Abstract
Background
Increasing knowledge about HPV and HPV vaccine is a potentially important way to increase vaccination rates, yet few education interventions have addressed these topics. We report the results of an education intervention targeting three key groups who have contact with adolescent females.
Methods
We conducted HPV education intervention sessions during 2008 and 2009 in Guilford County, North Carolina. Parents (n=376), healthcare staff (n=118), and school staff (n=456) attended the one-time sessions and completed self-administered surveys. Analyses used mixed regression models to examine the intervention’s effects on participants’ self-rated HPV knowledge, objectively assessed HPV and HPV vaccine knowledge, and beliefs about HPV vaccine.
Results
Participants had relatively low levels of objectively assessed HPV and HPV vaccine knowledge prior to the intervention. The education intervention increased self-rated HPV knowledge among all three key groups (all p<0.001), as well as objectively assessed knowledge about many aspects of HPV and HPV vaccine among healthcare and school staff members (all p<0.05). Following the intervention, over 90% of school staff members believed HPV and HPV vaccine education is worthwhile for school personnel and that middle schools are an appropriate venue for this education. Most parents (97%) and school staff members (85%) indicated they would be supportive of school-based vaccination clinics.
Conclusions
Our education intervention greatly increased HPV and HPV vaccine knowledge among groups influential to the HPV vaccination behaviors of adolescent females.
Impact
Education interventions represent a simple yet potentially effective strategy for increasing HPV vaccination and garnering stronger support for school-based vaccination clinics.
Keywords: Human papillomavirus, HPV vaccine, Healthcare provider, School, Adolescent
Introduction
Guidelines currently recommend that 11–12 year old females receive the 3-dose regimen of human papillomavirus (HPV) vaccine, with catch-up vaccination for 13–26 year old females (1). Widespread vaccination may greatly reduce cervical cancer incidence, perhaps by as much as 77% (2), as well as anal cancer incidence (3). However, recent data suggest fewer than half of 13–17 year old females in the United States (US) have received 1 or more doses of HPV vaccine, and only 32% have completed the 3-dose regimen (4).
Parents, healthcare providers, and school staff members are key stakeholders in the HPV vaccination behaviors of adolescent females. Parents are typically the main decision makers in choosing whether their adolescent daughters receive HPV vaccine (5). Healthcare providers are also important, since most females receive HPV vaccine at doctors’ offices (6) and provider recommendation is a key determinant of HPV vaccine uptake (7–9). Teachers and school administrators are likely to play an increasingly important role in influencing whether adolescent females receive HPV vaccine. School-based HPV vaccination programs, which have been exceptionally effective in Australia and the United Kingdom (10–12), have now started to expand to the US (13). Few schools in the US, however, currently provide vaccines of any type to students (14), likely because of issues concerning billing, insurance, and costs to the schools.
It is critical that key stakeholders possess adequate knowledge about HPV and the vaccine. Knowledge is important in the early stages of behavior change according to multiple frameworks that characterize the stages of adoption of health behaviors (15, 16). Furthermore, adequate knowledge is a prerequisite for making informed decisions about vaccination and vaccine policies. For this reason, providing information (to improve knowledge) is a common component of behavioral interventions (17).
Despite the role knowledge may play in HPV vaccination behaviors, several studies have shown HPV knowledge to be relatively low among parents and adult women in the US (18–21). Parents have also indicated that one of the main reasons why their daughters have not received HPV vaccine is a lack of information or knowledge about HPV and the vaccine (9, 22, 23). Many physicians and nurses in the US lack knowledge about certain aspects of HPV and HPV vaccine as well (24–27). We were not able to locate any studies examining HPV knowledge among school faculty and administrators. In addition to actual knowledge about HPV and the vaccine, it is important that these stakeholders have high levels of self-rated knowledge so that they feel confident discussing HPV vaccine with adolescent females and making informed decisions regarding vaccination.
Given inadequate HPV and HPV vaccine knowledge, education interventions designed to improve knowledge levels represent a potentially important initial step toward increasing vaccination rates among adolescent females. Such interventions may also influence individuals’ beliefs and attitudes about HPV vaccination, such as the acceptability of school-based HPV vaccination programs. Only a few intervention studies, however, have been conducted, all of which demonstrated that simple strategies (e.g., providing written materials or verbal information) improved knowledge among parents, adult women, or students (28–33). To the best of our knowledge, no studies have assessed the effectiveness of education interventions among healthcare providers or school employees. In this report, we describe the results of an HPV and HPV vaccine education intervention targeting three key groups who have contact with adolescent females: parents, healthcare staff, and school staff members. Results provide valuable information for future programs designed to increase not only knowledge about HPV and HPV vaccine but also vaccination rates.
