Abstract
Objective
Coronary artery calcification (CAC) has been associated with psychosocial factors in some but not all cross-sectional analyses. The goal of this study was to determine whether positive and negative psychosocial factors prospectively predict CAC progression in postmenopausal women.
Methods
Participants from the Healthy Women Study who also participated in the Pittsburgh Mind-Body Center protocol (n = 149) completed self-report psychosocial measures prior to two electron beam tomography scans of CAC separated by an average of 3.3 years. Results of exploratory factor analysis were used to create aggregate psychosocial indices: Psychological Risk (depressive symptoms, perceived stress, cynicism, anger-in) and Psychosocial Resources (optimism, purpose in life, mastery, self-esteem, and social support).
Results
The Psychological Risk index predicted significantly greater CAC progression over three years (β = .16, p = .035, ΔR2 = .03) while the Psychosocial Resources index was not predictive of CAC progression (β = -.08, p = .30, ΔR2 = .01). On individual scales, higher scores on cynicism emerged as a significant predictor of CAC progression, along with a trend linking anger-in to atherosclerosis progression. A post-hoc analysis showed a significant interaction between cynicism and anger-in (β =.20, p = .01, ΔR2 = .03), such that women reporting high levels of both cynicism and anger suppression exhibited the most CAC progression.
Conclusions
These findings highlight psychosocial risk factors that may accelerate the progression of subclinical atherosclerosis in older women, suggest the potential importance of examining combinations of psychosocial risk factors, and represent potential targets for psychological interventions to reduce cardiovascular risk.
Keywords: coronary atherosclerosis, psychosocial, atherosclerosis, women
Psychosocial factors have been associated with incident cardiovascular disease (CVD) in women as well as men. We recently completed a review of the literature, concluding that factors such as stress, anger-in, and low levels of positive psychological factors are prospectively associated with cardiovascular health in women (1). As technologies to noninvasively image subclinical atherosclerosis become increasingly available and reliable, there is a growing literature linking psychological factors to early subclinical CVD. These measures are particularly important for understanding links between psychological factors and cardiovascular risk in women, given that women tend to develop symptomatic CVD later in life than men.
Electron bean computed tomography (EBCT) permits quantification of calcification in the coronary arteries, a measure that significantly predicts future cardiovascular events (2). Coronary artery calcification (CAC) scores are associated with certain psychological attributes in some but not all cross-sectional studies. For example, depressive disorders, particularly recurrent depression, has been linked to calcification in both women and men (3, 4, 5), but continuous measures of depressive symptoms showed no significant association with CAC across eight studies (5, 6, 7, 8, 9, 10, 11, 12). Similarly, hostility has been concurrently associated with CAC in some (12, 13) but not all studies (6, 9, 10, 11).
Cross-sectional investigations provide limited information about the links between psychosocial factors and CAC, and more prospective data are needed to clarify the temporal nature of any relationship. With the exception of two recent paper from the Study of Women's Health across the Nation (14, 15), no published studies to date have identified the prospective psychological predictors of calcification progression over time. In the two papers that have examined CAC progression, both recurrent major depression and depressive symptoms were associated with greater progression of CAC among middle-aged women (14, 15). These longitudinal analyses have important clinical implications. If psychological factors can hasten or slow the progression of subclinical atherosclerosis in healthy women, they may represent targets for behavioral interventions to reduce the burden of CVD among women.
Another limitation of existing reports is the focus on negative psychological factors, such as depressive symptoms (3-11), anxiety (6, 10), hostility (6, 9, 10), and stress (6, 9, 11). Given mounting scientific evidence that positive psychological characteristics can affect biological processes and physical health (16, 17), the relationship between positive psychological factors and subclinical atherosclerosis warrants further investigation. Two recent studies (9, 11) included measures of positive psychosocial attributes, such as optimism, social support, and self-esteem, with neither finding significant cross-sectional associations between positive psychological characteristics and CAC. To date, no studies have investigated whether positive psychosocial factors predict CAC progression prospectively.
The goal of the current study was to examine both positive and negative psychosocial factors as predictors of coronary calcification progression. We hypothesized that women who scored high on measures of negative psychosocial attributes and states would exhibit greater CAC progression whereas women who endorsed high levels of positive psychosocial attributes would show less progression of CAC over time. These hypotheses were tested in a sample of initially healthy, postmenopausal women.
