Abstract
Objective
Bile duct injury is an uncommon but potentially serious complication in cholecystectomy. A recognized treatment for minor biliary injury is internal biliary decompression by endoscopic retrograde cholangiopancreatography (ERCP) and stent insertion. The aim of this study was to assess the effectiveness of ERCP in the management of minor biliary injuries.
Methods
A retrospective review of medical records at a tertiary referral centre identified 36 patients treated for postoperative minor biliary injuries between 2006 and 2010. Management involved establishing a controlled biliary fistula followed by ERCP to confirm the nature of the injury and decompress the bile duct with stent insertion.
Results
Controlled biliary fistulae were established in all 36 patients. Resolution of the bile leak was achieved prior to ERCP in seven patients, and ERCP with stent insertion was successful in 27 of the remaining 29 patients. Resolution of the bile leak was achieved in all patients without further intervention. The median time to resolution after successful ERCP was 4 days. Two patients underwent ERCP complicated by mild pancreatitis. No other complications were seen.
Conclusions
This review confirms that postoperative minor biliary injuries can be managed by sepsis control and semi-urgent endoscopic biliary decompression.
Keywords: endoscopy, cholelithiasis, bile duct injury, cholecystectomy, biliary fistula
Introduction
Cholelithiasis is common in Western populations and occurs at an incidence of 15–20%.1 Of patients with cholelithiasis, 1–2% per year develop gallstone-related symptoms.2 Laparoscopic cholecystectomy is currently the preferred method of treating symptomatic or complicated cholelithiasis.
Bile duct injury is a significant complication of cholecystectomy. Some authors have reported a higher incidence of biliary injury since the introduction of laparoscopic cholecystectomy.3–5 Large studies published in the last decade have demonstrated incidences of major and minor biliary injury of 0.25–1.90% and 0.38–1.20%, respectively.6–8
There are several classification systems designed to grade the severity of biliary tree injury.5 Minor injuries are usually defined as those of the cholecystohepatic duct (duct of Lushka), partial disruption of the right posterior sectoral duct, injuries to small subsegmental ducts in the gallbladder bed and cystic duct stump leaks. Major biliary injuries are those of the common hepatic duct, common bile duct (CBD), right hepatic duct and transection of the right posterior sectoral duct. It is generally accepted that minor biliary injuries can be managed endoscopically, but major injuries require biliary reconstruction.9,10
A postoperative bile leak is usually diagnosed within the first few postoperative days.4,11–13 It most commonly presents with excessive postoperative pain or bilious drain tube output.14 Less common presenting features include sepsis, cutaneous bile staining (Fig. 1) and bile discharge from cannula sites. The diagnosis requires no further confirmation in the presence of bile within the drain fluid; however, if no drain was placed at operation, cross-sectional imaging or, occasionally, a hepatobiliary imino-diacetic acid (HIDA) nuclear scan12 will be required. Imaging should be directed at excluding a major biliary injury. It is the practice of this unit to use an early computed tomography (CT) i.v. cholangiogram (CT-ivC). This allows the presence of undrained intraperitoneal bile to be assessed, but may also identify a major biliary injury if one is present. Major biliary injuries should be assessed for operative repair.
Figure 1.

Subcutaneous bile staining from postoperative minor biliary injury
The greatest cause of early morbidity and mortality in patients with minor biliary injury is uncontrolled sepsis. Early management should be directed towards sepsis control.15–17 A controlled biliary fistula can be created by percutaneous drainage or with laparoscopic washout and drain insertion. Laparoscopic washout facilitates more thorough clearance of intraperitoneal bile (particularly if there are multifocal or loculated collections), as well as more accurate drain placement adjacent to the gallbladder fossa and cystic duct stump. Very occasionally, early laparoscopy allows visualization of the cystic duct stump, the cystic stump clips or the presence of a leak from the gallbladder bed.
