Abstract
Graduation rates in drug courts average 50% to 70%, but it is unclear what proportion of graduates responded to the drug court services and what proportion might not have had serious drug problems upon entry. This study cluster-analyzed urine drug screen results during the first 14 weeks of treatment on 284 participants from three misdemeanor drug courts. A four-cluster solution (R2 > .75) produced distinct subgroups characterized by (1) consistently drug-negative urine specimens (34% of the sample), (2) consistently drug-positive specimens (21%), (3) consistently missed urine specimens (26%), and (4) urine specimens that began as drug-positive but became progressively drug-negative over time (19%). These data suggest that approximately one-third of the participants might not have had serious drug problems upon entry. Approximately one-fifth appeared to respond to drug court services, and nearly one-half continued to exhibit problems after 14 weeks. Implications for adaptive programming in drug courts are discussed.
Keywords: drug courts, drug-involved offenders, criminal justice, cluster analysis
Drug courts are special criminal court dockets that provide judicially supervised substance abuse treatment and case management services to nonviolent, drug-involved offenders in lieu of criminal prosecution or incarceration. According to the National Association of Drug Court Professionals (NADCP, 1997), the “key components” of a drug court include on-going status hearings before the judge to review participants’ progress, mandatory completion of substance abuse treatment and indicated adjunctive services, random weekly urine drug screens, and progressively escalating negative sanctions for infractions and positive rewards for accomplishments. In pre-adjudication drug courts, graduates have the criminal charge(s) dropped and may be eligible for record expungement after remaining arrest-free for a statutorily prescribed waiting period and meeting other obligations, such as paying a filing fee. Record expungement ordinarily permits the individual to respond truthfully on an employment application or similar document that he or she was not arrested for or convicted of the offense (Festinger, DeMatteo, Marlowe, & Lee, 2005). In post-adjudication drug courts, graduates may avoid incarceration, reduce their probationary obligations, or receive a sentence of time served in the drug court program.
The drug court model assumes that participants have a serious drug use problem that fuels or exacerbates their criminal activity (NADCP, 1997). As a result, participants must satisfy an intensive regimen of treatment and supervisory obligations. Evidence suggests, however, that a sizeable proportion of drug offenders do not have a diagnosable substance use disorder (e.g., Kleiman et al., 2003). Studies in several adult drug courts reported that nearly one-half of misdemeanor participants (Marlowe et al., 2003; Marlowe, Festinger, & Lee, 2003) and one-third of felony participants (Marlowe, Festinger, & Lee, 2004) produced sub-threshold drug abuse composite scores on the Addiction Severity Index (ASI) (McLellan et al., 1992) that were not significantly different from a community sample of non-treatment seeking individuals. Despite having been screened-in by program personnel as requiring formal drug treatment, the results of more in-depth and confidential assessments suggested these individuals may not have had an identifiable substance use disorder.
These findings raise a question about how to interpret graduation rates in drug courts. Nationally, drug courts report unusually high graduation rates averaging 50% to 70% (Belenko, 1998, 2001; Belenko, DeMatteo & Patapis, 2007; General Accounting Office, 1997). It is unclear, however, what proportion of those graduates entered the drug court programs with serious drug problems and responded to the drug court services, and what proportion might not have had serious drug problems to begin with. If, in fact, as many as 25% to 30% of drug court clients do not have a serious substance use disorder, then cases manifesting actual symptom improvement might represent roughly half of the graduating cohorts. Moreover, providing high-intensity services to non-clinically disordered individuals might waste resources, take treatment slots away from addicted offenders, or disrupt the clinical operations of the treatment programs. On the other hand, administering self-report assessments at or near entry to treatment could underestimate the severity of participants’ substance use problems (Peters et al., 2000). Some offenders might deny to themselves or minimize to others the degree of their drug involvement. They may have poor insight into their actions or be unwilling to disclose illicit activities to criminal justice authorities. Relying exclusively on self-report assessments could, therefore, lead to high false-negative rates and the denial of drug court services to otherwise needy individuals.
The provision of appropriately tailored clinical services to drug court clients is consistent with the Risk-Needs-Responsivity (RNR) model (Andrews & Bonta, 2006). The RNR model posits that interventions with criminal offenders are most effective if the interventions are properly tailored to the specific criminogenic needs of offenders. As such, tailoring treatments to drug court clients based on their drug use severity would likely be more effective than a one-size-fits-all treatment approach.
The current study sought to shed light on these issues by analyzing the outcome trajectories of 284 participants in three adult misdemeanor drug court programs. Urine results were selected as the dependent measure because (1) abstinence is one of the primary goals of drug court program, (2) urine screens are objectively measured (i.e., not derived from self-report) and therefore a reliable indicator of drug use during the program, and (3) urine data are collected on a weekly basis and thus can be longitudinally analyzed. Exploratory cluster analytic techniques were used to identify typologies of participants characterized by different trajectories of treatment response. We were particularly interested in determining whether there was a subgroup of participants who achieved abstinence early in the programs and remained continuously abstinent thereafter. Such a profile might reflect individuals who did not have serious drug problems upon entry. Importantly, because this study was conducted in misdemeanor drug courts, it might be expected that a greater proportion of participants would meet this profile as compared to felony drug courts that treat a more serious drug offender population.
We were also interested in identifying a sub-group of participants who provided drug-positive urine specimens early in the drug court programs, but who eventually achieved sobriety over time. This profile might reflect what would generally be considered the desired outcome of a drug court program; that is, individuals enter the drug court program with high levels of drug involvement, but reduce or eliminate their drug use after receiving treatment and other services.
Finally, we sought to determine whether baseline Addiction Severity Index (ASI) drug composite scores significantly distinguished cluster membership and predicted trajectories of drug use during participants’ enrollment in the drug court programs. The ASI is commonly used in drug court and drug abuse treatment programs, so examining the ASI’s ability to predict during-treatment drug use trajectories has clear importance. This would provide information about whether self-report assessment results can identify the appropriate target population for a drug court program.
