Abstract
Medical errors represent a serious public health problem and pose a threat to patient safety. As health care institutions establish “error” as a clinical and research priority, the answer to perhaps the most fundamental question remains elusive: What is a medical error? To reduce medical error, accurate measurements of its incidence, based on clear and consistent definitions, are essential prerequisites for effective action. Despite a growing body of literature and research on error in medicine, few studies have defined or measured “medical error” directly. Instead, researchers have adopted surrogate measures of error that largely depend on adverse patient outcomes or injury (i.e., are outcome-dependent). A lack of standardized nomenclature and the use of multiple and overlapping definitions of medical error have hindered data synthesis, analysis, collaborative work and evaluation of the impact of changes in health care delivery. The primary objective of this review is to highlight the need for a clear, comprehensive and universally accepted definition of medical error that explicitly includes the key domains of error causation and captures the faulty processes that cause errors, irrespective of outcome.
Abstract
Les erreurs médicales constituent un grave problème de santé publique et menacent la sécurité des patients. Alors même que les établissements de santé accordent la priorité dans les interventions cliniques et en recherche à l'«erreur», la réponse à la question peut-être la plus fondamentale nous échappe toujours : qu'est-ce qu'une erreur médicale? Afin de réduire les erreurs médicales et d'intervenir efficacement, il est essentiel de commencer par en mesurer précisément les incidences en fonction de définitions claires et uniformes. En dépit d'une masse croissante de documents et de recherches sur l'erreur en médecine, peu d'études ont défini «l'erreur médicale» ou l'ont mesurée directement. Les chercheurs ont plutôt adopté des substituts de mesures de l'erreur qui reposent en grande partie sur les résultats indésirables pour les patients ou les traumatismes (c.-à-d. liés aux résultats). Le manque de nomenclature normalisée et les multiples définitions de l'erreur médicale qui se chevauchent ont nui à la synthèse des données, à l'analyse, à la collaboration et à l'évaluation de l'incidence du changement sur la prestation des soins de santé. Cette étude vise principalement à mettre en évidence le besoin d'une définition claire, complète et universelle de l'erreur médicale incluant explicitement les domaines clés des causes d'erreur et saisissant les processus défectueux à l'origine des erreurs, sans égard aux résultats.
The issue of patient safety plays a prominent role in health care. Its prominence is fueled by an expanding body of literature that shows a high incidence of error in medicine,1,2,3,4,5 coupled with well-publicized medical error cases that have raised public concern about the safety of modern health care delivery.6
As empirical literature on medical error expands, medicine's vulnerability to error is becoming apparent. Medical errors are a leading cause of death in North America;7 between 44 000 and 98 000 patients are estimated to die each year in the USA as a result of medical errors.7 Using conservative estimates, deaths due to medical errors exceed the number attributable to the 8th leading cause of death in North America.8 Medical errors are estimated to cost between US$17-billion and US$29-billion per year in lost income, lost household production, disability and additional health care costs.9
To reduce the incidence of errors, health care providers must identify their causes, devise solutions and measure the success of improvement efforts. Moreover, accurate measurements of the incidence of error, based on clear and consistent definitions, are essential prerequisites for effective action. Unfortunately and understandably, what is considered a medical error (if the term is used at all) has been influenced by differing contexts and purposes, such as research, quality control, ethics, insurance, legislation, legal action and statutory regulation.1,3,5,10 As a result, a lack of standardized nomenclature and the use of multiple and overlapping definitions of medical error has hindered data synthesis and analysis, collaboration and evaluation of the impact of changes on health care delivery.11,12,13,14,15 Furthermore, few published studies have measured medical error directly.16,17 Instead, researchers have adopted surrogate measures of error such as noxious episodes,18 iatrogenic illness,19 critical incidents,20 potentially compensatable events,10 negligence,1 preventable adverse events,3 slips,21 mistakes21 and violations.14 Recognizing the limitations in defining medical error, leading medical error commentators Eric Thomas and Troyen Brennan22 have warned “Reader, beware” when making comparisons of error rates in the published literature.