The establishment of a controlled biliary fistula allows time for the patient's physiology to recover and for the careful planning of further treatment. Although small subgroups of patients may resolve spontaneously, the majority go on to require endoscopic intervention.8,17,18
Anatomical delineation can be achieved with magnetic resonance cholangiopancreatography (MRCP), CT-ivC or endoscopic retrograde cholangiopancreatography (ERCP). The first of these, MRCP, has been reported to have a sensitivity of 84–100%19–21 in diagnosing postoperative biliary injuries; however, ERCP allows the identification of the site of bile leak and, most importantly, allows internal biliary drainage if the diagnosis of minor biliary injury is confirmed.12 Incidental diagnoses such as choledocholithiasis or bile duct stricture may also be treated in a single procedure. However, ERCP does not delineate injuries in which a duct has been transected and cannot be filled with contrast material from below.22 A low threshold for further imaging with MRCP or CT-ivC should be applied to patients in whom resolution is not rapidly achieved after ERCP to avoid missing these injuries.
The aim of this study is to describe the experience of a tertiary hepatobiliary referral centre with consecutive patients treated over a 5-year period for minor post-cholecystectomy biliary injury.
Materials and methods
Medical records for all patients treated for minor biliary injuries at St Vincent's Hospital, Melbourne, Victoria, during 2006–2010 were reviewed. Patients were identified by an electronic search of discharge diagnosis. Reports of ERCP for the same period were also reviewed in a strategy to identify patients with a diagnosis of bile leak. St Vincent's Hospital is a tertiary referral centre for ERCP.
Patient demographics were recorded, along with operative details, time until diagnosis, method of sepsis control, time until ERCP and time until resolution of bile leak. Complications emanating from the management of the biliary injury were also recorded. Major biliary injuries were excluded from further analysis.
Figure 2 describes the management algorithm for patients presenting with suspected biliary injury. Patients in whom drain placement at the time of operation had controlled the bile leak proceeded to ERCP. Patients with undrained, intraperitoneal bile were managed with washout and drain insertion at laparoscopy or laparotomy (if the original operation had been conducted by laparotomy). Radiologically guided percutaneous drainage was used early in the study period in patients if a single accessible biloma was identified on imaging and ERCP was scheduled following this. In some patients, bilious drain tube output ceased prior to ERCP. In this group the drain was left for 1 or 2 days to ensure no further bile drainage, but no endoscopy was performed.
Figure 2.
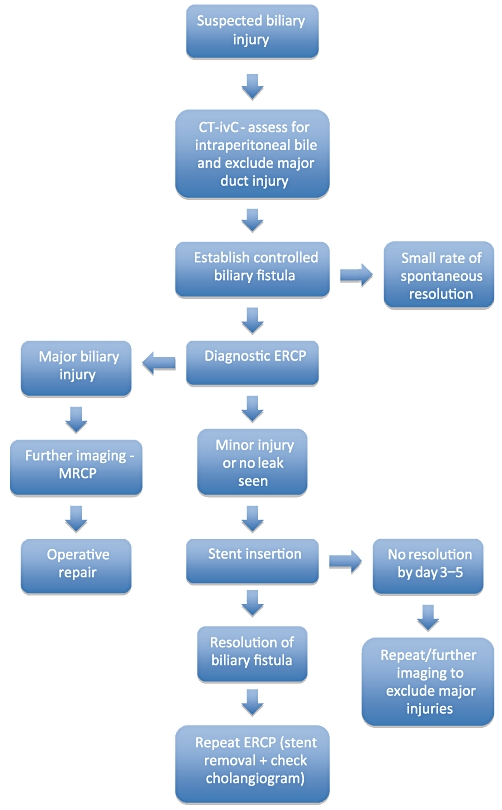
Management algorithm for minor biliary injury. CT-ivC, computed tomography i.v. cholangiogram; ERCP, endoscopic retrograde cholangiopancreatography; MRCP, magnetic resonance cholangiopancreatography
Endoscopic retrograde cholangiopancreatography was performed under conscious sedation or general anaesthesia administered by anaesthesia staff. Selective cannulation of the CBD was attempted using a 0.035-inch hydrophilic guidewire (Boston Scientific Corp., Natick, MA, USA). If initial attempts at cannulation were unsuccessful, a sphincterotomy was performed using a needle knife to cut down through the ampulla and facilitate access to the biliary tree. Cholangiography was used to assess for evidence of biliary leakage and the site of leakage. Following cholangiography, a removable plastic biliary stent was inserted to allow anterograde drainage. The use of sphincterotomy and the type of stent used were not controlled during the study period. Any other abnormal findings at ERCP (e.g. retained stones) were treated as required.
