On Mar. 12, 2003, the World Health Organization issued a global health alert for severe acute respiratory syndrome (SARS), a new illness that originated in Guangdong Province, China. It is known to be caused by a coronavirus. Its spread to Toronto, Canada, occurred in late February 2003. The spectrum of illness ranges from fever, muscle aches and mild respiratory symptoms to severe respiratory distress requiring mechanical ventilation.
The SARS epidemic introduced essential infection control considerations. SARS' respiratory-droplet route of transmission and the organism's potential to remain infectious on surfaces for long periods mandate extraordinary precautions. For this reason, the Centers for Disease Control and Prevention (CDC) have published recommendations for the personal protective equipment (PPE) appropriate as precautions, both standard and against contact and airborne infection.1 These recommendations included the use of caps, goggles, N95 masks, gowns and gloves (Fig. 1), hereinafter referred to as standard PPE.
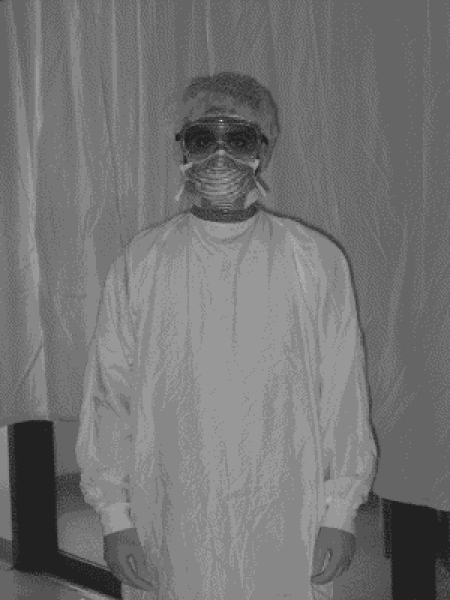
FIG. 1. Standard personal protective equipment: cap, goggles, N95 mask, gown and gloves.
We found only 2 reports in the literature on the conduct of operations upon patients known to have SARS, which describe 1 emergency and 3 elective tracheostomies.2,3 The staff involved used essentially the standard PPE recommended by the CDC; 2 weeks after the operations, they remained healthy.
In our institution 9 health care workers, after being involved with a difficult airway situation in a patient with SARS, were infected despite wearing standard PPE.4 As a result, the Ontario Ministry of Health and Long-Term Care published a directive mandating the use of additional personal protection for high-risk airway management situations.5 In our institution, additional protection consisted of wearing the Stryker T4 Personal Protection System® (hereafter referred to as T4 PPS), consisting of a helmet, a short hood with visor and a long toga-style gown (Fig. 2), over standard PPE. In this report, we describe the effect of our use of these additional precautions on the conduct of 3 elective tracheostomies and 1 emergency laparotomy on 3 patients with SARS.

FIG. 2. The Stryker T4 Personal Protection System, which is worn over standard personal protective equipment.
Cases 1–3: elective tracheostomies
From May 2 to May 9, 2003, we performed elective open bedside tracheostomies on 3 patients with SARS (2 men and 1 woman) in the intensive care unit (ICU) of our facility. All patients were considered to have probable SARS, on the basis of clinical criteria (all 3 had fever >38°C, dry cough and dyspnea, and 2 of 3 complained of myalgias) as well as epidemiological criteria (all 3 patients had, within 10 days of the onset of their illness, been in close contact with people with SARS). At the time of tracheostomy, patients were (medians) 58 years of age, had required 25 days of mechanical ventilation and exhibited a PaO2/ FIO2 ratio of 121. In all cases, chest radiographs showed bilateral infiltrates consistent with acute respiratory distress syndrome (ARDS). These clinical criteria correspond with the CDC's preliminary clinical description of SARS.6
Indications, setting and staff
In all 3 cases, tracheostomy was performed for respiratory failure and the need for prolonged endotracheal intubation. Each operation took place in the ICU, in a negative-pressure room isolated from the remainder of the unit. We chose to perform the tracheostomies in the ICU to avoid unnecessary transportation of the patients. In each case, the operating surgeon was the senior attending trauma surgeon of the hospital, and the surgical assistant was the most senior surgical staff member available (second attending surgeon, trauma surgery fellow or surgery resident). The attending ICU staff member is an anesthetist by training. There was no circulating nurse or scrub nurse in the room during any of the 3 procedures.