Methods
Participants
The 149 women in the analytic sample were enrolled in the Healthy Women Study (HWS) and also participated in an ancillary protocol as part of the Pittsburgh Mind-Body Center (PMBC) to determine whether there are common pathways to diverse disease. The PMBC protocol included assessment of a range of psychological attributes and health behaviors. Eligible participants had at least two EBCT assessments after completion of the PMBC protocol, and did not have a history of CVD.
The HWS began in 1983-84 with 541 premenopausal women ages 42 to 50 who did not have diabetes or hypertension. The Institutional Review Board of the University of Pittsburgh approved all research procedures. Of the 421 women invited to participate in the PMBC protocol starting in 1999, 379 completed self-report measures of psychosocial attributes. Of these women, 249 had at least two EBCT scans, with 168 women having two scans after the PMBC protocol (median time between completion of PMBC measures and first EBCT = 322 days, range = 3 to 1083 days; median time between CAC scans = 3.2 years, range = 256 to 1786 days). Nineteen women were excluded who reported a history of heart disease. Differences between the 149 women included in analyses and the 230 women who did not complete the EBCT protocol or who were excluded due to history of heart disease were modest. Women included in the analyses were slightly younger (64.17 vs. 65.05) and reported slightly fewer depressive symptoms (4.26 vs. 5.46) and less perceived stress (12.11 vs. 13.79) than those not included; there were no other differences with regard to psychosocial or cardiovascular risk factors.
Psychosocial Factors
As part of the Pittsburgh Mind-Body Center protocol, participants completed a packet of standardized questionnaires between 2000 and 2003. Measures included an abbreviated 10-item version of the Center for Epidemiologic Studies-Depression inventory (18), a measure of depressive symptoms in the past week; the 10-item Perceived Stress Scale (19), which assessed perceived stressfulness of life in the past month; an abbreviated 6-item Cynicism subscale of the Cook-Medley Hostility inventory (20), which taps cynical or mistrustful attitudes towards others; the 8-item Anger-in subscale of the Spielberger Anger Inventory (21), which assesses the tendency to suppress anger or keep it in; the 6-item Revised Life Orientation Test (22), a measure of dispositional optimism; the 6-item Life Engagement Test (23), a measure of purpose in life; the 7-item Pearlin Mastery Scale (24), which assesses perceived control over important life outcomes; an abbreviated 4-item Rosenberg Self-Esteem Scale (25); and an abbreviated12-item Interpersonal Support Evaluation List (26), a measure of perceived availability of social support. Abbreviated measures of depressive symptoms, cynicism, self-esteem, and perceived social support were used to minimize participant burden and were based on published psychometric analyses (27, 28) as well as validation by the PMBC investigators.
We first conducted exploratory factor analysis with varimax rotation to determine whether the psychosocial measures formed coherent factors. Analyses yielded a two-factor solution accounting for 59% of the variance, with all factor loadings exceeding 0.54. Factor 1 (eigenvalue = 3.08) accounted for 34% of the variance after rotation, whereas Factor 2 (eigenvalue = 2.21) accounted for 25% of the variance. Factor 1, the Psychological Resources factor (α = .91), included optimism, purpose in life, self-esteem, mastery, and perceived social support. Factor 2, the Psychological Risk factor (α = .92), included the measures of depressive symptoms, perceived stress, cynicism, and anger-in. To create aggregate psychosocial indices, standardized scores on measures for each factor were averaged. The two factors were significantly inversely correlated (r = -.63, p < .001).
Coronary Calcification
An EBCT–trained technician used an Imatron C150 scanner (Imatron, South San Francisco, CA) and its densitometric program to assess the extent of calcification in the coronary arteries. During coronary scanning, 30 to 40 contiguous 3-mm-thick transverse images were obtained from the level of the aortic root to the apex of the heart. The participant was asked to hold her breath during the time of scanning. From these images, we derived Agatston (29) calcium scores for the coronary arteries. Coronary artery calcium lesions were considered to be present when three contiguous pixels greater than 130 Hounsfield units were detected. The total calcium score was a combination of volume and lesions.
Covariates
Age at questionnaire completion (M = 64 years, range = 61 to 68) and time between both questionnaire completion and the first CAC scan and between the two CAC assessments were included as covariates in all analyses. Body mass index and systolic blood pressure from the examination closest to the first CAC scan were also included as covariates. These covariates were selected for inclusion on the basis of previously published associations with CAC progression in another sample of middle-aged women (14). Analytic results did not differ significantly when current smoking status, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, triglycerides, current statin use, glucose level, and physical activity at baseline were included as additional covariates.