Materials and Methods
Participants and recruitment
The Guilford County HPV Campaign sought to create a model for school-based HPV vaccination programs through collaborative partnerships between the local school system and local health department. Guilford County, North Carolina has the potential to benefit greatly from HPV vaccination since its cervical cancer mortality rate is among the highest in the state (6.1 deaths per 100,000 women annually) (34). A year prior to the launch of the school HPV vaccination campaign in Guilford County (results of which we report separately (35)), we conducted an HPV education campaign called “Don’t Wait….Educate!”. The campaign consisted of education intervention sessions throughout the county that targeted caregivers of middle school students (referred to as “parents”), nurses and health educators (referred to as “healthcare staff”), and school administration and faculty members (referred to as “school staff”). We conducted this initial phase of the project to increase knowledge about HPV and HPV vaccine among key groups who have contact with adolescent females, the target population for HPV vaccination. To assist with intervention development and implementation, we formed an advisory team comprised of individuals from the Guilford County Department of Public Health, the local school system, and the community.
After gaining approval from appropriate members of the Guilford County School System, we began conducting education sessions in middle schools. In participating schools, we held separate sessions for parents and school staff, which commonly occurred in locations such as the school library or media room. To reach a greater number of parents, we conducted additional sessions on-site at various community events and sites. Parent sessions were open to anyone interested in attending. For healthcare staff, we held education sessions for school health nurses, congregational nurses, student nurses, community health educators, and various professional medical societies. We also conducted an education session at the Guilford County Department of Public Health for all interested healthcare workers in the community. All education sessions occurred during 2008 and 2009.
To increase attendance at the education sessions, we developed a marketing and publicity plan to promote the sessions. We held many of the events outside of normal business hours or on weekends, and we held sessions for school staff during mandatory staff meetings. School websites and voicemail systems helped notify and remind parents about the education sessions. Participants did not receive incentives for attending a session. We report data from 118 healthcare staff members (from 5 education sessions), 456 school staff members (from 11 education sessions), and 376 parents (from 16 education sessions), excluding data for 5 healthcare staff members and 25 school staff members who did not complete both pre- and post-intervention surveys.
Intervention
We developed an educational PowerPoint presentation on HPV and HPV vaccine that provided information on HPV prevalence and transmission, diseases associated with HPV infection, vaccine recommendations, dosage schedule, vaccine efficacy and safety, and insurance coverage for the vaccine. The presentation lasted about 30–40 minutes including time for questions. A community health educator who was part of the advisory team gave the presentations. We also developed an educational handout to accompany the presentation that had similar information. We instructed participants from all three groups to refrain from using the educational handout when completing surveys. School and healthcare staff members completed self-administered written surveys both before and after the education intervention. Pre-intervention surveys were distributed, completed, and collected prior to presentations, and post-intervention surveys were distributed and completed following presentations. Based on advisory team members’ advice that multiple surveys may discourage parents’ participation, we asked parents to complete surveys only following presentations.
Measures
We designed the surveys mainly to assess participants’ knowledge about HPV and HPV vaccine (items shown in Table 1). To reduce respondent burden, we omitted some items for some groups. We asked participants to rate their knowledge of HPV from 1 to 10, with 10 being the highest level (i.e., self-rated knowledge). Both pre- and post-interventions surveys contained this item for school and healthcare staff members. On parents’ post-intervention surveys, they rated their current knowledge and estimated their knowledge before the educational presentation. School and healthcare staff surveys (pre- and post-intervention) contained multiple choice items regarding the number of new HPV cases diagnosed each year in the US (about 6 million), the percent of these cases that occur in 15–24 year olds (74%), and the percent of cervical cancer cases in which HPV can be found (99%) (36). For each item, we scored responses as “correct” or “incorrect”.
Table 1.
Survey measures
| Healthcare Staff | School Staff | Parents | |||
|---|---|---|---|---|---|
| Pre | Post | Pre | Post | Post | |
| Knowledge (self-rated)a | ● | ● | ● | ● | ● |
| Knowledge (objectively assessed) | |||||
| Number of new HPV cases each year in the US | ● | ● | ● | ● | |
| Percent of new HPV cases that occur in 15–24 year olds | ● | ● | ● | ● | |
| Percent of cervical cancers where HPV can be found | ● | ● | ● | ● | |
| Vaccine is effective in virus-naïve females but does not protect against or treat existing infections | ● | ● | ● | ● | |
| Half of cervical cancer cases between ages 35–50 were likely exposed to HPV in teens or early twenties | ● | ● | ● | ● | |
| A woman dies every 2.5 hours from cervical cancer in the US | ● | ● | |||
| Regular Pap smear tests are no longer needed after HPV vaccination | ● | ● | |||
| Beliefs | |||||
| Community education on HPV and HPV vaccine is valuable | ● | ● | |||
| Would choose to vaccinate daughter if they had one in the approved age range for HPV vaccine | ● | ● | |||
| HPV and HPV vaccine education is worthwhile for school personnel | ● | ● | |||
| Middle schools are an appropriate venue for HPV and HPV vaccine education | ● | ● | |||
| Course of action if a student approached them with questions about HPV or HPV vaccine | ● | ● | |||
| Would be supportive of a school-based vaccination clinic | ● | ● | ● | ||
Note. Surveys delivered before or after educational intervention.
