Abstract
Background
To establish the efficiency of minimally invasive procedures in the diagnosis and management of abdominal (intestinal and peritoneal) tuberculosis (AT), I retrospectively and then prospectively evaluated clinical, physical and laboratory findings in patients with AT at a university general-surgery clinic. Diagnostic and therapeutic options were also considered.
Methods
Data from the case records of 43 patients diagnosed with AT via laparotomy were collected and analyzed. On the basis of findings from that early analysis, a further 37 patients were studied prospectively. In the latter group, percutaneous aspiration, endoscopy and laparoscopy were used for diagnosis, except in cases with acute abdominal findings or failure of these diagnostic procedures. Morbidity and mortality rates and mean hospitalization time were evaluated for both groups.
Results
In the early group of 43 patients, the morbidity rate was 30%; mortality, 12%; and median hospital stay, 18.3 days (standard deviation [SD] 6.2 d). The diagnosis was confirmed by laparotomy in 18 patients in the prospective group: laparoscopy or endoscopy in 10 and percutaneous drainage of an intra-abdominal abscess in 9. Changes in our approach to diagnostic procedures in the prospective group led to decreased morbidity (11%), mortality (0) and median hospital stay (9.3 [SD 4.7] d).
Conclusions
Minimally invasive procedures such as laparoscopic, endoscopic and percutaneous biopsy should be used for diagnosis of IPTB as a first step in diagnosis. Laparotomy should be performed only when complications develop or diagnosis remains unclear in spite of these diagnostic modalities.
Abstract
Contexte
Pour établir l'efficience d'interventions à effraction minimale visant à diagnostiquer et à traiter la tuberculose intestinale et péritonéale (TBIP), j'ai évalué rétrospectivement et ensuite prospectivement les résultats d'examens cliniques, physiques et de laboratoire de patients atteints de TBIP dans une clinique universitaire de chirurgie générale. On a aussi tenu compte des options diagnostiques et thérapeutiques.
Méthodes
J'ai recueilli et analysé des données tirées de dossiers de 43 patients chez lesquels on a diagnostiqué une TBIP par laparotomie. Compte tenu des résultats de cette première analyse, j'ai étudié de façon prospective les dossiers de 37 autres patients. Dans ce dernier groupe, on a utilisé l'aspiration percutanée, l'endoscopie et la laparoscopie pour poser le diagnostic, sauf dans les cas de résultats abdominaux aigus ou lorsque ces interventions de diagnostic ont échoué. J'ai évalué pour les deux groupes les taux de morbidité et de mortalité, ainsi que la durée moyenne de l'hospitalisation.
Résultats
Dans le premier groupe, le taux de morbidité s'est établi à 30 %, le taux de mortalité, à 12 %, et la durée médiane de l'hospitalisation, à 18,3 jours (écart type [ET] 6,2 j). On a confirmé le diagnostic par laparotomie chez 18 patients du groupe de suivi, par laparoscopie ou endoscopie chez 10 autres et par drainage percutané d'un abcès intra-abdominal dans 9 cas. Dans ce dernier groupe, le taux de morbidité est tombé à 11 %, le taux de mortalité, à 0 %, et la durée médiane de l'hospitalisation, à 9,3 (ET 4,7) jours en raison du changement de méthodes de diagnostic.
Conclusions
Il faudrait utiliser des méthodes à effraction minimale comme la laparoscopie, l'endoscopie et la biopsie percutanée pour diagnostiquer une TBIP comme premier moyen de diagnostic. Il faudrait pratiquer une laparotomie seulement lorsque des complications font leur apparition ou que le diagnostic n'est toujours pas clair malgré le recours à ces méthodes de diagnostic.
