Abstract
The objective of the consensus conference of the Canadian Association of Thoracic Surgeons (CATS) was to define the scope of thoracic surgery practice in Canada, to develop standards of practice, to define training and resource requirements for the practice of thoracic surgery in Canada and to determine appropriate waiting times for thoracic surgery care. A meeting of the CATS membership was held in September 2001 to address issues facing thoracic surgeons practising in Canada. The discussion was facilitated by an expert panel of surgeons and supplemented by a survey. At the end of the meeting, consensus was reached by the membership regarding the issues outline above.
The membership agreed that the scope of practice includes diagnosis and management of conditions of the lungs, mediastinum, pleura and foregut. They agreed that appropriate training in thoracic surgery included completion and certification in general or cardiac surgery prior to completing a 2-year program in thoracic surgery. The membership supported the Canadian Society of Surgical Oncology recommendations for management of cancer patients that new patients should be seen within 2 weeks of referral and cancer therapy initiated within 2 weeks of consultation. Thoracic surgical care is best delivered by 2 or 3 fully certified thoracic surgeons, in regional centres linked to a cancer centre and trauma unit. The establishment of a critical mass of thoracic surgeons in each centre would lead to improved quality and delivery of care and allow for adequate coverage for on-call and continuing medical education.
Abstract
Circonscrire le champ d'exercice de la chirurgie thoracique au Canada, élaborer des normes de pratique, définir les besoins en formation et en ressources pour la pratique au Canada et déterminer les temps d'attente appropriés pour les soins en chirurgie thoracique. Au cours d'une conférence de concertation de l'Association canadienne de chirurgie thoracique (ACCT) en septembre 2001, les membres ont abordé les problèmes auxquels font face les chirurgiens thoraciques qui pratiquent au Canada. La discussion a été animée par un groupe d'experts constitué de chirurgiens, et complétée par une enquête. À la fin de la réunion, les membres se sont entendus sur les enjeux présentés.
Les membres ont convenu que le champ d'exercice comprend le diagnostic et la prise en charge de problèmes des poumons, du médiastin, de la plèvre et de l'intestin antérieur. Ils ont reconnu qu'une formation appropriée en chirurgie thoracique comprenait une formation et une certification en chirurgie générale et thoracique avant un programme de deux ans en chirurgie thoracique. Les membres ont appuyé des recommandations, présentées par la Société canadienne de chirurgie oncologique, sur la prise en charge de patients atteints de cancer, selon lesquelles il faudrait recevoir en consultation les nouveaux patients dans les deux semaines suivant la référence et commencer un traitement contre le cancer dans les deux semaines suivant la consultation. Il est préférable que les soins en chirurgie thoracique soient dispensés dans des centres régionaux reliés à un centre d'oncologie et un service de traumatologie, par deux ou trois chirurgiens thoraciques entièrement certifiés. La création d'une «masse critique» de chirurgiens thoraciques dans chaque centre améliorerait la qualité et la prestation des soins et permettrait une couverture suffisante pour les périodes de garde et l'éducation médicale continue.