On post-intervention surveys, parents self-rated their current HPV knowledge and estimated their knowledge before the educational presentation.
School and healthcare staff surveys (pre- and post-intervention) also included true/false items about HPV and the vaccine. We asked healthcare staff members whether: 1) a woman in the US dies every 2.5 hours from cervical cancer (true); 2) vaccinated females no longer need to receive regular Pap smear tests (false); 3) HPV vaccine has shown virtually 100% efficacy in preventing HPV infection among virus-naïve females but does not protect against or treat existing HPV infections (true); and 4) half of women diagnosed with cervical cancer between the ages of 35 and 50 were mostly likely exposed to HPV in their teens or early twenties (true). School staff surveys only included the last two true/false items. The presentation and handout provided information needed to correctly answer the items.
The surveys also assessed beliefs surrounding HPV vaccine, education programs, and school-based vaccination clinics. We asked school staff (pre- and post-intervention) if they believed HPV and HPV vaccine education is worthwhile for school personnel (yes or no), whether middle schools are an appropriate venue for this education (yes or no), and what they would do if a student approached them with questions about HPV or the vaccine. For the last item, response options included: 1) feel comfortable or confident enough in their knowledge about HPV to talk with the student themselves; 2) advise the student to speak with the school nurse; 3) advise the student to speak with a parent; and 4) tell the student they are too young to be concerned with such things. We allowed participants to select more than one answer for this item. We asked school staff (pre- and post-intervention) and parents (post-intervention) if they would be supportive of school-based vaccination clinics. Healthcare staff surveys (pre- and post-intervention) assessed whether they believed community education on HPV and HPV vaccine is valuable and whether they would choose to vaccinate their daughter if they had one in the approved age range for HPV vaccine. We collected data on gender, age, and race/ethnicity for all three groups, as well as occupation for healthcare staff members.
Data analysis
For all groups, we compared pre- and post-intervention self-rated HPV knowledge. For healthcare and school staff, we compared pre- and post-intervention objectively assessed HPV knowledge and beliefs regarding HPV and HPV vaccine. We also compared self-rated HPV knowledge across the three groups, using the Bonferroni correction to account for multiple comparisons. We used mixed regression models for analyses as participants were clustered within education sessions. Data were analyzed with SAS Version 9.2 (Cary, NC) using two-tailed statistical tests and a critical alpha of 0.05.
Results
Healthcare staff
About 60% of healthcare staff members were health educators, and just over 40% were nurses. Most were female (93%), older than 40 years of age (58%), and non-Hispanic white (50%) or non-Hispanic African American (46%) (Table 2). Healthcare staff members indicated much higher levels of self-rated HPV knowledge on their post-intervention surveys (mean=8.12, SD=1.09) compared to their pre-intervention surveys (mean=5.69, SD=2.01, p<0.001) (Figure 1). The education intervention substantially increased staff members’ objectively assessed knowledge about HPV and HPV vaccine (Table 3). Compared to pre-intervention surveys, more staff members indicated on their post-intervention surveys that there are about 6 million new HPV cases in the US each year (31% vs. 85%, p<0.001), that 74% of these new cases occur among 15–24 year olds (59% vs. 95%, p<0.001), that HPV can be found in 99% of cervical cancer cases (20% vs. 84%, p<0.001), that HPV vaccine will not protect against or treat existing infections (77% vs. 97%, p<0.001), and that a woman dies every 2.5 hours from cervical cancer in the US (77% vs. 87%, p<0.05).
Table 2.
Characteristics of healthcare staff (n=118), school staff (n=456), and parents (n=376)
| Healthcare Staff n (%) | School Staff n (%) | Parents n (%) | |
|---|---|---|---|
| Gender | |||
| Female | 109 (93) | 347 (77) | 343 (91) |
| Male | 8 (7) | 104 (23) | 33 (9) |
| Age (Years) | |||
| ≤40 | 49 (42) | 253 (57) | 190 (51) |
| >40 | 67 (58) | 191 (43) | 181 (49) |
| Race / Ethnicity | |||
| White, Non-Hispanic | 57 (50) | 300 (68) | 166 (44) |
| African American, Non-Hispanic | 53 (46) | 118 (27) | 183 (49) |
| Other | 4 (4) | 26 (6) | 25 (7) |
| Occupation | |||
| Nurse | 48 (41) | -- | -- |
| Health Educator | 70 (59) | -- | -- |
Note. Totals may be less than stated sample size due to missing data. Dashes (--) indicate item was not applicable.
Figure 1.
