Abstract
Early treatment of prolonged seizures with benzodiazepines given intravenously by paramedics in the prehospital setting has been shown to be associated with improved outcomes. However, an increasing number of Emergency Medical System (EMS) protocols use an intramuscular (IM) route because it is faster and consistently achievable. RAMPART (Rapid Anticonvulsant Medication Prior to Arrival Trial) is a double-blind randomized clinical trial to determine if the efficacy of IM midazolam is non-inferior by a margin of 10% to that of intravenous (IV) lorazepam in patients treated by paramedics for status epilepticus. Children and adults with >5 minutes of convulsions who are still seizing after paramedic arrival are administered study medication by IM autoinjector or IV infusion. The primary efficacy outcome is absence of seizures at emergency department (ED) arrival, without EMS rescue therapy. Safety outcomes include acute endotracheal intubation and recurrent seizures. Secondary outcomes include timing of treatment and initial seizure cessation. At the time of writing this communication, enrollment of all subjects is near completion and the study data will soon be analyzed.
Keywords: binary outcome, intravenous, intramuscular, lorazepam, midazolam, placebo, seizure termination
Background
Early treatment of status epilepticus (SE) by paramedics reduces the number of patients with persistent seizures on ED arrival and the number admitted to the ICU for refractory status (Alldredge et al., 2001). However, the optimal agent for prehospital treatment of SE is unknown. Intramuscular midazolam is an increasingly popular choice because of its ease of administration and practicality for EMS use, but the safety and efficacy of midazolam or the intramuscular route of administration have not been studied in a randomized controlled trial (Warden & Frederick, 2006). We hypothesized that in the prehospital treatment of SE, the efficacy of intramuscular (IM) midazolam is not inferior to that of intravenous (IV) lorazepam, as determined by the proportion of subjects with termination of clinically evident seizure at arrival in the Emergency Department (ED) after a single dose of study medication and without use of rescue medication.
Methods
This is a double-blind randomized non-inferiority clinical trial of the efficacy of IM midazolam versus IV lorazepam in the prehospital treatment of status epilepticus by paramedics. The trial is being carried out by the Neurological Emergencies Treatment Trials (NETT) network, a multidisciplinary clinical trials infrastructure funded by the National Institute of Neurological Disorders and Stroke (NINDS). The NETT is composed of 17 enrollment Hub sites, a Clinical Coordinating Center, and a Statistical Data Management Center. The Hubs are academic medical centers that coordinate enrollment within a number of Spokes consisting of EMS agencies and other regional academic and community hospitals. RAMPART has relied on more than 4,000 paramedics, 33 EMS agencies, and 79 receiving hospitals across the United States.
Approximately 1,000 adult and pediatric patients with continuing seizure activity after EMS arrival and meeting all inclusion and exclusion criteria are being enrolled and randomized in this trial. All subjects receive active treatment by either IM or IV routes of administration. Adults and children greater than or equal to 40 kg who are randomized to active IM therapy are treated with 10 mg midazolam IM followed by IV placebo. Adults and children greater than or equal to 40 kg who are randomized to IV active therapy are treated with IM placebo followed by 4 mg lorazepam IV. The weight of children is estimated from their length using a length based weight estimation tape that is included in each study box. Active therapy in children estimated to be less than 40 kg is either 5 mg midazolam IM or 2 mg lorazepam IV. Children estimated to be less than 13 kg are not enrolled.
The specially-designed study box incorporates a voice recorder activated by opening the box. Study personnel are instructed to provide verbal statements at the following times: IM treatment, IV access obtained, IV administered, administration of any rescue treatments, when and if convulsions are observed to stop, and whether the subject is seizing on arrival at the ED. The study box has an internal clock that time-stamps all statements.