Rapid resolution was expected after stent insertion. If bilious drain tube output had not markedly reduced by day 3–5, further imaging with CT-ivC or MRCP was performed to ensure that no major biliary injury or transected duct had been missed.
Repeat ERCP was performed at least 4 weeks after resolution of the biliary leak. Cholangiography was used to confirm the healing of the biliary fistula and the absence of a biliary stricture or other pathology such as choledocholithiasis. If the cholangiogram was normal, the plastic stent was removed.
On retrospective chart review it was not always possible to determine the exact day on which bile was no longer seen in the drain tube collecting system and therefore time until drain removal was used as a surrogate for time until the resolution of bile leak. It should be noted, however, that drains were often left for 1 or 2 days after cessation of bile output as a precaution.
All data are presented as medians (ranges) unless stated. Nominal data are presented as fractions. Statistical analysis for patient groups was performed using the Mann–Whitney U-test for non-parametric data.
Results
Thirty-six patients with minor post-cholecystectomy bile leaks were treated during the study period. Their median age was 52 years (range: 16–78 years) and 22 patients were female.
Laparoscopic cholecystectomy represented the procedure originally planned in all patients. Fourteen patients underwent an elective procedure for the management of biliary colic and 22 underwent emergency cholecystectomy for acute cholecystitis. Nine patients required conversion to open cholecystectomy as a result of intraoperative difficulties. Intraoperative cholangiography was attempted in 22 patients and was successful in 20. In no patient was a bile leak recognized at operative cholangiography. In no patient were bile duct stones identified. A drain was placed on completion of the procedure in 32 patients.
Post-cholecystectomy bile leaks were detected after a median of 4 days (range: 0–19 days). Modes of presentation are listed in Table 1.
Table 1.
Presentation of post-cholecystectomy bile leaks in the current series (n = 36)
| Symptom | n |
|---|---|
| Bile in drain tube | 13 |
| Abdominal pain | 12 |
| Abdominal sepsis | 10 |
| Subcutaneous bile stain | 1 |
The initial management of biliary sepsis and the method of establishing a controlled biliary fistula were not controlled during the study period. Thirteen patients presented with a controlled bile leak via the drain placed at cholecystectomy. In the remaining 23 patients, a controlled biliary fistula was created in 15, four and four patients by laparoscopy, laparotomy and percutaneous drain, respectively. Percutaneous drain was used in four patients early in the study period. These patients demonstrated a single, accessible, well-localized, intra-abdominal collection without evidence of systemic sepsis.
After sepsis control and drainage of intraperitoneal bile, a semi-elective ERCP was arranged. Spontaneous resolution of biliary leak prior to ERCP occurred in seven patients. In the remaining 29 patients, ERCP was attempted at a median of 8 days (range: 1–35 days) following cholecystectomy. The results of ERCP are shown in Table 2.
Table 2.
Results of endoscopic retrograde cholangiopancreatography (ERCP) (n = 29)
| Result | n |
|---|---|
| Successful cannulation at ERCP | 27/29 |
| Leak visualized | 16/27 |
| Cystic duct stump | 14/16 |
| Segment IV/V duct leak | 2/16 |
| Other pathology | 7/27 |
| Choledocholithiasis | 7/27 |
| Stricture | 0/27 |
| Intervention | 27/27 |
| Sphincterotomy | 17/27 |
| Stent insertion | 27/27 |
| 7-Fr stent | 9/27 |
| 10-Fr stent | 18/27 |
| Complications | |
| Post-ERCP pancreatitis | 2/29 |
The median time to resolution of the bile leak in the entire group was 4 days (range: 1–35 days) from the last intervention. In the seven patients who did not require ERCP, drain tubes were removed at a median of 8 days (range: 2–15 days) post-cholecystectomy. A total of 29 patients underwent ERCP. In 27 of these patients, drain tubes were removed at a median of 4 days (range: 1–35 days) after successful ERCP. In the two patients in whom ERCP failed, the ampulla could not be cannulated at endoscopy and therefore no stent was inserted. Drains were removed at a median of 17.5 days (range: 7–28 days) after ERCP in these patients.