Statistical Approach
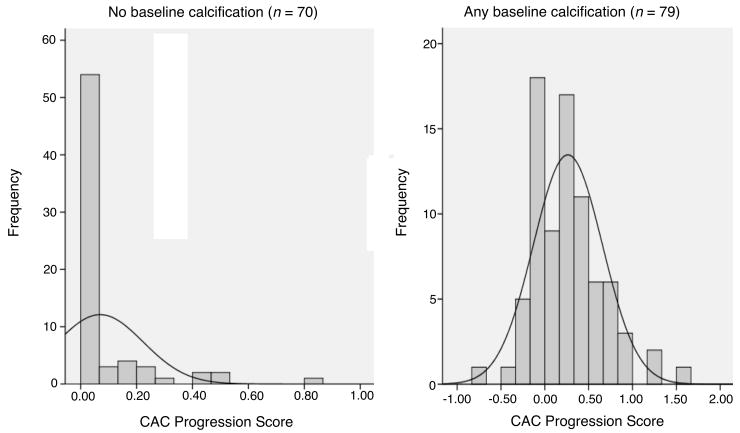
As in the Multi-Ethnic Study of Atherosclerosis (30), CAC progression over time was calculated as the difference between the log-transformed total calcification score measured at the first and second scan (i.e., ln (second CAC + 25) - ln (first CAC + 25)). Hierarchical regression models were used to predict CAC progression, entering covariates (i.e., age, body mass index, systolic blood pressure, baseline CAC, and time between assessments) in the first block and either Psychological Risk or Resources in the second block. For psychosocial indices that emerged as significant predictors, individual scales comprising that index were entered into separate regression analyses to determine which aspects of Psychological Risk or Resources were significantly associated with CAC progression. Because of reports that progression occurs in those with any CAC in several other studies (e.g. 14; see Figure 1), we also conducted stratified analyses to determine whether associations between psychosocial predictors and CAC progression differed between women with “no baseline CAC” and those with “any CAC.” A p-value of < .05 was considered statistically significant.
Figure 1.
Distribution of CAC progression scores by absence/presence of baseline CAC.
Results
Women were in their late-60s by the first CAC scan and were mostly white and overweight (Table 1). Covariates accounted for 19% of the variance in CAC progression, with both baseline CAC (β = .38, p < .001) and BMI (β = -.17, p = .03) significantly associated with progression score.
Table 1. Sample Characteristics (n = 149).
| Variable | ||
|---|---|---|
| Age at questionnaire completion, mean (SD) | 64 | (1.59) |
| White, n (%) | 140 | (94) |
| Systolic blood pressure (mm Hg), mean (SD) | 123.4 | (17.43) |
| Body mass index (kg/m2), mean (SD) | 27.51 | (5.35) |
| Baseline CAC score | ||
| 0, n (%) | 70 | (47.0) |
| 1 – 9, n (%) | 29 | (19.5) |
| ≥ 10, n (%) | 50 | (33.6) |
| Absolute change in CAC score, mean (SD) | 33.14 | 94.09 |
Consistent with previous cross-sectional analyses of this sample (9), neither the Psychosocial Resources index (ΔR2 < .001) nor the Psychological Risk index (R2 < .001) was significantly associated with baseline CAC (see Table 2). In hierarchical regression analyses with index scores, the Psychosocial Resources index was not significantly associated with CAC progression (ΔR2 = .01). In contrast, the Psychological Risk index predicted significantly greater CAC progression over three years (ΔR2 = .03, p = .035). The Psychological Risk index predicted CAC progression only for those 79 participants with any CAC at baseline (β = .22, ΔR2 = .04, p = .047) and was not significantly predictive of progression for the 70 women without any calcification at baseline (β = -.07, ΔR2 = .01, p = .57; presence of CAC × Psychological Risk interaction: β = .21, p = .059).
Table 2.