Methods
Participants
The sample consisted of 284 adult drug offenders participating in three misdemeanor drug court programs in Delaware. The drug courts were located in the urban city of Wilmington, the state capital of Dover, and the rural community of Georgetown. Eligibility criteria for these programs required defendants to be 18 years of age or older; charged with a misdemeanor drug offense involving possession or consumption of cannabis, possession of drug paraphernalia, possession of hypodermic syringes, or first-time driving under the influence; and not have a history of an offense involving drug dealing or manufacturing, death or serious injury to a victim, or use of a deadly weapon.
Eighty-seven percent (n = 248) of the participants were recruited as part of experimental studies investigating the effects of judicial status hearings on drug court outcomes. These participants were randomly assigned to meet with the judge for status hearings every 2 weeks (bi-weekly condition) or to be monitored by their clinical case managers who requested status hearings only as needed in response to poor performance in treatment (as-needed condition). The results of those studies revealed no main effects of the experimental conditions; however, there were significant interaction effects, in which participants who had (1) Antisocial Personality Disorder (APD) or (2) a history of drug abuse treatment performed significantly better in the bi-weekly condition (Festinger et al., 2002; Marlowe, Festinger, Dugosh, & Lee, 2005; Marlowe, Festinger, & Lee, 2003, 2004). For this reason, the clusters were compared on the variables of experimental condition (bi-weekly vs. as-needed), APD (yes or no), and prior drug treatment (yes or no) to determine whether these variables would need to be statistically controlled for in between-cluster comparisons. The remaining 13% (n = 36) of the participants were recruited from a natural history study that examined outcomes in the drug courts as usual. Because there was no experimental manipulation in the natural history study, it was not necessary to examine potential covariates for inclusion in the between-cluster comparisons. The experimental participants were recruited from all three drug courts, while the natural history participants were recruited from the drug courts in Dover and Georgetown.
Brief Description of the Drug Court Programs
The three drug court programs are similar in structure. Although there are minor differences in graduation criteria, the core graduation criteria are the same in all three drug courts. The programs are scheduled to be a minimum of 4 or 6 months in length (depending on the jurisdiction), although most participants require 6 to 8 months to satisfy the conditions for graduation. To graduate, participants must, at a minimum, complete a standard regimen of 12 weekly psycho-educational group counseling sessions, provide at least 14 consecutive drug-negative urine specimens, remain arrest-free, and pay a US $200 court fee.
The psycho-educational group sessions cover a standard sequence of prevention topics, including the pharmacology of drug and alcohol use, progression from substance abuse to dependence, the impact of addiction on the family, treatment options, HIV/AIDS risk reduction, and relapse prevention strategies. Participants provide urine specimens on a random, weekly basis in direct observation of a same-gender treatment staff person, and all urine drug screens are performed by an independent certified laboratory.
The judges are authorized to administer punitive sanctions or remedial interventions as consequences for poor performance in the program. These consequences may include verbal reprimands, written homework assignments, additional treatment or supervisory obligations, or day-long attendance in court as an observer. The judge or treatment team can also administer rewards for good performance, including verbal praise, token gifts, certificates of recognition, and reductions in participants’ treatment or supervisory obligations.
Baseline Measures
Participants received a US $20 check for completing a baseline assessment battery that was administered by trained research technicians. This battery included the fifth edition of the Addiction Severity Index (ASI) (McLellan et al., 1992), which assesses current (past 30 days) and lifetime problems in several domains: drug problems, alcohol problems, legal problems, medical problems, family and social problems, employment problems, and psychiatric problems. The ASI yields “composite scores,” based on events occurring during the previous 30 days, that are global indicators of problem-severity in each domain. Composite scores range from 0.00 to 1.00, and they were developed by selectively combining items from each of the ASI problem areas (McGahan, Griffith, Parente, & McLellan, 1986). In prior research, a drug composite score of ≤ .04 efficiently differentiated non-drug users from clinical samples of drug abuse clients (Lee et al., 2001). As such, a drug composite score of ≤ .04 is considered to be sub-threshold for a drug use disorder. Multiple studies of ASI composite scores and lifetime items have yielded impressive evidence of reliability, concurrent validity, predictive validity, and discriminative utility across groups of clients characterized by age, race, gender, and primary drug of abuse (e.g., Alterman et al., 1998; Cacciola, Koppenhaver, McKay, & Alterman, 1999; McDermott et al., 1996; McLellan et al., 1985, 1992; McLellan, Luborsky, O’Brien, & Woody, 1980).
Participants were also administered an “Antisocial Personality Disorder Interview,” which is a 29-item, true/false structured interview that assesses official diagnostic criteria for APD contained in the revised fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) (American Psychiatric Association, 2000). In inter-rater reliability scoring trials, there was between 90% and 100% exact agreement for dichotomous diagnoses of APD among our research technicians.
Finally, participants completed a “Prior Treatment Questionnaire” that inquired about prior drug abuse treatment episodes, the density of services for each episode, discharge status, satisfaction with treatment, and the longest interval of abstinence attained during and after each episode. A single dichotomized (yes or no) item inquiring whether the participant experienced any prior drug abuse treatment (excluding self-help groups) was used for the interaction analyses described above and in the cluster-validation analyses for the current study. Inter-rater reliability and test-retest stability for this item were consistently above 95% in all of our prior studies.
During-Treatment Performance
Measures of during-treatment performance included participants’ attendance at scheduled sessions, results of random weekly urine drug screens, and graduation rates. Urine specimens were delivered in the presence of a same-gender treatment staff person, and drug screens were performed by an independent certified laboratory using the enzyme multiplied immunoassay technique (EMIT) with gas chromatography/mass spectrometry (GCMS) confirmation of positive results on a six-panel screen for cannabis, alcohol, opiates, amphetamines, cocaine, and phencyclidine (PCP) plus any additional substances believed to be used by the individual. The urine specimens were tested for evidence of tampering or invalidity based on an analysis of creatinine, ph, and specific gravity in accordance with standard laboratory testing guidelines. In line with the policies of the drug courts, invalid or tampered specimens were presumed to be drug-positive and the specimens were not credited as having been delivered as directed.