In situations where it is difficult to start an IV, medics are expected to continue attempts for at least 10 minutes. An intraosseous (IO) route can be used at any time in lieu of IV access. Rescue therapy, as dictated by local EMS protocol, is expected to be used in subjects who are still seizing 10 minutes after the last study medication is administered. In cases where there is a delay in starting the IV and a subject no longer has seizures before IV study drug is given, the study intervention will be considered over and IV study medication does not need to be used. When seizures are observed to resume later during EMS transport, medics are instructed to use rescue therapy defined by local EMS protocol.
The study is being conducted under 21 CFR 50.24, FDA regulations governing emergency clinical research performed with exception from informed consent (EFIC) (FDA, 2005). An EFIC plan for the trial was included in the IND application submitted to the FDA and was approved by the Institutional Review Board (IRB) at the Clinical Coordinating Center. Institutional Review Boards (IRBs) at each NETT site have reviewed community consultation and public disclosure activities and provided local approval. Every EMS system participating in the study is covered under a new or existing Federal Wide Assurance delineating an IRB of record for that system. Subjects or their legally authorized representatives are notified about enrollment in the trial by the study team as soon as possible, and they are asked for approval for the study team to continue collecting data until the subject’s end of study.
Outcomes
The primary outcome measure is the binary outcome variable measuring whether or not there is termination of convulsive seizure activity prior to arrival in the ED after an initial dose of study medication without the need for a second “rescue” dose of benzodiazepine by EMS. Determination of termination of convulsive seizure activity upon arrival at the receiving emergency department is made clinically by the attending emergency physician treating the subject. Key secondary outcome measures include times from EMS arrival to termination of seizure and from initiation of treatment to termination of seizure. Other secondary outcomes include frequency of endotracheal intubation, the frequency and duration of hospitalization and of ICU admission, and the frequency of acute seizure recurrence. Time data are collected using an instrumented logger device that determines time of arrival and records voice time stamps when medications are given or convulsions are noted to have stopped.
Analysis
The primary analysis used in this trial will test the hypothesis that IM midazolam is not less effective than IV lorazepam on the primary endpoint by more than an absolute difference of 10% (i.e., non-inferiority margin) (Dunnett & Gent, 1977). Based on preliminary studies we estimate that 70% of subjects will terminate seizure prior to ED arrival after the initial dose of IV lorazepam. An absolute difference in the proportion of terminated seizures at ED arrival of less than 10% between the two treatment groups is considered to be clinically unimportant and is defined as the non-inferiority margin. The value of this margin is based on a combination of statistical and clinical judgement and was chosen to ensure that the overall success (termination of seizure) of the new treatment (IM midazolam) has a clinically relevant superiority over a putative placebo as well as a clinically unimportant difference from the currently used benzodiazepines. Based on the above information and taking into consideration the planned interim analysis, the study is powered to assure greater than 90% likelihood of identifying less than a 10% absolute difference in success rates between the two treatment groups. Sample size estimation is based on the comparison of independent proportions with a 1:1 randomization scheme and a one-sided type I error rate of 0.025. The maximum sample size required for randomization is 890 subjects (445 per treatment group). Due to the potential recurrence rate in patients with status epilepticus, the total sample size is inflated by 15% to account for multiple enrollments of a study subject. Subjects will be independent for the primary analysis. Thus approximately 1,024 subjects will be randomized.