Standardized betas from regression analyses linking psychosocial predictors to CAC outcomes.
| Psychosocial Predictor | Baseline CAC | CAC progression |
|---|---|---|
| Psychological Risk Index | -.014 | .160* |
| Depressive Symptoms | -.024 | .064 |
| Perceived Stress | -.051 | .117 |
| Cynicism | -.018 | .156* |
| Anger-in | .046 | .131† |
| Psychological Resources Index | -.018 | -.079 |
| Optimism | -.007 | -.010 |
| Purpose in Life | -.023 | -.107 |
| Mastery | -.014 | -.061 |
| Self-esteem | -.039 | .009 |
| Social Support | .016 | -.130† |
p < .10;
p < .05
All associations adjusted for age, time between questionnaire completion and CAC assessment, BMI, and systolic blood pressure; associations with CAC progression also adjusted for baseline CAC and time between CAC assessments.
When separate scales from the Psychological Risk index were entered as predictors into regression models, cynicism emerged as a significant predictor of greater CAC progression (ΔR2 = .02, p = .040). Anger-in was predictive of marginally greater CAC progression (ΔR2 = .02, p = .091). As reported in Table 2, neither depressive symptoms nor perceived stress was significantly associated with change in CAC.
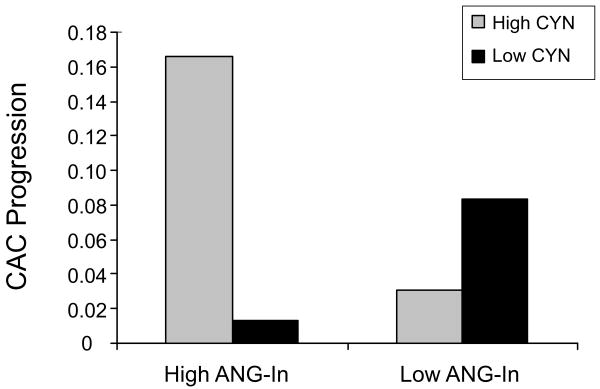
As a post-hoc analysis, we were interested in testing whether cynicism and anger-in interacted to predict CAC progression, as it seemed plausible that a tendency to suppress emotions (i.e., anger-in) might predict health only when there are high levels of negative emotions (i.e., anger resulting from cynical attitudes) to suppress (31, 32). Both variables were centered to facilitate interpretation and reduce multicollinearity, and significant interactions were analyzed via the method of Aiken and West (33) for continuous variables. As in planned analyses, covariates were entered in Step 1, anger-in and cynicism on Step 2, and the product of the two centered variables on Step 3. A significant interaction emerged (β = .20, p = .012, ΔR2 = .03). Analyses of the simple slopes tested the relation of anger-in with CAC progression as a function of cynicism at one SD above and below the mean. As displayed in Figure 2, the effect of anger-in was significant when cynicism was high (t(56) = 2.27, p = .025) but not when levels of cynicism were low (t(56) = -.95, p = .34). Similarly, the effect of cynicism was significant when anger-in was high (t(56) = 2.62, p = .010) but not when anger-in was low (t(56) = -.72, p = .47). Women who were high in both anger-in and cynicism had the greatest CAC progression, relative to those who had lower scores on either or both psychosocial measures. Consistent with the results reported for the Psychosocial Risk index, the effect of cynicism, anger-in, and their interaction approached or exceeded statistical significance only for women with some baseline CAC (data not shown; interaction between presence of CAC × cynicism: β = .14, p = .26; interaction between presence of CAC × anger-in: β = .27, p = .016; interaction between presence of CAC × anger-in × cynicism: β = .14, p = .31).
Figure 2.
Effect of high (M + SD) vs. low (M – SD) anger-in and cynicism on natural log of CAC progression.
Discussion
In a sample of relatively healthy postmenopausal women, we observed a prospective association between negative psychosocial factors and CAC progression over approximately three years. Although an aggregated index of negative psychosocial factors predicted greater CAC, this effect appears to be driven by significantly greater CAC progression among women who are both highly cynical and prone to anger suppression. The finding that the combination of cynicism and anger suppression may be cardiotoxic is consistent with results from an older cross-sectional study, which documented that hostility and anger-in interacted to determine extent of angiographically-determined atherosclerosis among (mostly male) patients (31; although note that this methodological approach has since been criticized; 34). Our findings are somewhat inconsistent with previous studies of carotid intima-media thickness (IMT), another noninvasive marker of subclinical atherosclerosis that is moderately correlated with CAC (35). Although both cynical hostility and anger suppression have been associated with carotid IMT in cross-sectional analyses (36, 37), neither predicts progression of IMT longitudinally (38, 39), with one exception. A study of 119 middle-aged men found that the interaction between cynical hostility and anger-in was nonsignificant but that cynicism and anger control (i.e., efforts to control angry feelings by avoiding open expression of irritation or aggression) additively predicted 2-year progression of carotid atherosclerosis (32). To our knowledge, the current study is the first to suggest the combination of hostility and anger suppression predicts progression of CAC in an initially healthy women. Results highlight the importance of examining the combination of negative attitudes relevant to emotional experience (in this case, frequent hostile cognitions) and differences in emotion regulation or expression to identify individuals at risk for CVD.
