Abstract
Background
Treatment of isolated stenosis or occlusion of the left anterior descending (LAD) coronary artery through a left anterior mini-thoracotomy has only recently been advocated as an acceptable alternative to standard coronary artery bypass through a sternotomy and with cardiopulmonary bypass grafting. We reviewed our experience with the minimally invasive direct coronary artery bypass (MIDCAB) procedure.
Methods
A retrospective clinical and angiographic review was conducted on all patients who underwent MIDCAB between October 1998 and February 2002 with subsequent telephone follow-up.
Results
Fifty-two consecutive patients (39 men, 13 women, mean [and standard deviation] age 57.3 [12.3] yr) underwent MIDCAB without videoscopic assistance. Eight patients (15%) were converted intraoperatively to sternotomy, and 5 (10%) patients required cardiopulmonary bypass after conversion. There were no perioperative deaths, myocardial infarctions, re-explorations for bleeding or need for transfusions. At a median follow-up time of 27.7 (range 1.9–40.5) months, there were no late deaths or myocardial infarctions. Four patients had anastomotic stenoses and underwent successful percutaneous coronary angioplasty and are asymptomatic. All patients are free of significant anginal symptoms (Canadian Cardiovascular Society class 0 or I).
Conclusions
Excellent early and mid-term clinical results can be obtained with MIDCAB. To ensure optimal graft quality, conversion to sternotomy should be liberally employed. It is anticipated that the use of an endoscope may limit this complication.
Abstract
Contexte
On préconise depuis peu seulement le traitement de la sténose ou de l'occlusion isolée de l'artère interventriculaire antérieure (AIA) par une mini-thoracotomie antérieure gauche comme solution de rechange acceptable au pontage aortocoronarien standard par sternotomie et circulation extracorporelle. Nous avons étudié notre expérience du pontage aortocoronarien direct à effraction minimale (PACDEM).
Méthode
On a effectué une étude clinique et angiographique rétrospective de tous les patients ayant subi un PACDEM entre octobre 1998 et février 2002 et l'on a procédé à un suivi téléphonique par la suite.
Résultats
Cinquante-deux patients consécutifs (39 hommes, 13 femmes, âgés en moyenne [écart type] de 57,3 [12,3] ans) ont subi un PACDEM pratiqué sans assistance vidéoscopique. Au cours de l'intervention, on a converti huit patients (15 %) à la sternotomie et cinq patients (10 %) ont eu besoin d'une circulation extracorporelle après la conversion. Il n'y a eu aucun décès périopératoire, infarctus du myocarde, nouvelle exploration pour saignement ou besoin de transfusion. Au suivi médian de 27,7 (intervalle de 1,9 à 40,5) mois, on n'a pas constaté de décès tardif ni d'infarctus du myocarde. Quatre patients ont eu une sténose de l'anastomose, ont subi une angioplastie coronarienne percutanée réussie et ne présentent pas de symptôme. Aucun patient ne présente de symptôme significatif d'angine (catégorie 0 ou I de la Société canadienne de cardiologie).
Conclusions
Il est possible d'obtenir d'excellents résultats cliniques précoces et à moyen terme avec le PACDEM. Afin d'assurer une qualité optimale du pontage, il faudrait recourir libéralement à la conversion à la sternotomie. On prévoit que l'utilisation d'un endoscope pourrait réduire cette complication.
Coronary artery bypass grafting (CABG) is one of the most commonly performed surgical procedures in Canada. A most important aspects of this procedure is the use of the left internal thoracic artery (LITA) to bypass lesions in the left anterior descending (LAD) coronary artery. The LITA to LAD bypass graft has excellent long-term patency, which has been associated with improved survival in patients who undergo CABG.1,2 In recent years there have been numerous attempts to minimize the morbidity associated with coronary artery surgery by taking steps to avoid cardiopulmonary bypass and by minimizing the size of the incision. One such technique, developed for the treatment of single-vessel disease of the LAD coronary artery, is minimally invasive direct coronary artery bypass (MIDCAB) grafting. This operation, performed through a left anterior mini-thoracotomy without the use of cardiopulmonary bypass, offers the potential for faster recovery, reduced pain and a decreased need for blood transfusion than conventional CABG.3 However, because of the limited surgical exposure and increased technical difficulty, there has been a concern that this approach could compromise anastomotic accuracy and result in perioperative myocardial infarction and recurrence of angina. This series reflects the application of a standard operative approach and reports the early and mid-term outcomes of MIDCAB at the Ottawa Heart Institute.