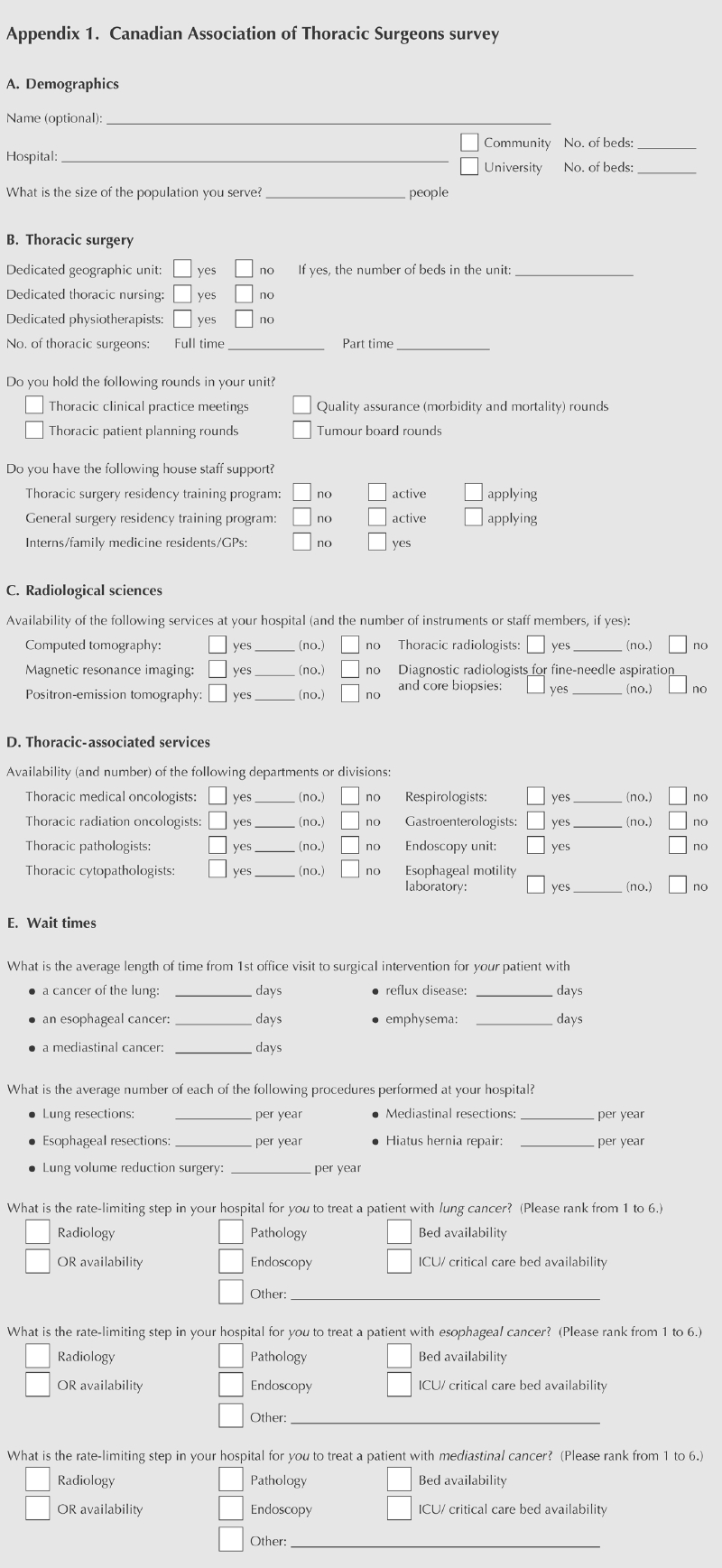
At the meeting of the Canadian Association of Thoracic Surgeons (CATS) in September 2001, a consensus conference was held to address issues surrounding the practice of thoracic surgery in Canada. The focus of the conference was to identify the scope of thoracic surgical practice in Canada, the resources and training required for it, and issues affecting delivery of care. The meeting included a panel of 8 thoracic surgeons from across Canada, 4 with community-based practices and 4 university-based. Results of a recent survey of the CATS membership (see Appendix 1 on pages 444–445) were reviewed as part of this conference. At the conclusion of the meeting, consensus from the membership was achieved on scope of practice, resource and training requirements and recommendations for the practice of thoracic surgery in Canada.
The membership of CATS includes full-time practitioners of general (noncardiac) thoracic surgery, along with qualified general and cardiovascular surgeons whose practice includes > 50% thoracic surgery. From the 68 members, 47 surveys were returned completed (69%), including 3 by members practising in the United States. The 44 Canadian surveys cited 32 participating hospitals, 18 of which were university-associated and 14 community-based. The population served ranged from 100 000 to 4 million.
Scope of practice
In Canada, the scope of thoracic surgical practice includes the diagnosis and management of benign and malignant diseases of the lung, esophagus, foregut, mediastinum, chest wall, pleura and pleural space. Even though the appropriate management of some conditions may not include surgery, thoracic surgeons are best qualified to determine or coordinate the appropriate therapy. This may include, for example, surgery, radiation, chemotherapy or image-guided surgery.