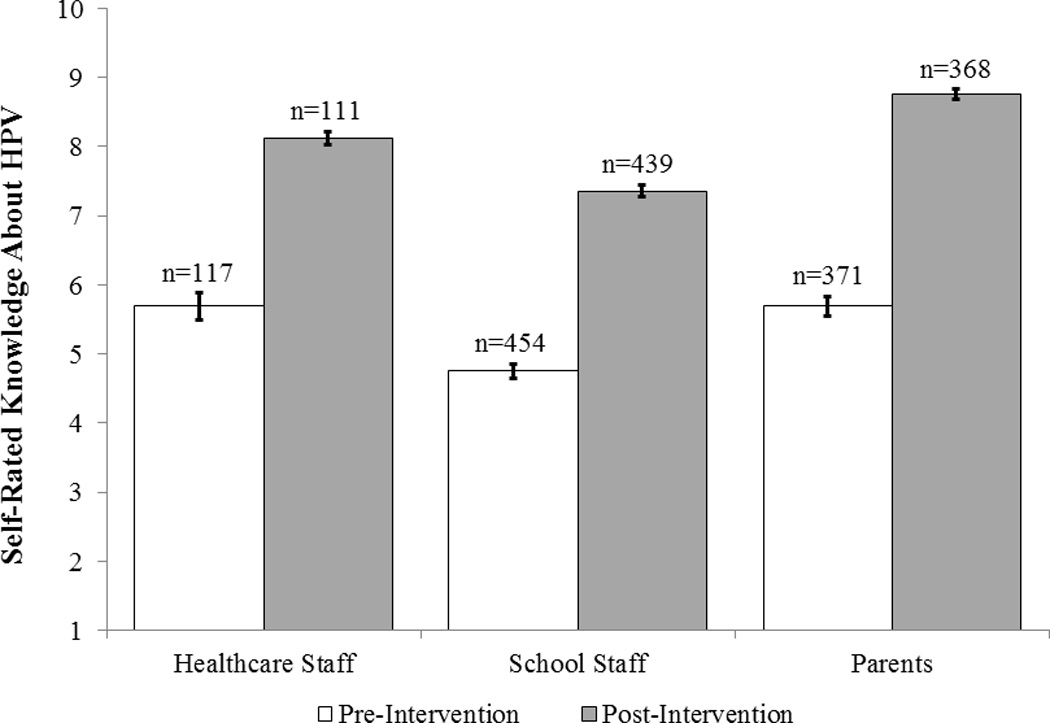
Self-rated knowledge about HPV. Parents self-rated their current knowledge and estimated their knowledge before the educational presentation in post-intervention surveys. Bars indicate standard errors.
Table 3.
HPV and HPV vaccine knowledge pre- and post-intervention (n correct / n total (%))
| Healthcare Staff | School Staff | |||
|---|---|---|---|---|
| Pre | Post | Pre | Post | |
| Number of new HPV cases each year in the USa | 36/115 (31) | 99/116 (85)** | 169/445 (38) | 393/452 (87)** |
| Percent of new HPV cases that occur in 15–24 year oldsa | 69/117 (59) | 111/117 (95)** | 228/446 (51) | 405/454 (89)** |
| Percent of cervical cancers where HPV can be founda | 24/118 (20) | 97/116 (84)** | 54/443 (12) | 311/450 (69)** |
| Vaccine is effective in virus-naïve females but does not protect against or treat existing infections | 90/117 (77) | 113/117 (97)** | 347/443 (78) | 437/449 (97)** |
| Half of cervical cancer cases between ages 35–50 were likely exposed to HPV in teens or early twenties | 113/118 (96) | 117/118 (99) | 408/442 (92) | 443/450 (98)** |
| A woman dies every 2.5 hours from cervical cancer in the US | 91/118 (77) | 103/118 (87)* | -- | -- |
| Regular Pap smear tests are no longer needed after HPV vaccinationb | 115/118 (97) | 117/117 (100) | -- | -- |
Note. Analyses used mixed regression models since participants were clustered within education sessions. Sample sizes differ due to missing data. Dashes (--) indicate item was not assessed.
Multiple choice item with responses scored as “correct” or “incorrect”. All other items used a true/false response scale.
Correct response was “false”.
p<0.05,
p<0.001
Healthcare staff members tended to hold positive beliefs about HPV vaccine. Most would choose to vaccinate their daughters against HPV if they were in the vaccine’s approved age range (pre=86%, post=91%, p=0.21) and thought community education on HPV and HPV vaccine is valuable (pre=98%, post=100%, p value could not be calculated) (Table 4).
Table 4.
