Abstract
Background
Severe trauma arising from electrocution is uncommon, and we wished to study the incidence, risk factors and outcome to identify potential areas of prevention. We therefore studied an active population of adult victims of severe electrical trauma in a large area of Canada (the Calgary Health Region [CHR]).
Methods
From 3 databases, we collected data on all adult (≥18 yr) residents of the CHR who suffered electrical injury associated with an Injury Severity Score of 12 or greater or died as a result of electrocution between Apr. 1, 1996, and Mar. 1, 2002. Of particular interest were the incidence, the age and sex of the victims, the mechanism, the type of electrical power and the outcome.
Results
Ten cases of severe electrical trauma were identified (2.4 per 1 million population annually). Victims' ages were a mean (and standard deviation) of 38.2 (10.3) years. All 10 victims were male for an annual sex-specific incidence of 4.9 per 1 million people. Men aged 18–49 years were nearly 3 times more likely to be victims of electrocution than older men, although this result was not statistically significant (6.1 v. 2.1 per 1 million annually; relative risk 2.9; 95% confidence interval 0.4–127.5). All episodes of electrocution were unintentional, and 7 were occupationally related. All 10 electrocutions resulted from domestically generated current, and 9 were related to power-line exposure. Overall, 6 patients died for a death rate due to severe electrical trauma of 1.4 per 1 million people annually.
Conclusion
This population-based study demonstrates that severe electrocution is rare but is associated with death in the majority of cases in this large Canadian region.
Abstract
Contexte
Les traumatismes graves causés par électrocution sont rares et nous voulions en étudier l'incidence, les facteurs de risque et l'issue afin de définir des domaines possibles de prévention. Nous avons donc étudié une population active d'adultes victimes d'un traumatisme sévère causé par l'électricité dans une grande région du Canada (la Région sanitaire de Calgary [RSC]).
Méthodes
Nous avons recueilli dans trois bases des données sur tous les résidents adultes (≥18 ans) de la RSC ayant été victimes d'un traumatisme causé par électrocution et associé à un indice de gravité de la blessure de 12 ou plus, ou qui sont morts électrocutés, entre le 1er avril 1996 et le 1er mars 2002. Nous nous intéressions particulièrement à l'incidence, à l'âge et au sexe des victimes, au mécanisme de l'incident, au type d'énergie électrique et à l'issue.
Résultats
Nous avons trouvé 10 cas de traumatismes graves causés par électrocution (2,4 par million d'habitants par année). Les victimes avaient en moyenne (et écart type) 38,2 (10,3) ans. Les 10 victimes étaient de sexe masculin, ce qui représente une incidence annuelle spécifique au sexe de 4,2 par million de personnes. Les hommes de 18 à 49 ans étaient presque trois fois plus susceptibles d'être victimes d'électrocution que les hommes plus âgés, même si ce résultat n'était pas statistiquement significatif (6,1 c. 2,1 par million par année; risque relatif de 2,9; intervalle de confiance à 95 %, 0,4–127,5). Aucun des épisodes d'électrocution n'était intentionnel et 7 étaient reliés au travail. Les 10 électrocutions ont été causées par des circuits domestiques et 9 étaient reliées à une exposition à des lignes de transmission. Au total, 6 patients sont morts, ce qui représente un taux de mortalité attribuable à un traumatisme grave causé par électrocution de 1,4 par million de personnes par année.
Conclusion
Cette étude représentative démontre que l'électrocution grave est rare, mais qu'elle entraÎne la mort dans la majorité des cas dans cette grande région canadienne.
Severe trauma resulting from electrical shock has been characterized by multisystem involvement and high death rates.1 Electrical trauma results from the direct effect of electric current, conversion of electrical to thermal energy or mechanical effects including shock waves, projectiles or violent muscle contractions. Although many people have experienced mild electrical shocks from domestic sources, severe trauma arising from electrocution is uncommon. In the United States, estimates of fatalities due to electrocution have been estimated at 5 per 1 million population annually.2,3,4,5 Death attributed specifically to lightning has varied considerably depending on geography, with the highest rates of approximately 1 per 1 million reported from southern US.6,7 Male gender and an occupation requiring exposure to electric current have been proposed as risk factors for severe electrical injury, although the actual risks have been poorly quantified.4,5,6,7,8
To define the burden of disease and risk factors so as to identify potential areas of prevention, population-based studies are optimal. However, existing studies in the literature have been either case reports or series or population-based studies restricted to highly focused populations.9,10,11,12 Further, no population-based studies have been reported from Canada. Our objective was therefore to conduct a population-based surveillance study to define the incidence, risk factors and outcome of severe electrocution in a large Canadian region.
