)** | 58.7 (28.0)** |
| Heavy drinking daysa (sd) | 7.5 (3.5)** | 6.9 (3.4)** |
| Baseline memory blackouts, past 12 months | ||
| 0 memory blackouts, % | 48.4 | 49.7 |
| 1–2 memory blackouts, % | 29.5 | 28.2 |
| 3–5 memory blackouts, % | 14.7 | 15.5 |
| 6+ memory blackouts, % | 7.2 | 6.6 |
| Alcohol-related injuryb, past 6 months | ||
| Baseline, % | 15.9 | 14.3 |
| 6-month follow-up, % | 10.4 | 10.9 |
| 12-month follow-up, % | 11.2 | 10.0 |
| 18-month follow-up, % | 8.9 | 9.0 |
| 24-month follow-up, % | 8.3 | 6.7 |
| All follow-ups combined, % | 24.6 | 26.5 |
p<.05,
p<.01
Days of drinking ≥5 drinks for men or ≥4 drinks for women
Positive response to both: ‘In the past 6 months, how many accidents or injuries have you had?’ and ‘Was alcohol a factor in any of your injuries?’
Memory blackouts were negatively associated with age (r=−0.24, p<.001). Students 24 years or older reported the lowest baseline memory blackout rates. Students 18 to 20 years of age reported the highest memory blackout rates. Memory blackout frequency was positively correlated with number of heavy drinking days (r=0.19, p<.001). Subjects reporting no heavy drinking days at baseline averaged 0 memory blackouts, while subjects reporting 9 or more heavy drinking days at baseline averaged 1–2 memory blackouts in past 12 months.
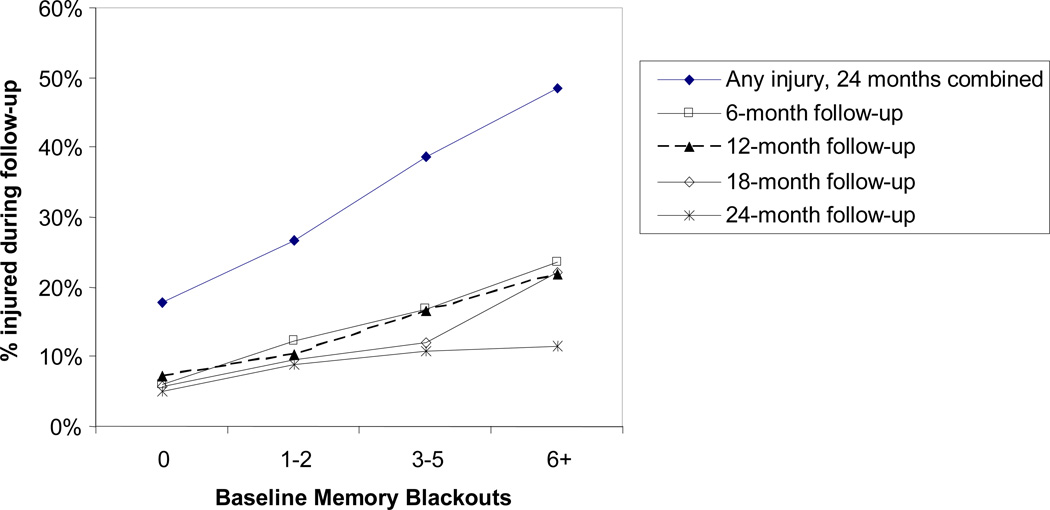
Figure 1 provides alcohol-related injury rates by baseline blackout frequency. The overall 24-month alcohol-related injury rates were 18% for subjects who reported no memory blackouts at study baseline, but jumped to 49% for drinkers reporting frequent (6+) memory blackouts at baseline. At the first 6-month follow-up post-randomization, injury rates were 6% for students reporting no memory blackouts, going up to 23% for study enrollees reporting frequent (6+) memory blackouts. At 12 months, alcohol injuries differed from 7% with no memory blackouts to 22% for frequent memory blackouts sufferers. Eighteen-month rates were similar, varying from 6% for students with no memory blackouts to 22% for participants with frequent memory blackouts. Injury rates were lower at 24-month follow-up, but still showed a positive association with memory blackouts at baseline. The correlations between memory blackouts and alcohol-related injuries were highly significant at 6-month (r=0.17, p<.001), 12-month (r=0.14, p<.001), and 18-month (r=0.14, p<.001) follow-up, and statistically significant (r=0.09, p=.04) at 24-month assessment.
Figure 1.