Surgical considerations
The surgeon and assistant wore standard PPE to prepare the room, which included moving in a portable operating light, the electrocautery machine, and all the standard instrument trays and operating equipment. The trays were opened and the tracheostomy tube, sutures and instruments laid out for easy access. The patient was then prepared and draped for surgery.
The surgeon and assistant then exited the room to don the additional protective gear. Each person on the operating team wore standard PPE, and then put on the T4 PPS. It was critical to defog personal eyeglasses and goggles before wearing the extensive gear required.
We performed a standard open tracheostomy procedure through a transverse neck incision, disregarding the percutaneous technique because of the additional risk associated with bronchoscopy in a ventilated or spontaneously breathing patient who has SARS. Diathermy was avoided when possible, for fear of aerosolizing viral particles. To further prevent respiratory-droplet contamination of the room, the procedure was carried out with the patient fully paralyzed. All mechanical ventilation was stopped from the time the tracheotomy was made until the tube placement was confirmed by capnography, the cuff inflated and the tracheostomy tube reconnected to the anesthetic circuit. We did not use suction after the trachea was opened. Ideally, suction should be performed with a closed system, and a viral filter should be used.
Anesthetic considerations
Like the surgical team, the anesthetist and the respiratory therapist initially moved all required equipment into the room while wearing standard PPE. One special consideration was using disposable equipment whenever possible. A disposable colorimetric in-line capnograph was used to avoid potential hardware damage from Virox decontamination (Virox Technologies Inc., Oakville, Ont.). The anesthetist then pre-oxygenated the patient before exiting the room with the respiratory therapist to don the T4 PPS.
Total intravenous anesthesia was used because an agent vaporizer was not available for the Puritan Bennett 840 ventilator at our institution. After checking the patient for responsiveness, the anesthetist administered rocuronium to attain neuromuscular paralysis. Supplemental rocuronium (0.1 mg/kg) was given every 10 minutes to maintain deep neuromuscular paralysis. Again to avoid potential hardware damage by Virox decontamination, a peripheral nerve stimulator was not used; close observation for signs of diaphragmatic activity was therefore required, especially at the time of tracheotomy. In 1 patient, a supplemental dose of rocuronium was given at this moment to prevent coughing, which otherwise might have exposed the team to droplet contamination.
Infection control and prevention
As described, over standard PPE we wore the Stryker T4 PPS: a helmet, a short hood with visor and a long toga-style gown. The T4 PPS provides a complete barrier from the patient's respiratory droplets. The helmet is connected to a rechargeable power pack, which is worn under the gown and clipped to a belt. The power pack powers a hose that circulates air in the hood.
Donning and removing suits
Toronto-area hospitals have established protocols for donning and removing the Stryker T4 protective gear.7 Most important is de-gowning, since it requires a strict procedure to protect the operator from becoming contaminated. It is critical to have an assistant who is familiar with the T4 PPS to help guide people through the steps of gowning and de-gowning.
Six months after the procedure, all staff involved in the 3 tracheostomies remained healthy.
Case 4: emergency laparotomy
A 54-year-old man with SARS was admitted on April 8, 2003. He required prolonged ventilation; an elective tracheostomy was performed in May. Two months later, he required percutaneous drainage of his gallbladder for acalculous cholecystitis. Although this was successful, shortly after he became septic. After an appropriate work-up, he was sent for a cholangiogram and for manipulation of his cholecystostomy tube. After returning from cholangiography, he unfortunately became hemodynamically unstable and developed abdominal distension. An emergency bedside abdominal ultrasound showed free fluid in his peritoneal cavity.
He was transferred for an emergency laparotomy to a negative-pressure operating room. He had approximately 5 L of blood in his peritoneal cavity. After the blood was suctioned out, it became evident that the gallbladder was necrotic, and that the bleeding was from the inferior surface of the liver, adjacent to the gallbladder. A rapid cholecystectomy was done in a retrograde fashion, but because of severe inflammation, the cystic artery and duct were never identified. Bleeding from the liver and gallbladder bed was eventually controlled with the Argon beam coagulator (Tyco Healthcare, Valleylab, Pointe Claire, Que.). The incision was then closed and the patient brought back to the ICU.
The patient unfortunately became increasingly unstable over the course of the night. Despite a reopening in the ICU of his abdomen for potential abdominal compartment syndrome, the patient died. The staff, who during this final procedure had worn standard PPE only, remained healthy as of 6 months afterward.