Methods
Patient population
The Calgary Health Region (CHR) is a fully integrated, publicly funded health care system that provides virtually all medical and surgical care to the residents of the cities of Calgary and Airdrie and approximately 20 nearby small towns, villages and hamlets.13 All adult (≥18 yr) residents of the CHR who were victims of severe trauma resulting from electrical injury between Apr. 1, 1996, and Mar. 31, 2002, were included in this study. Severe trauma was defined by an electrical injury associated with a presenting Injury Severity Score (ISS) of 12 or greater or by death before the trauma team could make an assessment.14 This study received approval of the ethics review board at the University of Calgary and CHR.
Study protocol
We used a population-based surveillance cohort design. Study patients were identified by 3 methods. First, the regional trauma services database that prospectively collects information on all patients assessed at the Foothills Medical Centre (FMC) was studied. The FMC is the only tertiary care trauma centre treating adults in southern Alberta and manages all burns and nearly all traumatic injuries occurring among adult residents of the CHR. Second, the Health Information Services database, which records administrative data on all hospitalized patients in the CHR, was searched to identify patients admitted to other acute care facilities in the region. Third, victims of severe electrical trauma who died before the trauma team could make an assessment were identified by the Medical Examiner's Office of Alberta database, which collects information on all unexpected deaths occurring in the CHR. Data from these 3 sources were exported and merged in Excel (Microsoft Corp., Redmond, Wash.). Patients who were not residents of the CHR were excluded. A CHR resident was defined as anybody with a home address within the boundaries of the CHR.7
Statistical analysis
Analysis was performed using Stata version 7.0 (Stata Corp., College Station, Tex.). Incidence and mortality were calculated by taking the numbers of cases observed in the study as the numerator and local population demographic data as the denominator.15 Category specific relative risks were calculated as previously described.16 Ninety-five percent confidence intervals (CIs) were calculated using exact statistics.
Results
Incidence and demographic features
We identified 10 adults, residents of the CHR, who suffered severe electrical trauma over the 6-year study period, for an incidence of 2.4 per 1 million population annually (estimated population at risk over 6 yr = 4 144 824). Six of the 10 patients survived at least to the point of assessment by the trauma team at the FMC. Five cases were clustered during the summer months of 1998, but, with the exception of 2, they were epidemiologically unrelated. Because of the small number of cases over the 6-year period, no clear temporally related trend in occurrence could be established.
Victims' ages ranged from 19 to 52 years (mean and standard deviation [SD] 38.2 [10.3] yr). All 10 victims were male, for an annual sex-specific incidence of 4.9 per 1 million population. Males aged 18–49 years were nearly 3 times more likely to be victims of electrocution than older men, although this finding was not statistically significant (6.1 v. 2.1 per 1 million; relative risk 2.9; 95% CI 0.4–127.5). Although 8 of the 10 victims resided within Calgary city limits, 5 of the electrocutions were documented to have occurred in smaller communities or rural areas within the boundaries of the CHR.