Beliefs pre- and post-intervention (n endorsed / n total (%))
| Healthcare Staff | School Staff | Parents | |||
|---|---|---|---|---|---|
| Pre | Post | Pre | Post | Post | |
| Community education on HPV and HPV vaccine is valuable | 113/115 (98) | 105/105 (100) | -- | -- | -- |
| Would choose to vaccinate daughter if they had one in the approved age range for HPV vaccine | 90/105 (86) | 90/99 (91) | -- | -- | -- |
| HPV and HPV vaccine education is worthwhile for school personnel | -- | -- | 356/446 (80) | 405/447 (91)** | -- |
| Middle schools are an appropriate venue for HPV and HPV vaccine education | -- | -- | 382/446 (86) | 407/445 (91)* | -- |
| Would be supportive of a school-based vaccination clinic | -- | -- | 344/435 (79) | 373/438 (85)* | 280/288 (97) |
Note. Analyses used mixed regression models since participants were clustered within education sessions. Sample sizes differ due to missing data. Dashes (--) indicate item was not assessed.
p<0.05,
p<0.001
School staff
Most school staff members were female (77%), 40 years of age or younger (57%), and non-Hispanic white (68%). About a quarter were non-Hispanic African American (27%) (Table 2). School staff members rated their HPV knowledge higher following the intervention (mean=7.36, SD=1.79) than before (mean=4.75, SD=2.36, p<0.001) (Figure 1). The education intervention also increased the proportion of staff members who answered HPV knowledge items correctly (Table 3). Compared to pre-intervention surveys, more staff members responded correctly following the intervention that there are about 6 million new HPV cases in the US each year (38% vs. 87%, p<0.001), that 74% of these new cases occur among 15–24 year olds (51% vs. 89%, p<0.001), that HPV can be found in 99% of cervical cancer cases (12% vs. 69%, p<0.001), that HPV vaccine will not protect against or treat existing infections (78% vs. 97%, p<0.001), and that half of cervical cancer cases between ages 35–50 were exposed to HPV in their teens or early twenties (92% vs. 98%, p<0.001).
Although school staff members tended to support HPV education and vaccination programs prior to the intervention, a higher proportion believed post-intervention that HPV and HPV vaccine education is worthwhile for school personnel (80% vs. 91%, p<0.001), that middle schools are an appropriate venue for such education (86% vs. 91%, p<0.05), and would be supportive of school-based vaccination clinics (79% vs. 85%, p<0.05) (Table 4). More school staff members reported after the intervention that they felt comfortable or confident enough in their knowledge to talk about HPV if approached by a student (14% vs. 42%, p<0.001), and about the same proportion would advise the student to talk with a parent (32% vs. 33%, p=0.60). After the intervention, fewer would need to refer the student to the school nurse (77% vs. 57%, p<0.001). Only two staff members indicated on their pre-intervention surveys they would tell the student they are too young to be concerned with such things; none indicated this on post-intervention surveys.
Parents
Most parents were female (91%), 40 years of age or younger (51%), and non-Hispanic white (44%) or non-Hispanic African American (49%) (Table 2). About 31% (115/354) of parents indicated they had daughters who had already received at least one dose of HPV vaccine. After the intervention, parents recalled having moderate self-rated knowledge about HPV prior to the intervention (mean=5.69, SD=2.76); they offered higher self-ratings of their HPV knowledge following the intervention (mean=8.76, SD=1.32, p<0.001) (Figure 1). Most parents indicated they would be supportive of a school-based vaccination clinic (97%) (Table 4).
Comparisons across groups
School staff members reported lower self-rated HPV knowledge on both pre- (compared to both parents and healthcare staff) and post-intervention (compared to parents) surveys (all p<0.05) (Figure 1). Self-rated knowledge among parents did not differ from that of healthcare staff on pre- or post-intervention surveys (both p>0.05). While all groups experienced an increase in self-rated knowledge, the largest increase was seen among parents, with healthcare and school staff experiencing smaller increases (p<0.05).
Discussion
HPV vaccination rates among adolescent females in the US continue to lag behind other developed countries (4, 10–12). Thus, it is important to implement intervention strategies to improve vaccine uptake. Given relatively low HPV and HPV vaccine knowledge levels observed among parents and healthcare providers (18–21, 24–27), education interventions represent a simple and promising, yet underexplored, strategy. The few education interventions conducted among parents, adult women, or students have produced encouraging results (28–33), yet such interventions have not included other potentially influential groups.
Similar to these past interventions (28–33), our education intervention increased actual HPV and HPV vaccine knowledge levels among participants. For most knowledge items in our surveys, higher proportions of healthcare staff and school staff members answered correctly post-intervention compared to pre-intervention. Interestingly, the items most frequently missed during pre-intervention surveys were similar for these two groups (i.e., knowing how common HPV infections are, the age distribution of infections, and the percent of cervical cancer cases where HPV can be found). Past studies have also shown that healthcare providers often lack knowledge about some epidemiological aspects of HPV and HPV-related disease (24, 27). Future education programs are needed for these groups, and a brief education session may be sufficient to provide the necessary information about HPV and HPV vaccine.
