A 54-year-old man came to the emergency department with acutely worsening abdominal pain, nausea, vomiting and low-grade temperature. Approximately 7 months before, he had been diagnosed with multiple myeloma (MM), IgA type. He initially completed 2 cycles of vincristine, doxorubicin (adriamycin), and dexamethasone, and more recently 2 cycles of dexamethasone, cyclophosphamide and etopocide with incomplete response and complicated by febrile neutropenia. His abdomen was distended, with hyperactive bowel sounds.
The results of upright and supine abdominal radiographs suggested an early or incomplete small bowel obstruction and showed a lytic lesion in the left hemipelvis. A subsequent computed tomographic scan revealed multiple intraluminal filling defects well defined within the small bowel, measuring 1–2 cm (Fig. 1). One was associated with a small-bowel intussusception localized to the right lower quadrant (Fig. 2). A previously documented lytic bony lesion of the pelvis was also confirmed (Fig. 2), compatible with the underlying diagnosis of MM.
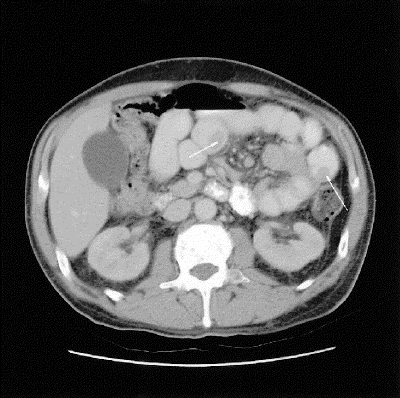
FIG. 1. Axial contrast-enhanced computed tomographic (CT) scan of the abdomen showing 2 well defined, intraluminal filling defects (arrows) within the small bowel.

FIG. 2. Axial contrast-enhanced CT scan of the abdomen showing intussusception (A) in the right lower quadrant. A large mixed lytic and sclerotic lesion in the left hemi-pelvis (B) extending to the sacroiliac joint, typical of multiple myeloma, was noted.
At laparotomy, the patient was found to have an intussusception of his distal ileum. The lead point was a nodular intraluminal lesion within the small bowel. About 20 other, similar lesions were found throughout his small bowel, and several nodularities within his liver.
The intussusception was reduced and its lead point resected along with with 1 other near-obstructing nodular small-bowel lesion. Primary anastomoses were then performed.
Microscopic examination showed the tumour to be composed of sheets of plasma cells. Some areas contained cells that were less mature; the immature cells remained plasmacytoid. The lesions involved the full thickness of the bowel, with obvious accompanying mucosal ulceration. Mesenteric lymph nodes were also found to be involved. In the presence of documented MM, a diagnosis of extramedullary plasmacytoma was made.
The patient did well initially and was discharged home on postoperative day 14 with a view for potential autologous peripheral blood stem cell transplant. Unfortunately, over the next 4 months his MM progressed. After a prolonged course of illness that included recurrent small- bowel obstruction, he died.
Discussion
MM belongs to the family of monoclonal, immunoproliferative plasma-cell neoplasms (plasmacytomas) arising from the B-cell line.1 Malignant plasmoblastic clones generally reside in bone marrow. When on rare occasions they migrate into soft tissues, it is termed extramedullary plasmacytoma (EMP).
EMP has 2 major subtypes, primary (without) and secondary (with prior bone-marrow involvement).1,2,3 Over 70% of primary and secondary EMP occur in the upper æro-digestive tract (nasopharynx, oropharynx, larynx, hypopharynx, trachea and esophagus),3,4 with epidermal lesions also occasionally encountered. Roughly 12% of all primary extramedullary EMP tumours have gastrointestinal involvement, which is much rarer in secondary EMP.5 In patients with MM, EMP may be observed in up to 65% of cases; the majority of these are paraskeletal tumours, with only one-third being true distant spread.5 Intestinal involvement is seldom reported in MM and appears to be a late occurrence.5
Prognosis of intestinal EMP is unclear. In 9 selected patients with MM-associated EMPs, Vaiopulos and colleagues2 reported a median survival of 4.6 years, none with intestinal involvement. Two cases involving the intestinal tract presented by Griffiths and associates5 had fatal outcomes not long after diagnosis with EMP. Our patient unfortunately had a similar course.
Acknowledgments
We would like to thank Annette Foyle, MDCM, Division of Pathology, Queen Elizabeth II Health Sciences Centre, for her contribution to this case report.
Competing interests: None declared.
Correspondence to: Dr. Geoffrey A. Porter, Department of Surgery, Dalhousie University, Surgical Oncology Queen Elizabeth II Health Sciences Centre, Ste. 7-007, Victoria Bldg. VG Site, 1278 Tower Rd., Halifax NS B3H 2Y9; fax 902 473-6496; geoff.porter@dal.ca
Accepted for publication Dec. 15, 2003
References
- 1.Alexiou C, Kau RJ, Dietzfelbinger H, Kremer M, Spiess JC, Schratzenstaller B, et al. Extramedullary plasmacytoma. Cancer 1999;85:2305-14. [PubMed]
- 2.Vaiopoulos G, Viniou N, Plata E, Konstantopoulos K, Andreopoulos A, Rombos Y, et al. Development of plasma cell tumors during treatment of multiple myeloma. Ann Hematol 1996;72:317-20. [DOI] [PubMed]
- 3.Datta RV, Daskalakis T, Adler H, Lehman H. Unusual presentations of uncommon tumors: case 3. Giant cell plasmacytoma presenting as an intraperitoneal mass. J Clin Oncol 2002;20:2405-6. [DOI] [PubMed]
- 4.Galieni P, Cavo M, Avvisati G, Pulsoni A, Falbo R, Bonelli MA, et al. Solitary plasmacytoma of bone and extramedullary plasmacytoma: two different entities? Ann Oncol 1995;6:687-91. [DOI] [PubMed]
- 5.Griffiths AP, Shepherd NA, Beddall A, Williams JG. Gastrointestinal tumour masses due to multiple myeloma: a pathological mimic of malignant lymphoma. Histopathology 1997;31:318-23. [DOI] [PubMed]