The median time to resolution was 4 days (range: 2–25 days) in patients undergoing endoscopic sphincterotomy (n = 17) and 4 days (range: 1–27 days) in those without sphincterotomy (n = 10) (P = 0.549).
The median time to resolution was 8 days (range: 2–16 days) after insertion of a 7-Fr stent (n = 9) and 4 days (range: 1–35 days) after insertion of a 10-Fr stent (n = 18) (P = 0.267).
Two episodes of post-ERCP pancreatitis occurred in the study group. Both episodes were mild and resolved without further operative intervention.
Patients treated with stent insertion underwent stent removal and repeat cholangiogram at a median of 69 days (range: 29–183 days). No persisting leaks and no strictures were seen at repeat ERCP. Stones were removed in one patient found to have choledocholithiasis. No complications occurred in this second procedure.
Discussion
Minor biliary tree injury is a common complication of laparoscopic cholecystectomy and is reported to occur at an incidence of up to 1.2%.6–8 With improper treatment, these injuries represent an iatrogenic catastrophe with the potential to reduce the patient's quality of life and cause serious longterm morbidity and mortality, and are associated with high rates of litigation.5
Endoscopic management of minor biliary tree injuries has a very high rate of success with minimal additional morbidity (Table 3). As this study shows, sepsis control followed by internal drainage results in the rapid resolution of these injuries without the need for an additional operation. Endoscopic retrograde cholangiopancreatography can be used to diagnose the site of biliary leakage and to overcome the pressure gradient at the ampulla of Vater in order to allow bile to flow into the duodenum and away from the site of bile leak. This allows for the healing of the affected biliary segment.
Table 3.
Endoscopic management of minor biliary injury
| Study | n | Successful ERCP | Days to resolution | Complication rate | Further intervention |
|---|---|---|---|---|---|
| Present study | 29 | n = 27 | 4 | n = 2/29 | n = 0 |
| Donnellan et al.24 | 48 | n = 44 | 5 | n = 0 | n = 0 |
| Tzovaras et al.26 | 20 | n = 19 | NA | n = 1 | n = 1 |
| Familiari et al.35 | 85 | 96.3% | NA | 2.9% | 2.3% |
| Mavrogiannis et al.31 | 52 | 100% | 2–4 | 7.7% | 0% |
| Katsinelos et al.14 | 60 | 94% | NA | 13% | 1.6% |
NA, not available
Seven patients in this series showed resolution of the bile leak prior to ERCP. Other series also show low rates of spontaneous resolution.8,17,18 Unfortunately, the data in this series do not imply a method of distinguishing which patients require ERCP and there are no other useful published guidelines.8,18,23 Patients in whom rapid, spontaneous resolution is achieved are generally in the minority and therefore it is the authors’ practice to schedule ERCP in all patients and to cancel the procedure if the bile leak settles.
Endoscopic retrograde cholangiopancreatography does not always show the exact point of leakage in minor biliary injuries; however, the most common locations are the cystic duct stump and gallbladder fossa. This is confirmed by both the current study and previously published data (Table 4). If a major biliary injury is identified at ERCP, the patient should be referred for consideration of biliary reconstruction. If no cause for a bile leak is seen at ERCP, the patient should be referred for further imaging. An excluded biliary segment (after transection at cholecystectomy) will not be seen in retrograde cholangiography and this group of patients may be better diagnosed with MRCP or CT-ivC.
Table 4.