Abdominal tuberculosis (AT) was quite common in the world in the first half of the 20th century.1,2,3 After the advent of effective antituberculous (anti-TB) chemotherapy and improved standards of living, AT diminished in frequency, particularly as a complication of pulmonary tuberculosis.1,3,4,5,6,7,8,9,10 Recently, however, the incidence of primary AT has increased slightly because of immigration, freedom of world travel and increasing prevalence of human immunodeficiency virus (HIV) infection.1,3,8,11,12,13,14 Diagnosis may also have increased due to wider awareness of the disease and use of improved diagnostic facilities.3,5,7,8,9,11,12,13,14,15,16
The peritoneum and intestine are the most frequently involved sites. Intestinal (IT) and peritoneal tuberculosis (PT) imitate many other abdominal diseases. Not only are the signs and symptoms of AT nonspecific, but laboratory and radiological findings are also insufficient for diagnosis. The disease can therefore easily be misdiagnosed or missed if the physician is unsuspicious. These delays in diagnosis result in high rates of morbidity and mortality.4,7,15,17,18,19,20
The aim of this study was to review the patients with IT and PT who came to our centre; to assess the value of the clinical, physical and laboratory findings; and to discuss diagnostic and therapeutic options.
Methods
From January 1990 through December 1994, 43 patients with IT or PT were diagnosed and treated at Dicle University Hospital, Diyarbakir, Turkey. Their age, sex, medical history, symptoms and physical findings were recorded. All patients underwent hematological, biochemical and radiographic investigations (chest and abdomen). Skin tests with purified protein derivative (PPD) and ultrasonography (US) were used for diagnosis in non-emergency conditions. All patients underwent surgery after resuscitation for drainage, intestinal bypass or resection. Preoperative antibiotics and adequate fluids and electrolytes were administered intravenously.
Diagnoses were based principally upon laparotomy and histopathologic examination of surgical specimens. Existence of caseating granuloma was accepted as indicative of tuberculosis (TB). Results of PPD skin tests were considered positive if the induration exceeded 10 mm in diameter. Diagnostic and surgical procedures were evaluated retrospectively in terms of morbidity and mortality rates and the time spent in hospital.
After consideration of these findings, a 5-year prospective study was planned for 1995 through 1999 of (as it turned out) 37 patients. Computed tomography and US were used as diagnostic procedures in all patients except those with acute abdominal symptoms. Percutaneous aspiration and secondary laparoscopy were performed in patients with an intra-abdominal abscess or fluid collection, located via US or CT. If imaging revealed an intra-abdominal mass on the bowel wall, colonoscopy was performed, then laparoscopy.
When the area of gut affected could be reached with a flexible endoscope, diagnosis was based on visible segmental ulcers (Fig. 1), inflammatory strictures or hypertrophic lesions, confirmed by biopsy. Upon laparoscopy, either the presence of ascites or tubercle formation on the peritoneum and bowel wall were considered diagnostic. When evidence from percutaneous aspiration, colonoscopy or laparoscopy was insufficient to diagnose AT, diagnosis was made by mini-laparotomy, which is performed under the umbilicus through a 5-cm midline incision. Therefore, the definitive diagnosis of AT was made by histopathological examination on material obtained by laparotomy, laparoscopy or endoscopy, isolation of Mycobacterium tuberculosis in cultures, or the presence of acid-fast bacilli in smears.
FIG. 1. Colonoscopic appearance of an ileocecal tuberculosis.
After the diagnosis was confirmed, anti-TB medications were given for at least 12 months to all patients: Rifampicin (600 mg/d for 9 mo), pyrizinamide (30 mg/kg/d for 2 mo) and isoniazid (300 mg/d for 12 mo). Deaths within the first month after surgery were categorized as operative mortalities. All patients were followed up for least 1 year, with abdominal US repeated at intervals of 6 months. Patients were followed monthly for the first 3 months, with less frequent follow-up and treatment thereafter, according to the clinical aspects of their TB.
The early and prospective groups were compared for diagnostic procedure, morbidity, mortality and length of hospital stay. Mean hospitalization times were evaluated by Student's t test for 2 independent means, and percentages by Student's t test modified for 2 independent ratios.
Results
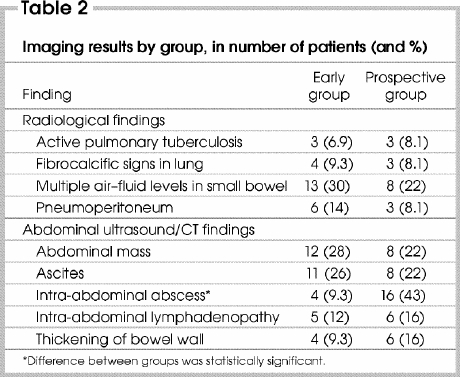
Properties of the patient population, clinical presentation and laboratory findings on admission according to groups are shown in Table 1, and early radiological and other imaging findings in Table 2. Except for anemia, high sedimentation rate and intra-abdominal abscess (upon US or CT) because of delayed diagnosis, differences between the 2 groups were not statistically significant. According to their medical histories, 19 patients (24% of all those studied), 12 in the early and 7 in the prospective group, had received anti-TB chemotherapy for pulmonary TB before admission to hospital.
