Abstract
Objective
To determine if blood transfusion requirements in patients with isolated blunt splenic injury (BSI) are greater if they are managed nonoperatively, we did a retrospective case study of patients with isolated BSI who were seen at a Canadian university teaching hospital over a 10-year period.
Method
Data such as number of units of packed erythrocytes transfused and mortality in the 75 patients with isolated BSI seen from 1992 to 2002 were separated into operative and nonoperative management groups.
Results
In the operative management group (n = 10), patients received more transfused erythrocytes (3.0 v. 0.7 units), and a higher proportion of patients were transfused (80% v. 20%). There were no deaths in either group.
Conclusion
In the management of isolated BSI, initial nonoperative management does not increase patients' requirements for blood transfusion.
Abstract
Objectif
Pour déterminer si les patients ayant subi un traumatisme splénique fermé (TSF) isolé ont davantage besoin de transfusions sanguines s'ils reçoivent un traitement non chirurgical, nous avons procédé à une étude de cas rétrospective sur 10 ans des patients victimes d'un TSF et traités à un centre hospitalier universitaire au Canada.
Méthode
On a séparé entre groupes de traitement chirurgical et non chirurgical des données portant notamment sur le nombre d'unités de culot globulaire transfusées et le taux de mortalité chez les 75 patients victimes d'un TSF traités de 1992 à 2002.
Résultats
Chez les sujets traités chirurgicalement (n = 10), les patients ont reçu moins de transfusions de culot globulaire (3,0 c. 0,7 unité) et une plus grande proportion de patients ont reçu une transfusion (80 % c. 20 %). On n'a signalé aucun décès dans les deux groupes.
Conclusion
Dans la prise en charge du TSF isolé, le traitement non chirurgical initial n'augmente pas le besoin de transfusions sanguines chez les patients.
At the present time, a trial of nonoperative management (nonOM) for a reasonable length of time is considered to be the standard of care in hemodynamically stable adult patients with blunt abdominal trauma who suffer splenic injury.1 Splenic salvage is seen to be important because splenectomized patients are susceptible to lifelong risks of rare but serious infections.2 Such a practice can also be seen as part of a broader trend in contemporary surgery toward the development of less invasive management strategies. Improved quality and accessibility of computed axial tomography (CT) and better monitoring of critically ill patients have also broadened surgeons' comfort level with nonOM.3 During the last decade, several studies have documented the safety and efficacy of nonOM for blunt splenic injury (BSI) in adults: Peitzman and colleagues4 showed in a multi-institutional study from the USA that a success rate of 61.5% was attainable for planned nonOM of BSI, and failures (i.e., initially unplanned operations) occurred in only 10.8% of these cases. Garber and associates,5 in a Canadian single-institution study, documented a similar 69% success with nonOM.
More recently, other studies5,6,7,8,9 have compared operative management (OM) and nonOM strategies by means of multiple parameters: mortality, infectious complications, lengths of stay (LoS) in the intensive care unit (ICU), LoS in hospital, blood transfusion requirement and comparative hospital costs. Several of these studies7,8 found that more units of blood were transfused into patients with BSI who were managed by operation. It would be disquieting if the price of nonOM seemed to be excessive use of blood products, with their attendant risks.
It is, however, quite possible that observed differences7,8 in units transfused might reflect major intrinsic differences between the groups chosen for OM and nonOM. If so, these differences could well be a source of unavoidable bias, and render any conclusions made on treatment strategies flawed. It seems likely on clinical grounds that patients with hemodynamic instability who are unresponsive to appropriate fluid resuscitation are going to require urgent operation, and are likely to be different from more stable patients in whom a true management option exists. It might seem also that the former group would be expected to have greater transfusion requirements. These studies7,8 involved patients with multiple injuries, some with potential to cause hemorrhage, which may have been at least partly responsible for worsening the degree of circulatory instability ascribed to BSI. This complexity may have been the reason for the higher reported Injury Severity Scores (ISS) in the OM groups; as such, the inclusion of such multiply injured patients may have weakened the conclusion that nonOM can of itself result in diminished transfusion requirements.