Distribution of minor biliary injuries
| Study | Cystic duct stump | Segment VI/V leak | Common hepatic duct |
|---|---|---|---|
| Present study | n = 14/27 | n = 2/27 | NA |
| Donnellan et al.24 | n = 19/44 | n = 11/44 | n = 5/44 |
| Tzovaras et al.26 | n = 16/20 | NA | n = 3/20 |
| Pinkas & Brady38 | n = 15/20 | n = 5/20 | NA |
| Familiari et al.35 | 75% | 22.3% | NA |
| Mavrogiannis et al.31 | 71.2% | NA | NA |
NA, not available
Intraoperative cholangiography was attempted in 22 of the patients in the present series. In none of these was the minor biliary injury detected. One reason for this is that most bile leaks occur through the cystic duct stump (Table 4) and obviously this diagnosis will not be seen on cholangiography. Thus, it is important to note that intraoperative cholangiography does not protect against and usually is not diagnostic of minor biliary injury.
It is probable that biliary tree injuries are more frequent in more difficult cholecystectomies.14,16,25,26 In the current series (n = 36), many surrogate markers for the degree of difficulty were identified frequently; these included emergent surgery for acute cholecystitis (n = 22/36), conversion to open operation (n = 9/36), failed cholangiogram (n = 2/20) and drain tube use (n = 32/36). Specific technical errors leading to biliary injury may be more likely to occur in more difficult procedures.14,26
Seven of the 27 patients in the current series in whom ERCP was performed were diagnosed with choledocholithiasis. Retained CBD stones can increase CBD pressure and perhaps promote clip slippage. Retained CBD stones may be a risk factor for cystic duct stump leak. Two of these seven patients underwent intraoperative cholangiography and thus stones were missed. The significance of this finding is unclear.
The importance of stent size and sphincterotomy in reducing the pressure gradient across the sphincter of Oddi remains controversial. Theoretically, a larger stent provides improved biliary drainage. A single randomized trial comparing 7-Fr and 10-Fr stents for this purpose showed a non-significant trend towards bile leak resolution with larger stents.14 In addition, non-resolution with 7-Fr stents was treated by the insertion of a larger stent. It is difficult to draw definitive conclusions from these data, but the current study also found a non-significant reduction in time to resolution with the use of larger stents.
There is little consensus on the role of sphincterotomy in combination with stent insertion in the management of these patients. When possible, avoiding a sphincterotomy minimizes risk for bleeding or perforation. Sphincterotomy is associated with an increase in complication rates of 7.3–9.8%27–29 and a mortality of up to 1.3%.27,30 In addition, sphincterotomy cannot be performed in patients with coagulopathy. Mavrogiannis et al.31 demonstrated no additional benefit from sphincterotomy in terms of leak resolution; however, they and other authors suggest there may be a higher incidence of pancreatitis without sphincterotomy.12,24,31–33 Earlier publications have reported sphincterotomy alone as a means of overcoming ampullary pressure, but have quoted a biliary leak resolution rate of only 87.1%.34 This is inadequate when compared with the findings of other reports using stents (Table 3) and both Aksoz et al. and Familiari et al. report that up to 12% of patients require subsequent stent insertion after sphincterotomy alone.34,35
The current policy in this unit is to use large-bore (10-Fr) stent insertion alone and to use sphincterotomy only for access or if an additional diagnosis such as choledocholithiasis is made and requires treatment. A short (5-cm) stent, which crosses the sphincter of Oddi, is all that is required. That it is not necessary to stent the leak point is supported by the current study and other published data.35
In this study, repeat cholangiography was performed at the time of stent removal, revealing choledocholithiasis in a single patient as the only positive finding. However, Cotéet al. reported pathology in 27.6% of their patients during follow-up.36 Routine follow-up cholangiography is likely to be useful in this population of patients in whom the risk for pathology is high, although it must be acknowledged that some centres have published good results of stent removal without cholangiography.37
Conclusions
Minor biliary injuries are relatively common following cholecystectomy. This diagnosis should be suspected in any patient who does not make a rapid postoperative recovery. The main treatment priorities are to exclude major biliary injury and then to ensure good drainage of bile in order to create a controlled external biliary fistula. Endoscopic retrograde cholangiopancreatography was useful for confirming the diagnosis of minor biliary injury and for definitive management with internal biliary drainage in all patients in this study. The issue of which technique of endoscopic drainage (particularly as it relates to the role of sphincterotomy and the choice of stent size) is best is still controversial, but ERCP in this setting can be performed with minimal morbidity.