Table 1
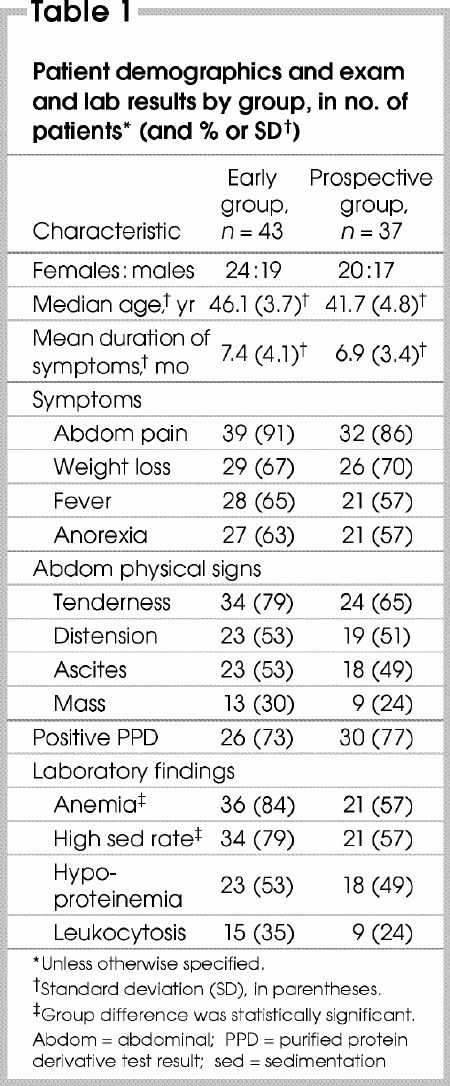
Table 2
Early group
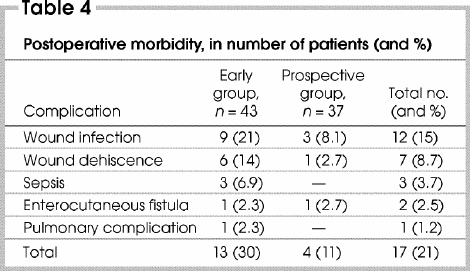
Of the 43 patients studied retrospectively, 17 (40%) underwent emergency surgery because of mechanical obstruction of the intestine in 7 cases (16%), intestinal perforation in 6 (14%) and intra-abdominal abscess in 4 (9.3%). On the operating table, PT was detected in 20 patients (47%) and IT in 23 (53%; Table 3). A total of 20 complications related to AT or its treatment occurred in 13 patients, for a patient morbidity rate of 30% (Table 4). One patient who had non- emergent and 4 patients who had urgent laparotomy died, for a mortality rate of 12%. Median hospitalization time was 18.3 days (SD 6.2 d).
Table 3
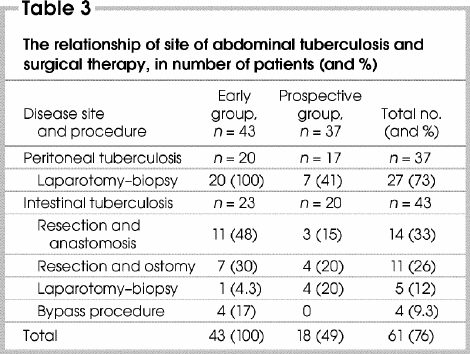
Table 4
Prospective group
Peritoneal tuberculosis was found in 17 patients (46%) and IT in 20 (54%; Table 3). Four patients with IT required urgent surgical treatment because of intestinal obstruction, and another 3 for intestinal perforation. Eight patients with radiological abnormalities underwent colonoscopy, but in 2 cases technical difficulties meant the abnormal site could not be reached. Laparoscopy was attempted in 7 patients, which in 3 cases confirmed IT histopathologically; in the other 4, multiple adhesions prevented completion. The remaining 4 patients were diagnosed with IT via laparotomy. Limited resection of the involved segment was performed in 7 patients, and biopsy with drainage alone in 4.