In addition to actual knowledge, our intervention also increased the self-rated knowledge about HPV among parents, healthcare staff, and school staff. It is important that members of these groups feel confident in making informed decisions regarding HPV vaccination. Interestingly, school staff members tended to report lower self-rated knowledge compared to parents and healthcare staff. As school-based HPV vaccination programs continue to develop in the US (13), it becomes increasingly important to ensure that school staff members feel (and are) knowledgeable about HPV and how it affects adolescents. To our knowledge, our study provides important initial insight into what this group currently knows about HPV and HPV vaccine.
Following the intervention, over 90% of school staff members believed HPV and HPV vaccine education is worthwhile for school personnel and that middle schools are an appropriate venue for this education. Furthermore, about 85% would be supportive of a school-based vaccination clinic, which is encouraging since school staff support is critical to the success of any school-based vaccination program. In fact, one of the main lessons learned from the few existing school-based HPV vaccination programs in the US is the importance of forming an open and honest partnership with the school systems (13). Parents were also very supportive of a school-based vaccination clinic following their education sessions, which is consistent with our past research showing many mothers were willing to get their adolescent daughters HPV vaccine at school (37). Taken together, our findings suggest that having an education component as an initial part of school-based HPV vaccination programs may garner even stronger support for the programs among parents and school staff, two important stakeholders in determining the success of such programs. Future research is needed to further examine the acceptability of school-based vaccination programs, particularly among school staff, and what factors influence whether US schools adopt such programs.
Our study had many strengths including focusing on three key groups important to vaccinating adolescent females against HPV, using various strategies to increase attendance at education sessions, and using an advisory team to assist with intervention development and implementation. Limitations include conducting education sessions among convenience samples in only one county in North Carolina, having relatively few male participants, and not having physicians as part of the healthcare staff group. We also did not conduct a pre-intervention survey for parents, instead asking them to self-rate their current HPV knowledge and estimate their knowledge before the educational presentation on post-intervention surveys. Some parents who completed surveys may not have had female children in the approved age range for HPV vaccination, as these sessions were open to anyone interested in attending. Since one-group pre- and post-study designs may overstate effect sizes (38), it is important for future controlled studies to confirm our findings.
An important first step in increasing HPV vaccination rates among adolescent females in the US is to improve knowledge levels among key groups influential to the adolescents’ vaccination behaviors. In this study, we demonstrated that a simple education intervention greatly improved objectively assessed and self-rated HPV and HPV vaccine knowledge levels among parents, healthcare staff, and school staff members. Such interventions offer a relatively low effort and potentially effective strategy for increasing HPV vaccination. Future research is needed to determine if education interventions affect vaccine uptake.
Acknowledgments
Financial Support: The Duke Endowment provided generous funding for the intervention and in-kind contributions from the Guilford County Department of Public Health supplemented. We received additional support from the American Cancer Society (MSRG-06-259-01-CPPB) and the Cancer Control Education Program at UNC Lineberger Comprehensive Cancer Center (R25 CA57726).
Footnotes
Conflicts of Interest: Authors have received research grants from Merck Sharp & Dohme Corp. (NB, PR) and GlaxoSmithKline (NB). NB has also received grants and/or honoraria from GlaxoSmithKline and Merck Sharp & Dohme Corp. PR has not received honoraria or consulting fees from these companies. These funds were not used to support this research study.
References
- 1.Centers for Disease Control and Prevention (CDC) FDA licensure of bivalent human papillomavirus vaccine (HPV2, Cervarix) for use in females and updated HPV vaccination recommendations from the Advisory Committee on Immunization Practices (ACIP) MMWR Morb Mortal Wkly Rep. 2010;59(20):626–629. [PubMed] [Google Scholar]
- 2.Smith JS, Lindsay L, Hoots B, Keys J, Franceschi S, Winer R, et al. Human papillomavirus type distribution in invasive cervical cancer and high-grade cervical lesions: a meta-analysis update. Int J Cancer. 2007;121(3):621–632. doi: 10.1002/ijc.22527. [DOI] [PubMed] [Google Scholar]
- 3.U.S. Food and Drug Administration. December 22, 2010 approval letter - Gardasil. Available from: http://www.fda.gov/BiologicsBloodVaccines/Vaccines/ApprovedProducts/ucm238074.htm.