As health care institutions establish error as a research priority, the answer to perhaps the most fundamental question remains elusive: What is a medical error? A theme that resonates throughout the current research literature is the need for a clear, comprehensive and universally accepted definition.11,16,17,21,23,24
Objectives
The objective of this paper is to highlight the need for a clear, comprehensive and universally accepted definition of medical error and propose a definition that fulfills those needs. As part of this proposition, we will review critically how the term medical error has been defined in the literature published over the past half-century; describe how other safety-critical industries define the term error; consider the impact of the term error on the psyche of health care professionals; and propose a new definition of medical error and justify its use in clinical practice and research.
Outcome- versus process-dependent definitions
Historically, patient safety researchers investigating the impact of error in medicine have adopted outcome-dependant definitions of medical error and its surrogate terms, and have limited their focus to patients experiencing adverse outcomes or injury as a consequence of medical care.1,2,3,4,5 Perhaps this tendency stems from a guiding principle of medical practice credited to Hippocrates, prium no nocere, which translates to “First, do no harm.”21,25,26 Moreover, the manner in which patient safety has been defined promotes an outcome-dependant approach to defining medical error.
Patient safety: the avoidance, prevention and amelioration of adverse outcomes or injuries stemming from the process of health care (US National Patient Safety Foundation, 1999).27 Freedom from accidental injury (Institute of Medicine, 2000).11
In the earliest studies on patient safety in the 1950s, medical errors were largely considered “diseases of medical progress”28 and dismissed as “the price we pay for modern diagnosis and therapy.”29 These reports tended to be limited to unusual patient reactions or those of magnitude and consequence.28,29
In “Hazards of hospitalization,” a pioneering investigation on error in medicine, Schimmel18 maintained that “assessment of all untoward reactions, regardless of severity, is essential to determine their total incidence and to indicate the cumulative risk assumed by the patient exposed to the many drugs and procedures used in his care.” With this imperative, he adopted the term noxious episode as a surrogate term for medical error, and studied prospectively the type and frequency of such episodes in patients admitted to a university medical service.
Noxious episode: all untoward events, complications, and mishaps that resulted from acceptable diagnostic or therapeutic measures deliberately instituted in the hospital (Schimmel, 1964).18
Reflecting the growing presence in the 1970s of third-party insurance companies in the economics of health care, The California Medical Insurance Feasibility Study10 adopted the term potentially compensatable event to reflect errors that could potentially lead to malpractice claims.
Potentially compensatable event: an event due to medical management that resulted in disability, which led to or prolonged a hospitalization (The California Medical Insurance Feasibility Study, 1977).10
In the 1990s, the publication of the 3 most extensive investigations on medical error — the Harvard Medical Practice Study,1,2 the Quality in Australian Health Study,3,4 and the Utah and Colorado Medical Practice Study5 — gave prominence to the term adverse event.
Adverse event: unintended injury to patients caused by medical management (rather than the underlying condition of the patient) that results in measurable disability, prolonged hospitalization or both (the Harvard Medical Practice Study,1,2 1991, and the Utah and Colorado Medical Practice Study,5 1999). Unintended injury or complication that results in disability, death, or prolonged hospital stay and is caused (including acts of omission and acts of commission) by health care management rather than the patients disease (Quality in Australian Health Study, 1995).3,4
Although adverse events typically result from medical intervention, not all adverse patient outcomes are the result of error. Reflecting this fact, many investigators suggest that only preventable adverse events be attributed to medical error.1,3,11,21,30 Patient-safety experts have considered an adverse event to be preventable when
…there is a failure to follow accepted practice (the current level of expected performance for the average practitioner or system that manages the condition in question) at an individual or system level (Quality in Australian Health Study, 1995);3 …it is widely established that a high incidence of this type of complication reflects low standards of care or technical expertise (Lucian Leape, 1994).21
The relationship between negligence and preventable adverse events was characterized in the publications of the Harvard1,2 and Utah and Colorado Medical Practice studies.5 Reduction of malpractice claims and litigation against health care providers were established as primary objectives in both of these investigations. Negligent adverse events represent a subset of preventable adverse events that satisfy the legal criteria used in determining negligence.