Sixteen patients in whom US or CT had located an intra-abdominal abscess or fluid collection underwent percutaneous aspiration; however, tubercle bacilli were noted in smears or cultures in only 9 (56%): M. bovis was isolated by culture in 5 patients, M. tuberculosis in 3 and atypical forms of mycobacterium in 1. Of 2 patients investigated laparoscopically, 1 was diagnosed successfully. In the remaining 7 patients with PT, diagnosis was made by means of mini-laparotomy. All 16 patients underwent drainage and peritoneal biopsy.
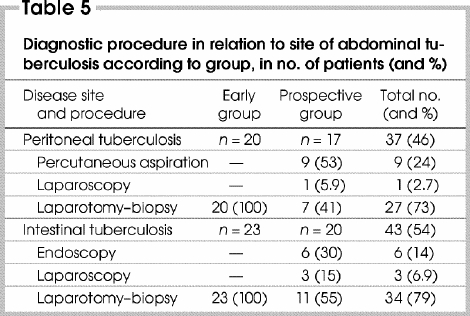
Diagnosis of AT with a minimally invasive procedure was successful in 19 patients (51%) studied prospectively; 11 (30%) had not been definitively diagnosed until surgery, and 7 (19%) had non-emergent surgery. Successful diagnostic method in relation to site of AT is shown in Table 5. Diagnosis of AT was made by histological examination of tissue in 28 patients (76%); samples were obtained via laparotomy in 18 (64%), endoscopic biopsy in 6 (21%) and laparoscopic biopsy in 4 (14%).
Table 5
During the postoperative period, 5 complications in 4 patients developed that were directly related to AT or the surgical procedure performed (49%); there were no deaths. Morbidity rate (11%; p < 0.05), mortality rate (0; p < 0.05) and median length of hospital stay (9.3 days, SD 4.7 d; p < 0.001) were all significantly lower than in the early group.
All patients
When early cases are combined with those studied prospectively, PT was detected in 37 patients and IT in 43. Morbidity (30%) and mortality rates (9.3%) in patients with IT were higher than in those with PT (11% morbidity, 2.7% mortality; p < 0.05). Emergency operations were had by 24 patients (30%) and non-emergent by 37 (46%). A total of 5 patients (6.2%) died in the early postoperative period, of whom 4 (17%) had urgent surgery. For those who underwent non-emergent procedures, the early postoperative mortality rate was 2.7%. Morbidity and mortality rates (both p < 0.05) and median hospitalization time (p < 0.001) of patients who had undergone elective surgery were significantly less than in those who underwent an emergency operation.
Bowel resection or a bypass procedure was performed in 29 patients. The incidence of postoperative complications in these patients (48%) was higher than in those who avoided bowel resection or bypass (9.3%; p < 0.001).
Fourteen patients were lost to follow-up. Three patients who, assuming they were entirely recovered, had interrupted their medical treatment required a reoperation because local fluid collections persisted. The remaining 58 surviving patients had follow-up periods of 12–33 months (mean 21 mo, SD 1.6 mo), during which they were considered cured. During this period 5 patients underwent additional emergency laparotomy to correct adhesive small-bowel obstruction.
