Abstract
Objective
The aim of this study was to examine whether lag-sequential analysis could be used to describe eye gaze orientation between clinicians and patients in the medical encounter. This topic is particularly important as new technologies are implemented into multi-user health care settings where trust is critical and nonverbal cues are integral to achieving trust. This analysis method could lead to design guidelines for technologies and more effective assessments of interventions.
Background
Nonverbal communication patterns are important aspects of clinician-patient interactions and may impact patient outcomes.
Method
Eye gaze behaviors of clinicians and patients in 110-videotaped medical encounters were analyzed using the lag-sequential method to identify significant behavior sequences. Lag-sequential analysis included both event-based lag and time-based lag.
Results
Results from event-based lag analysis showed that the patients’ gaze followed that of clinicians, while clinicians did not follow patients. Time-based sequential analysis showed that responses from the patient usually occurred within two seconds after the initial behavior of the clinician.
Conclusion
Our data suggest that the clinician’s gaze significantly affects the medical encounter but not the converse.
Application
Findings from this research have implications for the design of clinical work systems and modeling interactions. Similar research methods could be used to identify different behavior patterns in clinical settings (physical layout, technology, etc.) to facilitate and evaluate clinical work system designs.
Keywords: Nonverbal communication, medical encounter, health care system
INTRODUCTION
The clinician-patient relationship is a fundamental aspect of the health care system. Understanding the dynamics of this relationship is a necessary part of redesigning the work of the health providers. As technologies become more pervasive in the clinical encounter, a human factors and ergonomics approach can be used to evaluate the effects of technologies on other aspects of the system and to develop design guidelines for existing and future technologies. According to Blumenthal (2009), adoption of health information technology and electronic health records (EHRs) in the United States has been low, specifically “few U.S. doctors or hospitals — perhaps 17% and 10%, respectively — have even basic EHRs” (p.1477). Barriers to clinician adoption and use of health information technologies include cost, lack of technical support, and clinician and patient concerns about privacy and security (Blumenthal 2009). In addition to those overtly expressed concerns, there is evidence that health information technologies can alter cognitive performance of care providers. Holden (2010) conducted interviews with clinicians in two hospitals in the United States and found that EHRs contributed to both improvements and decrements in cognitive performance. These changes in cognitive performance have the potential to affect patient perceptions of the care provider, the technology and aspects of the communication. The communication process between patients and care providers is an essential component of the clinician-patient relationship, and thus comprises a large portion of the work conducted by care providers in primary care environments. Evaluating the effects of interventions and system changes on communication can contribute to the analysis of interventions and designs that include technologies.
The communication process is comprised of both nonverbal and verbal components. The verbal component is primarily communicated information, using sound, words, speech, and language. Nonverbal components include features such as social touch (e.g., hand shaking, eye contact), and emotional projection (e.g., smiling.)
In nonverbal communication, gaze is an important aspect of establishing common ground, which is a mutual belief that the communicants understand one another (Clark and Brennan, 1991). Gaze and other nonverbal cues also help convey emotional context (Ong, De Haes, Hoos, & Lammes, 1995; Bensing, 1991). In interpersonal contexts, technologies or other characteristics of work system designs may affect the communication process. Technologies, such as computers, can mask important communication cues or change an individual’s perception of the encounter. While other researchers have evaluated the effects of technologies on interpersonal communication in health care, most have used holistic or qualitative measures. For example, Margalit et al. (2006) evaluated electronic medical record use in physician-patient communication through video analysis. Their study explored communication and the amount of time care providers spent gazing at computer screens using the Roter Interaction Analysis System (RIAS) instrument. While their study was able to show that the way clinicians use computers in examination room can negatively affect interaction with patients, the analysis method did not lead to empirically driven guidelines for the design of technologies that might facilitate positive communication between doctors and patients.
Measures of positive technology use in interpersonal interactions may be more complex than the metrics many studies use to assess technology use. While many studies compare frequency and duration of gaze (Margalit, 2006; Schmid Mast, Hall, Klöckner, & Choi, 2008), it may be more useful to explore patterns and optimal sequences of gaze behaviors. Lag sequential analysis methods could be used to describe the influence of technology on interpersonal interactions and important communication outcomes, such as eye contact, turn taking, and emotional projection. This method could also be used to develop and evaluate technological interventions for settings where interpersonal communication is important.
Eye gaze
Eye contact is important for positive interpersonal communication between individuals. Farroni et al. (2002) argue that “eye contact is the most powerful mode of establishing a communicative link between humans” (p. 9602). In their research with infants they found that from very early ages humans prefer to look at faces that reciprocate gaze, i.e., engage in mutual gaze or make eye contact, and being gazed upon engages enhanced neural processes. Kleinke’s (1986) review paper on gaze and eye contact reports that in interactions between people, gaze provides information, regulates interaction, and expresses emotional state. During health care encounters, physician positive interactions and communication of appropriate emotional responses, such as empathy, are correlated with measures of patient satisfaction (DiMatteo 1980). Many studies have shown that gaze behaviors are related to a person’s likeability. For example, studies have shown that people in photographs and videotapes are rated as liking each other more when they share high levels of gaze (Kleinke, Meeker, & Fong, 1974; Mehrabian, 1968; Naiman & Breed, 1974; Scherer & Schiff, 1973; Thayer & Schiff, 1974). Researchers have also found that gaze influences people’s liking for each other; specifically in moderation, as study participants preferred people who provided moderate amounts of gaze over constant or no gaze (Argyle, Lefebvre, & Cook, 1974). The presence of gaze influences individuals’ perceptions of others and their willingness to work with them. In one study, participants more often chose to work with confederates who gazed at them during introductions as opposed to those who did not (Stass & Willis Jr, 1967). In another study, participants rated same-sex peers as more pleasant when the person gazed at them continuously, rather than not at all (Cook & Smith, 1975). Gazing confederates in studies by Exline and Eldridge (1967) and Ellsworth and Ludwig (1972) received more favorable evaluations than confederates who did not gaze when they communicated positive messages. Gaze is also related to perceptions of competence and intelligence; a study conducted in the context of interviewing found a positive correlation between observers’ estimates of the interviewee’s intelligence and the interviewee’s eye contact with an interviewer (Wheeler, Baron, Michell, & Ginsburg, 1979).
Finally, gaze is related to perceptions of suspiciousness and credibility; in a study with mock customs inspectors, travelers were perceived as less suspicious if they made eye contact with the inspector (Kraut & Poe, 1980). Hemsley and Doob (1978) found witnesses in a legal trial were assessed as more credible when they did not avert their gaze from the questioning attorney. These studies collectively support the notion that gaze is innately correlated with individual perceptions of positive interactions. Thus, gaze appears to be integral to positive communication in patient care-provider interactions.
Eye gaze in clinician-patient interaction
The present study focused on eye gaze in clinician-patient interaction to gain insight into the relationship between gaze, clinicians’ communication style, and outcomes of the medical encounter (health status and patient satisfaction). Duration of clinician gaze at patient is a significant predictor of patient satisfaction (Schmid Mast, Hall, Klöckner, & Choi, 2008). In a study of 34 videos from family practice physicians, two judges rated communication on 11 pre-defined parameters (Larsen & Smith, 1981). The duration of patient gaze at the clinician was negatively related to patient ratings of satisfaction (Larsen & Smith, 1981). A moderate level of mutual gaze between the clinician and patient was associated with patients’ perception of clinician empathy, interest in the patient, and warmth (Harrigan, Oxman, & Rosenthal, 1985).