Follow-Up Measures
Participants were scheduled to provide a confidential urine specimen at 6 and 12 months post-admission to the drug courts. The follow-up urine drug screens were performed by research staff using a hand-held device, the Roche Test-Cup 5©, which tested for metabolites of cannabis, opiates, amphetamines, cocaine, and PCP. Participants received a US $30 check for completing each of the 6-month and 12-month follow-ups. The re-contact rate was 60% (n = 170) for the 6-month follow-up urine and 46% (n = 130) for the 12-month follow-up urine.
Data Analyses
A number of investigators have employed cluster-analytic techniques to identify subtypes of drug abuse clients based upon longitudinal patterns of change on outcome measures (e.g., Magura, Kang, Nwakeze, & Demsky, 1998; Marlowe, Festinger, Foltz, Lee, & Patapis, 2005; Morral, Iguchi, Belding, & Lamb, 1997; Prochaska, Velicer, Guadagnoli, Rossi, & DiClemente, 1991; Willis, McNamara, Vaccaro, & Hirky, 1996). Following this approach, we subjected participants’ weekly urine drug-screen results to cluster analyses in SAS (2001, Release 8.02) using a disjoint method via the K-means procedure. This procedure places cases into mutually exclusive categories, in which the Euclidean distances between cases within a cluster are significantly smaller than the distances between cases in different clusters. Although it is common to employ Ward’s Method when conducting exploratory cluster analyses (e.g., Marlowe, Merikle, Kirby, Festinger, & McLellan, 2001), disjoint methods do not require cases to have complete data on all of the clustering variables. This allows for a larger percentage of the sample to be included in the cluster analyses and subsequent validation analyses. Therefore, using a disjoint method has the benefit of increasing the representativeness of the sample and enhancing statistical power for evaluating the convergent and predictive validity of the clusters.
Data analyses were limited to the first 14 weeks of the drug court programs because that is the minimum time period in which any participant could have satisfied the program requirements and graduated from a drug court program. This ensured that there would be an equivalent maximum number of data-points for all study participants, including those who were abstinent from the outset and graduated at 14 weeks. Looking at urine specimens beyond 14 weeks would result in participants having different numbers of data points, which would make the analysis and interpretation of the data more difficult.
Importantly, in drug courts, the failure to provide a scheduled urine specimen is viewed as a separate infraction from drug use, and it often constitutes a more serious violation than providing a drug-positive urine specimen (e.g., Marlowe, 2008; Marlowe & Wong, 2008). This is because the failure to provide a scheduled urine specimen is interpreted by the drug court as an effort at deception or an indication of irresponsibility. A drug court client who fails to provide a urine specimen is thus generally assumed by the drug court to have both engaged in drug use and also to have attempted to conceal the drug use or to have failed to behave responsibly by “owning up” to the drug use. Following this logic, we coded participants’ urine drug-screen results on a 3-point scale, ranging from 0 to 2:
A valid drug-negative urine specimen received a score of 2, reflecting the fact that a urine specimen was delivered as directed and also tested negative for recent drug use.
A valid drug-positive urine specimen received a score of 1, reflecting the fact that a urine specimen was delivered as directed, but tested positive for recent drug use.
An unexcused missing urine specimen or invalid or tampered specimen received a score of 0, reflecting the fact that a urine specimen was not delivered as directed and was presumed to have been drug-positive.
Results
Participants
Of the 284 participants, 183 (64%) were from Wilmington, 71 (25%) were from Georgetown, and 30 (11%) were from Dover. They were predominantly male (77%), young adult (mean age ± SD = 25.0 ± 8.0 years), Caucasian (57%) or African-American (37%), unmarried (82%), and high school educated (11.7 ± 1.5 years). Thirty-two percent of the participants met DSM-IV diagnostic criteria for APD, and 25% reported a history of drug abuse treatment. There were no significant differences between the three drug court programs in terms of participants’ age, gender, marital status, years of education, rates of APD, or history of drug abuse treatment. However, there was a significantly greater proportion of African-Americans in the Wilmington sample (44%) as compared to Dover (20 %), χ2 (2, n = 213) = 7.46, p = .02, and Georgetown (24 %), χ2 (2, n = 254) = 9.19, p = .01. Analyses of the initial urine specimens provided upon admission to the drug court programs revealed that the 44.0% of the participants (n = 125) tested positive for marijuana and 9.2% (n = 26) tested positive for cocaine. Other drugs were rarely used and each accounted for approximately 1% or less of the drug-positive urine specimens. It is important to note that cannabis has the longest detection window in urine, so it is possible that participants were using other drugs that were missed by the urine screens.
Clusters
Four disjoint cluster analyses were performed examining between three and six possible cluster solutions. All of the cluster solutions produced an acceptable pseudo F-statistic and a significant R2. We settled on the four-cluster solution because it (1) accounted for a substantial proportion of the variance in the data (R2 > .75), (2) yielded clusters that had sufficient cell sizes (n > 50 per cell) to conduct between-cluster comparisons, and (3) produced clusters that were all logically interpretable and potentially clinically relevant.
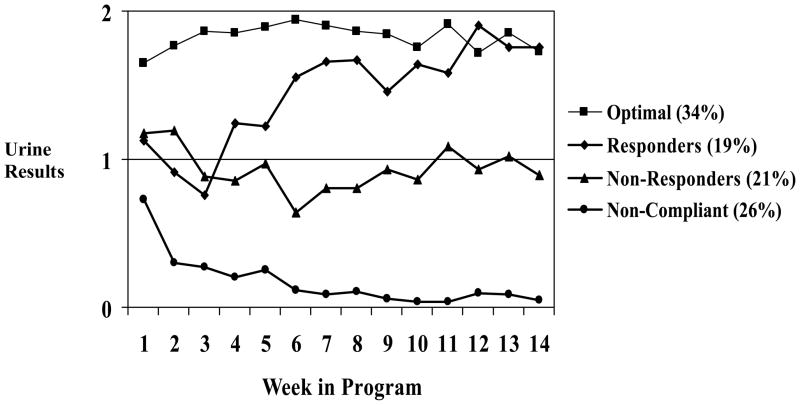
The mean scores for the four-cluster solution are depicted in Figure 1. The average clusters were distinctly classifiable as reflecting (1) consistently drug-negative urine specimens, (2) consistently drug-positive urine specimens, (3) consistently missed urine specimens, and (4) urine specimens that started out as drug-positive but became progressively drug-negative after approximately 6 weeks.