Infection control and staff morale
This patient had already had a tracheostomy. Theoretically, an emergency laparotomy for intraperitoneal bleeding should not be a high-risk procedure for SARS transmission; even so, the operating surgeons, anesthetist and scrub nurse all insisted upon wearing the T4 PPS. This helped reduce the level of emotional stress in the operating staff.
Wearing the T4 PPS, however, imposed certain other difficulties that not been obvious during the tracheostomies. Despite the power pack and circulating air, the length of the laparotomy procedure caused people in the suits to become quite hot. Furthermore, peripheral vision and hearing was limited, and mobility restricted. With the headgear on, the surgeon and assistant often got in each other's way while operating deep in the abdomen.
Logistical issues
Our institution has purchased numerous T4 PPS systems and placed them strategically in high-risk environments. The emergency department and intensive care units were all equipped with these units, and select personnel have been trained in their use.
At the time of this patient's laparotomy our operating room was unequipped with these units. A considerable delay totalling 2 hours resulted while hospital operations personnel were contacted to temporarily reallocate these resources to the operating room.
Another delay occurred to find a knowledgeable assistant available to help the operating room staff with gowning and de-gowning. A negative-pressure operating room was required; this required additional time to set up. The patient was transferred from the ICU to the operating room by means of a back hallway that is less travelled. Finally, the entire gowning and de-gowning procedure imposed a third delay, in this emergency situation.
Such time delays in the face of emergency surgery may have negative implications for patient outcomes.
Discussion
This is the third report in the literature describing tracheostomies in people with SARS, and the first to describe an emergency laparotomy. When Wei and colleagues2 published their own experience with 1 emergency and 2 elective tracheostomies in patients with SARS, they recommended that all involved medical personnel use standard PPE during these procedures. On the other hand, when Kwan and colleagues3 performed a tracheostomy on a patient with SARS, they did so while wearing additional protection: Tyvek BarrierMan (Dupont; distributed by PDS International Pte Ltd., Hong Kong).
After 9 health care workers who took standard precautions were infected with SARS at our institution during a difficult airway situation, we opted to use additional protection during airway procedures on patients with SARS. There is no literature, however, that suggests that the T4 PPS offers better protection against SARS transmission than standard PPE. Investigation of this particular episode suggests that case-specific features may have compounded the risk of infectivity. The use of BiPap and high-frequency oscillatory ventilation, the lack of adequate sedation (with subsequent agitation and coughing), and a repeated requirement to clean copious secretions from obstructed ventilator tubing all may explain the transmission of infection despite standard PPE.
Evidence-based guidelines are needed to describe the levels of precautions required for different procedures involving patients with SARS. One potential approach is to stratify the risk of infection in each individual patient by monitoring viral load and IgG seroconversion. Peiris and associates8 documented a decrease in rates of viral shedding from the nasopharynx, stool and urine from day 10 to 21 after the onset of SARS symptoms in a cohort of patients. These authors noted that seroconversion of SARS-associated coronavirus IgG, which starts on day 10, seems to correlate with the fall in viral load. Potentially, then, the level of precautions could be determined for each individual patient by monitoring clinical parameters, viral loads and levels of anti-SARS–associated coronavirus IgG.
In the absence of prospectively validated guidelines, using T4 PPS for elective airway surgery is reasonable, with preplanning and coordination. Ideally the entire operation, from set-up of equipment to the exit of the operating team, would be fully rehearsed by the team before donning the T4 PPS. All of these measures can mitigate the disadvantages of using the T4 PPS, which include reduced vision and mobility, and increased risk of contamination during de-gowning. Even so, there is no evidence to support that T4 PPS offers any better protection than standard PPE in these situations.
Using T4 PPS to conduct emergency airway procedures is controversial. On the one hand, the spread of SARS to 9 workers at our institution despite their use of standard precautions argues in favour of using additional staff protection in emergency airway procedures. However, specific features of that episode may have been such that T4 PPS would also have failed to protect the workers involved. Certainly, the best approach is to emphasize safe airway management techniques9 in patients with SARS, and to avoid high-risk emergency situations. In the event of an emergency tracheostomy, however, we would adopt the “protected code blue” protocol advocated by Mazurik and coworkers.10 In this protocol, high-flow oxygen therapy (with no ventilation) would be initiated by staff wearing standard PPE while the resuscitation / surgical team dons the T4 PPS. The tracheostomy would then be conducted only after the team is wearing the full T4 PPS outfit.