Eye gaze in medical encounters has been evaluated qualitatively (Malterud, 1999; Robinson, 1998; Ruusuvuori, 2001) and quantitatively for duration (Bensing, Kerssens, & van der Pasch, 1995; Harrigan et al., 1985) or frequency (Street & Buller, 1987) of gaze. Previous studies have not addressed the dynamic nature of gazing between the clinician and the patient or explored how gaze could inform design guidelines for technologies and the system. If switching the object of the gaze orientation is considered an event, gaze in the medical encounter can be analyzed as a stream of sequential events. Sequential analysis of these event patterns can quantify, for example, whether the clinician is gazing at the patient reciprocally or whether the patient is passively following the clinician’s gaze. Such data can guide the design of interventions to improve clinical outcomes. For example, a training intervention could help clinicians increase mutual gaze in an encounter. If the goal is to increase patients’ mutual gaze in an encounter, a different intervention may be needed, such as, increasing the number of questions asked of the patient or creating more opportunities to share information with patients. Finally, little work has been done to determine how interpersonal cues should be incorporated into the design of clinical information systems. Limited information is available on training clinicians to work with clinical information systems. A precursor to developing interventions is being able to evaluate gaze and other nonverbal behaviors in a manner that can be linked to outcomes of interest such as patient trust or adherence to care recommendations.
Analyzing sequential data
Lag-sequential analysis, which is based on contingency table analysis, is the most commonly used sequential analysis method (Connor, Fletcher, & Salmon, 2009). Incorporating the log-linear model, the likelihood-ratio chi-square test can be used to test the dependence of the initial and response behaviors (Wickens, 1989) while adjusted residuals can be used to detect significant behavior sequences (Bakeman & Gottman, 1997).
Lag-sequential analysis has been widely used in research, specific topics include: foraging patterns in animal behavior research (Butler, 2005), children’s mealtime behaviors before and after parental attention (Woods, Borrero, Laud, & Borrero, 2010), transition patterns of preschooler’s social play (Robinson, Anderson, Porter, Hart, & Wouden-Miller, 2003), precursors of problem behavior in individuals with autism (Borrero & Borrero, 2008), sequences in therapist’s intervention and patient’s levels of defensive functioning (Drapeau, de Roten, Beretta, Blake, Koerner, & Despland, 2008), online asynchronous problem-solving discussion patterns (Hou, Chang, & Sung, 2008), patterns of work group discussions about complaints and solutions (Kauffeld & Meyers, 2009), and communication sequences that contribute to better team performance (Bowers, Jentsch, Salas, & Braun, 1998).
Sequential analysis has also been applied in research on clinician-patient interactions. These studies include descriptive research detecting patterns of utterance sequences in verbal communication (Eide, Quera, & Finset, 2003; Eide, Quera, Graugaard, & Finset, 2004; Epstein et al., 2007; Scrimin et al., 2005) and investigation of the relationship between patient provision of information and speech sequences between clinicians and patients (Del Piccolo, Mazzi, Dunn, Sandri, & Zimmermann, 2007; Zimmermann, Del Piccolo, & Mazzi, 2003). In the Eide et al. (2004) study, patient-clinician dialogue was evaluated through audio recordings of clinical interactions. Researchers found that RIAS sequential analysis provided insights into the communication process. Specifically, they were able to show that physicians used silence and minimal encouragers before patients’ expressions of concern and minimal encouragers and optimistic responses after the expressions of concern. They looked for potential differences in patterns between different types of physician groups, which could influence physician training. However, very little is published about nonverbal communication using sequential analysis.
Relevance of modeling gaze to human factors and ergonomics
Nonverbal communication is particularly important in clinical encounters, but largely neglected in work system design and interventions. In this study, we propose an approach for analyzing nonverbal communication, specifically gaze, in health care work systems. This approach can lead to a better understanding of the importance of nonverbal interactions in patient-clinician relationships. Additionally, better understanding of the relevance of nonverbal interactions in health care may influence design guidelines for health information technologies. The lag sequential analysis method, popularized in other domains such as communication and counseling psychology (Gottman & Roy, 1990), has not been widely cited in the human factors and ergonomics literature. This paper explores the efficacy of this method in a work system without technologies, which is most appropriate for the development of guidelines to overcome “barriers” that may impede nonverbal communication.
Human factors and ergonomics researchers have studied eye gaze previously; therefore lag sequential analysis of gaze patterns may be relevant to domains outside of health care. For example, Salvucci (2007) used gaze models to characterize how humans use technologies in automobiles. In a usability study, Martin and Smith-Jackson (2008) used gaze to evaluate children’s understanding of instructions. Shah and Breazeal (2010) explored gaze as a source of nonverbal communication between humans and robots. Studies like these could incorporate lag sequential analysis methods to move beyond measuring gaze frequency or duration to better understand gaze patterns and the effects of their interventions on gaze patterns.
Research questions
New clinical technologies and work systems will need to consider nonverbal interactions that may affect patient perception of the care provider and the health system. These cues may influence important health outcomes such as patient trust in provider, adherence to medical advice, satisfaction with provider, and return to practice (Pearson & Raeke, 2000). However, there are few methods available to provide accurate guidelines for nonverbal cues in the design of information technologies.
The research described in this paper explores gaze behaviors between patients and clinicians in clinical interactions; specifically to better understand dyadic gaze behaviors. Lag sequential analysis was used to quantify the eye gazes of the clinician and patient based on the sequence (occurrence) as well as the timing (temporal immediacy) of gaze activity. The main research questions were:
How was the clinician’s gaze related to the patient’s gaze: (a) Did patients follow where the clinician gazed (occurrence)? (b) If so, what was the timing of this behavior relative to the clinician’s behavior (temporal immediacy)?
How was the patient’s gaze related to the clinician’s gaze: (a) Did clinicians follow where the patient gazed (occurrence)? (b) If so, what was the timing of this behavior relative to the patient’s behavior (temporal immediacy)?
METHOD
Participants
The data set was derived from videotaped medical encounters of clinicians with patients being seen for acute upper respiratory infection (common cold). Patients with new onset colds were recruited from the community. 110 encounters were included in the present analysis and were recorded with high video resolution after obtaining informed consent. The encounters took place in one of two clinics in Dane County, Wisconsin between April 2004 and February 2006. Institutional Review Board approval was obtained through the University of Wisconsin School of Medicine and Public Health and the study complied with HIPAA (Health Insurance Portability and Accountability Act) regulations. Five Caucasian clinicians participated in this study; four family physicians (four men and one woman) and one female family nurse practitioner. We did not collect data regarding clinician education or socioeconomic status. Each encounter was with a different patient and the five clinicians interacted with 13, 16, 22, 17, and 32 unique patients, respectively.
Each clinical encounter included a history of the present illness, past medical history, a physical exam, diagnosis and a treatment plan. For each encounter, the clinicians were randomized to interact with the patient in either the routine manner or one that emphasized positive prognosis, education, empathy, empowerment, and connectedness (Barrett et al., 2007). Each clinician had roughly equal numbers of standard and enhanced interactions with patients. However, because some videos were of poor quality, the cases in the present analysis were not fully balanced (58 routine and 52 enhanced interactions).
The patients ranged in age from 12 to 71 with 69 (63%) female and 41 male (37%). 108 (98%) participants were White/Caucasian. Twelve patients (11%) had “some high school”, 7 (6%) had “high school grad/GED”, 24 (22%) had “some college/tech school”, 56 (51%) had “college grad/post grad” and 11 (10%) did not provide this information. 35 (32%) patients met with a female clinician and 75 (68%) met with a male clinician.
Coding the medical encounter
All videos were coded with Noldus Observer XT 9.0 software. An a priori coding scheme was developed which included participant, behavior, and modifiers for events in the videos (see Table 1) (Krippendorff, 2004). The code ‘Participant’ indicated whether the participant was the clinician or the patient. The code ‘Behavior’ indicated gaze. Modifier codes described the clinician, patient, chart, or other artifacts. The coding scheme and its definition used in this research are shown in Table 1. Coders recorded the start and stop time of events in the video by pressing keyboard hot keys. For example, “clinician gaze patient” was coded when the clinician shifted their eye orientation to the patient from somewhere else, and “clinician gaze chart” was coded when the clinician shifted their gaze from the patient to the chart containing patient’s medical history. All events were stored as codes, which allowed calculation of the duration and frequency of each behavior in a certain time period or throughout a single encounter. Sequential analysis was performed by considering codes as a stream of events.