Thoracic surgeons are experts in the management of diseases within their scope of practice and not just practitioners of particular surgical techniques. In this, they differ from some surgical specialties (indeed, this pattern may differ from the practice of thoracic surgery in other countries). For example, a patient with an abnormal chest radiograph may be referred to a thoracic surgeon who will then determine the diagnosis. If the diagnosis is lung cancer, the thoracic surgeon will proceed with a staging evaluation of that cancer and assess the patient for possible surgery or, if that is not appropriate, refer the patient to medical and/or radiation oncology, or coordinate combined chemotherapy, radiation and surgery. That is not to say that thoracic surgeons are expert in all these disciplines, but they are knowledgeable of the appropriate treatment options for lung cancer of all stages, and participate in multidisciplinary care when appropriate.
After a surgical procedure for cancer, thoracic surgeons continue to follow patients, as would any oncologist. Such follow-up is not limited to oncology cases. Long-term follow-up for some benign diseases, such as gastroesophageal reflux disease, is also appropriate for proper evaluation of surgical results.
Another example of the scope of thoracic surgical practice is the management of pleural space problems. Although an interventional radiologist may drain a pleural fluid collection such as an empyema and leave a small bore drain in place, sometimes this therapy is inadequate. Someone with knowledge of the management of pleural-space problems must determine when a simple drain is not adequate and surgical intervention is necessary, rather than inserting another small-bore drain. Often, a thoracic surgeon will be asked to follow a patient with a pleural drain inserted by a radiologist. The thoracic surgeon has the knowledge of management of pleural-space problems and is in the best position to decide when a simple drain is appropriate or when decortication or rib resection is required.
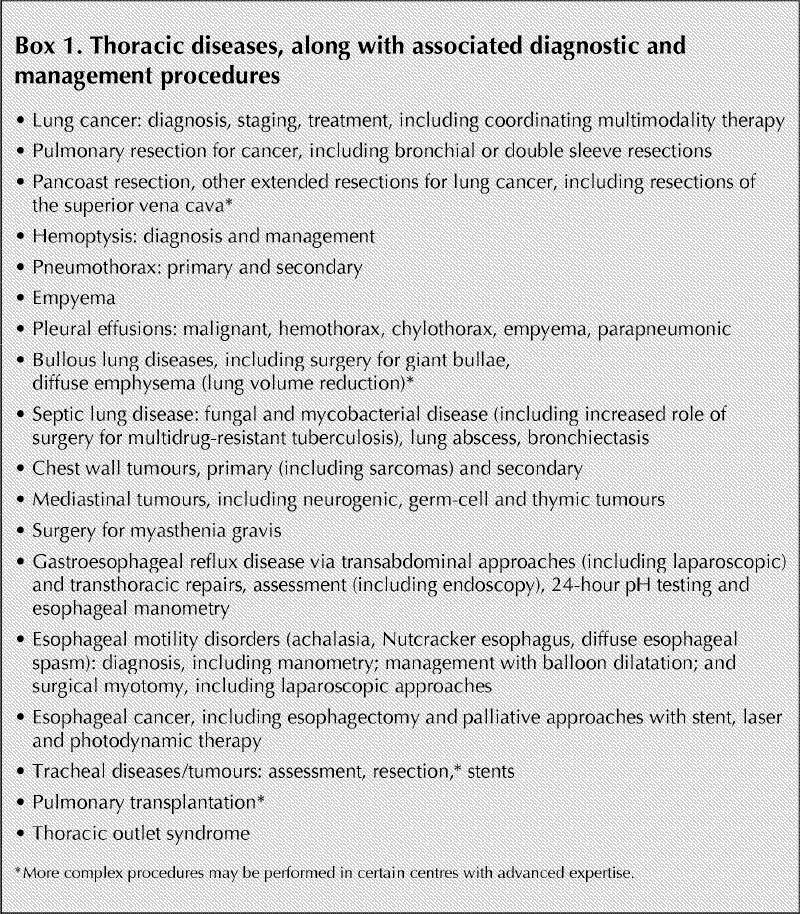
What is the scope of thoracic surgical practice in Canada? Box 1 lists the diseases or problems that thoracic surgeons consider within their purview. There may be overlap with other specialists for some of these diseases. Some treatments or techniques may be limited to centres with specialized expertise, e.g., pulmonary transplantation or lung-volume reduction surgery.