Negligence: failure to meet the standard of care reasonably expected of an average physician qualified to take care of the patient in question (Brennan et al, 1991).1 Care that fell below the standard expected of physicians in their community (Thomas et al, 1995).5
Negligent adverse event: injury caused by substandard medical management (Leape, 1991).2
Adverse patient outcomes represent a limited subset of medical errors. The vast majority of errors do not result in injury to patients because the error was identified in time and mitigated; because the patient was resilient; or because of simple good luck.11,14 James Reason's “Swiss cheese” model of error causation31 illustrates how this notion applies to health care (Fig. 1). According to Reason, most complex systems and work environments (such as hospitals) have several layers of defence that offer protection against the adverse consequences of error (signified by several slices of Swiss cheese). In spite of such safeguards, several holes or flaws exist within each individual layer of defence (the holes in each individual slice). Injury to patients occurs only when circumstances arise that cause the flaws in each individual layer of protection (or holes in the cheese slices) to align in a way that allows an error to penetrate their defences and reach the patient.31
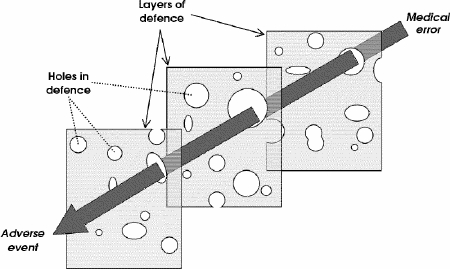
FIG. 1. James Reason's “Swiss cheese” model of error causation. In complex organizations (hospitals, clinics, biomedical institutes), medical errors cause adverse patient outcomes only when they penetrate through the holes or flaws in the multiple layers of defence (slices of Swiss cheese).
Outcome-dependant definitions of medical error have provided valuable insight into the costs, morbidity and magnitude of harm resulting from such events. Nonetheless, quality improvement initiatives require understanding of the processes that lead to such errors.22 Building a safer health care system will depend on our success at designing processes of care that ensure patients are protected from the threat of injury.11,12,13,16,21,24,32 Therefore, a definition of medical error should capture process or system failures that cause errors, irrespective of outcome (a process-dependant approach). Ideally, process-dependant definitions of medical error should capture the full spectrum of medical errors, namely, errors that result in adverse patient outcomes as well as those that expose patients to risk but do not result in injury or harm.11,16,33,34 Errors that do not result in injury are often referred to as near misses, close calls, potential adverse events or warning events.34
Near miss: any event that could have had an adverse patient consequence but did not, and was indistinguishable from a full-fledged adverse event in all but outcome ( Barach and Small, 2000).34
Given that many of the factors that lead to both near misses and adverse events are identical, identification and analysis of the processes that potentially can (near misses) and actually do (adverse events) lead to adverse patient outcomes is critical.11,16,34 Examples of process- dependant definitions of medical error in the published literature include
Medical error: the failure of a planned action to be completed as intended (an error of execution) or the use of a wrong plan to achieve an aim (an error of planning) (Reason, 1990).35 An unintended act (either of omission or commission) or one that does not achieve its intended outcome (Leape, 1994).21 Deviations from the process of care, which may or may not cause harm to the patient (Reason, 2001).14
Reason's definition35 distinguishes between errors of execution and errors in planning, acknowledging that mental/judgmental and physical / technical failures both contribute to errors. However, his definition neglects errors of omission: What if there was no plan, or no action? Leape's definition recognizes that both actions (acts of commission) and inaction (acts of omission) contribute to medical errors,21 but omits intended acts that are based on wrong plans except for when the actions based on those plans lead to unintended outcomes.
Reason's and Leape's definitions have further limitations. Although action plans may not “be completed as intended” or “achieve their intended outcomes,” errors do not necessarily account for all of those failures. Often, circumstances beyond the physician's control influence patient outcomes. For example, consider a patient with no known history of allergies who experiences an allergic drug reaction upon starting a new medication. The outcome is unintended, yet not convincingly attributable to medical error. To suggest that all unintended outcomes can be attributed to medical error is not justifiable.
Reason's definition14 is appropriately both process-dependant and outcome-independent. Unfortunately, it is in our opinion too general, by simply referring to “the process of care” rather than stating those processes explicitly.
How do other safety-critical industries define error?
Medicine is beginning to benefit from interdisciplinary and collaborative efforts between specialists in health care and other high-reliability and safety-critical industries with a long history of recording and analyzing errors.11,14,36 Such experiences reveal that the distinction between process and outcome-dependant approaches to defining error is not unique to medicine.