TABLE 1.
Coding scheme and definitions
| Participant | Behavior | Modifier |
|---|---|---|
| Patient | Gaze | Patient |
| Doctor | Doctor | |
| Chart | ||
| Other artifact | ||
| Unknown |
Note. Definitions of the terms: 1. Modifiers of Gaze — participant’s eye gaze orientation or participant’s head direction when back is to camera. 2. Chart — paper with information about the patient; or notes written by the clinician during the encounter. 3. Other artifact — other objects in the room, including chairs, examination table, sink, medical tools, magazines, etc. 4. Unknown — included three situations: (a) Coder can see participant’s eyes but is not able to specify object, this also includes the situation when the participant is moving and looking somewhere while thinking. (b) Coder is not able to code participant’s gazing due to the participant facing away from the camera or being out of screen. (c) Participant is gazing at other person rather than clinician and patient in the consultation room.
The coders used a two-pass procedure; in the first video viewing, coders only coded the patient’s behavior. During the second pass, the clinician’s behavior was coded. The video speed was set at one-half real-time to increase the precision of time marks. There were three distinct phases in each medical encounter: pre-exam consultation, physical examination, and post-exam consultation. The physical exam component was not included in the analysis of this study.
Three coders developed the coding scheme and executed the coding process for three weeks. Coders were trained before starting the analysis to ensure they were able to reliably code events in the same way. During training, each coder coded five videos to ensure appropriate reliability before moving forward. Each subsequent week, one video was assigned to be coded by all three coders. When a coder coded an event at a specific time (X), if the other coder gave the same code in the period of X± 1 second, it was counted as agreement. If the coder gave a different code or did not code anything, it was counted as disagreement. In this study, the proportion of agreements and Cohen’s Kappa coefficient were used to evaluate reliability. The average value of Cohen’s Kappa coefficient of all the reliability check videos was between 0.67 and 0.77. The conservative X± 1 second time period contributed to reliability scores that were lower than .80. The average reliability among the coders was 0.76 and 0.74 (Table 2). Based on Bakeman’s (2000) recommendations for inter-coder reliability, Kappa values between 0.60 and 0.75 are considered “good” while scores greater than 0.75 are considered excellent.
Table 2.
Reliability report
| Week1 | Week2 | Week3 | ||
|---|---|---|---|---|
| Average | Kappa | 0.67 | 0.77 | 0.77 |
| Range | Kappa | - | 0.76–0.78 | 0.74–0.80 |
Note. The ranges of Kappa were not available for week 1 since there were only 2 coders coded in that week.
Identifying the behavior patterns to be tested
Based on the research question, two classes of behavior patterns were analyzed. The first class was the clinician-initiated pattern (i.e. the clinician gaze preceded the patient’s gaze). Three sequential behavior pairs were included in this category: 1) clinician-gaze-patient (DGP) followed by patient-gaze-clinician (PGD), 2) clinician-gaze-chart (DGC) followed by patient-gaze-chart (PGC), and 3) clinician-gaze-other artifact (DGO) followed by patient-gaze-other artifact (PGO). The second class of behavior pattern was the patient-initiated pattern, (i.e. the patient’s gaze preceded the clinician’s gaze). The three sequential behavior pairs in this pattern were similar to the ones in the clinician-initiated pattern, but in a reversed sequence: 1) patient-gaze-clinician (PGD) followed by clinician-gaze-patient (DGP), 2) patient-gaze-chart (PGC) followed by clinician-gaze-chart (DGC), and 3) patient-gaze-other artifact (PGO) followed by clinician-gaze other-artifact (DGO). The sequences related to patient-gaze-unknown (PGU) and clinician-gaze-unknown (DGU) were not considered. Two behavior patterns and respective sequential behavior pairs are shown in Table 3.
TABLE 3.
Behavior patterns investigated in this study
| Pattern | Sequential behavior pair
|
|
|---|---|---|
| Initial Behavior | Response Behavior | |
| Doctor directed pattern | clinician gaze patient (DGP) | patient gaze clinician (PGD) |
| clinician gaze chart (DGC) | patient gaze chart (PGC) | |
| clinician gaze other artifact (DGO) | patient gaze other artifact (PGO) | |
| Patient directed pattern | patient gaze clinician (PGD) | clinician gaze patient (DGP) |
| patient gaze chart (PGC) | clinician gaze chart (DGC) | |
| patient gaze other artifact (PGO) | clinician gaze other artifact (DGO) | |
Note. Clinician gaze unknown (DGU) and patient gaze unknown (PGU) were not included in the behavior patterns identified.
Generating contingency tables
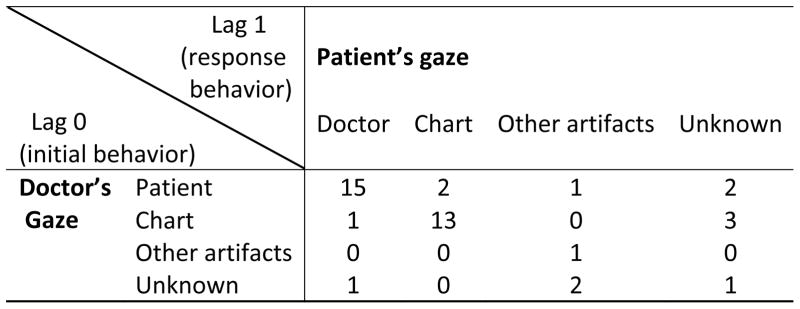
The concept of “lag” was defined differently for each of the two methods of generating the contingency table. For the first method, lag was defined based on events, regardless of time. For example, if lag 0 represented the initial gaze behavior of the clinician or patient, then lag 1 represented the subsequent response behavior of the other participant. There were two tables generated for each encounter; one was the patient’s behavior following the clinician’s behavior, the other one was the clinician’s behavior following the patient’s behavior. An example of the contingency table generated by this approach is shown in Figure 1. The purpose of generating the event-based lag contingency table was to determine the frequency of sequential behavior pairs.
Figure 1.
An example of an event-based lag contingency table generated from one coded video.
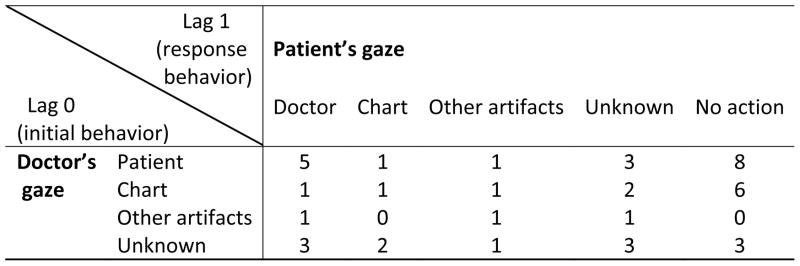
In the second method, we defined lag based on a two-second interval. Lag 0 represented the moment when the initial behavior occurred. Lag 1 represented the first gaze behavior of the other participant occurring during 0–2 second after lag 0. Lag 2 represented the first behavior of another participant that occurred during 2–4 second after lag 0. Lag 3, 4, and 5 represent 4–6, 6–8, and 8–10 second intervals respectively. Similar to the event-based tables, two tables were generated for each lag, so there were 10 tables generated for each encounter. In this case, a new behavior category was added to the table – “no action”, which meant that no behavior was recorded for the target participant during that time period. An example of the contingency table generated by the method is shown in Figure 2. Lags 1 through lag 5 were investigated in the time-based lag table, i.e., the analysis included response behaviors within 10 seconds of the initial behavior. As timing of the response behavior could be examined through time-based lag tables, these tables were used for answering the temporal immediacy questions.