Methods
Preoperative and postoperative data were collected prospectively on all patients who underwent MIDCAB grafting between October 1998 and February 2002. Preoperative coronary angiograms on all patients were reviewed, and lesions were classified according to the American Heart Association classification.4 Telephone follow-up was conducted by a research nurse to determine clinical status. Perioperative myocardial infarction was defined as the presence of significant electrocardiographic changes (ST segment elevation, new Q-waves) or a significant rise in troponin T associated with clinical evidence of myocardial infarction (e.g., low cardiac output syndrome, need for inotropes, symptoms of cardiac ischemia). Strict transfusion guidelines were used in determining the use of blood products. Packed red cells were transfused for a hematocrit of less than 21% and fresh frozen plasma was used only with an International Normalized Ratio greater than 1.8 and evidence of bleeding.
Operative technique
After the establishment of general anesthesia, a 7–10-cm standard left anterolateral thoracotomy incision was made in the 5th intercostal space. The pericardium was opened and the target vessel identified. The LITA was exposed using a Ruhltract retractor (Genzyme, Cleveland, Ohio) and harvested under direct vision with the use of low-voltage electrocautery and hemoclips. After the administration of 10 000 units of heparin, Silastic snare sutures were placed proximal and distal to the anastomotic site. Using the Genzyme MIDCAB retractor for stabilization, the LAD artery was opened and the anastomosis constructed with use of a double suture technique and 7–0 polypropylene. We used a shunt only when necessary and did not use ischemic preconditioning. Post-anastomotic Doppler flows were measured in all patients. Conversion to sternotomy was adopted if suboptimal revascularization was suspected due to lack of conduit viability, poor exposure or native vessel problems such as diffuse disease or intramyocardial vessels.
Results
There were 52 patients who underwent the MIDCAB procedure during the study period. The preoperative demographic characteristics are listed in Table 1. A review of the angiograms revealed that 65% of lesions were American Heart Association type C lesions, 25% were type B2, and 10% were type B1. Eight (15%) patients required conversion to sternotomy for technical reasons, which included LITA damage (2), intramyocardial LAD coronary artery (1), pleural adhesions (1) and poor anastomosis quality or graft Doppler flow (4). Five of those patients required cardiopulmonary bypass to revise the graft. Table 2 describes the operative data and postoperative outcomes, and Table 3 presents follow-up information. There were no deaths or perioperative myocardial infarctions. The patients were discharged home at a mean of 4.1 days postoperatively, and 100% of the patients in whom follow-up data were available were symptom-free (Canadian Cardiovascular Society class 0 or I) at a median follow-up of 27 months.
Table 1
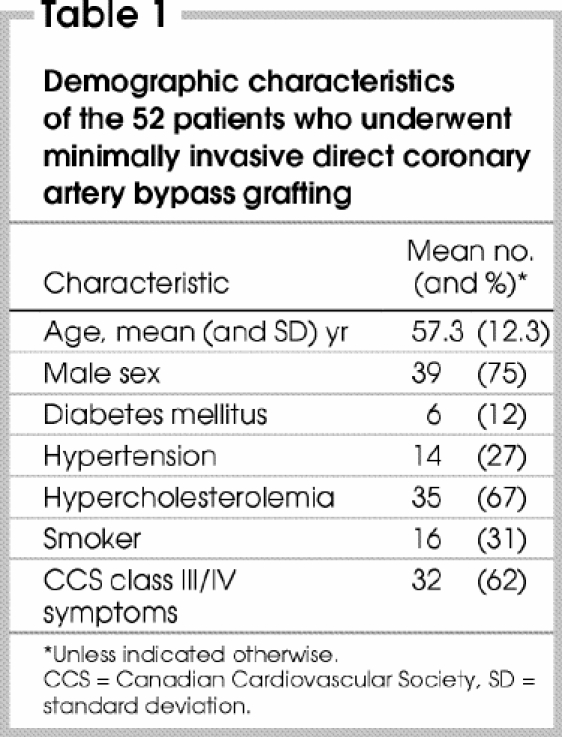
Table 2
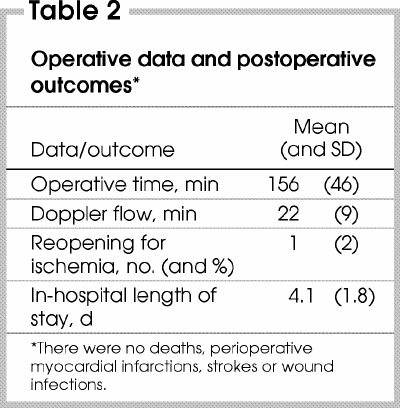
Table 3

Discussion
We have demonstrated herein the safety and efficacy of the MIDCAB procedure, which is comparable to previously published results.5 Essential features of our operative approach include intraoperative graft assessment by transit-time Doppler flow and liberal conversion to sternotomy if a suboptimal result is suspected. Although this approach led to a higher-than-average conversion to sternotomy (15%) in our patients, this may be partly due a learning curve associated with the procedure. Increased experience has led to a reduction in the rate of conversion to less than 5% in the last 20 patients. Four patients who presented postoperatively with symptoms underwent angiography, which revealed anastomotic stenoses. These patients underwent angioplasty without complication and none had a documented postoperative myocardial infarction. Due to its invasive nature and cost, angiographic follow-up was not obtained routinely in asymptomatic patients. However, all patients were free of angina at mid-term (median 27.7 mo) clinical follow-up.
