A saddle embolism of the aorta causes an acute ischemia of the lower extremities (LX). In a third of patients, various degrees of sensory and motor deficits occur,1 but sudden paraplegia is seen rarely and its cause is unclear.
Case report
On March 5, 2002, a woman 85 years of age (body surface area, 1.5 m2) had a sudden episode of severe pain in both groins with radiation to the LX. Ten minutes later, she was affected by paraplegia.
Her pulse and heart rate were rapid and irregular; abdominal tenderness precluded the exclusion of an abdominal aortic aneurysm. Both LX were bluish and cold. She lost her sensory and motor function completely to the level of the hypogastrium, and her femoral and distal pulses were absent. Her urinary output was normal.
Electrocardiography showed atrial fibrillation–flutter with episodes of bradycardia and supraventricular tachycardia, from 25 to 166 beats/min. Arterial blood-gas analysis revealed metabolic acidosis. After a rapid intravenous (IV) bolus infusion of contrast medium administered while waiting for the operative room, computed tomography of the chest and abdomen disclosed a saddle embolism of the aorta at the level of L4 (Fig. 1). There was no evidence of an aortic dissection, aneurysm or atherosclerosis.
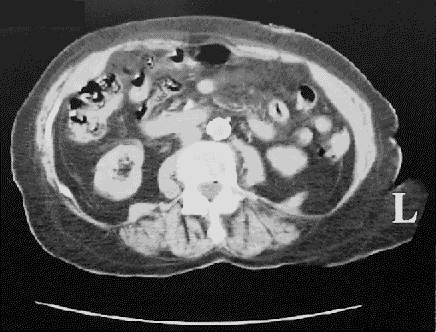
FIG. 1. A computed tomographic view of the aortic bifurcation. A rapid intravenous bolus infusion of contrast medium revealed a thrombus at the L4 level, without significant aortic-wall disease.
She was given oxygen and an IV infusion of 0.9% NaCl with 100 mEq sodium bicarbonate per litre, along with a bolus of 6000 units of heparin sodium, followed by a drip of 600 units/h, and she was digitalized by an IV route.
Four hours later the common, superficial and deep femoral arteries were exposed through a bilateral vertical groin incision. She had no pain, no bleeding from vessels and no pulse in her LX. The left common femoral artery (CFA) had an extensive obstructive atherosclerotic plaque. The embolism was removed through a longitudinal arteriotomy of the left CFA and a transverse arteriotomy of the right CFA with use of a No. 6 Fogarty balloon catheter. Exploration of the right superficial femoral, popliteal and tibial arteries (carried out with the aid of a No. 4 Fogarty catheter) and of the right deep femoral artery (with a No. 3 Fogarty balloon catheter) yielded multiple clots.
There was satisfactory backbleeding. Each CFA system was infused with 125 mL of a 0.9% NaCl solution with 2500 units of heparin sodium. The left CFA was endarterectomized and widened with a synthetic patch angioplasty.
After removal of the vascular clamps from the femoral arteries, the patient's distal pulses returned, followed by a prompt return of sensory and motor function of both LX. The interval from the onset of paraplegia to reperfusion of the LX was about 6 h, 15 min.
She became fully ambulatory within a week and achieved a normal sinus rhythm with the help of a permanent dual-chamber (DDDR) pacemaker with a switch mode and sotalol hydrochloride (80 mg by mouth, every 12 h for 1 wk).
Comment
The arterial blood supply to the spinal cord is supplied to 1 anterior and 2 posterior spinal arteries of the cervical (C1– 7) cord by the vertebral and subclavian arteries; to the arteries of the upper thoracic (T1–7) cord, by the aorta via the upper intercostal branches; to those of the thoracolumbal (T8–L5) cord, by the lower intercostal and lumbal arteries via the greater radicular artery (GRA — the arteria radicularis magna of Adamkiewicz2); and to the cauda equina, and rarely to the conus, by the lower lumbal, iliolumbal and lateral sacral arteries.2,3 The “watershed” system exists only between the cervical and the upper thoracic arterial blood supply to the spinal cord. In 85% of patients the GRA originates on the left side of the aorta, via branches of the intercostal arteries at the level of T7–12; in 60% of patients it originates via branches of the intercostal or lumbar arteries at the level of T8–L4. It rarely arises at the level of L3 (1.4%) or L4–5 (0.2%). A low origin of the GRA at the level of L1–5, or a high origin at T5–6 with the supplementary anastomotic arterial ansa of the conus at L1–5, occurs in 15% of patients.
We have assumed that in this patient, the cause of paraplegia was both ischemia of the lowest portion of the spinal cord from an occlusion of the supplementary anastomotic arterial ansa of the conus at the L4 level with a high origin of the GRA, and ischemia of the peripheral nerves.
Competing interests: None declared.
Correspondence to: Dr. Andrew S. Olearchyk, 129 Walt Whitman Blvd., Cherry Hill, NJ 08003-3746, USA; telephone or fax 856 428-0505; asolearchyk@yahoo.com
Accepted for publication Mar. 23, 2004
References
- 1.Surowiec SM, Isiklar H, Sreeram S, Weiss VJ, Lumsden AB. Acute occlusion of the abdominal aorta. Am J Surg 1998;176:193-7. [DOI] [PubMed]
- 2.Adamkiewicz A. Die Blutgefässe des menschlichen Rückenmarkes (Blood vessels of the human spinal cord) [monograph in 2 parts: Sitz K Akad Wiss (Wien), Math-naturwiss Klass 84, 85]. I Theil. Die Gefässe der Rückenmarkssubstantz (Vessels of the spinal cord substance). 1881; 84: 469-502. II Theil. Die Gefässe der Rückenmarkesoberflache (Vessels of the spinal cord surface). 1882; 85:101-30. Polish.
- 3.Connolly JE. Prevention of spinal cord complications in aortic surgery. Am J Surg 1998;176:92-101. [DOI] [PubMed]