The aviation industry uses terms like incidents and accidents as substitutes for medicine's near misses and adverse events, respectively.
Incident: an occurrence other than an accident associated with the operation of an aircraft, which affects or could affect the safety of operations (Federal Aviation Regulations, 2001).37
Accident: an occurrence associated with the operation of an aircraft…in which any person suffers death or serious injury or in which the aircraft receives substantial damage (Federal Aviation Regulations, 2001).37
The nuclear power industry has adopted a more inclusive (process- and outcome-dependant) definition of accident that accounts for both the actual and potential consequences of the event.
Accident: any unintended event, including operating error, equipment failures or other mishaps, the consequences or potential consequences of which are not negligible from the point of view of protection or safety (the International Atomic Energy Agency, 2000).38
Should the term error be used at all, in medicine?
With growing public concern over the impact of medical errors on patient populations, we must not ignore the profound psychological effect that errors can have on the health care professionals who make them.11,39 The term error carries with it a stigma that can evoke feelings of guilt, anger, inadequacy and depression.14 The threat of legal action compounds such feelings. Some authors have maintained that the term error is excessively negative and antagonistic, and perpetuates a culture of blame.23,24,33 A physician or nurse whose confidence and morale has been shattered as a result of an error may work less effectively and efficiently, and may even consider abandoning a career in medicine.14 This raises an important question: Should the term error be used at all?
We acknowledge that it may be prudent to limit the use of the term error when seeking causes in specific, identifiable cases or patient populations, especially if the documentation may become public record. However, apprehension over the use of the term error should not lead to its complete removal from work to improve patient safety and redesign health care systems. Adverse patient outcomes do occur because of errors; to delete the term error from discussion of such outcomes obscures the goal of preventing and managing its causes and effects. Human-factor scientists have acknowledged the importance of recognizing error (with appropriate, timely feedback) as a powerful tool for learning, shaping behaviour, and achieving goals.11,14,40,41
Reason35 has pointed out that commonly, errors occur from the convergence of multiple and complex contributing factors.36 Public and legislative intolerance for medical errors illustrate a lack of understanding of Reason's observations of complex human systems. The human factor will always be a problem, and acknowledging such factors does permit improvement strategies to be undertaken that promote both system changes and education. However, blaming or punishing individuals for errors related to underlying systemic causes will not change or address those causes, nor prevent repetition of the errors.
For this reason, patient-safety experts are focusing not on the perpetrators of individual errors or getting rid of “bad apples,” but on building safer health care systems to reduce the probability of errors and mitigate their effects on patients, employees and society when they do occur.11,35,36,42 Errors represent opportunities for education and constructive changes in health care delivery. Ultimately, we may regard them as “beacons of safety.”24
An outcome- and process-dependent definition of medical error
We propose the following definition:
Medical error: an act of omission or commission in planning or execution that contributes or could contribute to an unintended result.
This definition of medical error includes explicitly the key domains of error causation (omission and commission, planning and execution), and captures faulty processes that can and do lead to errors, whether adverse outcomes occur or not. The inclusivity and explicitness of the definition should make it useful for research into the etiology of errors from the perspective of the provider: given this definition, a health care worker has a clear roadmap with which to designate a process as error-prone or error-laden. By including potential adverse outcomes, the definition includes the “silent majority” of errors that do not cause harm but reflect faulty processes. At the same time, it ignores trivial mistakes (for example, taking the wrong route to visit a patient) that have no potential for adverse outcome.
To stimulate collaborative efforts and facilitate data collection, synthesis and analysis, we have defined medical error explicitly and directly, avoiding the use of surrogate terms. We believe that this will help focus error measurement for research, quality control and legislative purposes, but allow the use of surrogate terms for regulatory, legal and insurance purposes.
Medical, legal and governmental institutions must work collaboratively to break down the culture of blame while retaining methods for accountability. When this challenge has been met, health care institutions will not be constrained from measuring the most useful target for process improvement: all errors, whether or not they lead to adverse outcomes. When that happens, health care can join the ranks of similar high-reliability and safety-conscious industries such as aviation.