It is almost certainly not acceptable to randomize all patients with BSI to OM or nonOM, and because of this it is unlikely that conclusions about blood transfusion requirements in the 2 groups can be reached by results from randomized controlled trials.
Our clinical impression has been that there is no cost in terms of excessive blood transfusion requirements in patients with BSI who are appropriately selected for nonOM. We believe that for comparison purposes, a patient subgroup that was treated for isolated BSI, free of other injuries that might contribute to blood loss, might better address this question than the broader group of all BSI cases. The purpose of our review was therefore to attempt to confirm that there is no cost in terms of excessive transfusion needs for adult patients with isolated BSI who were treated initially with a trial of nonOM.
Methods
The study proposal was approved by the Ottawa Hospital Research Ethics Board. All patients with BSI seen at that institution from April 1992 to March 2002 were identified through a trauma registry and hospital medical records. Data extracted included age, sex, comorbidities, admission medications, mechanism of injury, ISS, admission hemodynamic parameters (systolic blood pressure, heart rate and respiratory rate), worst hemodynamic parameters in the emergency department (ED), admission hemoglobin (Hb), lowest Hb, hours until first transfusion, number of units of packed erythrocytes transfused, findings from CT and ultrasound imaging, timing and nature of any operative procedures (splenectomy, splenorrhaphy, splenic artery embolization), operative findings, AAST (American Association for the Surgery of Trauma) grade of injury, hospital LoS and eventual outcome.
During this decade a total of 338 patients with BSI were seen. Of these, 107 had isolated BSI, defined as BSI with imaging or operative findings of spleen damage but without any other abdominal or extra-abdominal injuries with potential to contribute to hemodynamic instability. Minor injuries that were not expected to contribute to such instability were allowed: minor closed head injuries, rib fractures without hemothorax, minor soft-tissue injuries and metacarpal fractures. As well, 32 more patients were excluded because they either had pre-existing splenic pathology or were taking anti-coagulants. These exclusions were made in the belief that such patients would be much more likely to require OM, and as such would inevitably contribute to creating bias.
This left a group of 75 patients whom we believed best fit our criteria for isolated BSI. Although this is a small number of patients, it does represent the total experience of a decade at a busy regional trauma centre, and we feel it is a large enough group to offer insights into the relative merits of the 2 management strategies of interest.
The 75 patients were separated into 2 groups by initial intent to manage. Ten patients were defined as an OM group, all of whom underwent operative interventions within 6 hours of arrival in hospital. The other 65 patients were treated nonoperatively for at least 6 hours after arrival; they were categorized as the nonOM group. We looked closely at 5 failures (7.7%) in the nonOM group; although this was a very small subgroup, we hoped to gain some insights into the reasons for failure in these patients.
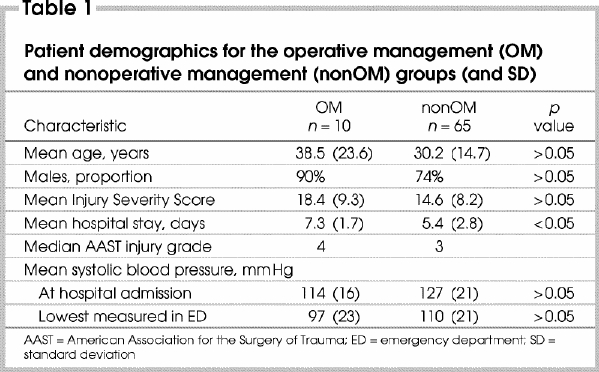
Continuous variables were compared using the 2-sample 2-tailed t test and categorical variables by χ2 analysis. Analysis of variance was used to compare OM and nonOM and AAST grade as covariables affecting the number of units of packed erythrocytes transfused. An alpha error of p < 0.05 was considered statistically significant. Patient demographics for the groups are presented in Table 1.