Figure 2.
An example of time-based lag contingency table generated from one coded video.
There were 12 contingency tables generated for each individual video. Sets of 12 tables were pooled together for each clinician. Lag sequential analysis with the procedure described in the following section was applied to the data from each clinician. The tests showed that different clinicians had similar tendencies (in terms of eye gaze behavior patterns), so the tables for each clinician were pooled together into a single table. Finally 12 contingency tables (2 for event-based analysis and 10 for time based analysis) were generated for the whole data set and the general initial response behavior pattern was examined.
Testing the connection of the sequential behavior pairs
Several statistical techniques were applied in the lag-sequential analysis method. An initial likelihood-ratio chi-square test was conducted for each table generated. The expected cell values in the test were calculated by assuming the behaviors listed in the column and the behaviors listed in the row were independent. The purpose of this test was to determine whether the cell values were distributed by chance in the whole table level. Next, the unconditional probability, conditional probability, and adjusted residual were calculated for each table cell found significant in the first step. This step identifies specific behavior pairs showing a strong association in terms of initial-response sequence. Unconditional probability was an expected value, which assumed that clinician behaviors and patient behaviors were independent. Conditional probability was calculated according to the observed value. Adjusted residual was a parameter comparing the observed value with the expected value, which assumed independence. Although other investigators have used an adjusted residual above 1.96 per cell to indicate significant association between the initial behavior and the response behavior (Bakeman & Quera, 1995), we applied a more restrictive criterion 2.58 (α=0.01) to control Type I error. Statistically speaking, a cell with an adjusted residual lower than −2.58 should also be considered significant; however, this study only emphasized cells with adjusted residuals over 2.58 since that level implies positive linkage between the initial behavior and the response behavior. The calculations for chi-square test and adjusted residual were done with the general log-linear function of SPSS (version 17.0). Finally, Yule’s Q was calculated for the sequential behavior pairs in the two behavior patterns. Yule’s Q was used for cross-table comparison of the two behavior patterns as it is a transformation of odds ratio and unaffected by the total event frequency of the whole table (Bakeman & Gottman, 1997; Bakeman, McArthur, & Quera, 1996). Yule’s Q estimates the strength of the association between behavior pairs.
RESULTS
General description of the gaze behavior
The average total communication length during the encounters was 192.8 seconds (standard deviation 122.8, range 27s–643s). The duration of the gaze behaviors relative to total communication length (%) and the average frequencies of occurrence of each gaze behavior per visit are shown in Table 4.
TABLE 4.
General statistical description of gaze behavior
| Patient’s behavior
|
Doctor’s behavior
|
|||||||
|---|---|---|---|---|---|---|---|---|
| PGD | PGC | PGO | PGU | DGP | DGC | DGO | DGU | |
| Average percentages of duration | 55.37% | 27.51% | 2.87% | 14.24% | 44.38% | 45.07% | 3.27% | 7.29% |
| Average frequencies | 14.37 | 6.94 | 2.27 | 6.96 | 16.41 | 13.57 | 2.65 | 2.28 |
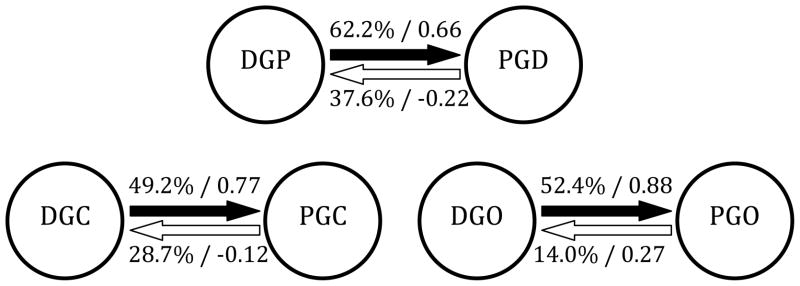
Event-based lag sequential analysis
Likelihood-ratio chi-square was 556.7 (df=9) for the clinician-initiated pattern table and 163.3 (df=9) for the patient-initiated pattern table. Both estimates exceeded the 0.01 critical values of 21.67, so cell values in both tables were not distributed by chance. The observed frequencies, conditional probabilities, and adjusted residuals of the response behaviors in clinician-initiated and patient-initiated patterns are shown in Tables 5 and 6, respectively, with the significant cells highlighted. All the initial-response behavior pairs in the clinician-initiated pattern showed significant connection. In contrast, no sequential behavior pair had significance in the patient-initiated pattern. This finding was supplemented by Yule’s Q values for the sequential behavior pairs in both patterns (see Table 7).
TABLE 5.
Observed frequencies, Conditional probabilities and adjusted residuals of patients’ behaviors in response to clinicians’ behaviors
| Initial behavior | Response behavior
|
|||
|---|---|---|---|---|
| PGD | PGC | PGO | PGU | |
| DGP | 450 | 81 | 54 | 138 |
| 62.2% (15.45) | 11.2% (−11.51) | 7.5% (−3.93) | 19.1% (−3.19) | |
| DGC | 147 | 320 | 32 | 152 |
| 22.6% (−11.92) | 49.2% (17.59) | 4.9% (−6.25) | 23.3% (0.35) | |
| DGO | 36 | 9 | 76 | 24 |
| 24.8% (−4.07) | 6.2% (−5.55) | 52.4% (16.70) | 16.6% (−1.90) | |
| DGU | 73 | 31 | 28 | 83 |
| 34.0% (−2.16) | 14.4% (−3.96) | 13.0% (1.04) | 38.6% (5.86) | |
Note. Values in parentheses were adjusted residuals. Highlighted cells showed statistical significance, α<0.01.
TABLE 6.
Observed frequencies, Conditional probabilities and adjusted residuals of clinicians’ behaviors in response to patients’ behaviors
| Initial behavior | Response behavior
|
|||
|---|---|---|---|---|
| DGP | DGC | DGO | DGU | |
| PGD | 330 | 330 | 95 | 123 |
| 37.6% (−4.67) | 37.6% (4.60) | 10.8% (2.90) | 14.0% (−1.83) | |
| PGC | 276 | 131 | 19 | 31 |
| 60.4% (8.67) | 28.7% (−2.01) | 4.1% (−4.10) | 6.8% (−6.03) | |
| PGO | 43 | 17 | 18 | 51 |
| 33.3% (−2.33) | 13.2% (−4.86) | 14.0% (2.12) | 39.5% (7.78) | |
| PGU | 111 | 94 | 24 | 70 |
| 37.1% (−2.29) | 31.5% (−0.41) | 8.0% (−0.55) | 23.4% (4.09) | |
Note. Values in parentheses were adjusted residuals. Highlighted cells showed statistical significance, α<0.01.
TABLE 7.
Yule’s Q for sequential behavior pairs
| clinician-initiated pattern
|
patient-initiated pattern
|
||
|---|---|---|---|
| sequential behavior pairs | Yule’s Q | sequential behavior pairs | Yule’s Q |
| DGP-PGD | 0.66 | PGD-DGP | −0.22 |
| DGC-PGC | 0.77 | PGC-DGC | −0.12 |
| DGO-PGO | 0.88 | PGO-DGO | 0.27 |
Time-based lag sequential analysis
Likelihood-ratio chi-square tests were conducted for the tables generated from each lag. As the degree of freedom of the time-based lag tables was 12, the 0.01 critical values for the tables were 26.22. Results showed that only the tables for lag 1 and lag 2 showed dependence between the behavior pairs for the whole table (see Table 8).
TABLE 8.