Figure 1.
Mean profiles for a four-cluster solution. 2 = drug-negative urine specimen. 1 = drug-positive urine specimen. 0 = failure to provide a valid urine specimen.
Cluster One: “Optimal Performers”
Ninety-six participants (34% of the total sample) were classified into an average cluster characterized by consistently drug-negative urine specimens. These individuals were generally capable of achieving abstinence soon after entry into the programs and continued at that optimal level of performance over the next 14 weeks.
Cluster Two: “Responders”
Fifty-four participants (19%) were classified into an average cluster characterized by urine specimens that started out as drug-positive, but became drug-negative after approximately 6 weeks in the programs. These participants were labeled as responsive because they exhibited decreased drug use after having been exposed to several weeks of the drug court interventions.
Cluster Three: “Non-Responders”
Sixty-one participants (21%) were classified into an average cluster characterized by consistently drug-positive urine specimens. Although these participants were generally compliant in terms of providing urine specimens when directed to do so, their performance did not improve during the initial 14 weeks of the programs.
Cluster Four: “Non-Compliant”
Seventy-three participants (26%) were classified into an average cluster characterized by a frequent failure to provide scheduled urine specimens. These individuals generally exhibited spotty attendance, submitted invalid or tampered specimens, or absconded from the programs.
Baseline ASI Drug Composite Scores
Nearly one-half of the sample (n = 129, 46%) produced sub-threshold ASI drug composite scores (≤ .04), similar to a community sample of non-treatment seeking individuals. Participants classified as “Optimal Performers” were significantly more likely to produce sub-threshold ASI drug composite scores (63%) compared to participants classified as “Responders” (34%), “Non-Responders” (40%), or “Non-Compliant” (38%), χ2 (3, n = 281) = 16.58, p < .001.
We examined the sensitivity and specificity of the ASI, using the ≤ .04 cut-off, for predicting membership in the Optimal Performers cluster. In this context, sensitivity refers to the correct identification of participants as being Optimal Performers (i.e., true positive rate) and specificity refers to the correct identification of participants as not being Optimal Performers (i.e., true negative rate). Sensitivity and specificity were both 0.63, indicating that the ASI correctly predicted membership in the Optimal Performers cluster roughly two-thirds of the time.
Between-Cluster Comparisons
Table 1 presents between-cluster comparisons on demographic and outcome variables. The analyses focused on comparing Optimal Performers to the remaining participants, which is consistent with the primary goal of this project (i.e., determining if there was a sub-group of participants who achieved abstinence early in the programs and remained consistently abstinent thereafter). Prior to conducting these analyses, we determined whether there were site-by-cluster differences. Results revealed that Wilmington had a significantly lower proportion of Optimal Performers as compared to Dover and Georgetown, χ2 (2, n = 284) = 15.67, p = .001. Therefore, site was entered as a covariate. The clusters did not differ by research condition, APD, or prior drug treatment, and it was therefore not necessary to control for these variables in the analyses.
Table 1.
Between-cluster comparisons (Optimal Performers vs. the other clusters) on demographic and outcome variables controlling for site differences: n (%) or mean (SD)
| Optimal Performers | Responders | Non-Responders | Non-Compliant | p | |
|---|---|---|---|---|---|
| Total sample (N = 284) | 96 (34%) | 54 (19%) | 61 (21%) | 73 (26%) | |
| Site | .001 | ||||
| Wilmington | 47 (49%) | 31 (57%) | 40 (66%) | 65 (89%) | |
| Dover | 13 (14%) | 5 (9%) | 8 (13%) | 4 (5%) | |
| Georgetown | 36 (37%) | 18 (33%) | 13 (21%) | 4 (5%) | |
| Research condition | n.s. | ||||
| As needed | 39 (41%) | 29 (54%) | 31 (51%) | 35 (48%) | |
| Bi-weekly | 40 (42%) | 19 (35%) | 23 (38%) | 32 (44%) | |
| As usual | 17 (18%) | 6 (11%) | 7 (11%) | 6 (8%) | |
| APD diagnosis | 26 (27%) | 18 (33%) | 20 (33%) | 28 (38%) | n.s. |
| Prior drug treatment | 19 (20%) | 9 (17%) | 16 (27%) | 26 (36%) | n.s. |
| Sub-threshold ASI drug composite score at entry | 60 (63%) | 18 (34%) | 24 (40%) | 27 (38%) | .001 |
| Gender | n.s. | ||||
| Male | 72 (75%) | 41 (76%) | 46 (75%) | 59 (81%) | |
| Female | 24 (25%) | 13 (24%) | 15 (25%) | 14 (19%) | |
| Race | .022 | ||||
| African-American | 19 (20%) | 19 (35%) | 27 (44%) | 39 (53%) | |
| Caucasian | 72 (75%) | 30 (56%) | 31 (51%) | 29 (40%) | |
| Other | 5 (5%) | 5 (9%) | 3 (5%) | 5 (7%) | |
| Age | 25.85 (9.27) | 23.91 (6.18) | 26.11 (8.76) | 23.78 (6.46) | n.s. |
| Years of education | 12.05 (1.45)a | 11.89 (1.54) | 11.64 (1.67) | 11.30 (1.22)a | .016 |
| Unmarried | 83 (87%) | 49 (94%) | 58 (95%) | 70 (99%) | n.s. |
| Graduation rate | 89 (93%) | 44 (82%) | 27 (44%) | 7 (10%) | .001 |
| Drug-negative urine at 6 month follow-up | 34 (60%) | 17 (46%) | 18 (46%) | 7 (19%) | .002 |
| Drug-negative urine at 12 month follow-up | 14 (30%) | 9 (32%) | 8 (40%) | 8 (23%) | n.s. |
Notes. APD = Antisocial Personality Disorder. ASI = Addiction Severity Index. Sub-threshold ASI drug composite score: ≤ .04.
Optimal Performers were significantly more educated than Non-Compliant (p = .002).