Conclusions
Medical errors represent an important public health problem and pose a serious threat to patient safety. The growing awareness of the frequency, causes and consequences of error in medicine reinforces an imperative to improve our understanding of the problem and to devise workable solutions and prevention strategies. Variations in nomenclature without a universally accepted definition of medical error hinder data collection and collaborative work to improve health care systems. If health care providers and researchers are to improve patient safety, we must all speak the same language. The definition of medical error we have proposed explicitly addresses the key domains of error causation and includes process faults that have the potential for, but do not necessarily lead to, adverse patient outcomes.
Competing interests: None declared.
Correspondence to: Dr. John M. A. Bohnen, Department of Surgery, University of Toronto, 100 College St., Toronto ON M5G 1L5; fax 416 978-3928; bohnenj@smh.toronto.on.ca
Accepted for publication Jan. 26, 2004
References
- 1.Brennan TA, Leape LL, Laird NM, Hebert L, Localio AR, Lawthers AG, et al. Incidence of adverse events and negligence in hospitalized patients: results of the Harvard Medical Practice Study I. N Engl J Med 1991;324:370-6. [DOI] [PubMed]
- 2.Leape LL, Brennan TA, Laird N, Lawthers AG, Localio AR, Barnes BA, et al. The nature of adverse events in hospitalized patients: results of the Harvard Medical Practice Study II. N Engl J Med 1991;324:377-84. [DOI] [PubMed]
- 3.Wilson RM, Runciman WB, Gibberd RW, Harrison BT, Newby L, Hamilton JD. The Quality in Australian Health Care Study. Med J Aust 1995;163:458-71. [DOI] [PubMed]
- 4.Wilson RM, Harrison GB, Gibberd RW, Hamilton JD. An analysis of the causes of adverse events from the Quality in Australian Health Care Study. Med J Aust 1999;170:411-5. [DOI] [PubMed]
- 5.Thomas EJ, Studdert DM, Burstin HR, Orav EJ, Zeena T, Williams EJ, et al. Incidence and types of adverse events and negligent care in Utah and Colorado. Medical Care 1999;38(3):261-71. [DOI] [PubMed]
- 6.Cook R, Woods D, Miller C. A tale of two stories: contrasting views of patient safety. Chicago: National Patient Safety Foundation; 1998.
- 7.American Hospital Association. Hospital statistics. Chicago: the Association; 1999.
- 8.Center for Disease Control and Prevention (National Center for Health Statistics). Deaths: final data for 1997. National Vital Statistics Reports. 1999;47(19):27. [PubMed]
- 9.Thomas EJ, Studdert DM, Newhouse JP, Zbar BI, Howard KM, Williams EJ, et al. Costs of medical injuries in Utah and Colorado. Inquiry 1999;36:255-64. [PubMed]
- 10.Mills DH, Boyden JS, Rubamen DS. Report on The Medical Insurance Feasibility Study. San Francisco (CA): Sutter Publications; 1977.
- 11.Kohn LT, Corrigan JM, Donaldson MS. To err is human: building a safer health system. Washington: National Academy Press; 2000. [PubMed]
- 12.Hebert PC, Levin AV, Robertson G. Bioethics for clinicians 23: disclosure of medical error. CMAJ 2001;164(4):509-13. [PMC free article] [PubMed]
- 13.Hatch D. Incidence and acceptance of errors in medicine. Schweiz Arzte, Bull Med Swiss 2001; 82: 1339-43.
- 14.Reason JT. Understanding adverse events: the human factor. In: Vincent C, editor. Clinical risk management: enhancing patient safety. London: BMJ Publishing Group; 2001. p. 9-30.
- 15.Senders JW. Medical devices, medical errors and medical accidents. In: Bogner MS, editor. Human error in medicine. Hillsdale (NJ): Lawrence Erlbaum Associates; 1994.
- 16.Senders JW. On errors, incidents and accidents. Human Factors Science. Available: www.visualexpert.com/Resources/roadaccidents.html (accessed 2005 Jan 14).