Consistent with results from another sample (14), psychosocial risk factors were significantly predictive of CAC progression only for women who had initial CAC at baseline. This suggests that the trajectory to CAC progression in late-life may begin before women are in their mid-50s and that those who have developed a significant atherosclerotic burden evidenced by CAC by midlife may be more vulnerable to the effects of psychosocial and other risk factors. CAC by EBCT measures calcified plaque as an estimate of total plaque burden (both calcified and noncalcified). It is possible that psychosocial risk factors accelerate the natural history from soft, potentially unstable to more stable plaque. More likely, however, our findings indicate that psychosocial factors predict increasing atherosclerotic burden over time in midlife women.
Contrary to hypotheses, results revealed no significant association between positive psychosocial resources, including optimism, purpose in life, self-esteem, mastery, and perceived social support, and CAC progression. Relative to psychological risk factors such as negative emotions and stress, protective factors have received limited empirical attention as potential predictors of CVD (1). Optimism has been prospectively linked to incident CVD in women (40) as well as progression of carotid IMT (41), but an earlier analysis of the HWS cohort reported that positive factors were cross-sectionally associated with aortic but not coronary calcification (9). Perhaps positive psychosocial factors are more important once CVD has developed, helping individuals to cope with medical procedures and symptoms and to sustain adherence to medication and lifestyle changes.
A recent paper by Rozanski and colleagues (11) highlighted an intriguing difference in findings of cross-sectional versus longitudinal studies linking psychological risk factors and CAC. They argued that studies examining concurrent measures of psychological risk tend to report null results, whereas those that measured psychological factors several years prior to CAC scanning reported positive results. This discrepancy parallels the observed associations between CAC and traditional CVD risk factors such as low-density lipoprotein cholesterol assessed prospectively but not concurrently (42). The current study contributes to this literature by demonstrating that psychosocial factors assessed prior to CAC predicted change in CAC over several years, whereas previous analyses of this same cohort reported no significant cross-sectional association between positive or negative psychosocial attributes and CAC (9). As this is only the second sample in which psychosocial factors have been examined as predictors of CAC progression (14, 15), more research is needed to determine whether emotional and social factors predict not only presence or extent of calcification at a single timepoint, but also the extent of change in calcification over time.
This study has several limitations. First, participants in our sample were predominantly well-educated white women, and findings may not generalize to other racial or socioeconomic groups. Second, the sample was relatively small, which may have limited statistical power to detect effects. Third, psychological attributes and states were assessed at a single timepoint, when women were in their mid-60s. Given that atherosclerosis develops over the life course, the association between psychosocial factors and atherosclerosis may be strongest when chronic, cumulative emotional or social factors (e.g., recurrent major depression; consistently low social support) are assessed (11). Repeated assessment of psychosocial factors may be particularly important to understanding the role of positive attributes and coping resources in the development of CVD, as these factors may be particularly likely to exhibit variability over time as participants age (43, 44, 45). Assessment of psychosocial risk and protective factors was also limited to self-report in this study; given that some cross-sectional reports find associations between spousal reports of psychological traits and CAC but not self-reported traits (12), our reliance on self-reports could have resulted in an underestimate of some associations. A final limitation of the study was the use of abbreviated measures (e.g., cynicism scale reduced to 6 items from 13 items), which may limit comparability to previous work. Strengths of the study include the examination of a wide range of psychosocial measures, prospective design, and focus on older women without history of frank cardiovascular disease.
In summary, our results suggest that psychosocial risk factors, particularly the combination of cynical attitudes and a tendency to suppress anger, predict greater increases in CAC among relatively healthy older women. These findings highlight psychosocial risk factors that may accelerate the progression of subclinical coronary atherosclerosis and that may therefore represent potential targets for psychological intervention. Interventions aimed at reducing cynical attitudes and/or encouraging constructive expression of anger may not only benefit psychological well-being, but could also alter the trajectory of cardiovascular risk among older women.
Acknowledgments
This research was supported in part by the National Institutes of Health grants (HL007560, HL28266).