There were no significant differences between the Optimal Performers and participants in the other three clusters in terms of gender, age, or marital status. However, an omnibus ANCOVA revealed a significant difference among the clusters in terms of years of education, F(3, 278) = 3.49, p = .016, η2 = .036, and post-hoc tests revealed that the Optimal Performers were significantly more educated than participants in the Non-Compliant cluster (p = .002). In addition, a significantly greater proportion of Caucasian participants were classified as Optimal Performers as compared to African-American participants, χ2 (6, n = 284) = 14.74, p = .022. Further analyses revealed that this difference was limited solely to Wilmington, and appeared to result from the fact that there was of a larger proportion of African-Americans and a smaller proportion of Optimal Responders in Wilmington.
With regard to longer-term outcomes, participants classified as Optimal Performers had significantly higher graduation rates than participants in the other clusters, χ2 (9, n = 254) = 128.04, p = .001. As noted previously, re-contact rates for the follow-up urine screens were 60% at 6 months and 46% at 12 months. There were no significant differences in follow-up rates between the clusters at either the 6-month (p = .197) or 12-month follow-ups (p = .140); therefore, it was not necessary to control for re-contact rates in the between-cluster comparisons of urine results. Participants classified as Optimal Performers were significantly more likely to provide a drug-negative urine specimen at the 6-month follow-up, χ2 (3, n = 170) = 15.16, p = .002. There was, however, no significant difference in urine results at the 12-month follow-up. This indicates that the Optimal Performers continued to demonstrate superior performance for at least 6 months after their entry into the programs. The relatively low re-contact rate at the 12-month assessment may account for the lack of statistical significance.
Discussion
The results of this study suggest that approximately one-third of participants in three misdemeanor drug court programs may have had relatively minimal drug use problems. These individuals – classified as “Optimal Responders” based upon their urine screen results – were generally capable of achieving abstinence soon after entering the programs and remaining continuously abstinent for most of the ensuing 14 weeks. They were also significantly more likely to test negative for drugs at the 6-month follow-up and to successfully graduate from the programs. In addition, approximately two-thirds of these individuals produced sub-threshold drug composite scores on the Addiction Severity Index (ASI) similar to a community sample of non-treatment seeking individuals. This provides convergent evidence for the existence of a subgroup of individuals who may not have had a clinically significant substance use disorder.
As noted earlier, this finding raises a question about how to interpret success rates for drug court programs. It is possible, for example, that as many as one-half of graduates were drug experimenters who were not predisposed to continue or escalate their drug use. These individuals might have relinquished drug involvement on their own, even if they had not become involved with the criminal justice system.
This does not necessarily imply, however, that these individuals were mismatched to the drug court programs. As described earlier, the programs were specifically developed for misdemeanor offenders charged with low-level offenses related to the possession of marijuana or drug paraphernalia. These pre-adjudication diversion programs are scheduled for a relatively brief period of 4 to 6 months and focus primarily on prevention and psycho-education. Such a regimen could, in fact, be well suited to individuals coming into early contact with the criminal justice system. If these individuals had not been under drug court supervision, they might not have exhibited optimal performance and may have continued to abuse drugs or alcohol.
Regardless, it is possible that such individuals could have been effectively managed in less intensive and less costly programs that do not require over 4 months of group counseling, court hearings, and weekly urine testing. Perhaps they could have been adequately supervised by pre-trial services officers or probation officers, or assigned to alternative tracks within the drug court programs that had lesser service requirements (DeMatteo, Marlowe, & Festinger, 2006, 2007). Several drug courts are developing less-intensive treatment tracks for offenders with less severe drug problems, but data on the effectiveness of these tracks are not yet available. Such an arrangement could conserve scarce resources for the more serious offenders (i.e., those labeled as “Non-Responsive” or “Non-Compliant”) who may require more intensive treatment and supervision to reduce their involvement with drug abuse and crime.
Importantly, approximately one-fifth (19%) of the participants appeared to respond as intended to the drug court interventions. These individuals (n = 54) exhibited substantial drug involvement upon entry into the drug courts and may have required several weeks of services to respond to the interventions. This is not an insubstantial proportion of individuals. Reducing substance abuse and crime among even a few dozen offenders per year could, in the long run, make meaningful contributions to public health and public safety and produce substantial cost-savings for a community. The benefits achieved by this subset of “Responders” could, in themselves, justify the cost and effort of the drug court programs. Importantly, research suggests that drug courts are associated with significant cost savings over traditional criminal justice interventions (Belenko, Patapis, & French, 2005; Bhati, Roman, & Chalfin, 2008; Logan et al., 2004). Whereas incarceration can cost $20,000 to $50,000 per inmate per year, research suggests drug courts cost roughly $3,000 per client per year (Belenko et al., 2005). Tailoring treatment to the needs of the clients could produce even more cost savings.
Nearly one-half (47%) of the participants were labeled as Non-Responsive or Non-Compliant during the first 14 weeks of the programs. This should not, however, be interpreted to mean that treatment was not effective in nearly one-half of the cases. Graduation rates for these specific programs generally exceed 60% to 70% (e.g., Festinger et al., 2002; Marlowe, Festinger, Dugosh, Lee, & Benasutti, 2007; Marlowe, Festinger, & Lee, 2004) and averaged 58% across all three programs in this study. This would suggest that a substantial number of these individuals simply needed more than 14 weeks of exposure to the interventions to succeed.
The results of this study also revealed a significant relationship between baseline ASI drug composite scores and participants’ performance in the drug court programs. The utility of the ASI for predicting DSM-IV substance dependence diagnoses has previously been established (Rikoon, Cacciola, Carise, Alterman, & McLellan, 2006), and the results of the present study suggest that ASI drug composite scores correctly predicted cluster membership for “Optimal Performers” more than 60% of the time. This suggests that the ASI may have practical utility for identifying low-needs drug offenders who could perhaps be managed in less-intensive programs or less-intensive tracks within the drug court programs. As a result, drug courts should use the ASI, along with other screening/assessment measures, to evaluate the needs of clients upon entry into drug courts, which would seemingly permit the most efficient use of limited court and treatment resources.