Likelihood-ratio chi-square result of contingency tables for each time-based lag
| Patient’s behavior following clinician’s behavior | |||||
|---|---|---|---|---|---|
| Lag 1 | Lag 2 | Lag 3 | Lag 4 | Lag 5 | |
| G2 | 344.42 | 42.11 | 16.00 | 13.89 | 14.17 |
| Doctor’s behavior following patient’s behavior | |||||
| Lag 1 | Lag 2 | Lag 3 | Lag 4 | Lag 5 | |
| G2 | 68.48 | 27.88 | 25.24 | 7.42 | 22.24 |
Note. Highlighted cells showed statistical significance, α<0.01.
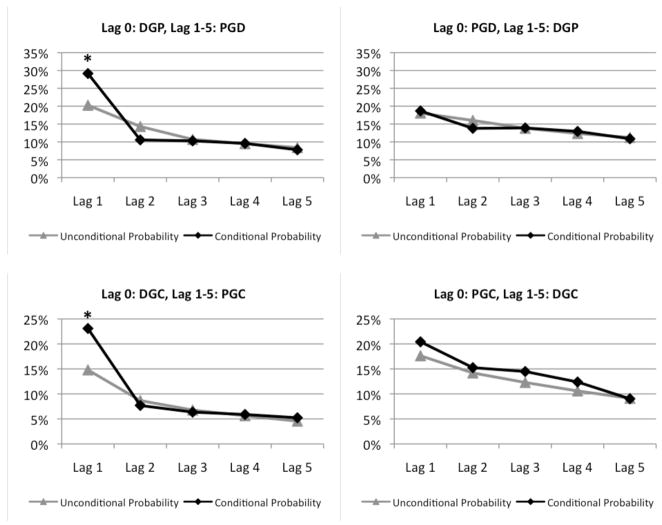
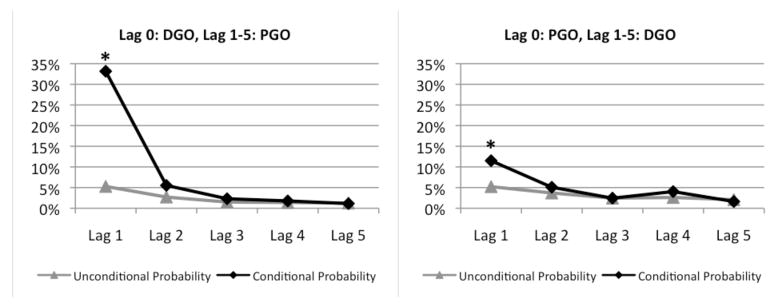
Sequential behavior pairs were analyzed in the two behavior patterns picked for cross lag comparison. Figure 3 shows the conditional probabilities and unconditional probabilities of the particular sequential behavior pairs in each lag. All behavior pairs in the clinician-initiated pattern and for PGO-DGO showed significant connection in lag 1. No significance was found in the subsequent lags.
Figure 3.
Comparison of the sequential behavior pairs of the two behavior patterns with time-based lag sequential analysis in multiple lags, in terms of conditional probabilities and unconditional probabilities. The * means the behavior showed statistical significance (α<0.01) in that lag.
DISCUSSION
This study sought to provide insight into how clinicians’ eye gaze orientation is related to patients’ eye gaze orientation. We found, in general, that patients followed where the clinician was gazing and this occurred relatively soon after the clinician’s gaze behavior. This implies that the clinician’s gaze is related to the patient’s gaze during the medical encounter and may influence the patient’s gaze. Whether this is a direct causal relationship will need to be tested in future studies.
Overall, event-based lag analysis showed clinician gaze predicted patients’ gaze. Average gaze duration as a percent of total encounter time for each modifier of gaze was similar for clinician and patient (see Table 4). However, the conditional probability and Yule’s Q value of the initial-response sequences for the sequential behavior pairs in two patterns were very different. Figure 4 shows these differences more explicitly. We conclude that clinician-initiated patterns were the main gaze behavior rather than patient-initiated patterns in this research sample, which involved brief (2–3 minutes) non-physical interactions in ambulatory clinician-patient encounters.
Figure 4.
Differences in conditional probabilities and Yule’s Q between the behavior pairs when they were in opposite sequences. These values showed that clinician’s gaze behavior was related to patient’s gaze behavior, but patient’s behavior was not.
There were two main findings in the time-based lag analysis. First, only the tables of lag 1 and lag 2 showed significance in the likelihood-ratio chi-square test. This means that any association between an initial and subsequent gaze behavior disappeared after four seconds. Second, findings in the association between lag 0 and lag 1 in time-based lag sequential analysis matched findings in the event-based lag sequential analysis. In lag 1, all the behavior pairs in clinician-initiated pattern were significant whereas only PGO-DGO is significant in the patient-initiated pattern.
We found advantages to using both event-based and time-based lag sequential analysis. Event-based analyses determined whether behavioral pairs were significantly associated, independent of time. Time-based analyses were able to distinguish associations between behavior pairs in different time periods, but could not discern general trends of association because its lags were constrained by time. Combining these two methods allows each to compensate for the limitations of the other.
In this study, patients’ gaze tended to follow physicians’ gaze. There are several theories related to eye contact that may explain these results. Senju and Johnson (2009) define the eye contact effect as the “phenomenon that perceived eye contact with another human face modulates certain aspects of the concurrent and/or immediately following cognitive processing” (p. 129). Social, cognitive and physiological theories have been proposed to explain the effect of humans returning the gaze of those who look at them.
Studies have shown that eye contact influences neurological activity in infants. For example, Farroni et al. (2002) argue that infants learn that eye contact communicates important information and they therefore prefer to look at faces that are mutually gazing at them. Senju and Johnson (2009) suggest that there is a developmental basis for the eye contact effect, because human infants are “equipped with a bias to detect and orient towards faces that make eye contact with them,” (p. 131). Therefore, humans are biologically equipped to look at people who are looking at them. If clinicians are the initiators of gaze in an encounter, they may influence the return gaze of other individuals.
There is also evidence that adult humans are not necessarily aware of their own gaze behaviors (i.e. gaze leakage) or those of others. A classic study conducted by Argyle and Williams (1970) found that participants were unable to identify whether confederates were gazing at them 20% or 80% of the time. Our results may be explained through these social and developmental theoretical perspectives. First, because infants and children receive information-related benefits from returning gaze, adults may also be pre-disposed to returning gaze. This effect may be further amplified in situations where humans are unclear of the social expectations and when they are interested in gaining as much information as possible from their communication partner. Examples of these situations would be health care settings where patients are interested in learning about their condition and may be more attuned to the clinician’s nuanced communication patterns. This behavior may also occur in situations where individuals need to make quick decisions about a person’s trustworthiness with little evidence. The gaze-related studies described also imply that patients who followed their clinician’s gaze may not have been aware of their gaze behaviors or their clinicians’ gaze behaviors. Patients may unconsciously follow clinician’s nonverbal behaviors, because following their gaze provided them with potentially useful information about the encounter. While this theory is viable, recent cognitive science research may offer further explanation.
Cognitive science research has explored the effects of being gazed at and several studies have found connections between eye contact, communication (Kleinke, 1986) and neurological structures sometimes referred to as the ‘social brain.’ The social brain is a “network of regions of the adult cortex activated during social perception and cognition tasks” (Johnson et al., 2005, p. 599). Within this body of literature, the affective arousal model provides insight into why individuals are compelled to return gaze. In this model, researchers argue that “eye contact activates brain arousal systems and/or elicits a strong emotional response” (Senju & Johnson, 2009, p. 129). Thus, being looked at activates positive emotional arousal systems, which then initiates successive perceptual and cognitive processes. In support of this model there are physiological correlates associated with being looked at (Andersen, Guerrero, Buller, & Jorgensen, 1998), including galvanic skin response (Nichols & Champness, 1971), heart rate (Kleinke & Pohlen, 1971) and electroencephalographic activity (Gale, Lucas, Nissin, & Harpham, 1972). This model suggests that eye contact between patients and may facilitate important and possibly unappreciated social interactions. Patients may have unconscious physiological reactions to nonverbal interactions that influence how they perceive their clinician and the health encounter. If such interactions are not facilitated or are inhibited by information technologies, patients may perceive their healthcare encounters more negatively. The method proposed in this manuscript provides a promising tool for investigating this intriguing hypothesis.