Conflicts of interest
None declared.
References
- 1.Gurusamy KS, Samraj K. Cholecystectomy versus no cholecystectomy in patients with silent gallstones. Cochrane Database Syst Rev. 2007;(1) doi: 10.1002/14651858.CD006230.pub2. CD006230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stinton LM, Myers RP, Shaffer EA. Epidemiology of gallstones. Gastroenterol Clin North Am. 2010;39:157–169. doi: 10.1016/j.gtc.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 3.Connor S, Garden OJ. Bile duct injury in the era of laparoscopic cholecystectomy. Br J Surg. 2006;93:158–168. doi: 10.1002/bjs.5266. [DOI] [PubMed] [Google Scholar]
- 4.Kapoor VK. Management of bile duct injuries: a practical approach. Am Surg. 2009;75:1157–1160. [PubMed] [Google Scholar]
- 5.Lau WY, Lai EC. Classification of iatrogenic bile duct injury. Hepatobiliary Pancreat Dis Int. 2007;6:459–463. [PubMed] [Google Scholar]
- 6.Verma GR, Bose SM, Singh R, Singh G. Biliary mishaps in laparoscopic cholecystectomy. Trop Gastroenterol. 2002;23:38–40. [PubMed] [Google Scholar]
- 7.Karvonen J, Gullichsen R, Laine S, Salminen P, Gronroos JM. Bile duct injuries during laparoscopic cholecystectomy: primary and longterm results from a single institution. Surg Endosc. 2007;21:1069–1073. doi: 10.1007/s00464-007-9316-7. [DOI] [PubMed] [Google Scholar]
- 8.Nuzzo G, Giuliante F, Persiani R. [The risk of biliary ductal injury during laparoscopic cholecystectomy.] J Chir (Paris) 2004;141:343–353. doi: 10.1016/s0021-7697(04)95358-6. [DOI] [PubMed] [Google Scholar]
- 9.Holte K, Bardram L, Wettergren A, Rasmussen A. Reconstruction of major bile duct injuries after laparoscopic cholecystectomy. Dan Med Bull. 2010;57:4135. [PubMed] [Google Scholar]
- 10.Nordin A, Gronroos JM, Makisalo H. Treatment of biliary complications after laparoscopic cholecystectomy. Scand J Surg. 2011;100:42–48. doi: 10.1177/145749691110000108. [DOI] [PubMed] [Google Scholar]
- 11.Barkun AN, Rezieg M, Mehta SN, Pavone E, Landry S, Barkun JS, et al. Post-cholecystectomy biliary leaks in the laparoscopic era: risk factors, presentation, and management. McGill Gallstone Treatment Group. Gastrointest Endosc. 1997;45:277–282. doi: 10.1016/s0016-5107(97)70270-0. [DOI] [PubMed] [Google Scholar]
- 12.Carr-Locke AD. Biliary stenting alone versus biliary stenting plus sphincterotomy for the treatment of post-laparoscopic cholecystectomy bile leaks. Eur J Gastroenterol Hepatol. 2006;18:1053–1055. doi: 10.1097/01.meg.0000231751.50587.75. [DOI] [PubMed] [Google Scholar]
- 13.Diamantis T, Tsigris C, Kiriakopoulos A, Papalambros E, Bramis J, Michail P, et al. Bile duct injuries associated with laparoscopic and open cholecystectomy: an 11-year experience in one institute. Surg Today. 2005;35:841–845. doi: 10.1007/s00595-005-3038-z. [DOI] [PubMed] [Google Scholar]
- 14.Katsinelos P, Kountouras J, Paroutoglou G, Chatzimavroudis G, Germanidis G, Zavos C, et al. A comparative study of 10-Fr vs. 7-Fr straight plastic stents in the treatment of post-cholecystectomy bile leak. Surg Endosc. 2008;22:101–106. doi: 10.1007/s00464-007-9381-y. [DOI] [PubMed] [Google Scholar]