On the other hand, the ASI produced approximately one-third false negatives and one-third false positives in terms of the classification of Optimal Performers. No measurement tool is perfectly valid and reliable and there will often be an appreciable number of false positives and false negatives in any program. Some individuals with serious drug problems may be erroneously assigned to low-intensity conditions and others with mild problems may be assigned to high-intensity conditions. This requires some mechanism to be in place to adjust the initial assessment as a consequence of participants’ subsequent performance in treatment. For example, if a participant continues to provide drug-positive urine specimens after having been assessed as sub-threshold and placed on a low-intensity track, this should trigger a case review by the drug court treatment team to re-consider the initial disposition.
This approach, sometimes referred to as an adaptive treatment or stepped care model, has been demonstrated to improve outcomes and conserve treatment resources in community-based substance abuse treatment programs (e.g., Breslin et al., 1999; Brooner et al., 2004; Brooner, Kidorf, Stoller, Neufeld, & Kolodner, 2007; Kidorf, Neufeld, King, Clark, & Brooner, 2007; Reid et al., 2003), and has recently shown promise for improving outcomes in drug courts (Marlowe et al., 2007, 2008). Adaptive treatment models adjust the type or dose of serveices administered to clients based on clients’ initial clinical presentation or ongoing performance in treatment (Murphy, Lynch, McKay, Oslin, & TenHave, 2007). Adaptive interventions have been shown to be effective in treating a wide range of substance use disorders involving licit drugs (e.g., tobacco) and illicit drugs (e.g., cannabis) (see Marlowe et al., 2008, for a review). Given the ASI’s rates of false positives and false negatives in terms of classifying Optimal Performers, an adaptive treatment approach may be useful in helping programs adjust the type or dose of treatment over time. More research is needed to identify valid performance indicators for determining whether clients are demonstrating sufficient progress in drug court programs. In addition, research should focus on developing effective adaptive strategies for intervening with non-responsive and non-compliant individuals in drug courts.
Limitations
An important limitation of this study is that it focused exclusively on misdemeanor drug offenders who were charged with relatively minor offenses and did not have serious criminal histories. It is perhaps not unexpected that a substantial proportion of such individuals would not have serious drug problems. However, national data reveal that most drug courts treat felony drug offenders, and an increasing proportion of drug courts utilize post-adjudication models for repeat probation violators (Huddleston, Marlowe, & Casebolt, 2008). It is possible that a substantially larger proportion of participants in felony drug courts or post-adjudication drug courts would have more severe drug use problems. One possibility is that examining drug court clients with more severe drug problems would result in the same cluster solution found in this study, but with difference proportions of offenders in each cluster. Another possibility is that a different cluster would be obtained. Further research should be conducted in felony and post-adjudication programs to determine what proportion of those populations can achieve abstinence after only minimal exposure to the clinical and supervisory interventions. Future research should also examine sub-types of clients based upon the type of drug being abused. Unfortunately, in this study, there was insufficient variance in the type of drug being used, which prevented us from exploring that variable in the cluster analysis.
Because these were relatively brief programs, outcome trajectories were only examined over a 14-week interval. Some individuals who were capable of remaining sober for a few months might have relapsed later in response to new stressors or changing life circumstances. Retaining such individuals in a strict drug court program may be an effective and cost-effective strategy over the long run, even if they are capable of abstaining from drugs on their own in the immediate aftermath of a criminal arrest. Additional research should be conducted over longer follow-up intervals to determine whether outcome trajectories remain stable for several months or even years after participants’ arrests. A related point concerns the re-contact rates, which were 60% at 6 months and 46% at 12 months. Although there were no significant differences in follow-up rates between the clusters at either the 6-month or 12-month follow-ups, it is possible that the re-contacted participants differed in some systematic way from the participants we were unable to re-contact. Future research with higher follow-up rates would be informative.
Finally, the cluster analyses were exploratory in nature, and therefore may have capitalized on chance variation in the derivation sample. It is not unusual to experience “shrinkage” in the variance accounted for (i.e., R2) by clustering algorithms when they are applied to new samples. Additional research is needed to determine whether the clusters remain stable, interpretable, and clinically useful when applied to new samples of drug court clients.
Conclusion
Although drug courts often report impressive graduation rates, there is little information on whether drug court graduates responded to the drug court interventions or perhaps had less severe drug problems upon entry. This study found that over one-third of clients in three misdemeanor drug courts showed little evidence of having a drug use problem upon entry into the drug courts, which raises important questions about how to interpret the documented success of drug courts. The results of this study have implications for how drug courts assess and treat clients. Careful screening upon entry to the drug court can identify clients who have less severe drug use problems. The ASI reliably identified the “Optimal Perfomers” over 60% of the time, and combining the ASI with other assessment approaches would likely result in an increased ability to identify low-needs clients. Moreover, an adaptive ntervention approach that adjusts the intensity of treatment based on clients’ performance in the drug court program may be useful in light of the ASI’s rates of false positive and false negatives. These assessment and treatment approaches will help to ensure that drug court clients are receiving appropriately tailored interventions.
Acknowledgments
This research was supported by Grants No. R01-DA-013096 and R21-DA-022293 from the National Institute on Drug Abuse (NIDA).
Biographies
David DeMatteo is an Assistant Professor of Psychology at Drexel University and Co-Director of the JD/PhD Program in Law and Psychology. His research interests include drug policy, psychopathy, mental health law, and forensic mental health assessment.
Douglas B. Marlowe is Chief of Science, Policy & Law for the National Association of Drug Court Professionals, Senior Scientist at the Treatment Research Institute, and Adjunct Associate Professor of Psychiatry at the University of Pennsylvania School of Medicine. His research focuses on the effects of drug courts and other diversion programs for drug-abusing offenders, the role of coercion in drug abuse treatment, and behavioral treatments for drug abusers and criminal offenders.
David S. Festinger is Director of the Treatment Research Institute’s Section on Law and Ethics Research and Adjunct Assistant Professor of Psychiatry at the University of Pennsylvania School of Medicine. His research focuses on empirically isolating the active mechanisms of drug courts, developing empirically based dispositional procedures for substance abusing offenders, and major ethical questions facing research participants in substance abuse research.