Study Limitations
This study has limitations. First, for an individual coded video, the total amount of tallies was too small to divide into different sub-episodes to test whether it was stationary (whether or not sequential relationships were consistent throughout the encounter). With 16 cells for the event-based lag table and 20 for the time-based lag table, the total event frequency of a table would need to be 4 or 5 times higher to obtain more valid statistical results (Bakeman & Gottman, 1997; Wickens, 1989).
Second, the classic lag-sequential analysis method has limitations in distinguishing different episodes (Connor et al., 2009). In this case, pooling tables from individual videos into one table may introduce problems such as “outlier” episodes (i.e. episodes that contain very different sequential relationships with the rest of the episodes), which could skew the results. Given the exploratory nature of this non-experimental study, causality cannot be inferred from a non-experimental design and future research should explore these variables using a more controlled design.
Third, although our inter-coder reliability could be considered “good” (Bakeman, 2000), improvements to the methodology might improve reliability in future studies. Two potential improvements could be: improving the resolution (or facial close-ups) of the videos to avoid ambiguity of the gaze direction and introducing an automated coding system to replace human coders.
Finally, these clinician-patient interactions were part of a larger study in which the clinical encounters were relatively simple and the patients did not have pre-existing relationships with these clinicians. Patients who have existing relationships with clinicians may exhibit different non-verbal behaviors. Gaze analyses in other types of clinical encounters might yield different results.
CONCLUSION
This study found that clinician gaze was associated with subsequent patient gaze orientation, but not the converse, in the medical encounters. This finding may have implications for medical practice design. For instance, unidirectional influence of gaze may reflect underlying processes important for clinical outcomes such as education, healing, and informed decision-making. Control of gaze direction may reflect underlying communication and relationship dynamics important for clinical interaction. Also, analyses such as those portrayed here could be developed to measure important constructs such as patient-centeredness. Other proximal measures such as patient satisfaction may be influenced by dominance or mutuality of gaze.
Individual clinicians will interact with different patients in different ways. Participants in this study were relatively homogenous in terms of illness, and race/ethnicity. Studies have shown that demographic variables such as health status, race/ethnicity, and gender concordance may be important factors to consider in studies of patient perception of care providers, and clinical encounters (Cooper-Patrick et al., 2009; Cooper-Patrick et al., 2004). The lag sequential analysis method can provide insights into questions about interactional differences related to outcomes related to gender, socioeconomic status, language, and race/ethnicity as well as differences in patients with socially stigmatizing illnesses, e.g., HIV/AIDS and substance abuse. Future research can explore gaze behavior in settings where patients have existing relationships with clinicians and settings with varied demographics.
Future questions
Future studies should explore the underlying meaning behind clinician-initiated gaze. If clinician’s nonverbal behaviors influence patient’s nonverbal communication, they might be more important in trust-critical work systems such as primary health care than previously appreciated. Post-visit interviews and surveys might provide additional insight into patients’ nonverbal behaviors and their association with the patient-clinician relationship. These results may influence training interventions and the implementation of technology (e.g. documentation systems) in primary care encounters. These findings may also inform theory about patients’ roles in clinical encounters. Other nonverbal cues besides gaze should be studied. Physicians may benefit from targeted training in nonverbal interactional cues, particularly when they use computers or other health information technologies during clinical encounters.
We can then determine how to use these models to design systems that account for the important human-human interactions that occur in health care systems. The results of this study suggest that technologies used in human-human interactions, such as computers, might impair the clinician’s ability to initiate eye contact with patients. This method can help us better understand when and why these differences might exist and can be used to lead effective system interventions such as training for clinicians, appropriately designed technologies and physical work environments, and educational tools for patients.
Acknowledgments
This publication was supported by grant 1UL1RR025011 from the Clinical & Translational Science Award (CTSA) program of the National Center for Research Resources of the National Institutes of Health. The University of Wisconsin-Madison Systems Engineering Initiative for Patient Safety (SEIPS) provided support on this project http://cqpi.engr.wisc.edu. The authors thank undergraduate research assistants who assisted with data analysis, the editor Matt Wiegner and three anonymous reviewers for their many helpful suggestions. The trial from which these data come was sponsored by the National Center for Complementary and Alternative Medicine at the National Institutes of Health (NCCAM grant #R01AT001428) and was registered as NCT00065715.
References
- Andersen PA, Guerrero LK, Buller DB, Jorgensen PF. An empirical comparison of three theories of nonverbal immediacy exchange. Human Communication Research. 1998;24(4):501–535. [Google Scholar]
- Argyle M, Lefebvre L, Cook M. The meaning of five patterns of gaze. European Journal of Social Psychology. 1974;4(2):125–136. [Google Scholar]
- Argyle M, Salter V, Nicholso H, Williams M, Burgess P. Communication Of inferior and superior attitudes by verbal and non-verbal signals. British Journal of Social and Clinical Psychology. 1970;9:222–231. [Google Scholar]
- Bakeman R. Behavioral observation and coding. In: Reis HT, Judd CM, editors. Handbook of research methods in social and personality psychology. Cambridge: Cambridge University Press; 2000. pp. 138–159. [Google Scholar]
- Bakeman R, Gottman J. Observing interaction: An introduction to sequential analysis. New York, NY: Cambridge University Press; 1997. [Google Scholar]
- Bakeman R, McArthur D, Quera V. Detecting group differences in sequential association using sampled permutations: Log odds, kappa, and phi compared. Behavior Research Methods Instruments and Computers. 1996;28(3):446–457. [Google Scholar]
- Bakeman R, Quera V. Analyzing interaction: Sequential analysis with SDIS & GSEQ. New York, NY: Cambridge University Press; 1995. [Google Scholar]
- Barrett B, Rakel D, Chewning B, Marchand L, Rabago D, Brown R, Scheder J, Schmidt R, Gern JE, Bone K, Thomas G, Barlow S, Bobua J. Rationale and methods for a trial assessing placebo, echinacea, and clinician-patient interaction in the common cold. EXPLORE: The Journal of Science and Healing. 2007;3(6):561–572. doi: 10.1016/j.explore.2007.08.001. [DOI] [PubMed] [Google Scholar]
- Bensing J. Doctor-patient communication and the quality of care. Social Science & Medicine. 1991;32(11):1301–1310. doi: 10.1016/0277-9536(91)90047-g. [DOI] [PubMed] [Google Scholar]