- 17.Hofer TP, Hayward RA. What is an error? Eff Clin Pract 2000;3(6):261-9. [PubMed]
- 18.Schimmel EM. The hazards of hospitalization. Ann Intern Med 1964;60:100-9. [DOI] [PubMed]
- 19.Steel K, Gertman PM, Crescenzi C, Anderson J. Iatrogenic illness on a general medical service at a university hospital. N Engl J Med 1981;304:638-42. [DOI] [PubMed]
- 20.Cooper JB, Newbower RS, Long CD, McPeek B. Preventable anesthesia mishaps: a study of human factors. Anesthesiology 1978;49:399-406. [DOI] [PubMed]
- 21.Leape L. Error in medicine. JAMA 1994; 272:1851-7. [PubMed]
- 22.Thomas EJ, Brennan TA. Errors and adverse events in medicine: an overview. In: Vincent C, editor. Clinical risk management: enhancing patient safety. London: BMJ Publishing Group; 2001. p. 31-43.
- 23.Wears RL, Janiak B, Moorehead JC, Kellermann AL, Yeh CS, Rice MM, et al. Human error in medicine: promise and pitfalls, part 2. Ann Emerg Med 2000;36(2):142-4. [DOI] [PubMed]
- 24.Fish JM. Human error in medicine: promise and pitfalls, part 2 [letter]. Ann Emerg Med 2001;37(4):419-20. [DOI] [PubMed]
- 25.Veatch RM. Cross cultural perspectives in medical ethics readings. Boston: Jones and Bartlett Publishers; 1989.
- 26.Nightingale F. Notes on hospitals. London: Longman; 1863.
- 27.National Patient Safety Foundation. Agenda for research and development in patient safety. Available: www.npsf.org (accessed 2005 Jan 14). [PubMed]
- 28.Moser RH. Diseases of medical progress. N Engl J Med 1956;255:606-14. [DOI] [PubMed]
- 29.Barr DP. Hazards of modern diagnosis and therapy: the price we pay. JAMA 1955;159:1452-6. [PubMed]
- 30.Nora PF. Improving safety for surgical patients: suggested strategies. Bull Am Coll Surg 2000;85(9):11-4. [PubMed]
- 31.Reason J. Managing the risks of organizational accidents. Aldershot: Ashgate; 1997.
- 32.Liang BA, Storti K. Creating problems as part of the “solution”: the JCAHO Sentinel Event Policy, legal issues, and patient safety. J Health Law 2000;33(2):263-85. [PubMed]
- 33.Holloway RG, Panzer RJ. Lawyers, litigation, and liability: Can they make patients safer? Neurology 2001;56(8):24-5. [DOI] [PubMed]
- 34.Barach P, Small SD. Reporting and preventing medical mishaps: lessons form non-medical near miss reporting. BMJ 2000;320:759-63. [DOI] [PMC free article] [PubMed]
- 35.Reason J. Human error. Cambridge: Cambridge University Press; 1990.
- 36.Cook RI, Woods DD. Operating at the sharp end: the complexity of human error. In: Bogner MS, editor. Human errors in medicine. Hillsdale (NJ): Erlbaum; 1994. p. 255-310.
- 37.Federal Aviation Administration. Aviation glossary, Federal Aviation Regulations. In: Aviation safety data [Web page]. Washington: FAA. Available: www.asy.faa.gov/internet/fw_learn.htm (accessed 2005 Jan 27).
- 38.NUSAFE Nuclear Installation Safety Net. IAEA safety glossary. In: Regulatory control of nuclear power plants, 1st ed. 2002. Vienna (Austria): International Atomic Energy Agency. 2002. Available: www-ns.iaea.org/tutorials/regcontrol/intro/glossarya.htm (accessed 2005 Jan 27).
- 39.Kaufmann M. Medical error: the human perspective. Ont Med Rev 2002:50-1.
- 40.Weinger MB, Paniskas C, Wilklund M, Carstensen P. Incorporating human factors into the design of medical devices. JAMA 1998;280(17):1484. [DOI] [PubMed]
- 41.Andrews LB, Stocking C, Krizek T, Gottlieb L, Krizek C, Vargish T, et al. An alternative strategy for studying adverse events in medical care. Lancet 1997;349(9048):309-13. [DOI] [PubMed]
- 42.Deming WE. Elementary principles of the statistical control of quality: a series of lectures. Tokyo: Nippon Kagaku Gijutsu Remmei; 1952.