Box 1.
Training requirements for general thoracic surgery
Given the scope of practice of thoracic surgery in Canada, which differs somewhat from other countries, how should we train thoracic surgeons for practice here? In Canada, thoracic surgery arose as a subspecialty of general surgery, and cardiac surgery subsequently developed from thoracic surgery. Cardiac and thoracic surgery were combined as a specialty in the United States; but in Canada in the 1970s, the Royal College of Physicians and Surgeons of Canada recognized that the practice of general thoracic surgery was markedly different from cardiac surgery and established the Certificate of Competence in Thoracic Surgery. As a result, thoracic surgery in Canada developed as a more-or-less independent specialty, with training in thoracic surgery occurring after completion of general surgery training. However, thoracic surgery has continued to have some overlap with cardiac surgery, particularly in issues regarding training.
In an effort to reduce the length of surgical training, in 1997 an initiative was begun to have medical students choose to enter either cardiac or thoracic surgery residencies directly out of medical school.1 However, the consensus of the membership was that full training and certification in either general or cardiac surgery was required before thoracic surgery training, and that certification with examination in thoracic surgery should be is required to practice thoracic surgery in Canada. As a result, this “Canadian Initiative” has since been reversed for thoracic surgery, so that applicants for thoracic surgery must now complete training in general or cardiac surgery before entering thoracic surgery training.2
Discussion at the consensus conference emphasized that since thoracic surgery includes surgery of the tracheobronchial tree and upper alimentary tract, thoracic surgeons must be knowledgeable of the anatomy of the abdomen as well as the chest and neck. They must be facile with esophageal resection and reconstruction, which by definition includes surgery of the stomach, small bowel and colon. Required technical skills include laproscopy, thoracoscopy, intestinal resection and anastomoses, gastric resection and reconstruction as well as techniques of pulmonary resection, chest wall resection and reconstruction, and vascular anastomoses and repair. Thus, full training in general surgery is essential.
Thoracic surgeons must be capable of dissection and repair of the great vessels and heart. They must be knowledgeable of cardiac physiology and pharmacology in the intraoperative and postoperative management of patients having a pulmonary resection. For some procedures such as pulmonary transplantation, competency in instituting cardiopulmonary bypass is required. Hence, training in cardiac surgery is also important.
In addition, the thoracic surgeon must be a skilled endoscopist and bronchoscopist with both flexible and rigid bronchoscopy, laryngoscopy and upper gastrointestinal endoscopy. Therapeutic bronchoscopy is predominantly done by thoracic surgeons rather than respirologists. Management of hemoptysis, airway tumours and airway foreign bodies is still best handled using a rigid bronchoscope. Insertion of esophageal and airway stents to relieve malignant obstruction is an important component of thoracic surgery practice.
The training of a thoracic surgeon must be broad-based and include knowledge of cardiopulmonary anatomy, physiology and resuscitation; gastrointestinal anatomy and physiology; microbiology and immunology; radiology of the chest, neck and abdomen; and principles of thoracic anesthesia. Thoracic surgeons must be knowledgeable about appropriate treatment options, including chemotherapy and radiation for neoplasms of the lung, esophagus, stomach, mediastinum and pleura.
In Canada, thoracic surgery is practised in 12 large urban, usually academic, centres and in many smaller communities. In the community, thoracic surgeons often must cover general surgery for the purposes of being on call. General surgery also accounts for 25%–40% of their elective practice. They therefore must be certified in general surgery in order to practice in the community.
The RCPSC recently attempted to address length of training with a program whereby thoracic surgery was a primary specialty with entry from medical school.1 This program has since been terminated, largely for the reasons just discussed. There was concern that residents were not adequately trained in general surgery. Because residents were not certified in general surgery, they were limited to centres large enough to permit restriction of their practice to thoracic surgery only and were unable to practise in other, smaller communities.
Resource requirements for thoracic surgery
During the consensus conference, a panel of thoracic surgeons from across Canada discussed their practice environment. On average, each full-time equivalent thoracic surgeon provides service to 150 000–500 000 people. They have 1.1–2.0 operating room (OR) days available per week and practise in hospitals with more than 250 beds. Bed allotment to thoracic surgery varies, as many share beds with general surgery.