- Bensing JM, Kerssens JJ, van der Pasch M. Patient-directed gaze as a tool for discovering and handling psychosocial problems in general practice. Journal of nonverbal behavior. 1995;19(4):223–242. [Google Scholar]
- Blumenthal D. Stimulating the adoption of health information technology. New England Journal of Medicine. 2009;360(15):1477–1477. doi: 10.1056/NEJMp0901592. [DOI] [PubMed] [Google Scholar]
- Borrero CSW, Borrero JC. Descriptive and experimental analyses of potential precursors to problem behavior. Journal of applied Behavior analysis. 2008;41(1):83–96. doi: 10.1901/jaba.2008.41-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowers CA, Jentsch F, Salas E, Braun CC. Analyzing communication sequences for team training needs assessment. Human Factors. 1998;40(4):672–680. [Google Scholar]
- Buller DB, Street RL. Physician-patient relationships. In: Feldman R, editor. Application of Nonverbal Behavioral Theories and Research. Hillsdale, NJ: Lawrence Erlbaum; 1992. pp. 119–141. [Google Scholar]
- Buller MK, Buller DB. Physicians’ communication style and patient satisfaction. Journal of Health and Social Behavior. 1987;28(4):375–388. [PubMed] [Google Scholar]
- Butler MA. Foraging mode of the chameleon, Bradypodion pumilum: a challenge to the sit-and-wait versus active forager paradigm? Biological Journal of the Linnean Society. 2005;84(4):797–808. [Google Scholar]
- Carayon P. Human factors of complex sociotechnical systems. Applied Ergonomics. 2006;37(4):525–535. doi: 10.1016/j.apergo.2006.04.011. [DOI] [PubMed] [Google Scholar]
- Carayon P, Alvarado CJ, Hundt AS. Work system design in health care. In: Carayon P, editor. Handbook of Human Factors and Ergonomics in Health Care and Patient Safefty. Mahwah: Lawrence Erlbaum Associates, Inc; 2007. [Google Scholar]
- Chau PYK, Hu PJ. Examining a model of information technology acceptance by individual professionals: an exploratory study. Journal of Management Information Systems. 2002;18(4):191–229. [Google Scholar]
- Clark HH, Brennan SE. Grounding in communication. In: Resnick LB, Levine JM, Teasley SD, editors. Perspectives on socially shared cognition. Washington: APA Books; 1991. [Google Scholar]
- Clark HH, Schaefer EF. Collaborating on contributions to conversations. Language and cognitive processes. 1987;2(1):19–41. [Google Scholar]
- Clark HH, Schaefer EF. Contributing to Discourse. Cognitive Science. 1989;13(2):259–294. [Google Scholar]
- Clark HH, Wilkes-Gibbs D. Referring as a collaborative process. Cognition. 1986;22(1):1–39. doi: 10.1016/0010-0277(86)90010-7. [DOI] [PubMed] [Google Scholar]
- Connor M, Fletcher I, Salmon P. The analysis of verbal interaction sequences in dyadic clinical communication: A review of methods. Patient Education and Counseling. 2009;75(2):169–177. doi: 10.1016/j.pec.2008.10.006. [DOI] [PubMed] [Google Scholar]
- Cook M, Smith JM. The role of gaze in impression formation. The British Journal of Social and Clinical Psychology. 1975;14(1):19–19. doi: 10.1111/j.2044-8260.1975.tb00144.x. [DOI] [PubMed] [Google Scholar]
- Cooper LA, Powe NR Commonwealth Fund. Disparities in Patient Experiences, Health Care Processes, and Outcomes: The Role of Patient-Provider Racial, Ethnic, and Language Concordance. New York, NY: Commonwealth Fund; 2004. [Google Scholar]
- Cooper-Patrick L, Gallo JJ, Gonzales JJ, Vu HT, Powe NR, Nelson C, Ford DE. Race, gender, and partnership in the patient-physician relationship. Jama-Journal of the American Medical Association. 1999;282(6):583–589. doi: 10.1001/jama.282.6.583. [DOI] [PubMed] [Google Scholar]
- Del Piccolo L, Mazzi MA, Dunn G, Sandri M, Zimmermann C. Sequence analysis in multilevel models. A study on different sources of patient cues in medical consultations. Social Science & Medicine. 2007;65(11):2357–2370. doi: 10.1016/j.socscimed.2007.07.010. [DOI] [PubMed] [Google Scholar]
- DiMatteo MR, Taranta A, Friedman HS, Prince LM. Predicting patient Satisfaction from physicians’ nonverbal communication skills. Medical Care. 1980;18(4):376–387. doi: 10.1097/00005650-198004000-00003. [DOI] [PubMed] [Google Scholar]
- Drapeau M, de Roten Y, Beretta V, Blake E, Koerner A, Despland J. Therapist technique and patient defensive functioning in ultra-brief psychodynamic psychotherapy: a lag sequential analysis. Clinical Psychology & Psychotherapy. 2008;15(4):247–255. doi: 10.1002/cpp.575. [DOI] [PubMed] [Google Scholar]
- Eide H, Quera V, Finset A. Exploring rare patient behaviour with sequential analysis: An illustration. Epidemiologia e Psichiatria Sociale. 2003;12(2):109–114. doi: 10.1017/s1121189x00006175. [DOI] [PubMed] [Google Scholar]
- Eide H, Quera V, Graugaard P, Finset A. Physician-patient dialogue surrounding patients’ expression of concern: applying sequence analysis to RIAS. Social Science & Medicine. 2004;59(1):145–155. doi: 10.1016/j.socscimed.2003.10.011. [DOI] [PubMed] [Google Scholar]
- Ellsworth PC, Ludwig LM. Visual behavior in social interaction. Journal of Communication. 1972;22(4):375–403. [Google Scholar]
- Epstein RM, Hadee T, Carroll J, Meldrum SC, Lardner J, Shields CG. ‘Could this be something serious?’ Reassurance, uncertainty, and empathy in response to patients’ expressions of worry. JGIM: Journal of General Internal Medicine. 2007;22(12):1731–1739. doi: 10.1007/s11606-007-0416-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Exline RV, Eldridge C. Effects of two patterns of a speaker’s visual behavior upon the perception of the authenticity of his verbal message. Paper presented at the meeting of the Eastern Psychological Association; Boston. 1967. [Google Scholar]
- Farroni T, Csibra G, Simion F, Johnson MH. Eye contact detection in humans from birth. Proceedings of the National Academy of Sciences of the United States of America. 2002;99(14):9602–9602. doi: 10.1073/pnas.152159999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gale A, Lucas B, Nissin R, Harpham B. Some EEG correlates of face to face contact. British Journal of Social and Clinical Psychology. 1972;11:326–332. doi: 10.1111/j.2044-8260.1972.tb00822.x. [DOI] [PubMed] [Google Scholar]
- Gottman JM, Roy AK. Sequential analysis: A guide for behavioral researchers. New York: Cambridge University Press; 1990. [Google Scholar]
- Harrigan J, Oxman T, Rosenthal R. Rapport expressed through nonverbal behavior. Journal of Nonverbal Behavior. 1985;9(2):95–110. [Google Scholar]
- Hemsley GD, Doob AN. The effect of looking behavior on perceptions of a communicator’s credibility. Journal of Applied Social Psychology. 1978;8(2):136–142. [Google Scholar]
- Holden RJ. Cognitive performance-altering effects of electronic medical records: an application of the human factors paradigm for patient safety. Cognition, Technology & Work. 2010:1–19. doi: 10.1007/s10111-010-0141-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou H, Chang K, Sung Y. Analysis of problem-solving-based online asynchronous discussion pattern. Educational Technology & Society. 2008;11(1):17–28. [Google Scholar]
- Johnson MH, Griffin R, Csibra G, Halit H, Farroni T, De Haan M, et al. The emergence of the social brain network: Evidence from typical and atypical development. Development and psychopathology. 2005;17(03):599–619. doi: 10.1017/S0954579405050297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kauffeld S, Meyers R. Complaint and solution-oriented circles: Interaction patterns in work group discussions. European Journal of Work and Organizational Psychology. 2009;18(3):267–294. [Google Scholar]