Using the T4 PPS during emergency procedures not involving the airway can adversely affect patient outcomes. Unless sufficient units are allocated to the operating suites and until operating teams are completely familiar with how to don and remove the garments, immoderate delays can result from using T4 PPS, with no established protective benefit. Furthermore, the problems of decreased mobility, hearing and vision and increased discomfort to the wearer may impede operator performance during the conduct of challenging emergency cases.
If the T4 PPS is to be used in emergency circumstances, essential contingency planning, coordination and training should be implemented well in advance. Use of the T4 PPS should not impose so long a logistical delay on the conduct of an emergency procedure that patient outcomes are affected.
In the absence of guidelines, some staff may accept the logistical delays brought on by wearing the additional personal protection offered by the T4 PPS or any similar system. These additional protective measures can reduce some of the stress involved in operating on people with SARS. Maintaining a dialogue with the operating room staff about appropriate levels of personal protection for SARS cases would help to reduce some of this stress. Established credible guidelines would reduce that stress even further, because staff would be better able to quantify the risk to themselves.
Conclusions
Operating while wearing the Stryker T4 PPS requires significant preplanning and coordination of all involved staff, to avoid logistical delays and staff contamination during PPS removal. In the absence of credible evidence-based guidelines, we think additional personal protection is warranted in elective and emergency airway operations, but also that the benefit of these additional precautions is likely offset by their disadvantages during emergency operations not involving the airway. The logistical delays imposed by finding and donning these garments during off-hours, and the restrictions to movement and the vision of the operating staff, could combine to adversely affect outcomes in challenging emergency cases.
Competing interests: None declared.
Correspondence to: Dr. Fred Brenneman, Sunnybrook and Women's College Health Sciences Centre, Ste. H-170, 2075 Bayview Ave., Toronto ON M4N 3M5; fax 416 480-4225; fred.brenneman@sw.ca
Accepted for publication Mar. 24, 2004
References
- 1.Centers for Disease Control and Prevention (CDC). Interim domestic guidance on the use of respirators to prevent transmission of SARS. Atlanta (GA): CDC; 2003. Available: www.cdc.gov/ncidod/sars/pdf/respirators-sars.pdf (accessed 2004 Nov 8).
- 2.Wei W, Tuen H, Ng R, Lam L. Safe tracheostomy for patients with severe acute respiratory syndrome. Laryngoscope 2003;113:1777-9. [DOI] [PMC free article] [PubMed]
- 3.Kwan A, Fok WG, Law KI, Lam SH. Tracheostomy in a patient with severe acute respiratory syndrome. Br J Anesth 2004;92(2):280-2. [DOI] [PMC free article] [PubMed]
- 4.Ofner M, Lem M, Sarwal S, Vearncombe M, Simor A. Cluster of severe acute respiratory syndrome cases among protected health care workers — Toronto, April 2003. Can Commun Dis Rep 2003;29(11):93-7. [PubMed]
- 5.Centers for Disease Control and Prevention. Preliminary clinical description of severe acute respiratory syndrome. JAMA 2003;289(15):1920-1. [DOI] [PubMed]
- 6.Wax R, Mazurik L, Campbell VT. Using the Stryker T4 personal protection system for high-risk procedures during SARS outbreaks. Toronto: The Greater Toronto Area Critical Care / Emergency Medicine Advisory Group, Mount Sinai Hospital; 2003.
- 7.SARS Provinicial Operations Centre. Directives to all Ontario acute care hospitals for high-risk procedures involving SARS patients critical care areas. Directive 03-06 (R). Toronto: Ontario Ministry of Health and Long-Term Care; 2003 May 13. Available: http://sars.medtau.org/revisedhighrisk.pdf (accessed 2004 May 17).
- 8.Peiris JSM, Chu CM, Cheng VCC, Chan KS, Hung IF, Poon LL, et al. Clinical progression and viral load in a community outbreak of coronavirus-associated SARS pneumonia: a prospective study. Lancet 2003;361:1767-72. [DOI] [PMC free article] [PubMed]
- 9.Cooper A, Joglekar A, Adhikari N. A practical approach to airway management in patients with SARS. CMAJ 2003;169(8):785-7. [PMC free article] [PubMed]
- 10.Mount Sinai Hospital Critical Care Unit. SARS resources. Protected code blue. Available: http://sars.medtau.org/pcb.html (accessed 2004 Mar 17).