Although those practising in larger centres may practice and share call with other thoracic surgeons, most of those in small-to-medium– sized cities are isolated from other thoracic surgeons and share call with general surgeons. Although the communities in which these surgeons practice are smaller, the catchment area they serve is often extensive. This can translate into being on-call for thoracic surgery virtually 100% of the time, and covering general surgery calls as well in ratios varying from 1 day in 6 (1:6) to 1:3. These surgeons have no thoracic backup when they want to attend continuing medical education (CME) events or take vacation.
According to CATS survey responses, almost all university centres (83%) have a geographic thoracic unit with patients centralized in a ward with dedicated nursing and physiotherapists, compared with only 14% of community-based hospitals. University-based thoracic practices all consisted of full-time thoracic surgeons, with an average of 2.4 per centre (range 2–5), whereas in the community the average was 1 surgeon/centre. Respondents practising at university centres reported having access to general (94%) or thoracic (91%) surgery or family medicine residents (56% of respondents) as house staff. In the community, only 43% had access to house staff (entirely family medicine residents).
From an education and quality assurance point of view, there was little disparity between the 2 practices. All university hospitals held morbidity and mortality rounds, compared with 86% of community hospitals. Most university hospitals held clinical practice meetings and multidisciplinary tumour board rounds (each 83%), but only half or so had patient planning rounds (56%). In the community setting, considerable drop-off in all these types of rounds was reported (7%, 57% and 14%, respectively).
All hospitals, university and community, had access to computed tomography and image-guided fine-needle or core biopsy. However, only 83% of university centres had dedicated thoracic radiologists; in community hospitals, even fewer (50%). Access to magnetic resonance imaging was about equal in all centres (86%–89%), as was positron emission tomographic scanning (11%– 14%).
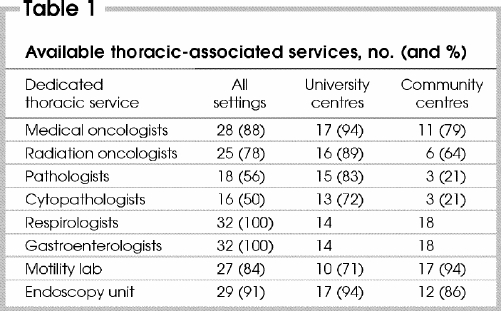
Although associated services were available in all centres, dedicated thoracic subspecialists, medical oncologists, radiation oncologists, pathologists and cytopathologists were more often available at university centres than at community centres. Although both types of centre had respirologists and gastroenterologists available, their numbers were reported as being higher at university centres (7.9 respirologists and 5.6 gastroenterologists) than at community hospitals (2.6 respirologists and 3.3 gastroenterologists; Table 1).
Table 1
The membership agreed that the following 4 resource requirements are recommended for the delivery of optimum patient care in the practice of thoracic surgery:
Each community should have at least 2 thoracic surgeons to provide coverage for call, holidays and CME. The population base required for a full-time thoracic surgeon is estimated at 300 000– 500 000. For a community to have 2 surgeons, both likely will have to practice general surgery or each some other subspecialty (e.g., vascular surgery). Community centres serving catchment areas with populations > 500 000 will have enough work for full-time thoracic surgeons.
A clinical program in thoracic surgery should include a thoracic surgeon, respirologist, gastroenterologist, chest radiologist, interventional radiologist, dedicated thoracic anaesthesiologist, thoracic pathologist, medical oncologist, intensivist, dedicated nurses with expertise in thoracic surgery and oncology, physiotherapist and respiratory technologist. A radiation oncologist is also desirable.
Physical requirements include a dedicated thoracic unit with 5–6 ward beds per surgeon and 2 intensive care unit (ICU) beds per surgeon, associated with a cancer centre. The surgeon must have block time in the OR (16 h/wk) and endoscopy (2–3 h/wk). The OR must have up-to-date video equipment for laparoscopy, thoracoscopy, bronchoscopy and gastroscopy. These staff and resource requirements are best provided at institutions with > 250 beds.