Patricia L. Arabia is a Research Coordinator at the Treatment Research Institute. She is responsible for the operational management of all of the projects in the Law & Ethics Section.
Footnotes
The views expressed are those of the authors and do not necessarily reflect the views of NIDA.
Contributor Information
David DeMatteo, Drexel University.
Douglas B. Marlowe, Treatment Research Institute & National Association of Drug Court Professionals.
David S. Festinger, Treatment Research Institute.
Patricia L. Arabia, Treatment Research Institute.
References
- Alterman AI, McDermott PA, Cook TG, Metzger D, Rutherford MJ, Cacciola JS, et al. New scales to assess change in the Addiction Severity Index for the opioid, cocaine, and alcohol dependent. Psychology of Addictive Behaviors. 1998;12:233–246. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 2000. Text revision. [Google Scholar]
- Andrews DA, Bonta J. The psychology of criminal conduct. 4. Newark, NJ: Lexis Nexis/Matthew Bender; 2006. [Google Scholar]
- Belenko S. Research on drug courts: A critical review. National Drug Court Institute Review. 1998;1:1–42. [Google Scholar]
- Belenko S. Research on drug courts: A critical review: 2001 update. New York: National Center on Addiction and Substance Abuse at Columbia University; 2001. [Google Scholar]
- Belenko S, DeMatteo D, Patapis N. Drug courts. In: Springer DW, Roberts AR, editors. Handbook of forensic mental health with victims and offenders: Assessment, treatment, and research. New York: Springer Publishing Co; 2007. pp. 385–423. [Google Scholar]
- Belenko S, Patapis N, French MT. Economic benefits of drug treatment: A critical review of the evidence for policy makers. Philadelphia, PA: Treatment Research Institute; 2005. [Google Scholar]
- Bhati AS, Roman JK, Chalfin A. To treat or not to treat: Evidence on the prospects of expanding treatment to drug-involved offenders. Wash., DC: Urban Institute; 2008. [Google Scholar]
- Breslin FC, Sobell MB, Sobell LC, Cunningham JA, Sdao-Jarvie K, Borsoi D. Problem drinkers: Evaluation of a stepped-care approach. Journal of Substance Abuse. 1999;10:217–232. doi: 10.1016/s0899-3289(99)00008-5. [DOI] [PubMed] [Google Scholar]
- Brooner RK, Kidorf MS, King VL, Stoller KB, Peirce JM, Bigelow GE, et al. Behavioral contingencies improve counseling attendance in an adaptive treatment model. Journal of Substance Abuse Treatment. 2004;27:223–232. doi: 10.1016/j.jsat.2004.07.005. [DOI] [PubMed] [Google Scholar]
- Brooner RK, Kidorf M, Stoller KB, Neufeld KJ, Kolodner K. Comparing adaptive stepped care and monetary-based voucher interventions for opioid dependence. Drug & Alcohol Dependence. 2007;88:14–23. doi: 10.1016/j.drugalcdep.2006.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacciola JS, Koppenhaver JM, McKay JR, Alterman AI. Test-retest reliability of the lifetime items on the Addiction Severity Index. Psychological Assessment. 1999;11:86–93. [Google Scholar]
- DeMatteo DS, Marlowe DB, Festinger DS. Secondary prevention services for clients who are low risk in drug court: A conceptual model. Crime & Delinquency. 2006;52:114–134. doi: 10.1177/0011128705281746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeMatteo D, Marlowe DB, Festinger DS. The appropriateness of standard drug court treatment for low-risk clients. Offender Substance Abuse Report. 2007;7(6):89–92. [Google Scholar]
- Festinger DS, DeMatteo DS, Marlowe DB, Lee PA. Expungement of arrest records in drug court: Do clients know what they’re missing? Drug Court Review. 2005;5:1–21. [Google Scholar]
- Festinger DS, Marlowe DB, Lee PA, Kirby KC, Bovasso G, McLellan AT. Status hearings in drug court: When more is less and less is more. Drug & Alcohol Dependence. 2002;68:151–157. doi: 10.1016/s0376-8716(02)00187-4. [DOI] [PubMed] [Google Scholar]
- General Accounting Office. Drug courts: Overview of growth, characteristics, and results. Washington, DC: Author; 1997. [Google Scholar]
- Huddleston CW, Marlowe DB, Casebolt R. Painting the current picture: A national report card on drug courts and other problem solving court programs in the United States. 1. II. Alexandria, VA: National Drug Court Institute; 2008. May, [Google Scholar]
- Kidorf M, Neufeld K, King VL, Clark M, Brooner RK. A stepped care approach for reducing cannabis use in opioid-dependent outpatients. Journal of Substance Abuse Treatment. 2007;32(4):341–347. doi: 10.1016/j.jsat.2006.09.005. [DOI] [PubMed] [Google Scholar]
- Kleiman MAR, Tran TH, Fishbein P, Magula MT, Allen W, Lacy G. Opportunities and barriers in probation reform: A case study of drug testing and sanctions. University of California, California Policy Research Center; 2003. [Google Scholar]
- Lee PA, Marlowe DB, Festinger DS, Cacciola JS, McNellis J, Schepise NM, et al. Did “Breaking The Cycle” (BTC) clients receive appropriate services? [abstract]. Drug & Alcohol Dependence; Presentation at the 63rd Annual Scientific Meeting of the College on Problems of Drug Dependence; Scottsdale, AZ. 2001. p. S89. [Google Scholar]
- Logan TK, Hoyt WH, McCollister KE, French MT, Leukefeld C, Minton L. Economic evaluation of drug court: Methodology, results, and policy implications. Evaluation & Program Planning. 2004;27:381–396. [Google Scholar]
- Magura S, Kang SY, Nwakeze PC, Demsky S. Temporal patterns of heroin and cocaine use among methadone patients. Substance Use & Misuse. 1998;33:2441–2467. doi: 10.3109/10826089809059334. [DOI] [PubMed] [Google Scholar]