Advances in percutaneous techniques have led to the treatment of the majority of patients having single-vessel coronary disease with a combination of angioplasty and stent placement. Although these techniques produce good results, high-grade lesions of the LAD coronary artery have been identified as being at a higher risk of restenosis and stent failure,6 which can present with periprocedural myocardial injury or late myocardial infarction and recurrence of angina. Conventional CABG, with a sternotomy, use of cardiopulmonary bypass and LITA to LAD bypass grafting offers an excellent long-term outcome but carries higher early morbidity and cost than percutaneous interventions. On the other hand, MIDCAB grafting using the LITA to the LAD bypass represents an ideal strategy for this low-risk patient population because it offers the benefits of low early morbidity and mortality combined with the promise of long-term therapeutic success.
Numerous studies comparing surgical versus percutaneous revascularization for isolated LAD artery disease have demonstrated a higher rate of repeat interventions in the percutaneously treated group.7,8,9,10,11 To date, there have been 2 randomized, controlled trials comparing MIDCAB grafting to percutaneous coronary intervention (PCI) for isolated LAD artery disease. Both demonstrated a benefit in favour of MIDCAB grafting with respect to major adverse cardiac events, which include death, myocardial infarction and the need for repeat revascularization. Recurrence of angina, need for antianginal medications and angiographic stenoses were all higher in the PCI group.12,13
The MIDCAB procedure is a reproducible and effective treatment modality for isolated LAD coronary artery disease, particularly in patients who have failed percutaneous therapy or those with high-risk anatomy that is not amenable to angioplasty and stenting. With the advent of new technologies in interventional cardiology as well as cardiac surgery, the treatment of isolated LAD artery disease is evolving. The use of thoracoscopic assistance in the MIDCAB procedure offers the potential for increased technical accuracy with even smaller incisions and may reduce the rate of conversion to sternotomy. In addition to videoscopic assistance, robotic telemanipulation technology has been used with the goal of performing totally endoscopic coronary artery bypass (TECAB). Several centres have demonstrated the feasibility and procedural success in small series of selected patients.14,15 Evolving technologies in the areas of endoscopic stabilization devices, haptics feedback technology and sutureless anastomosis have been employed in animal models as well as humans and are bringing the goal of TECAB closer to reality.16,17 Although early results are promising, challenges posed by the significant learning curve and cost associated with the application of this technology will have to be overcome before TECAB becomes part of mainstream cardiac surgery.
Conclusions
This case series has demonstrated that the MIDCAB procedure is a safe and effective treatment modality for isolated LAD coronary artery disease and is an important first step in achieving the goal of totally endoscopic coronary artery bypass.
Presented at the Canadian Cardiovascular Congress, Edmonton, Alta., Oct. 26–30, 2002.
Competing interests: None declared.
Correspondence to: Dr. Munir Boodhwani, 40 Ruskin St., H3401, Ottawa ON K1Y 4W7; fax 613 761-4713; mboodhwani@ottawaheart.ca
Reprint requests to: Dr. Fraser Rubens, 40 Ruskin St., Rm. H3403, Ottawa ON K1Y 4W7
Accepted for publication July 21, 2004.