Glossary
- CAC
coronary artery calcification
- CVD
cardiovascular disease
- EBCT
electron bean computed tomography
- HWS
Healthy Women Study
- IMT
intima-media thickness
- PMBC
Pittsburgh Mind-Body Center
References
- 1.Low CA, Thurston RC, Matthews KA. Psychosocial factors in the development of heart disease in women: Current research and future directions. Psychosom Med. 2010;72:842–854. doi: 10.1097/PSY.0b013e3181f6934f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Folsom AR, Kronmal RA, Detrano RC, O'Leary DH, Bild DE, Bluemke DA, Budoff MJ, Liu K, Shea S, Szklo M, Tracy RP, Watson KE, Burke GL. Coronary artery calcification compared with carotid intima-media thickness in the prediction of cardiovascular disease incidence: the Multi-Ethnic Study of Atherosclerosis (MESA) Arch Intern Med. 2008;168:1333–1339. doi: 10.1001/archinte.168.12.1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Agatisa PK, Matthews KA, Bromberger JT, Edmundowicz D, Chang YF, Sutton-Tyrell K. Coronary and aortic calcification in women with a history of major depression. Arch Intern Med. 2005;165:1229–1236. doi: 10.1001/archinte.165.11.1229. [DOI] [PubMed] [Google Scholar]
- 4.Hamer M, Kivimaki M, Lahiri A, Marmot MG, Steptoe A. Persistent cognitive depressive symptoms are associated with coronary artery calcification. Atheroscler. 2010;210:209–213. doi: 10.1016/j.atherosclerosis.2010.01.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tiemeier H, van Dijck W, Hofman A, Witteman JCM, Stijnen T, Breteler MMB. Relationship between atherosclerosis and late-life depression: The Rotterdam Study. Arch Gen Psychiatry. 2004;61:369–376. doi: 10.1001/archpsyc.61.4.369. [DOI] [PubMed] [Google Scholar]
- 6.Diez Roux AV, Ranjit N, Powell L, Jackson S, Lewis TT, Shea S, Wu C. Psychosocial factors and coronary calcium in adults without clinical cardiovascular disease. Ann Intern Med. 2006;144:822–831. doi: 10.7326/0003-4819-144-11-200606060-00008. [DOI] [PubMed] [Google Scholar]
- 7.Kop WJ, Berman DS, Gransar H, Wong ND, Miranda-Peats R, White MD, Shin M, Bruce M, Krantz DS, Rozanski A. Social networks and coronary artery calcification in asymptomatic individuals. Psychosom Med. 2005;67:343–352. doi: 10.1097/01.psy.0000161201.45643.8d. [DOI] [PubMed] [Google Scholar]
- 8.Lewis TT, Everson-Rose SA, Colvin A, Matthews KA, Bromberger JT, Sutton-Tyrell K. The interactive effects of race and depressive symptoms on calcification in African-American and white women. Psychosom Med. 2009;71:163–170. doi: 10.1097/PSY.0b013e31819080e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Matthews KA, Owens JF, Edmundowicz D, Lee L, Kuller LH. Positive and negative attributes and risk for coronary and aortic calcification in healthy women. Psychosom Med. 2006;68:355–361. doi: 10.1097/01.psy.0000221274.21709.d0. [DOI] [PubMed] [Google Scholar]
- 10.O'Malley PG, Jones JL, Feuerstein IM, Taylor AJ. Lack of correlation between psychological factors and subclinical coronary artery disease. N Engl J Med. 2000;343:1298–1304. doi: 10.1056/NEJM200011023431803. [DOI] [PubMed] [Google Scholar]
- 11.Rozanski A, Gransar H, Kubzansky LD, Wong N, Shaw L, Miranda-Peats R, Thomson LE, Hayes SW, Friedman JD, Berman DS. Do psychological risk factors predict the presence of coronary atherosclerosis? Psychosom Med. 2011;73:7–15. doi: 10.1097/PSY.0b013e3181fd94f5. [DOI] [PubMed] [Google Scholar]
- 12.Smith TW, Uchino BN, Berg CA, Florsheim P, Pearce G, Hawkins M, Henry NJM, Beveridge RM, Skinner MA, Hopkins PN, Yoon HC. Associations of self-reports versus spouse ratings of negative affectivity, dominance, and affiliation with coronary artery disease: Where should we look and who should we ask when studying personality and health? Health Psychol. 2008;27:676–684. doi: 10.1037/0278-6133.27.6.676. [DOI] [PubMed] [Google Scholar]