Mechanism of injury
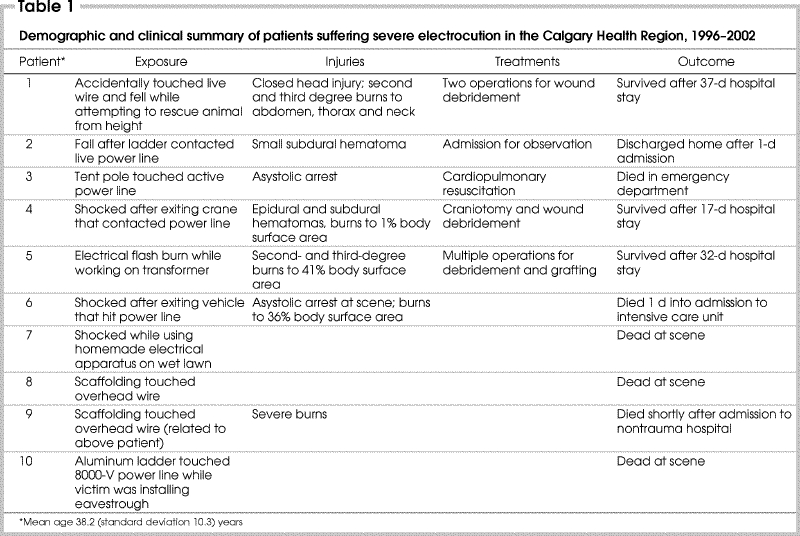
All episodes of electrocution were accidental in nature, and 7 were occupationally related. The mechanism of injury and the outcome are summarized in Table 1. All 10 patients' injuries resulted from domestically generated electric current. All 6 patients who were assessed by the trauma team suffered electrical shock related to power-line sources. Three patients touched power lines with objects, and 2 of these fell from a height after electrocution. Two other patients entered an energized field when they attempted to exit their vehicles after contacting power lines. The remaining patient assessed by the trauma services suffered electrical shock and a flash burn while working on a power transformer. Of the 4 patients who died before assessment by the trauma service, 3 received a shock when ladders or scaffolding contacted active power lines. The remaining patient was electrocuted while using a homemade electrical apparatus on a wet lawn.
Table 1
Management and outcomes
Of the 6 patients assessed by the trauma services, the mean (and SD) ISS was 21.7 (5.6). In general, injuries were characterized by head trauma and burns (Table 1). Two patients presented with asystolic arrest at the accident scene. One of these patients was resuscitated with return of spontaneous circulation, although he died shortly after of complications from severe burns. Of the 4 remaining patients assessed by the trauma service, all survived to hospital discharge (Table 1). Only limited scene details were available for the 4 patients who died before the trauma service could make an assessment at FMC (Table 1). Overall, 6 adult patients died for an annual death rate due to severe electrical trauma of 1.4 per 1 million population.
Discussion
This study provides important information about the epidemiologic features of severe electrical trauma occurring in a large Canadian population. We used the population-based surveillance cohort design that is the standard for observational epidemiologic investigation.16 As a result we were able to establish population incidence and death rates for severe electrical injuries. Although the incidence of severe electrical trauma was low, the case fatality rate was high (60%). This study was adequately methodologically designed to evaluate and quantify category specific risk factors such as age and sex. However, since there was only a small number of cases during surveillance of more than 4 million patient-years and none were female, information on category specific risk factors was limited. Although not statistically significant, young men were at the highest risk for severe electrical trauma in the adult population and represent a target group for future preventive efforts.
A number of clinical observations in this study are noteworthy. First, all 10 electrocutions were caused by domestically generated electrical current; none were from lightning. Clearly, efforts aimed at reducing the impact of serious electrocutions should focus on this aspect. Second, 7 of the 10 cases were occupationally related such that the workplace should be recognized as an area on which to focus preventive efforts. However, the possibility does exist that there is no true association between occupation and electrocution. This is because to convincingly establish an occupational link, knowledge of the baseline workplace exposure of males in the base CHR population would be required as denominator data for comparison. Third, all patients with spontaneous circulation documented at the scene survived and those in asystolic arrest died. There are a number of case reports of electrocuted patients recovering after prolonged resuscitation attempts, and some experts recommend to continue efforts longer than usual for other causes of asystolic arrest that often carry poor prognoses.3,17,18 Since the number of patients in this study was small, our data do not suggest that this practice should be otherwise.
There are few published data with which to compare our incidence and mortality, but our rates appear to be lower than those observed in the US. US studies have suggested death rates due to electrocution of 5–25 per 1 million population annually, although these rates depend on the specific populations studied.3 In addition, lightning injuries vary considerably according to geography, with southern and coastal regions at highest risk. Since the CHR is both land-locked and northern, it is not surprising that there were no cases attributable to lightning in this study. A reason why the electrocution rates were low in our study would be our failure to identify all relevant cases. However, we believe this is an unlikely source of bias because we used a comprehensive case identification protocol that involved 3 independent databases. One potential for missed cases was if CHR residents suffered electrical injuries outside the region and failed to subsequently receive health care services in the CHR. Given that Calgary is geographically isolated from other large metropolitan areas, with the second nearest trauma centre being approximately 300 km away, we believe this bias is minor. Thus, the low rate of electrocution in our study likely reflects the true population incidence.