- 15.Sicklick JK, Camp MS, Lillemoe KD, Melton GB, Yeo CJ, Campbell KA, et al. Surgical management of bile duct injuries sustained during laparoscopic cholecystectomy: perioperative results in 200 patients. Ann Surg. 2005;241:786–792. doi: 10.1097/01.sla.0000161029.27410.71. discussion 786–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Joshi RM, Shetty TS, Singh R, Adhikari DR, Patil BP, Bhange SA. Biliary complications of cholecystectomy. Int Surg. 2008;93:251–256. [PubMed] [Google Scholar]
- 17.Singh V, Kacker LK, Sikora SS, Saxena R, Kapoor VK, Kaushik SP. Post-cholecystectomy external biliary fistula. Aust N Z J Surg. 1997;67:168–172. doi: 10.1111/j.1445-2197.1997.tb01933.x. [DOI] [PubMed] [Google Scholar]
- 18.Zerem E, Omerovic S. Minimally invasive management of biliary complications after laparoscopic cholecystectomy. Eur J Intern Med. 2009;20:686–689. doi: 10.1016/j.ejim.2009.07.010. [DOI] [PubMed] [Google Scholar]
- 19.Aduna M, Larena JA, Martin D, Martinez-Guerenu B, Aguirre I, Astigarraga E. Bile duct leaks after laparoscopic cholecystectomy: value of contrast-enhanced MRCP. Abdom Imaging. 2005;30:480–487. doi: 10.1007/s00261-004-0276-2. [DOI] [PubMed] [Google Scholar]
- 20.Ragozzino A, De Ritis R, Mosca A, Iaccarino V, Imbriaco M. Value of MR cholangiography in patients with iatrogenic bile duct injury after cholecystectomy. AJR Am J Roentgenol. 2004;183:1567–1572. doi: 10.2214/ajr.183.6.01831567. [DOI] [PubMed] [Google Scholar]
- 21.Bujanda L, Calvo MM, Cabriada JL, Orive V, Capelastegui A. MRCP in the diagnosis of iatrogenic bile duct injury. NMR Biomed. 2003;16:475–478. doi: 10.1002/nbm.853. [DOI] [PubMed] [Google Scholar]
- 22.Honore C, Vibert E, Hoti E, Azoulay D, Adam R, Castaing D. Management of excluded segmental bile duct leakage following liver resection. HPB (Oxford) 2009;11:364–369. doi: 10.1111/j.1477-2574.2009.00062.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Darwin P, Goldberg E, Uradomo L. Jackson Pratt drain fluid-to-serum bilirubin concentration ratio for the diagnosis of bile leaks. Gastrointest Endosc. 2010;71:99–104. doi: 10.1016/j.gie.2009.08.015. [DOI] [PubMed] [Google Scholar]
- 24.Donnellan F, Zeb F, Courtney G, Aftab AR. Successful outcome of sphincterotomy and 7-French pigtail stent insertion in the management of post-cholecystectomy bile leaks. Hepatobiliary Pancreat Dis Int. 2009;8:309–311. [PubMed] [Google Scholar]
- 25.Antonopoulos C, Voulimeneas I, Ioannides P, Kotsifas T, Kavallieratos N, Vagianos C. Bile leaks after cholecystectomy: the significance of patient selection. Surg Laparosc Endosc Percutan Tech. 2009;19:379–383. doi: 10.1097/SLE.0b013e3181ba8206. [DOI] [PubMed] [Google Scholar]
- 26.Tzovaras G, Liakou P, Fafoulakis F, Baloyiannis I, Zacharoulis D, Hatzitheofilou C. Is there a role for drain use in elective laparoscopic cholecystectomy? A controlled randomized trial. Am J Surg. 2009;197:759–763. doi: 10.1016/j.amjsurg.2008.05.011. [DOI] [PubMed] [Google Scholar]