Table 1
Results
Most patients (65) were in the nonOM group, but 5 of these did require eventual OM, a failure rate of 7.7% for this strategy. The 15 operations required among all 75 patients included 12 splenectomies, 2 splenorrhaphies and 1 embolization. The 2 groups appeared to be generally similar in demographics (Table 1), with no significant differences except for mean hospital LoS, which averaged nearly 2 days longer in the OM group.
The median AAST grade of splenic injury (4 in the OM and 3 in the nonOM group) was also 3 in the 60 in whom nonOM was successful; although not statistically significant, this may be an indication that injuries were more severe in the OM group. In the absence of randomization, it is not possible to discount the possibility that those in the OM group had a worse pattern of injury and that higher transfusion requirements resulted from this rather than from the management strategy chosen. The median AAST grade for the 5 patients who “failed” in the nonOM group was 4 (1 patient was grade 3, 3 were grade 4 and 1 was grade 5). Figure 1 illustrates transfusion requirements by grade of injury for the OM versus nonOM groups. When type of management strategy and AAST grade of injury were analyzed as covariables to the number of units of packed erythrocytes transfused, only management strategy was significant (p < 0.05) as an independent factor influencing transfusion volume.
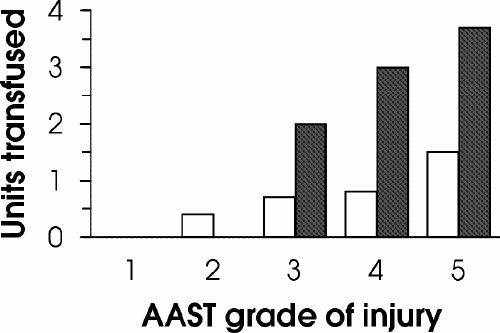
FIG. 1. Transfusion requirements of patients managed nonoperatively (white columns) and operatively (black columns), in units of packed erythrocytes, by American Association for the Surgery of Trauma grade of injury.
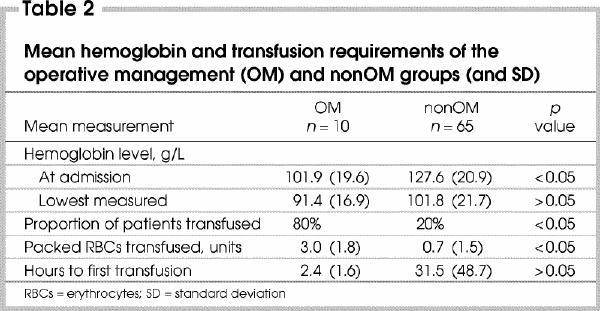
Table 2 summarizes the Hb and transfusion requirements for the 2 groups. Significant differences were seen for average Hb concentration at admission (101.9 g / L in the OM group v. 127.6 g/L nonOM), percent of patients transfused (80% OM v. 20% nonOM), and the mean volume of packed erythrocytes transfused (3.0 units OM v. 0.7 units nonOM). Notably, the group proportion being transfused and the mean transfusion volumes were taken to be clinically relevant as well as statistically significant.
Table 2
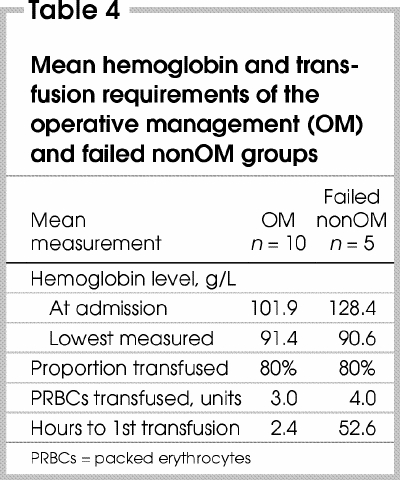
We were particularly interested in the small group of patients who failed nonOM and required delayed operative intervention. Although comparisons with the OM group of their demographics (Table 3) and Hb values and transfusion requirements (Table 4) are shown, because of the small numbers no attempt was made to perform statistical analysis. Nonetheless, because the 2 groups appear at least similar in injury severity and in transfusion requirements, the “failed” nonOM patients would not seem to have been seriously disadvantaged by not undergoing an earlier operation. The mean time to operation in the failed group was 47.9 hours, but the range was wide, from 6 to 18 hours plus a notable outrider at 198 hours. The mean time to first transfusion of about 2 days in the failed group suggests post-injury bleeding that was delayed rather than immediate was the major clinical manifestation, but again the same outrider (transfused first at 182.7 h) may have unduly influenced this impression. In fact, we identified no clear way in which these failures could have been predicted.