Discussion
TB continues to be an important medical, social and economic problem in many developing countries where public health and sanitation are minimal. The most common site of TB is the lung, followed by the gastrointestinal tract and genitourinary system. Abdominal tuberculosis comprises tuberculous infection of the gastrointestinal tract; the mesentery, its nodes and omentum; the peritoneum; and the solid organs related to the gastrointestinal tract, such as the liver and spleen.4,5,12,13,14,15
Although AT can develop at any age, it is most common in patients 25– 45 years of age: 51 patients in my study (64%) were in this age range. Females with AT predominate slightly (45%:55%, in this study). Because the disease is insidious, symptoms of AT are generally of lengthy duration before hospital admission, ranging 1–14 months (in this study, a mean of 7.2 [SD 4.8] mo). Hematological and biochemical analyses commonly show nonspecific changes that can be important evidence of malnutrition and infection.1,2,3,4,5,6,8,9,11,12,13,14,15,16,17,18,20,21,22
Diagnosing AT with non-invasive procedures requires a high index of suspicion. A diagnosis can be made only if caseation is revealed upon histopathological examination, or if acid-fast bacilli (AFB) are found in tissue. Although radiography, US and CT imaging should be used initially in suspected cases, these are not definitive for diagnosis.1,2,3,4,5,6,8,9,12,14,17,18,22 X-ray films of the chest show evidence of active or healed pulmonary TB in 10%– 68.5% of patients with AT,3,10,12,14,15 and PPD skin test is positive in 14%–77%.5,6,8,9,12,14,17,18,22 Thus, a negative result does not rule out AT. My findings are consistent with these observations. Minimally invasive diagnostic procedures such as percutaneous aspiration and biopsy, endoscopic biopsy and laparoscopy have low rates of complication and are helpful in establishing the diagnosis in 85%–90% of recent cases.1,2,3,6,7,8,9,18,23
Initially, AFB smears and culture are helpful for diagnosis of PT. Results of microscopic examinations of ascitic fluid from patients with PT are positive for AFB in less than 5% of infected cases, and culture of ascitic fluid in 20%–83%.6,8,11,12,14,18 Cultures also take > 6 weeks, which delays diagnosis. However, when a peritoneal biopsy specimen is taken or > 1 L of ascitic fluid is aspirated and sent for AFB smears and culture, the sensitivity rate for PT exceeds 80%.5,8,9,13,16,18,22 In my series this rate was 38% for AFB smears and 19% for cultures of ascitic fluid because the amount of fluid taken was < 1 L.
Laparoscopy is a safe and accurate method for diagnosing AT. Its sensitivity is > 80%, especially in the presence of ascites, and laparoscopically guided peritoneal biopsies will detect caseating granulomas in 85%– 90% of cases. Laparoscopy unfortunately has a higher risk in patients with AT, whose abdominal organs are frequently adhered to the abdominal wall and therefore susceptible to trocar injury.2,8,9,12,13,18,22,23 In this series, when laparoscopy was attempted in 7 patients with IT, it could not be completed in 4 cases because of multiple adhesions.
In recent years, colonoscopy has been found to be very useful in the diagnosis of colonic and ileocolic TB. The most common colonoscopic features are ulcers, nodules and a deformed cecum and ileocecal valve. Colonoscopy with direct biopsy may provide rapid diagnosis for large-bowel or ileocecal TB.11,12,15,20 When colonoscopy was used in my 8 patients with colonic or ileocecal TB, it failed twice because of technical difficulties such as inappropriate bowel preparation, marked angulation of the splenic flexure and bleeding.
Since the treatment of uncomplicated AT is medical, surgical procedures for diagnosis should be avoided when possible. But when nonsurgical diagnostic procedures fail, AT cannot be considered diagnosed until exploratory laparotomy.3,5,6,8,9,10,11,12,13,15,16,17,20,22,23 In this study, diagnostic laparotomy was performed in 26 patients in the early group (60%) and 11 in the prospective group (30%), which therefore had significantly lower morbidity and mortality rates and a shorter median stay in hospital.
In the treatment of AT, surgery is used to manage complications such as obstruction, free perforation, confined perforation with abscess or fistula, massive hemorrhage and malabsorbtion syndrome.4,8,11,12,13,14,16,17,18,19 It can sometimes be difficult for a surgeon to make an appropriate decision intraoperatively on how to treat AT so as to achieve the best postoperative prognosis. Because I found the risk of postoperative abdominal complications such as intestinal obstruction or enterocutaneous fistula to be significantly higher in patients who underwent bowel resection,15 I recommend that when surgery is necessary, surgeons avoid extensive resection and operate conservatively.8,9,12,13,17,19 Because of delayed diagnosis, I saw intestinal obstruction in 11 patients (14%) and perforation in 9 (11%), requiring emergency surgery. In the prospective group my surgical team limited resection to severely inflamed, perforated or necrotic segments and avoided bypass procedures, which can lead to blind loop syndrome. Recently, however, the use of stricturoplasty has become popular in patients with minimal narrowing.13
Early diagnosis and therapy reduce mortality, whereas complications during the progress of the disease contribute to it considerably.2 In my opinion, besides the change in diagnostic approach, lower rates of complications in the prospective group (7/37, 19%) than in the early group (17/43, 40%) and urgency of operation contribute to improved morbidity and mortality rates and median hospitalization time in follow-up group with respect to early group.