Follow-Up Alcohol Injury Rates among High-Risk College Drinkers by Baseline Memory Blackouts from 2004 to 2009
The multivariate GEE analysis results presented in Table 3 model odds of alcohol-related injury during 24-month follow-up. The blackout-only GEE model shows a strong association between memory blackouts and alcohol-related injuries before adjusting for covariates. In the full GEE model, memory blackouts at baseline still exhibited a significant dose-response on alcohol injuries. Statistically significant baseline covariates for predicting future injury were prior alcohol-related injury, younger age (18 to 20 years), sensation-seeking disposition, and heavy drinking days. Experimental group status was not a significant predictor of injury during follow-up. Odds of alcohol-related injury in the 24-month follow-up steadily increased from 1.57 (95% CI: 1.13–2.19) for subjects reporting at least one memory blackout to 2.64 (95% CI: 1.65–4.21) for students acknowledging 6+ memory blackouts at baseline. Heavy drinking days were associated with an 8% increase (95% CI 1.01–1.16) in injury risk for each reported day. Notably, the effect size for the memory blackout measure was larger than for the heavy drinking measure.
Table 3.
Repeated Measures GEE Model for Alcohol-Related Injury during 24-Month Follow-Up among High-Risk College Drinkers
| Blackouts Only Model | Full Model with Covariates | |||||
|---|---|---|---|---|---|---|
| Covariate | OR | (95% CI) | p-value | OR | (95% CI) | p-value |
| Baseline memory blackouts | ||||||
| 1–2 memory blackoutsa | 1.79 | (1.28–2.52) | 0.001 | 1.57 | (1.13–2.19) | 0.01 |
| 3–5 memory blackoutsa | 2.55 | (1.77–3.68) | <0.001 | 1.85 | (1.27–2.77) | 0.003 |
| 6+ memory blackoutsa | 3.85 | (2.52–5.88) | <0.001 | 2.64 | (1.65–4.21) | <0.001 |
| Experimental groupb | 0.90 | (0.68–1.18) | 0.44 | |||
| Prior injury at baselineb | 1.67 | (1.19–2.36) | 0.003 | |||
| Age 18 to 20b | 1.73 | (1.10–2.73) | 0.02 | |||
| Age 21 to 23b | 1.09 | (0.70–1.71) | 0.69 | |||
| Maleb | 0.98 | (0.68–1.40) | 0.89 | |||
| Non-hispanic whiteb | 1.97 | (0.69–5.63) | 0.20 | |||
| White hispanicb | 3.03 | (0.93–9.90) | 0.07 | |||
| Asianb | 2.12 | (0.55–8.14) | 0.27 | |||
| Freshmanb | 0.82 | (0.57–1.19) | 0.29 | |||
| Sensation seeking | 1.29 | (1.01–1.65) | 0.04 | |||
| Weight, per 10 lbs | 1.02 | (0.98–1.07) | 0.31 | |||
| Baseline drinks, per 10 drinks | 0.97 | (0.90–1.05) | 0.50 | |||
| Baseline heavy drinking days | 1.08 | (1.01–1.16) | 0.02 | |||
The reference group is no memory blackouts at baseline.
The reference category for comparison is control group status, no alcohol-related injury at baseline, age 24 or more, female, African American or other race category, and non-freshman.
DISCUSSION
The objective of this analysis was to assess the link between baseline memory blackouts and alcohol-related injury in the following 24-month period among high risk college drinkers seen at university health services. The analysis allowed us to identify prospectively an independent main effect between history of memory blackouts and future college alcohol-related injury after adjusting for a range of covariates (gender, age, class level, weight, alcohol use, sensation-seeking, and prior alcohol-related injury). Frequent memory blackout sufferers were almost three times more likely to suffer an alcohol-related injury during the two year follow-up period than students who consumed the same amount of alcohol without experiencing memory blackouts. More than half of all high-risk drinkers in our sample suffered at least one memory blackout in the past 12 months. This suggests that fifty percent of these heavy drinkers are at increased risk of injury. Given that campus resources are limited, our findings support further investigation of memory blackout sufferers in college injury prevention efforts.