Table 3
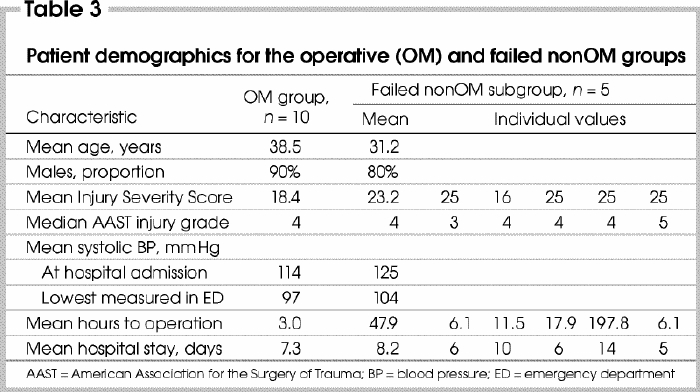
Table 4
Discussion and conclusion
For adult patients with blunt abdominal trauma and splenic injury, if they are judged hemodynamically stable, management now involves a trial of nonoperative care. However, there are no absolute guidelines as to when operative intervention becomes necessary. Even within our single institution, variations in practice exist between individual surgeons; some are comfortable staying with nonOM for a little longer than others. Unless hemodynamic instability supervenes, the decision to operate is usually based on falling hemoglobin values along with rising and unacceptable transfusion requirements.
In the end, the purpose of splenic operation is to prevent further bleeding and to protect against the consequences of transfusion. Large-volume transfusion can result in catastrophic problems like coagulopathy and organ failure, but lower amounts are still able to cause serious difficulties from incompatibility reactions and disease transmission.10 Concerns about transfusion-related dangers as a consequence of nonOM clearly work as a trigger in deciding to intervene operatively.
In this report, we have attempted to address the question of whether there is a cost in terms of excess transfusion requirements when patients are managed by the contemporary standard of an initial trial of nonoperative care. Although our comparison groups (OM and nonOM) were unlikely to have excluded all sources of bias, stronger evidence in the form of randomized treatment groups is unlikely to emerge. For the present, by including only patients who had suffered isolated BSI, we hoped to select a fairly uniform population on which to base our conclusions. With these limitations, the 2 groups appeared to be quite similar in respect to patient demographics (age, sex, ISS and admission systolic blood pressure). The median AAST injury grade was higher in the OM group, though not significantly. Parameters that reflected more severe initial hemorrhage (mean admission blood pressure, lowest ED systolic blood pressure, admission Hb, lowest Hb, proportion transfused, units of packed erythrocytes transfused and hours to first transfusion) were all less favourable in the OM group, and some reached statistical significance. From a clinical standpoint this finding is not really unexpected, and it underscores the reality that there remains a group of patients with BSI for whom nonOM is not feasible and for whom the therapeutic goals should be early recognition and prompt intervention. The finding that the mean volume of packed erythrocytes transfused differed significantly (an average of 3.0 units in the OM group and 0.7 in the nonOM group) reassured us that transfusion requirements for the nonOM group were well below those seen in our more severely injured OM group.
The most interesting group of all were our 5 patients who failed in the nonOM group. Because of the small number, it is difficult to draw firm conclusions, but it took 10 years to assemble even these few cases, and they represent only 7.7% of the entire nonOM group. There are clearly some risks to undertaking nonOM of BSI: if ongoing hemorrhage occurs and is profuse or undetected, the results could be catastrophic, and it is in this group that such events are able to occur. It is in patients like these that the highest potential exists for poor clinical outcomes, and for medicolegal difficulties. It would be most beneficial to be able to identify, when they are first seen, patients with a strong likelihood of failure with nonoperative treatment: they could be either converted to an operative strategy or monitored particularly closely. In either approach the expectation would be that they could be spared the consequences of excess transfusions.