Since much of thoracic surgery relates to oncology, proximity to a cancer centre would be ideal. This is increasingly important, as many patients require combined-modality therapy, which appears to yield the best results if chemotherapy and radiation are given concurrently. Many smaller centres have medical oncologists, but patients must be sent to larger centres for radiation. For optimal care delivery, thoracic surgery services should be delivered in centres with a radiation facility. Permitting thoracic surgeons to practise together in centres of excellence should also improve care and can facilitate an improved practice environment for the surgeons.
On-call requirements
The recommendation, as for other surgical specialties and trainees, is 1:3 or 1:4. Thoracic surgeons who share call with general surgeons are effectively on-call for thoracic surgery all the time; we have therefore suggested reducing their formal requirement to 1:6. Those in an academic centre with other thoracic surgeons should have normal on-call responsibilities, 1:3.
Waiting times
The problem of waiting times was formally addressed in the CATS survey (Appendix 1).
Table 2 lists the average annual number of surgeries performed per centre for the 5 most common thoracic procedures. By far the majority occur in university centres (e.g., 168 v. 66 lung resections/site), but even at those the range is broad. (Data on outcome, length of stay, morbidity and mortality of each of these procedures was not collected.)
Table 2
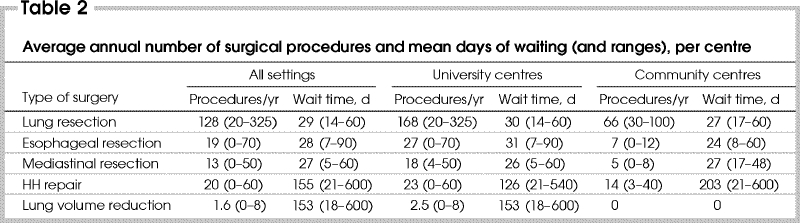
Table 2 also displays the average wait time for each of the 5 chosen procedures. Wait time was defined as the time from the first office visit to surgical intervention; it does not include the wait between receiving a request for consultation and the actual consultation visit. For operations for malignant disease, mean wait time was less in community than university centres (e.g., 24 v. 28 d for lung resections), but differences were not large, and there was considerable overlap in range. For the 2 operative procedures for benign disease, wait times were shorter at university centres, but again, all ranges were large.
In the survey, for all 5 procedures, the rate-limiting step was OR availability, in both community and university hospitals. The second most common, for malignant procedures, was availability of diagnostic imaging; for the 2 benign procedures, bed availability. In contrast, for the 3 physicians who practise in the United States, the rate-limiting step for all 5 procedures was diagnostic imaging.
All surgeons who participated in the consensus conference expressed concern about the length of waiting lists for cancer surgery as well as the interval between consultation and operative intervention. Tumour growth clearly occurs while patients are waiting for treatment, which in some cases results in tumours becoming incurable.3,4,5 The membership agreed with the recommendation of the Canadian Society for Surgical Oncology that new cancer referrals should be seen within 2 weeks of referral, and treatment initiated within 2 weeks of consultation.6 All surgeons indicated they would see a new cancer patient within 1–2 weeks of receiving the referral. However, if the patient required surgery, the shortest reported interval between decision to operate and operative intervention was 3 weeks. Delays in taking the patient to the OR most frequently resulted from 3 factors: OR unavailability; requirements for diagnostic imaging or image-guided biopsy; and consultations to internists and/or cardiologists. Average time from decision to operate to surgical intervention varied between 3 and 12 weeks. The interval between initial consultation and decision to operate varied considerably because of diverse investigative requirements. The best-case scenario for consultation to operative intervention was 3– 4 weeks; worst-case, 12–16 weeks.
The CATS recommendation is that the time from consultation to operative intervention ideally should be 2 weeks, but certainly no more than 4 weeks, for cancer patients.
Standards of practice
The consensus of the Canadian Association of Thoracic Surgery is that the practice of thoracic surgery should be associated with a regional cancer centre and trauma centre. It should be performed in regional centres with appropriate manpower and physical resources. There should be at least 2 (ideally 3 or more) thoracic surgeons per centre. Surgeons practising thoracic surgery should be fully trained in thoracic surgery and meet the requirements for certification of special competence in thoracic surgery as specified by the RCPSC. Each regional centre should have the resource requirements to be able to meet the guideline of 2–4 weeks from consult to resection.