Conclusions
To our knowledge, this is the first population-based surveillance cohort study conducted in a nonselected Canadian region, and it provides important information regarding the epidemiologic features of severe electrical shock injuries. These injuries occur rarely among residents of the CHR but are associated with high death rates. Although the current public health impact of these injuries is relatively small, there exists an opportunity to prevent approximately 1 death per year among the residents of this region.
Acknowledgments
We thank MaryEllen Arnup, MSc, for her contribution to this article.
Competing interests: None declared.
Correspondence to: Dr. S. Morad Hameed, Trauma Services, Vancouver General Hospital, 855 W 12th Ave., Vancouver BC V5Z 1M9; fax 604 875-5348; morad.hameed@vch.ca
Accepted for publication Nov. 26, 2003.
References
- 1.Jain S, Bandi V. Electrical and lightning injuries. Crit Care Clin 1999;15:319-31. [DOI] [PubMed]
- 2.Lederer W, Wiedermann FJ, Cerchiari E, Baubin MA. Electricity-associated injuries I: outdoor management of current-induced casualties. Resuscitation 1999;43:69-77. [DOI] [PubMed]
- 3.Lederer W, Wiedermann FJ, Cerchiari E, Baubin MA. Electricity-associated injuries II: outdoor management of lightning-induced casualties. Resuscitation 2000;43:89-93. [DOI] [PubMed]
- 4.Ore T, Casini V. Electrical fatalities among U.S. construction workers. J Occup Environ Med 1996;38:587-92. [DOI] [PubMed]
- 5.Wright RK, Davis JH. The investigation of electrical deaths: a report of 220 fatalities. J Forensic Sci 1980;25:514-21. [PubMed]
- 6.Lightning-associated deaths — United States, 1980–1995. MMWR Morb Mortal Wkly Rep 1998;47:391-4. [PubMed]
- 7.Lightning-associated injuries and deaths among military personnel — United States, 1998–2001. MMWR Morb Mortal Wkly Rep 2002;51:859-62. [PubMed]
- 8.Butler ED, Gant TD. Electrical injuries, with special reference to the upper extremities. A review of 182 cases. Am J Surg 1977;134:95-101. [DOI] [PubMed]
- 9.Lipscomb HJ, Dement JM, Rodriguez-Acosta R. Deaths from external causes of injury among construction workers in North Carolina, 1988–1994. Appl Occup Environ Hyg 2000;15:569-80. [DOI] [PubMed]
- 10.Loomis D, Dufort V, Kleckner RC, Savitz DA. Fatal occupational injuries among electric power company workers. Am J Ind Med 1999;35:302-9. [DOI] [PubMed]
- 11.Rossignol M, Pineault M. Classification of fatal occupational electrocutions. Can J Public Health 1994;85:322-5. [PubMed]
- 12.Taylor AJ, McGwin G Jr, Davis GG, Brissie RM, Rue LW 3rd. Occupational electrocutions in Jefferson County, Alabama. Occup Med (Lond) 2002;52:102-6. [DOI] [PubMed]
- 13.Calgary Health Region Web site. Available: www.calgaryhealthregion.ca/hecomm/main/pdf/HecommBrochure.pdf (accessed 2005 May 4).
- 14.Baker S, O'Neill B, Haddon W Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma 1974;14:187-96. [PubMed]
- 15.Alberta Health. Population estimates of Calgary Region by age group, 2000–2007. In: Calgary Health Region [Web site of the Calgary Health Region] Available: www.crha-health.ab.ca/hocr/influ/demo/popage.htm (accessed 2005 Jun 27).
- 16.Laupland KB, Church DL, Mucenski M, Sutherland LR, Davies HD. Population-based study of the epidemiology and the risk factors for invasive Staphylococcus aureus infections. J Infect Dis 2003;187:1452-9. [DOI] [PubMed]
- 17.Brindley PG, Markland DM, Mayers I, Kutsogiannis DJ. Predictors of survival following in-hospital adult cardiopulmonary resuscitation. CMAJ 2002;167:343-8. [PMC free article] [PubMed]
- 18.Doig CJ, Boiteau PJ, Sandham JD. A 2-year prospective cohort study of cardiac resuscitation in a major Canadian hospital. Clin Invest Med 2000;23:132-43. [PubMed]