Our results suggest that memory blackout screening at student health services could be a useful tool in college alcohol-related injury prevention. Memory blackout screening may accomplish several tasks at once: (1) identifying students at risk for alcohol-related injury; (2) recognizing drinking to the point of having a disruptive effect on cognitive function; (3) raising awareness about extreme levels of drinking and its consequences. As an example, consider a student who has experienced one alcohol memory blackout in the past 6 months and several heavy drinking days in the past 30 days, and who presents himself to student health services for a primary care appointment. A clinician armed with the heavy drinking measure screening alone may ask him about alcohol intake and suggest that the patient’s injury risk is increased by 20–30%. On the other hand, under similar circumstances, a clinician equipped with the memory blackout screening tool may inquire about both heavy drinking and memory blackouts and advise this patient that his chances for injury rise by more than 50%. In both cases, the doctor will point to risky drinking behavior as increasing the likelihood for injury. The memory blackout injury risk information, however, may drive home the point about extreme levels of alcohol intoxication more strongly than the heavy alcohol drinking risk data. It may be easier for a student to dismiss general warnings on excessive alcohol drinking harms than to refute that his extreme alcohol drinking is causing impairment in brain function. Future studies may wish to examine the efficacy of memory blackout screening for college alcohol-related injury prevention.
As seen in other studies,[5, 22–23] the females in our study were equally likely to experience an alcohol-related memory blackout or an alcohol-related injury despite drinking at lower quantities and frequencies than the males. More than 50% of the women in the study experienced a memory blackout in the 12 months prior to study enrollment. This finding suggests tailoring injury prevention efforts by gender, since, at equivalent levels of alcohol consumption, women are likely be at higher risk for injuries than men.
Alcohol-related injury in the 6 months prior to the study was also positively associated with injury during the follow-up period. This finding is in line with prior research that suggests that college students do not necessarily alter drinking behavior as a result of negative consequences (Mallett et al, 2006). Incorporating a history of alcohol-related injury into screening and injury prevention could improve specificity of risk prediction.
Sensation-seeking also was found to be a significant predictor of alcohol-related injury in the next 24 months. Several cross-sectional studies have identified an association between sensation-seeking and alcohol injuries.[24–26] Sensation seeking has been shown to be an independent predictor of alcohol traumatic injury in hospital ER patients.[27–28] Our study results suggest that campus alcohol-related injury prevention efforts may need to account for sensation-seeking nature when devising alternatives to heavy alcohol use. Future studies are needed to investigate this further.
Limitations
A potential limitation of the study is sample selection bias. Because the data were collected as part of a randomized controlled trial, only students who drank above at-risk drinking thresholds and who provided informed consent were included in this analysis. The students who participated in the study may not be representative of college students in general at the participating university sites. A comparison of eligible subjects who declined any further participation after the initial alcohol screen shows that study participants were younger and more likely to have experienced a recent alcohol-related injury. However, alcohol consumption levels and attribution of alcohol as an injury factor were similar between study participants and non-responders. Also, enrollment took place at student health centers, so the study sample was limited to students obtaining routine university health services. However, studies on college health services indicate that almost all students have access to a campus health clinic, with utilization of approximately 2 visits per student per year.[29] While the study results may not generalize to college students as a whole, they may be pertinent to the set of college students who would be targeted for alcohol intervention through university health services.
Another potential study limitation is that respondents were asked to self-report whether alcohol use was a factor in their injuries and to assess the history of memory blackouts. Study participants could potentially minimize the role of alcohol with their injury and underestimate the frequency of memory blackouts. Future studies could examine whether self-reported attribution of alcohol-related injury and memory blackouts produces lower alcohol-related injury and memory blackout rates than objectively collected data.
The strengths of the study are the prospective design, large sample size, and detailed information on alcohol use and other explanatory variables. Since students were asked about alcohol-related problems at baseline and then followed prospectively for the next 24 months, the study does not suffer from the common temporal issues related to cross-sectional research.
CONCLUSION
Memory blackouts are a strong predictor of future alcohol-related injury among college drinkers. The link between memory blackouts and injury is mediated by younger age, prior alcohol-related injury, heavy drinking, and sensation-seeking disposition. Our findings may have implications for prevention and intervention efforts by health care professionals working with college students and other populations at high risk for alcohol-related injuries.
What is already known on this subject:
Alcohol-related injury is a pervasive health problem on college campuses
Alcohol-induced memory blackouts are common among college drinkers
What this study adds:
Screening at-risk drinkers using a memory blackout question prospectively identifies college students at highest risk for alcohol-related injury
Memory blackout screening provides more specificity in screening for alcohol-related injury risk than screening with traditional alcohol quantity-frequency measures
Acknowledgments
FUNDING
This work was supported by NIAAA 1R01 AA014685-01 and NIAAA 1K01 AA018410-01.
Footnotes
There are no conflicts of interest.
Contributor Information
Marlon P. Mundt, University of Wisconsin-Madison, Department of Family Medicine, Madison WI, USA.