Several studies have shown improved patient outcomes for complex procedures when performed by surgeons who do a high volume of such procedures. Just as importantly, complex procedures have better outcomes if performed in high-volume centres.7,8
The standards outlined above will allow surgeons to participate more fully in continuous professional development, as well as allow adequate practice volumes to maintain and improve outcomes. By establishing a critical mass of thoracic surgeons and patients, recruitment of associated specialists will be facilitated, which in turn will improve both the quality and delivery of care.
Summary
The practice of thoracic surgery includes the diagnosis and management of diseases of the lungs, mediastinum, foregut, pleura and pleural space. The scope of practice is quite broad; thoracic surgeons thus need the breadth of general surgical training as well as focused training in thoracic surgery. As complexity of care continues to increase, many general surgery trainees receive inadequate training in thoracic surgery, so the burden of thoracic surgical care falls to surgeons who have had additional training in thoracic surgery.
To maintain competence and quality of care, practitioners of thoracic surgery must maintain adequate volumes of surgery and have time for CME. This would be facilitated by establishing centres for thoracic surgery wherein several surgeons could provide care, which would allow adequate volumes to maintain competence, development of support services and backup for on call, vacation and CME purposes.
Surgical waiting times and health care delivery are problems across Canada, affecting all areas of medicine.9 They have resulted from increasing demand and a chronically under-resourced health care system. Thoracic surgery is clearly falling short of meeting the recommendations of the Canadian Society of Surgical Oncology.
Appendix 1.
Competing interests: None declared.
Correspondence to: Dr. Gail E. Darling, Toronto General Hospital, 200 Elizabeth St. 10EN-228, Toronto ON M5G 2C4; fax 416 340-3660; gail.darling@uhn.on.ca
Accepted for publication Dec. 22, 2003
References
- 1.Mulder DS, McKneally MF. The education of thoracic and cardiac surgeons: a Canadian initiative. Ann Thorac Surg 1995;60:236-8. [DOI] [PubMed]
- 2.Royal College of Physicians and Surgeons of Canada. Objective of training and specialty training requirements in thoracic surgery. Ottawa: the College; 2002. Available: http://rcpsc.medical.org/residency/certification/training/thorsur_e.html (accessed 2004 Aug 9).
- 3.O'Rourke N, Edwards R. Lung cancer treatment waiting times and tumour growth. Clin Oncol 2000;12:141-4. [DOI] [PubMed]
- 4.Bozcuk H, Martin C. Does treatment delay affect survival in non-small cell lung cancer? A retrospective analysis from a single UK centre. Lung Cancer 2001;34:243-52. [DOI] [PubMed]
- 5.Christensen ED, Harvald T, Jendresen M, Aggestrup S, Petterson G. The impact of delayed diagnosis of lung cancer on the stage at the time of operation. Eur J Cardiothorac Surg 1997;12:880-4. [DOI] [PubMed]
- 6.CSCC. Canadian Strategy for Cancer Control draft synthesis report. Ottawa: CSCC; 2001. Available: http://209.217.127.72/cscc/pdf/Synthesis_Jan18_e.pdf (accessed 2004 Aug 9).
- 7.Dimick JB, Pronovost PJ, Cowan JA, Lipsett PA. Surgical volume and quality of care for esophageal resection: Do high-volume hospitals have fewer complications? Ann Thorac Surg 2003;75:337-41. [DOI] [PubMed]
- 8.Simunovic M, To T, Theriault M, Langer B. Relation between hospital surgical volume and outcome for pancreatic resection for neoplasm in a publicly funded health care system. CMAJ 1999;160(5):643-8. [PMC free article] [PubMed]
- 9.Simunovic M, Gagliardi A, McCready D, Coates A, Levine M, DePetrillo D. A snapshot of waiting times for cancer surgery provided by surgeons affiliated with regional cancer centres in Ontario. CMAJ 2001;165(4):421-5. [PMC free article] [PubMed]