- 4.Centers for Disease Control and Prevention (CDC) National and state vaccination coverage among adolescents aged 13–17 years --- United States, 2010. MMWR Morb Mortal Wkly Rep. 2011;60(33):1117–1123. [PubMed] [Google Scholar]
- 5.McRee AL, Reiter PL, Brewer NT. Vaccinating adolescent girls against human papillomavirus-who decides? Prev Med. 2010;50(4):213–214. doi: 10.1016/j.ypmed.2010.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reiter PL, Cates JR, McRee AL, Gottlieb SL, Shafer A, Smith JS, et al. Statewide HPV vaccine initiation among adolescent females in North Carolina. Sex Transm Dis. 2010;37(9):549-–556. doi: 10.1097/OLQ.0b013e3181d73bf8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rosenthal SL, Weiss TW, Zimet GD, Ma L, Good MB, Vichnin MD. Predictors of HPV vaccine uptake among women aged 19–26: importance of a physician's recommendation. Vaccine. 2011;29(5):890–895. doi: 10.1016/j.vaccine.2009.12.063. [DOI] [PubMed] [Google Scholar]
- 8.Reiter PL, Brewer NT, Gottlieb SL, McRee AL, Smith JS. Parents’ health beliefs and HPV vaccination of their adolescent daughters. Soc Sci Med. 2009;69(3):475–480. doi: 10.1016/j.socscimed.2009.05.024. [DOI] [PubMed] [Google Scholar]
- 9.Dempsey AF, Abraham LM, Dalton V, Ruffin M. Understanding the reasons why mothers do or do not have their adolescent daughters vaccinated against human papillomavirus. Ann Epidemiol. 2009;19(8):531–538. doi: 10.1016/j.annepidem.2009.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brabin L, Roberts SA, Stretch R, Baxter D, Chambers G, Kitchener H, et al. Uptake of first two doses of human papillomavirus vaccine by adolescent schoolgirls in Manchester: prospective cohort study. BMJ. 2008;336(7652):1056–1058. doi: 10.1136/bmj.39541.534109.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brotherton JM, Deeks SL, Campbell-Lloyd S, Misrachi A, Passaris I, Peterson K, et al. Interim estimates of human papillomavirus vaccination coverage in the school-based program in Australia. Commun Dis Intell. 2008;32(4):457–461. doi: 10.33321/cdi.2008.32.45. [DOI] [PubMed] [Google Scholar]
- 12.Reeve C, De La Rue S, Pashen D, Culpan M, Cheffins T. School-based vaccinations delivered by general practice in rural north Queensland: an evaluation of a new human papilloma virus vaccination program. Commun Dis Intell. 2008;32(1):94–98. doi: 10.33321/cdi.2008.32.14. [DOI] [PubMed] [Google Scholar]
- 13.Hayes KA, Entzel P, Berger W, Caskey RN, Shlay JC, Stubbs BW, et al. Early lessons learned from extramural vaccination programs that offer HPV vaccine in US schools. Working Paper. doi: 10.1111/josh.12007. [DOI] [PubMed] [Google Scholar]
- 14.Brener ND, Wheeler L, Wolfe LC, Vernon-Smiley M, Caldart-Olson L. Health services: Results from the school health policies and programs study 2006. J Sch Health. 2007;77(8):464–485. doi: 10.1111/j.1746-1561.2007.00230.x. [DOI] [PubMed] [Google Scholar]
- 15.Weinstein ND. The precaution adoption process. Health Psychol. 1988;7(4):355–386. doi: 10.1037//0278-6133.7.4.355. [DOI] [PubMed] [Google Scholar]
- 16.Glanz K, Rimer BK, Viswanath K. Health behavior and health education: theory, research, and practice. Fourth edition. San Francisco, CA: Jossey-Bass; 2008. [Google Scholar]
- 17.Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol. 2008;27(3):379–387. doi: 10.1037/0278-6133.27.3.379. [DOI] [PubMed] [Google Scholar]
- 18.Tiro JA, Meissner HI, Kobrin S, Chollette V. What do women in the U.S. know about human papillomavirus and cervical cancer? Cancer Epidemiol Biomarkers Prev. 2007;16(2):288–294. doi: 10.1158/1055-9965.EPI-06-0756. [DOI] [PubMed] [Google Scholar]
- 19.Pruitt SL, Parker PA, Peterson SK, Le T, Follen M, Basen-Engquist K. Knowledge of cervical dysplasia and human papillomavirus among women seen in a colposcopy clinic. Gynecol Oncol. 2005;99(3 Suppl 1):S236–S244. doi: 10.1016/j.ygyno.2005.07.095. [DOI] [PubMed] [Google Scholar]
- 20.Fazekas KI, Brewer NT, Smith JS. HPV vaccine acceptability in a rural southern area. J Womens Health (Larchmt) 2008;17(4):539–548. doi: 10.1089/jwh.2007.0489. [DOI] [PubMed] [Google Scholar]
- 21.Allen JD, Othus MK, Shelton RC, Li Y, Norman N, Tom L, et al. Parental decision making about the HPV vaccine. Cancer Epidemiol Biomarkers Prev. 2010;19(9):2187–2198. doi: 10.1158/1055-9965.EPI-10-0217. [DOI] [PubMed] [Google Scholar]