Progress
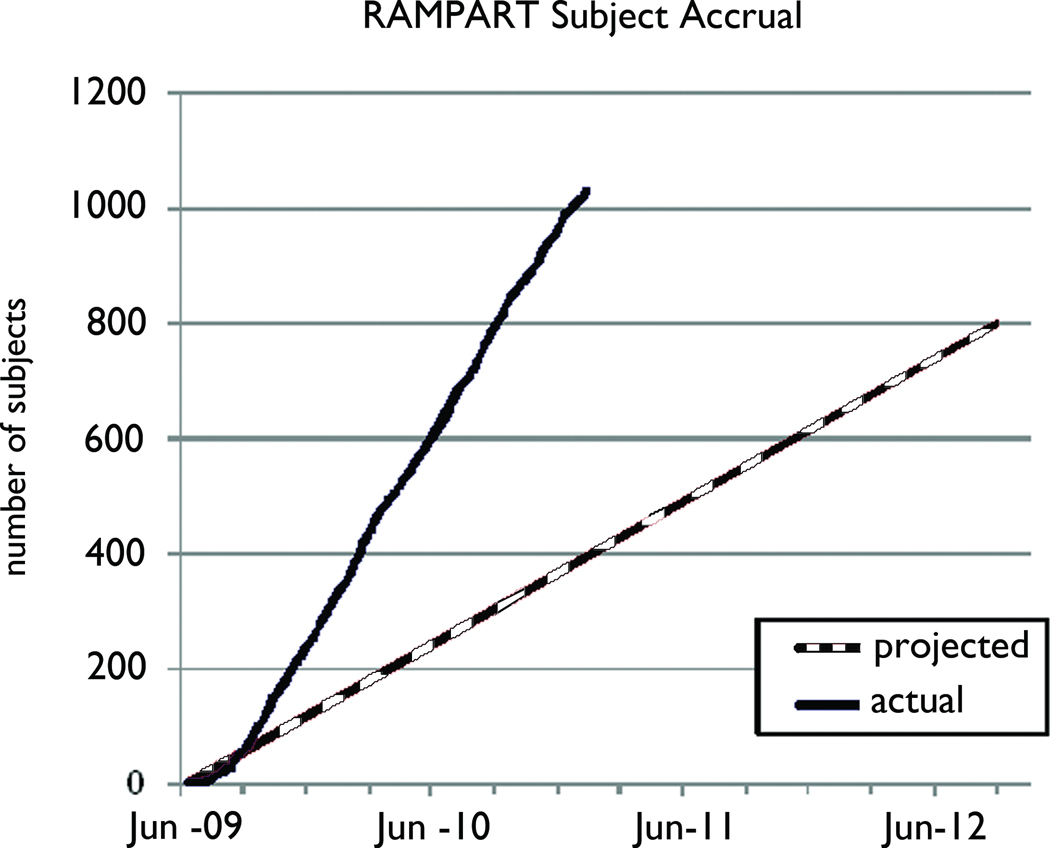
As of the submission of this manuscript, subject enrollment was completed with a total enrollment of 1,023. Analysis of data is currently underway.
Figure 1.
Projected versus actual subject accrual for RAMPART
Acknowledgements
This work is supported by award 5U01NS056975-04 from the National Institute of Neurological Disorders and Stroke (NINDS), the Office of the Director, National Institutes of Health (OD), BARDA, and the NIH CounterACT program. This trial is registered with ClinicalTrials.gov (NCT00809146).
Footnotes
Disclsoures: The authors confirm that they have no conflicts of interest to declare. The authors confirm that they have read the Journal's position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
REFERENCES
- Alldredge BK, Gelb AM, Isaacs SM, Corry MD, Allen F, Ulrich S, Gottwald MD, O’Neil N, Neuhaus JM, Segal MR, Lowenstein DH. A comparison of lorazepam, diazepam, and placebo for the treatment of out-of-hospital status epilepticus. N Engl J Med. 2001;345:631–637. doi: 10.1056/NEJMoa002141. [DOI] [PubMed] [Google Scholar]
- Dunnett CW, Gent M. Significance testing to establish equivalence between treatments, with special reference to data in the form of 2×2 tables. Biometrics. 1977;33:593–602. [PubMed] [Google Scholar]
- FDA. Code of Federal Regulations. U.S. Government Printing Office via GPO Access; 2005. Exception from informed consent requirements for emergency research. (Accessed 21CFR50.24, at http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?fr=50.24.) [Google Scholar]
- Warden CR, Frederick C. Midazolam and diazepam for pediatric seizures in the prehospital setting. Prehosp Emerg Care. 2006;10:463–467. doi: 10.1080/10903120600885126. [DOI] [PubMed] [Google Scholar]