References
- 1.Loop FD, Lytle BW, Cosgrove DM, Stewart RW, Goormastic M, Williams GW, et al. Influence of the internal-mammary-artery graft on 10-year survival and other cardiac events. N Engl J Med 1986;314:1-6. [DOI] [PubMed]
- 2.Cameron A, Davis KB, Green G, Schaff HV. Coronary bypass surgery with internal-thoracic-artery grafts — effects on survival over a 15-year period. N Engl J Med 1996;334:216-9. [DOI] [PubMed]
- 3.Subramanian VA, Patel NU. Current status of MIDCAB procedure. Curr Opin Cardiol 2001;16:268-70. [DOI] [PubMed]
- 4.Smith SC Jr, Dove JT, Jacobs AK, Kennedy JW, Kereiakes D, Kern MJ, et al. ACC/AHA ACC/AHA guidelines for percutaneous coronary intervention (revision of the 1993 PTCA guidelines)-executive summary: a report of the American College of Cardiology/American Heart Association task force on practice guidelines (Committee to revise the 1993 guidelines for percutaneous transluminal coronary angioplasty) endorsed by the Society for Cardiac Angiography and Interventions. Circulation 2001;103:3019-41. [DOI] [PubMed]
- 5.Gill IS, Fitzgibbon GM, Higginson LA, Valji A, Keon WJ. Minimally invasive coronary artery bypass: a series with early qualitative angiographic follow-up. Ann Thorac Surg 1997;64:710-4. [DOI] [PubMed]
- 6.Versaci F, Gaspardone A, Tomai F, Crea F, Chiariello L, Gioffre PA. A comparison of coronary artery stenting with angioplasty for isolated stenosis of the proximal left anterior descending coronary artery. N Engl J Med 1997;336:817-22. [DOI] [PubMed]
- 7.Goy JJ, Kaufmann U, Goy-Eggenberger D, Garachemani A, Hurni M, Carrel T, et al. A prospective randomized trial comparing stenting to internal mammary artery grafting for proximal, isolated de novo left anterior coronary artery stenosis: the SIMA trial. Mayo Clin Proc 2000;75:1116-23. [DOI] [PubMed]
- 8.Hannan EL, Racz MJ, McCallister BD, Ryan TJ, Arani DT, Isom OW, et al. A comparison of three-year survival after coronary artery bypass graft surgery and percutaneous transluminal coronary angioplasty. J Am Coll Cardiol 1999;33:63-72. [DOI] [PubMed]
- 9.Greenbaum AB, Califf RM, Jones RH, Gardner LH, Phillips HR, Sketch MH Jr, et al. Comparison of medicine alone, coronary angioplasty, and left internal mammary artery-coronary artery bypass for one-vessel proximal left anterior descending coronary artery disease. Am J Cardiol 2000;86:1322-6. [DOI] [PubMed]
- 10.Hueb WA, Bellotti G, Almeida S, Arie S, de Albuquerque CP, Jatene AD, et al. The medicine, angioplasty or surgery study (MASS): a prospective, randomized trial of medical therapy, balloon angioplasty or bypass surgery for single proximal left anterior descending artery stenoses. J Am Coll Cardiol 1995;26:1600-5. [DOI] [PubMed]
- 11.Goy JJ, Eeckhout E, Burnard B, Vogt P, Stauffer JC, Hurni M, et al. Coronary angioplasty versus left internal mammary artery grafting for isolated proximal left anterior descending artery stenosis. Lancet 1994;343:1449-53. [DOI] [PubMed]
- 12.Diegeler A, Thiele H, Falk V, Hambrecht R, Spyrantis N, Sick P, et al. Comparison of stenting with minimally invasive bypass surgery for stenosis of the left anterior descending coronary artery. N Engl J Med 2002;347:561-6. [DOI] [PubMed]
- 13.Drenth DJ, Veeger J, Winter JB, Grandjean JG, Mariani MA, Boven van AJ, et al. A prospective randomized trial comparing stenting with off-pump coronary surgery for high-grade stenosis in the proximal left anterior descending coronary artery: three-year follow-up. J Am Coll Cardiol 2002;40:1955-60. [DOI] [PubMed]
- 14.Kappert U, Cichon R, Schneider J, Gulielmos V, Ahmadzade T, Nicolai J, et al. Technique of closed chest coronary artery surgery on the beating heart. Eur J Cardiothorac Surg 2001;20:765-9. [DOI] [PubMed]
- 15.Bonatti J, Schachner T, Bernecker O, Chevtchik O, Bonaros N, Ott H, et al. Robotic totally endoscopic coronary artery bypass: program development and learning curve issues. J Thorac Cardiovasc Surg 2004;127:504-10. [DOI] [PubMed]
- 16.Aybek T, Kessler P, Khan MF, Dogan S, Neidhart G, Moritz A, et al. Operative techniques in awake coronary artery bypass grafting. J Thorac Cardiovasc Surg 2003;125:1394-400. [DOI] [PubMed]
- 17.Carrel TP, Eckstein FS, Englberger L, Berdat PA, Schmidli J. Clinical experience with devices for facilitated anastomoses in coronary artery bypass surgery. Ann Thorac Surg 2004;77:1110-20. [DOI] [PubMed]