- 27.Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909–918. doi: 10.1056/NEJM199609263351301. [DOI] [PubMed] [Google Scholar]
- 28.Rabenstein T, Schneider HT, Nicklas M, Ruppert T, Katalinic A, Hahn EG, et al. Impact of skill and experience of the endoscopist on the outcome of endoscopic sphincterotomy techniques. Gastrointest Endosc. 1999;50:628–636. doi: 10.1016/s0016-5107(99)80010-8. [DOI] [PubMed] [Google Scholar]
- 29.Salminen P, Laine S, Gullichsen R. Severe and fatal complications after ERCP: analysis of 2555 procedures in a single experienced centre. Surg Endosc. 2008;22:1965–1970. doi: 10.1007/s00464-007-9711-0. [DOI] [PubMed] [Google Scholar]
- 30.Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383–393. doi: 10.1016/s0016-5107(91)70740-2. [DOI] [PubMed] [Google Scholar]
- 31.Mavrogiannis C, Liatsos C, Papanikolaou IS, Karagiannis S, Galanis P, Romanos A. Biliary stenting alone versus biliary stenting plus sphincterotomy for the treatment of post-laparoscopic cholecystectomy biliary leaks: a prospective randomized study. Eur J Gastroenterol Hepatol. 2006;18:405–409. doi: 10.1097/00042737-200604000-00014. [DOI] [PubMed] [Google Scholar]
- 32.Agarwal N, Sharma BC, Garg S, Kumar R, Sarin SK. Endoscopic management of postoperative bile leaks. Hepatobiliary Pancreat Dis Int. 2006;5:273–277. [PubMed] [Google Scholar]
- 33.Simmons DT, Petersen BT, Gostout CJ, Levy MJ, Topazian MD, Baron TH. Risk of pancreatitis following endoscopically placed large-bore plastic biliary stents with and without biliary sphincterotomy for management of postoperative bile leaks. Surg Endosc. 2008;22:1459–1463. doi: 10.1007/s00464-007-9643-8. [DOI] [PubMed] [Google Scholar]
- 34.Aksoz K, Unsal B, Yoruk G, Buyrac Z, Haciyanli M, Akpinar Z, et al. Endoscopic sphincterotomy alone in the management of low-grade biliary leaks due to cholecystectomy. Dig Endosc. 2009;21:158–161. doi: 10.1111/j.1443-1661.2009.00878.x. [DOI] [PubMed] [Google Scholar]
- 35.Familiari L, Scaffidi M, Familiari P, Consolo P, Ficano L, Micelic D, et al. An endoscopic approach to the management of surgical bile duct injuries: nine years’ experience. Dig Liver Dis. 2003;35:493–497. doi: 10.1016/s1590-8658(03)00223-8. [DOI] [PubMed] [Google Scholar]
- 36.Coté GA, Ansstas M, Shah S, Keswani RN, Alkade S, Jonnalagadda SS, et al. Findings at endoscopic retrograde cholangiopancreatography after endoscopic treatment of post-cholecystectomy bile leaks. Surg Endosc. 2010;24:1752–1756. doi: 10.1007/s00464-009-0842-3. [DOI] [PubMed] [Google Scholar]
- 37.Coelho-Prabhu N, Baron TH. Assessment of need for repeat ERCP during biliary stent removal after clinical resolution of post-cholecystectomy bile leak. Am J Gastroenterol. 2010;105:100–105. doi: 10.1038/ajg.2009.546. [DOI] [PubMed] [Google Scholar]
- 38.Pinkas H, Brady PG. Biliary leaks after laparoscopic cholecystectomy: time to stent or time to drain. Hepatobiliary Pancreat Dis Int. 2008;7:628–632. [PubMed] [Google Scholar]