Larissa I. Zakletskaia, University of Wisconsin-Madison, Department of Family Medicine, Madison WI, USA.
David D. Brown, SeaPath Consulting, Vancouver BC, Canada.
Michael F. Fleming, University of Wisconsin-Madison, Department of Family Medicine, Madison WI, USA.
REFERENCES
- 1.Wechsler H, Nelson TF. What we have learned from the Harvard School of Public Health College Alcohol Study: Focusing attention on college student alcohol consumption and the environmental conditions that promote it. J Stud Alcohol Drugs. 2008;69(4):481–490. doi: 10.15288/jsad.2008.69.481. [DOI] [PubMed] [Google Scholar]
- 2.Hingson RW, Zha WX, Weitzman ER. Magnitude of and trends in alcohol-related mortality and morbidity among US college students ages 18–24, 1998–2005. J Stud Alcohol Drugs Suppl. 2009;16:12–20. doi: 10.15288/jsads.2009.s16.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beseler CL, Taylor LA, Leeman RF. An item-response theory analysis of DSM-IV alcohol-use disorder criteria and "binge" drinking in undergraduates. J Stud Alcohol Drugs. 2010;71(3):418–423. doi: 10.15288/jsad.2010.71.418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.White AM. What happened? Alcohol memory blackouts, and the brain. Alcohol Res Health. 2003;27(2):186–196. [PMC free article] [PubMed] [Google Scholar]
- 5.Givens B, Williams JM, Gill TM. Septohippocampal pathway as a site for the memory–impairing effects of ethanol. Hippocampus. 2000;10:111–121. doi: 10.1002/(SICI)1098-1063(2000)10:1<111::AID-HIPO12>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 6.Tomberg C. Alcohol pathophysiology circuits and molecular mechanisms. J Psychophysiol. 2010;24(4):210–212. [Google Scholar]
- 7.Rose ME, Grant JE. Alcohol-induced blackout phenomenology, biological basis, and gender differences. J Addict Med. 2010;4(2):61–73. doi: 10.1097/ADM.0b013e3181e1299d. [DOI] [PubMed] [Google Scholar]
- 8.White AM, Jamieson-Drake DW, Swartzwelder HS. Prevalence and correlates of alcohol-induced blackouts among college students: Results of an e-mail survey. J Am Coll Health. 2002;51(3):117–131. doi: 10.1080/07448480209596339. [DOI] [PubMed] [Google Scholar]
- 9.Wechsler H, Lee JE, Kuo MC, et al. College binge drinking in the 1990s: A continuing problem - Results of the Harvard School of Public Health 1999 College Alcohol Study. J Am Coll Health. 2000;48(5):199–210. doi: 10.1080/07448480009599305. [DOI] [PubMed] [Google Scholar]
- 10.Meilman PW, Stone JE, Gaylor MS, et al. Alcohol-consumption by college undergraduates - current use and 10-year trends. J Stud Alcohol. 1990;51(5):389–395. doi: 10.15288/jsa.1990.51.389. [DOI] [PubMed] [Google Scholar]
- 11.Wechsler H, Nelson TF. Binge drinking and the American college student: What's five drinks? Psychol Addict Behav. 2001;15(4):287–291. doi: 10.1037//0893-164x.15.4.287. [DOI] [PubMed] [Google Scholar]
- 12.Presley CA, Pimentel ER. The introduction of the heavy and frequent drinker: A proposed classification to increase accuracy of alcohol assessments in postsecondary educational settings. J Stud Alcohol. 2006;67(2):324–331. doi: 10.15288/jsa.2006.67.324. [DOI] [PubMed] [Google Scholar]
- 13.Mundt MP, Zakletskaia LI, Fleming MF. Extreme college drinking and alcohol-related injury risk. Alcohol Clin Exp Res. 2009;33(9):1532–1538. doi: 10.1111/j.1530-0277.2009.00981.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fleming MF, Balousek SL, Grossberg PM, et al. Brief physician advice for heavy drinking college students: A randomized controlled trial in college health clinics. J Stud Alcohol Drugs. 2010;71:23–31. doi: 10.15288/jsad.2010.71.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sobell LC, Sobell MB. Timeline follow-back: a technique for assessing self-reported alcohol consumption. In: Litten ZR, Allen JP, editors. Measuring Alcohol Consumption: Psychosocial and Biochemical Methods. Totowa, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- 16.Sobell LC, Sobell MB. Alcohol Timeline Followback (TFLB) In: Rush AJ, editor. Handbook of Psychiatric Measures. Washington, DC: American Psychiatric Association; 2000. pp. 477–479. [Google Scholar]