We found “failed nonOM” patients to be similar to those in the OM group, but were unable to identify features that would separate them from the majority who were successfully managed in the nonOM group. For the present, at any rate, the only safe course of management would seem to be continued careful monitoring of and aggressive use of splenic arteriography/embolization or operation in patients for whom concerns arise. We were gratified to find that even in the failed subgroup of nonOM patients, there were no deaths, and the mean volume of packed erythrocytes transfused (4.0 units) compared favourably to the 3.0-unit average in the OM group.
In summary, we believe that in the absence of higher levels of evidence our findings support our clinical impression that that there is no cost in terms of excessive blood transfusion requirements in those patients appropriately selected for nonoperative management of BSI. The price in the occasional patient who has failed nonOM appears to have been about one extra unit transfused, without mortality; this does not seem clinically highly relevant. This in no way negates the need for meticulous monitoring of patients managed nonoperatively, with aggressive intervention when needed.
Acknowledgments
Thanks to E. Brennan. RN, C. Larabie, data analyst, and C. Martel, administrative assistant.
Competing interests: None declared.
Correspondence to: Dr. John Lorimer, Ottawa Hospital — General Campus, 501 Smyth Rd., Rm. K-11, Ottawa ON K1H 8L6; fax 613 737-8371; jlorimer@ottawahospital.on.ca
Accepted for publication Nov. 8, 2004
References
- 1.Clancy TV, Ramshaw DG, Maxwell JG, Covington DL, Churchill MP, Rutledge R, et al. Management outcomes in splenic injury: a statewide trauma center review. Ann Surg 1997;226:17-24. [DOI] [PMC free article] [PubMed]
- 2.Pachter HL, Guth AA, Hofstetter SR, Spencer FC. Changing patterns in the management of splenic trauma: the impact of nonoperative management. Ann Surg 1998;227:708-19. [DOI] [PMC free article] [PubMed]
- 3.Brasel KJ, DeLisle C, Olson CJ, Borgstrom DC. Splenic injury: trends in evaluation and management. J Trauma 1998;44:283-6. [DOI] [PubMed]
- 4.Peitzman AB, Heil B, Rivera L, Federle MB, Harbrecht BG, Clancy KD, et al. Blunt splenic injury in adults: multi-institutional study of the Eastern Association for the Surgery of Trauma. J Trauma 2000;49:177-87; discussion 187-9. [DOI] [PubMed]
- 5.Garber BG, Pham B, Fairfull-Smith RJ, Yelle JD. Management of adult splenic injuries in Ontario: a population-based study. Can J Surg 2000;43:283-8. [PMC free article] [PubMed]
- 6.Cocanour C, Moore FA, Ware DN, Marvin RG, Duke JH. Age should not be a consideration for non-operative management of blunt splenic injury. J Trauma 2000;48:606-12. [DOI] [PubMed]
- 7.Konstantakos AK, Barnoski AL, Plaisier BR, Yowler CJ, Fallon WF Jr, Malangoni MA. Optimizing the management of blunt splenic injury in adults and children. Surgery 1999;126:805-13. [PubMed]
- 8.Garber BG, Yelle JD, Fairfull-Smith RJ, Lorimer JW, Carson C. Management of splenic injuries in a Canadian trauma centre. Can J Surg 1996;39:474-80. [PMC free article] [PubMed]
- 9.Nix JA, Costanza M, Daley BJ, Powell MA, Enderson BL. Outcome of the current management of splenic injuries. J Trauma 2001;50:835-42. [DOI] [PubMed]
- 10.McIntyre L, Hébert P. To transfuse or not in trauma patients: a presentation of the evidence and rationale. Curr Opin Anæsthesiol 2002;15:179-85. [DOI] [PubMed]