- Kiesler DJ, Auerbach SM. Integrating measurement of control and affiliation in studies of physician-patient interaction: the interpersonal circumplex. Social Science & Medicine. 2003;57(9):1707–1722. doi: 10.1016/s0277-9536(02)00558-0. [DOI] [PubMed] [Google Scholar]
- Kleiner BM. Macroergonomics: work system analysis and design. Human Factors: The Journal of the Human Factors and Ergonomics Society. 2008;50(3):461–467. doi: 10.1518/001872008X288501. [DOI] [PubMed] [Google Scholar]
- Kleinke CL. Gaze and eye contact: a research review. Psychological Bulletin. 1986;100(1):78–100. [PubMed] [Google Scholar]
- Kleinke CL, Meeker FB, Fong CL. Effects of gaze, touch, and use of name on evaluation of. Journal of Research in Personality. 1974;7(4):368–373. [Google Scholar]
- Kleinke CL, Pohlen PD. Affective and emotional responses as a function of other person’s gaze and cooperativeness in a two-person game. Journal of Personality and Social Psychology. 1971;17(3):308–313. doi: 10.1037/h0030600. [DOI] [PubMed] [Google Scholar]
- Kraut RE, Poe D. Behavioral roots of person perception: The deception judgments of customs inspectors and laymen. Journal of Personality and Social Psychology. 1980;39(5):784–798. [Google Scholar]
- Krippendorff K. Content Analysis: An Introduction to Its Methodology. Thousand Oaks: SAGE; 2004. [Google Scholar]
- Larsen K, Smith C. Assessment of nonverbal communication in the patient-physician interview. The Journal of Family Practice. 1981;12(3):481. [PubMed] [Google Scholar]
- Malterud J. “Feeling your large intestines a bit bound”: clinical interaction-talk and gaze. Scandinavian Journal of Primary Health Care. 1999;16(4):211–215. doi: 10.1080/028134398750002972. [DOI] [PubMed] [Google Scholar]
- Margalit RS, Roter D, Dunevant MA, Larson S, Reis S. Electronic medical record use and physician-patient communication: An observational study of Israeli primary care encounters. Patient Education and Counseling. 2006;61(1):134–141. doi: 10.1016/j.pec.2005.03.004. [DOI] [PubMed] [Google Scholar]
- Martin CV, Smith-Jackson TL. Evaluation of pictorial assembly instructions for young children. Human Factors: The Journal of the Human Factors and Ergonomics Society. 2008;50(4):652–662. doi: 10.1518/001872008X288592. [DOI] [PubMed] [Google Scholar]
- Nichols KA, Champness BG. Eye gaze and the GSR. Journal of Experimental Social Psychology. 1971;7(6):623–626. [Google Scholar]
- Schmid Mast M, Hall JA, Klöckner C, Choi E. Physician gender affects how physician nonverbal behavior is related to patient satisfaction. Medical Care. 2008;46(12):1212–1218. doi: 10.1097/MLR.0b013e31817e1877. [DOI] [PubMed] [Google Scholar]
- Mehrabian A. Inference of attitudes from the posture, orientation, and distance of a communicator. Journal of Consulting and Clinical Psychology. 1968;32:296–308. doi: 10.1037/h0025906. [DOI] [PubMed] [Google Scholar]
- Moore G, Benbasat I. Development of an instrument to measure the perceptions of adopting an information technology innovation. Information Systems Research. 1991;2(3):192–222. [Google Scholar]
- Naiman TH, Breed G. Gaze duration as a cue for judging conversational tone. Representative Research in Social Psychology. 1974;5(2):115–122. [Google Scholar]
- Ong L, De Haes J, Hoos A, Lammes F. Doctor-patient communication: a review of the literature. Social Science & Medicine. 1995;40(7):903–918. doi: 10.1016/0277-9536(94)00155-m. [DOI] [PubMed] [Google Scholar]
- Pearson SD, Raeke LH. Patients’ trust in physicians: Many theories, few measures, and little data. Journal of General Internal Medicine. 2000;15(7):509–513. doi: 10.1046/j.1525-1497.2000.11002.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice RE, Stohl C. Communication and human factors. In: Salvendy G, editor. Handbook of Human Factors and Ergonomics. 3. New York: John Wiley & Sons, Inc; 2006. [Google Scholar]
- Robinson C, Anderson G, Porter C, Hart C, Wouden-Miller M. Sequential transition patterns of preschoolers’ social interactions during child-initiated play: Is parallel-aware play a bidirectional bridge to other play states? Early Childhood Research Quarterly. 2003;18(1):3–21. [Google Scholar]
- Robinson J. Getting down to business: Talk, gaze, and body orientation during openings of clinician-patient consultations. Human Communication Research. 1998;25(1):97–123. [Google Scholar]
- Rogers EM. Diffusion of innovations. 4. New York, NY: Free Press; 1995. [Google Scholar]
- Roter D, Frankel R, Hall J, Sluyter D. The expression of emotion through nonverbal behavior in medical visits. Journal of General Internal Medicine. 2006;21:28–34. doi: 10.1111/j.1525-1497.2006.00306.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruusuvuori J. Looking means listening: Coordinating displays of engagement in clinician-patient interaction. Social Science & Medicine. 2001;52(7):1093–1108. doi: 10.1016/s0277-9536(00)00227-6. [DOI] [PubMed] [Google Scholar]
- Salvucci DD, Mandalia HM, Kuge N, Yamamura T. Lane-change detection using a computational driver model. Human Factors: The Journal of the Human Factors and Ergonomics Society. 2007;49(3):532–542. doi: 10.1518/001872007X200157. [DOI] [PubMed] [Google Scholar]
- Scherer SE, Schiff MR. Perceived intimacy, physical distance and eye contact. Perceptual and Motor Skills. 1973;36(3):835–835. doi: 10.2466/pms.1973.36.3.835. [DOI] [PubMed] [Google Scholar]
- Senju A, Johnson MH. The eye contact effect: mechanisms and development. Trends in Cognitive Sciences. 2009;13(3):127–134. doi: 10.1016/j.tics.2008.11.009. [DOI] [PubMed] [Google Scholar]
- Scrimin S, Axia G, Tremolada M, Pillon M, Capello F, Zanesco L. Conversational strategies with parents of newly diagnosed leukaemic children: An analysis of 4880 conversational turns. Supportive Care in Cancer. 2005;13(5):287–294. doi: 10.1007/s00520-004-0679-1. [DOI] [PubMed] [Google Scholar]
- Shah J, Breazeal C. An empirical analysis of team coordination behaviors and action planning with application to human–robot teaming. Human Factors: The Journal of the Human Factors and Ergonomics Society. 2010;52(2):234–245. doi: 10.1177/0018720809350882. [DOI] [PubMed] [Google Scholar]
- Smith M, Sainfort P. A balance theory of job design for stress reduction. International Journal of Industrial Ergonomics. 1989;4(1):67–79. [Google Scholar]
- Stass JW, Willis FN., Jr Eye contact, pupil dilation, and personal preference. Psychonomic science. 1967;7(10):375–376. [Google Scholar]
- Street RL, Buller DB. Nonverbal response patterns in physician-patient interactions: A functional analysis. Journal of Nonverbal Behavior. 1987;11(4):234–253. [Google Scholar]
- Thayer S, Schiff W. Observer judgment of social interaction: Eye contact and relationship inferences. Journal of Personality and Social Psychology. 1974;30(1):110–114. [Google Scholar]
- Wheeler RW, Baron JC, Michell S, Ginsburg HJ. Eye contact and the perception of intelligence. Bulletin of the Psychonomic Society. 1979;13(2):101–102. [Google Scholar]
- Wickens T. Multiway contingency tables analysis for the social sciences. Hillsdale, NJ: Lawrence Erlbaum Associates; 1989. [Google Scholar]
- Wilson J. Fundamentals of ergonomics in theory and practice. Applied Ergonomics. 2000;31(6):557–567. doi: 10.1016/s0003-6870(00)00034-x. [DOI] [PubMed] [Google Scholar]
- Woods J, Borrero J, Laud R, Borrero C. Descriptive analyses of pediatric food refusal: the structure of parental attention. Behavior Modification. 2010;34(1):35. doi: 10.1177/0145445509355646. [DOI] [PubMed] [Google Scholar]
- Zimmermann C, Del Piccolo L, Mazzi M. Patient cues and medical interviewing in general practice: examples of the application of sequential analysis. Epidemiologia e Psichiatria Sociale. 2003;12:115–123. doi: 10.1017/s1121189x00006187. [DOI] [PubMed] [Google Scholar]