- 13.Iribarren C, Sidney S, Bild DE, Lieu K, Markovitz JH, Roseman JM, Matthews K. Association of hostility with coronary artery calcification in young adults: The CARDIA study. JAMA. 2000;283:2546–2551. doi: 10.1001/jama.283.19.2546. [DOI] [PubMed] [Google Scholar]
- 14.Matthews KA, Chang YF, Sutton-Tyrell K, Edmundowicz D, Bromberger JT. Recurrent major depression predicts progression of coronary calcification in healthy women: Study of Women's Health across the Nation. Psychosom Med. 2010;72:742–747. doi: 10.1097/PSY.0b013e3181eeeb17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Janssen I, Powell LH, Matthews KA, Cursio JF, Hollenberg SM, Sutton-Tyrell K, Bromberger JT, Everson-Rose SA. Depressive symptoms are related to progression of coronary calcium in midlife women: The Study of Women's Health Across the Nation (SWAN) Heart Study. Am Heart J. 2011;161:1186–1191. doi: 10.1016/j.ahj.2011.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lyubomirsky S, King L, Diener E. The benefits of frequent positive affect: Does happiness lead to success? Psychol Bull. 2005;131:803–855. doi: 10.1037/0033-2909.131.6.803. [DOI] [PubMed] [Google Scholar]
- 17.Pressman SD, Cohen S. Does positive affect influence health? Psychol Bull. 2005;131:925–971. doi: 10.1037/0033-2909.131.6.925. [DOI] [PubMed] [Google Scholar]
- 18.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Measure. 1977;1:385–401. [Google Scholar]
- 19.Cohen S, Williamson GM. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The Social Psychology of Health. Newbury Park, CA: Sage; 1988. [Google Scholar]
- 20.Cook WW, Medley DM. Proposed hostility and pharisaic-virtue scales for the MMPI. J Appl Psychol. 1954;38:414–418. [Google Scholar]
- 21.Spielberger CD, Johnson EH, Russell SF, Crane RJ, Jacobs GA, Worden TJ. The experience and expression of anger: Construction and validation of an anger expression scale. In: Chesney MA, Rosenman RH, editors. Anger and Hostility in Cardiovascular and Behavioral Disorders. Cambridge: Hemisphere; 1985. [Google Scholar]
- 22.Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A re-evaluation of the Life-Orientation Test. J Pers Soc Psychol. 1994;67:1063–1078. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- 23.Scheier MF, Wrosch C, Zdaniuk B, Cohen S, Matthews KA, Schulz R. Life Engagement Test: Assessing purpose in life. J Beh Med. 2006;29:291–298. doi: 10.1007/s10865-005-9044-1. [DOI] [PubMed] [Google Scholar]
- 24.Pearlin LI, Schooler C. The structure of coping. J Health Soc Behav. 1978;19:2–21. [PubMed] [Google Scholar]
- 25.Rosenberg M. Society and Adolescent Self-image. Princeton, NJ: Princeton University Press; 1965. [Google Scholar]
- 26.Cohen S, Mermelstein R, Kamarck T, Hoberman H. Measuring the functional components of social support. In: Sarason IG, Sarason B, editors. Social Support: Theory, Research, and Applications. The Hague: Martinus Nijhoff; 1985. [Google Scholar]
- 27.Andresen EM, Carter WB, Malmgren JA, Patrick DL. Screening for depression in well older adults: Evaluation of a short form of the CES-D. Am J Prev Med. 1994;10:77–84. [PubMed] [Google Scholar]
- 28.Barefoot KC, Dodge KA, Peterson BL, Dahlstrom WG, Williams RB. The Cook-Medley Hostility Scale: Item content and ability to predict survival. Psychosom Med. 1989;51:46–57. doi: 10.1097/00006842-198901000-00005. [DOI] [PubMed] [Google Scholar]
- 29.Agatston AS, Janowitz WR, Hildner FJ, Zuamer NR, Viamonte M, Detrano R. Quantification of coronary artery calcium using ultrafast computer tomography. J Am Coll Cardiol. 1990;15:827–832. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 30.Kronmal RA, McClelland RL, Detrano R, Shea S, Lima JA, Cushman M, Bild DE, Burke GL. Risk factors for the progression of coronary artery calcification in asymptomatic subjects: Results from the Multi-Ethnic Study of Atherosclerosis. Circulation. 2007;115:2722–2730. doi: 10.1161/CIRCULATIONAHA.106.674143. [DOI] [PubMed] [Google Scholar]