- 17.White HR, Labouvie EW. Towards the assessment of adolescent problem drinking. J Stud Alcohol. 1989;50(1):30–37. doi: 10.15288/jsa.1989.50.30. [DOI] [PubMed] [Google Scholar]
- 18.Martens MP, Neighbors C, Dams-O'Connor K, et al. The factor structure of a dichotomously scored rutgers alcohol problem index. J Stud Alcohol Drugs. 2007;68(4):597–606. doi: 10.15288/jsad.2007.68.597. [DOI] [PubMed] [Google Scholar]
- 19.Borsari B, Carey KB. Effects of a brief motivational intervention with college student drinkers. J Consult Clin Psychol. 2000;68(4):728–733. [PubMed] [Google Scholar]
- 20.Larimer ME, Turner AP, Anderson BK, et al. Evaluating a brief alcohol intervention with fraternities. J Stud Alcohol. 2001;62(3):370–380. doi: 10.15288/jsa.2001.62.370. [DOI] [PubMed] [Google Scholar]
- 21.Ham LS, Hope DA. Incorporating social anxiety into a model of college student problematic drinking. Addict Behav. 2005;30(1):127–150. doi: 10.1016/j.addbeh.2004.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sher KJ, Bartholow BD, Wood MD. Personality and substance use disorders: A prospective study. J Consult Clin Psychol. 2000;68(5):818–829. [PubMed] [Google Scholar]
- 23.Hoyle RH, Stephenson MT, Palmgreen P, et al. Reliability and validity of a brief measure of sensation seeking. Pers Individ Dif. 2009;32(3):401–414. [Google Scholar]
- 24.Zeger SL, Liang KY, Albert PS. Models for longitudinal data - A generalized estimating equation approach. Biometrics. 1988;44(4):1049–1060. [PubMed] [Google Scholar]
- 25.Mallett KA, Lee CM, Neighbors C, Larimer ME, Turrisi R. Do we learn from our mistakes? An examination of the impact of negative alcohol-related consequences on college students' drinking patterns and perceptions. J Stud Alcohol. 2006;67(2):269–276. doi: 10.15288/jsa.2006.67.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lee JH, Herzog TA, Meade CD, et al. The use of GEE for analyzing longitudinal binomial data: A primer using data from a tobacco intervention. Addict Behav. 2007;32(1):187–193. doi: 10.1016/j.addbeh.2006.03.030. [DOI] [PubMed] [Google Scholar]
- 27.Frezza M, Dipadova C, Pozzato G, et al. High blood-alcohol levels in women - the role of decreased gastric alcohol-dehydrogenase activity and 1st-pass metabolism. N Engl J Med. 1990;322(2):95–99. doi: 10.1056/NEJM199001113220205. [DOI] [PubMed] [Google Scholar]
- 28.Mumenthaler MS, Taylor JL, O'Hara R, et al. Gender differences in moderate drinking effects. Alcohol Res Health. 1999;23(1):55–64. [PMC free article] [PubMed] [Google Scholar]
- 29.Mcmillen DL, Pang MG, Wellsparker E, et al. Alcohol, personality-traits, and high-risk driving - a comparison of young, drinking driver groups. Addict Behav. 1992;17(6):525–532. doi: 10.1016/0306-4603(92)90062-z. [DOI] [PubMed] [Google Scholar]
- 30.Pickett W, Molcho M, Simpson K, et al. Cross national study of injury and social determinants in adolescents. Inj Prev. 2005;11(4):213–218. doi: 10.1136/ip.2004.007021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cherpitel CJ, Meyers AR, Perrine MW. Alcohol consumption, sensation seeking and ski injury: A case-control study. J Stud Alcohol. 1998;59(2):216–221. doi: 10.15288/jsa.1998.59.216. [DOI] [PubMed] [Google Scholar]
- 32.Field CA, O'Keefe G. Behavioral and psychological risk factors for traumatic injury. J Emerg Med. 2004;26(1):27–35. doi: 10.1016/j.jemermed.2003.04.004. [DOI] [PubMed] [Google Scholar]
- 33.Cherpitel CJ. Substance use, injury, and risk-taking dispositions in the general population. Alcohol Clin Exp Res. 1999;23(1):121–126. [PubMed] [Google Scholar]
- 34.Patrick K. Student health - medical-care within institutions of higher-education. JAMA. 1988;260(22):3301–3305. doi: 10.1001/jama.260.22.3301. [DOI] [PubMed] [Google Scholar]