- Marlowe DB. Application of sanctions. In: Hardin C, Kushner JN, editors. Quality improvement for drug courts: Evidence-based practices. Alexandria, VA: National Drug Court Institute; 2008. pp. 107–114. Monograph Series No. 9. [Google Scholar]
- Marlowe DB, Festinger DS, Arabia PL, Dugosh KL, Benasutti KM, Croft JR, et al. Adaptive interventions in drug court: A pilot experiment. Criminal Justice Review. 2008;33:343–360. doi: 10.1177/0734016808320325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlowe DB, Festinger DS, Dugosh KL, Lee PA. Are judicial status hearings a “key component” of drug court? Six and twelve month outcomes. Drug & Alcohol Dependence. 2005;79:145–155. doi: 10.1016/j.drugalcdep.2005.01.019. [DOI] [PubMed] [Google Scholar]
- Marlowe DB, Festinger DS, Dugosh KL, Lee PA, Benasutti K. Adapting judicial supervision to the risk level of drug offenders: Discharge and six-month outcomes from a prospective matching study. Drug & Alcohol Dependence. 2007;88S:4–13. doi: 10.1016/j.drugalcdep.2006.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlowe DB, Festinger DS, Foltz C, Lee PA, Patapis NS. Perceived deterrence and outcomes in drug court. Behavioral Sciences &the Law. 2005;23:189–198. doi: 10.1002/bsl.636. [DOI] [PubMed] [Google Scholar]
- Marlowe DB, Festinger DS, Lee PA. The role of judicial status hearings in drug court. Offender Substance Abuse Report. 2003;3:33–46. [Google Scholar]
- Marlowe DB, Festinger DS, Lee PA. The judge is a key component of drug court. Drug Court Review. 2004;4(2):1–34. [Google Scholar]
- Marlowe DB, Festinger DS, Lee PA, Schepise MM, Hazzard JER, Merrill JC, et al. Are judicial status hearings a key component of drug court? During-treatment data from a randomized trial. Criminal Justice & Behavior. 2003;30:141–162. [Google Scholar]
- Marlowe DB, Merikle EP, Kirby KC, Festinger DS, McLellan AT. Multidimensional assessment of perceived treatment-entry pressures among substance abusers. Psychology of Addictive Behaviors. 2001;15:97–108. doi: 10.1037//0893-164x.15.2.97. [DOI] [PubMed] [Google Scholar]
- Marlowe DB, Wong CJ. Contingency management in adult criminal drug courts. In: Higgins ST, Silverman K, Heil SH, editors. Contingency management in substance abuse treatment. New York: Guilford Press; 2008. pp. 334–354. [Google Scholar]
- McDermott PA, Alterman AI, Brown L, Zaballero A, Snider EC, McKay JR. Construct refinement and confirmation for the Addiction Severity Index. Psychological Assessment. 1996;8:182–189. [Google Scholar]
- McGahan PL, Griffith JA, Parente P, McLellan AT. Addiction Severity Index: Composite scores manual. Philadelphia, PA: Treatment Research Institute; 1986. [Google Scholar]
- McLellan AT, Cacciola J, Kushner H, Peters R, Smith I, Pettinati H. The fifth edition of the Addiction Severity Index: Cautions, additions and normative data. Journal of Substance Abuse Treatment. 1992;9:461–480. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, Cacciola JS, Griffith J, Evans F, Barr HL, et al. New data from the Addiction Severity Index: Reliability and validity in three centers. Journal of Nervous & Mental Disease. 1985;173:412–423. doi: 10.1097/00005053-198507000-00005. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, O’Brien CP, Woody GE. An improved diagnostic instrument for substance abuse clients: The Addiction Severity Index. Journal of Nervous & Mental Disease. 1980;168:26–33. doi: 10.1097/00005053-198001000-00006. [DOI] [PubMed] [Google Scholar]
- Morral AR, Iguchi MY, Belding MA, Lamb RJ. Natural classes of treatment response. Journal of Consulting &Clinical Psychology. 1997;65:673–685. doi: 10.1037//0022-006x.65.4.673. [DOI] [PubMed] [Google Scholar]
- Murphy SA, Lynch KG, McKay JR, Oslin D, TenHave T. Developing adaptive treatment strategies in substance abuse research. Drug & Alcohol Dependence. 2007;88:S24–S30. doi: 10.1016/j.drugalcdep.2006.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Association of Drug Court Professionals. Defining drug courts: The key components. Washington, DC: Office of Justice Programs, U.S. Dept. of Justice; 1997. [Google Scholar]
- Peters RH, Greenbaum PE, Steinberg ML, Carter CR, Ortiz MM, Fry BC, et al. Effectiveness of screening instruments in detecting substance use disorders among prisoners. Journal of Substance Abuse Treatment. 2000;18:349–358. doi: 10.1016/s0740-5472(99)00081-1. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, Velicer WF, Guadagnoli E, Rossi JS, DiClemente CC. Patterns of change: A dynamic typology applied to smoking cessation. Multivariate Behavioral Research. 1991;26:83–107. doi: 10.1207/s15327906mbr2601_5. [DOI] [PubMed] [Google Scholar]
- Reid R, Pipe A, Higginson L, Johnson K, D’Angelo MS, Cooke D, et al. Stepped care approach to smoking cessation in patients hospitalized for coronary artery disease. Journal of Cardiopulminary Rehabilitation. 2003;23(3):176–182. doi: 10.1097/00008483-200305000-00003. [DOI] [PubMed] [Google Scholar]
- Rikoon SH, Cacciola JS, Carise D, Alterman AI, McLellan AT. Predicting DSM-IV dependence diagnoses from ASI composite scores. Journal of Substance Abuse Treatment. 2006;31:17–24. doi: 10.1016/j.jsat.2006.03.003. [DOI] [PubMed] [Google Scholar]
- SAS Institute. SAS Release 8.02. Cary, NC: Author; 2001. [Google Scholar]
- Willis TA, McNamara G, Vaccaro D, Hirky AE. Escalated substance use: A longitudinal grouping analysis from early to middle adolescence. Journal of Abnormal Psychology. 1996;106:166–180. doi: 10.1037//0021-843x.105.2.166. [DOI] [PubMed] [Google Scholar]