- 31.Dembroski TM, MacDougall JM, Williams RB, Haney TL, Blumenthal JA. Components of Type A, hostility and anger-in: Relationship to angiographic findings. Psychosom Med. 1985;47:219–233. doi: 10.1097/00006842-198505000-00001. [DOI] [PubMed] [Google Scholar]
- 32.Julkunen J, Salonen R, Kaplan GA, Chesney MA, Salonen JT. Hostility and the progression of carotid atherosclerosis. Psychosom Med. 1994;56:519–525. doi: 10.1097/00006842-199411000-00007. [DOI] [PubMed] [Google Scholar]
- 33.Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks (CA): Sage Publications; 1991. [Google Scholar]
- 34.Pickering TG. Should studies of patients undergoing coronary angiography be used to evaluate the role of behavioral risk factors for coronary heart disease? J Behav Med. 1985;8:203–211. doi: 10.1007/BF00870308. [DOI] [PubMed] [Google Scholar]
- 35.Newman AB, Naydeck BL, Sutton-Tyrrell K, et al. Relationship between coronary artery calcification and other measures of subclinical cardiovascular disease in older adults. Arterioscler Thromb Vasc Biol. 2002;22:1674–1679. doi: 10.1161/01.atv.0000033540.89672.24. [DOI] [PubMed] [Google Scholar]
- 36.Everson-Rose SA, Lewis TT, Karavolos K, Matthews KA, Sutton-Tyrell K, Powell LH. Cynical hostility and carotid atherosclerosis in African American and white women: The Study of Women's Health Across the Nation Heart Study. Am Heart J. 2006;152:e7–e13. doi: 10.1016/j.ahj.2006.08.010. [DOI] [PubMed] [Google Scholar]
- 37.Matthews KA, Owens JF, Kuller LH, Sutton-Tyrell K, Jansen-McWilliams L. Are hostility and anxiety associated with carotid atherosclerosis in health postmenopausal women. Psychosom Med. 1998;60:633–638. doi: 10.1097/00006842-199809000-00021. [DOI] [PubMed] [Google Scholar]
- 38.Räikkönen K, Matthews KA, Sutton-Tyrrell K, Kuller LH. Trait anger and the metabolic syndrome predict progression of carotid atherosclerosis in healthy middle-aged women. Psychosom Med. 2004;66:903–8. doi: 10.1097/01.psy.0000143638.31297.11. [DOI] [PubMed] [Google Scholar]
- 39.Stewart JC, Janicki DL, Muldoon MF, Sutton-Tyrrell K, Kamarck TW. Negative emotions and 3-year progression of subclinical atherosclerosis. Arch Gen Psychiatry. 2007;64:225–33. doi: 10.1001/archpsyc.64.2.225. [DOI] [PubMed] [Google Scholar]
- 40.Tindle HA, Chang YF, Kuller LH, Manson JE, Robinson JG, Rosal MC, Siegle GJ, Matthews KA. Optimism, cynical hostility, and incident coronary heart disease and mortality in the Women's Health Initiative. Circulation. 2009;120:656–62. doi: 10.1161/CIRCULATIONAHA.108.827642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Matthews KA, Räikkönen K, Sutton-Tyrrell K, Kuller LH. Optimistic attitudes protect against progression of carotid atherosclerosis in healthy middle-aged women. Psychosom Med. 2004;66:640–4. doi: 10.1097/01.psy.0000139999.99756.a5. [DOI] [PubMed] [Google Scholar]
- 42.Matthews KA, Kuller LH, Chang Y, Edmundowicz D. Premenopausal risk factors for coronary and aortic calcification: A 20-year follow-up in the Healthy Women Study. Prev Med. 2007;45:302–308. doi: 10.1016/j.ypmed.2007.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Isaacowitz DM. Correlates of well-being in adulthood and old age: A tale of two optimisms. J Res Pers. 2005;39:224–244. [Google Scholar]
- 44.Krause N. Assessing change in social support during late life. Res Aging. 1999;21:539–569. [Google Scholar]
- 45.Robins RW, Trzesniewski KH. Self-esteem development across the lifespan. Curr Dir Psychol Sci. 2005;14:158–162. [Google Scholar]