- 22.Read DS, Joseph MA, Polishchuk V, Suss AL. Attitudes and perceptions of the HPV vaccine in Caribbean and African-American adolescent girls and their parents. J Pediatr Adolesc Gynecol. 2010;23(4):242–245. doi: 10.1016/j.jpag.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 23.Brewer NT, Gottlieb SL, Reiter PL, McRee AL, Liddon N, Markowitz L, et al. Longitudinal predictors of human papillomavirus vaccine initiation among adolescent girls in a high-risk geographic area. Sex Transm Dis. 2011;38(3):197–204. doi: 10.1097/OLQ.0b013e3181f12dbf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Daley MF, Crane LA, Markowitz LE, Black SR, Beaty BL, Barrow J, et al. Human papillomavirus vaccination practices: a survey of US physicians 18 months after licensure. Pediatrics. 2010;126(3):425–433. doi: 10.1542/peds.2009-3500. [DOI] [PubMed] [Google Scholar]
- 25.Henderson Z, Irwin KL, Montano DE, Kasprzyk D, Carlin L, Greek A, et al. Anogenital warts knowledge and counseling practices of US clinicians: results from a national survey. Sex Transm Dis. 2007;34(9):644–652. doi: 10.1097/01.olq.0000258434.08035.ca. [DOI] [PubMed] [Google Scholar]
- 26.Jain N, Irwin KL, Montano D, Kasprzyk D, Carlin L, Freeman C, et al. Family physicians' knowledge of genital human papillomavirus (HPV) infection and HPV-related conditions, United States, 2004. Fam Med. 2006;38(7):483–489. [PubMed] [Google Scholar]
- 27.Riedesel JM, Rosenthal SL, Zimet GD, Bernstein DI, Huang B, Lan D, et al. Attitudes about human papillomavirus vaccine among family physicians. J Pediatr Adolesc Gynecol. 2005;18(6):391–398. doi: 10.1016/j.jpag.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 28.Lambert EC. College students' knowledge of human papillomavirus and effectiveness of a brief educational intervention. J Am Board Fam Pract. 2001;14(3):178–183. [PubMed] [Google Scholar]
- 29.Dempsey AF, Zimet GD, Davis RL, Koutsky L. Factors that are associated with parental acceptance of human papillomavirus vaccines: a randomized intervention study of written information about HPV. Pediatrics. 2006;117(5):1486–1493. doi: 10.1542/peds.2005-1381. [DOI] [PubMed] [Google Scholar]
- 30.Papa D, Moore Simas TA, Reynolds M, Melnitsky H. Assessing the role of education in women's knowledge and acceptance of adjunct high-risk human papillomavirus testing for cervical cancer screening. J Low Genit Tract Dis. 2009;13(2):66–71. doi: 10.1097/LGT.0b013e31818a53f0. [DOI] [PubMed] [Google Scholar]
- 31.Gottvall M, Tyden T, Hoglund AT, Larsson M. Knowledge of human papillomavirus among high school students can be increased by an educational intervention. Int J STD AIDS. 2010;21(8):558–562. doi: 10.1258/ijsa.2010.010063. [DOI] [PubMed] [Google Scholar]
- 32.Kwan TT, Tam KF, Lee PW, Chan KK, Ngan HY. The effect of school-based cervical cancer education on perceptions towards human papillomavirus vaccination among Hong Kong Chinese adolescent girls. Patient Educ Couns. 2011;84(1):118–122. doi: 10.1016/j.pec.2010.06.018. [DOI] [PubMed] [Google Scholar]
- 33.Kennedy A, Sapsis KF, Stokley S, Curtis CR, Gust D. Parental attitudes toward human papillomavirus vaccination: evaluation of an educational intervention, 2008. J Health Commun. 2011;16(3):300–313. doi: 10.1080/10810730.2010.532296. [DOI] [PubMed] [Google Scholar]
- 34.North Carolina State Center for Health Statistics. Cervical cancer mortality rates. 2000–2009. [Google Scholar]
- 35.Stubbs B, Panozzo CA, Reiter PL, Whitesell D, Brewer NT. Evaluation of a school-located HPV vaccine intervention in Guilford County, North Carolina. Working Paper [Google Scholar]
- 36.Markowitz LE, Dunne EF, Saraiya M, Lawson HW, Chesson H, Unger ER, et al. Quadrivalent human papillomavirus vaccine: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2007;56(RR-2):1–24. [PubMed] [Google Scholar]
- 37.Kadis JA, McRee AL, Gottlieb SL, Lee MR, Reiter PL, Dittus PJ, et al. Mothers' support for voluntary provision of HPV vaccine in schools. Vaccine. 2011;29(14):2542–2547. doi: 10.1016/j.vaccine.2011.01.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lipsey MW, Wilson DB. The efficacy of psychological, educational, and behavioral treatment. Confirmation from meta-analysis. Am Psychol. 1993;48(12):1181–1209. doi: 10.1037//0003-066x.48.12.1181. [DOI] [PubMed] [Google Scholar]