Anti-TB chemotherapy with triple drugs should be started as soon as AT is diagnosed.1,2,3,4,5,6,8,9,11,12,13,14,15,16,17,18 The mortality of AT, recorded at 20%– 50%1,6,12 prior to anti-TB chemotherapy, has decreased to 2%–21% of patients treated, depending on timing of presentation.2,4,6,13,14,17
In spite of developed diagnostic techniques, some authors2,4,8,12 have suggested that an empirical therapeutic trial of anti-TB chemotherapy is often justified in suspected cases, especially in areas where it is endemic. Even though TB is still endemic in Turkey, empirical anti-TB therapy was never begun in my series of patients without tissue diagnosis.
In conclusion, since poor hygiene and nutrition are making TB more common, physicians should keep AT in mind. In the initial investigation of suspected cases, less invasive procedures such as laparoscopy, endoscopy and percutaneous aspiration should be applied. Only when complications occur or diagnosis is in doubt should laparotomy be performed. Among surgical treatments, resection should be limited and intestinal bypass avoided. Once properly diagnosed, standard regimens of anti-TB chemotherapy are effective in eradicating the infection. A suspicious approach combined with early diagnosis and treatment will reduce the complications that can develop during the progress of the disease, and thereby decrease rates of mortality and morbidity.
Competing interests: None declared.
Correspondence to: Dr. Yilmaz Akgun, Dicle Universitesi Tip Fakultesi, Genel Cerrahi Anabilim Dali, 21280 Diyarbakir, Turkey; dryilmazakgun@yahoo.com
Accepted for publication Mar. 3, 2004
References
- 1.Guth AA, Kim U. The reappearance of abdominal tuberculosis. Surg Gynecol Obstet 1991;172:432-6. [PubMed]
- 2.Lingenfelser T, Zak J, Marks IN, Steyn E, Halkett J, Price SK. Abdominal tuberculosis: still a potentially lethal disease. Am J Gastroenterol 1993;88:744-9. [PubMed]
- 3.Underwood MJ, Thompson MM, Sayers RO, Hall AW. Presentation of abdominal tuberculosis to general surgeons. Br J Surg 1992;79:1077-9. [DOI] [PubMed]
- 4.Akinoglu A, Bilgin I. Tuberculous enteritis and peritonitis. Can J Surg 1988;31:55-8. [PubMed]
- 5.Lisehora GE, Lee M, Barcia PJ. Exploratory laparotomy for diagnosis of tuberculous peritonitis. Surg Gynecol Obstet 1989;169:299-302. [PubMed]
- 6.Al-Quorain AA, Satti MB, Al-Freihi HM, Al-Gindan YM, Al-Awad N. Abdominal tuberculosis in Saudi Arabia: a clinicopathological study of 65 cases. Am J Gastroenterol 1993;88:75-9. [PubMed]
- 7.Balthazar EJ, Gordon R, Hulnick D. Ileocæcal tuberculosis: CT and radiologic evaluation. AJR Am J Roentgenol 1990;154:499-503. [DOI] [PubMed]
- 8.Marshall JB. Tuberculosis of the gastrointestinal tract and peritoneum. Am J Gastroenterol 1993;88:989-99. [PubMed]
- 9.Manohar A, Simjee AE, Haffejee AA. Symptoms and investigative findings in 145 patients with tuberculous peritonitis diagnosed by peritoneoscopy and biopsy over a five year period. Gut 1990;31:1130-2. [DOI] [PMC free article] [PubMed]
- 10.Chen WS, Leu SY, Hsu H, Lin JK, Lin TC. Trend of large bowel tuberculosis and relation with pulmonary tuberculosis. Dis Colon Rectum 1992;35:189-92. [DOI] [PubMed]
- 11.Watters DA. Surgery for tuberculosis before and after human immunodeficiency virus infection: a tropical perspective. Br J Surg 1997;84:8-14. [PubMed]
- 12.Aston NO. Abdominal tuberculosis [review]. World J Surg 1997;21:492-9. [DOI] [PubMed]
- 13.Weeragandham BRS, Lynch FP, Canty TG, Collins DL, Dankner WM. Abdominal tuberculosis in children: review of 26 cases. J Pediatr Surg 1996;31:170-6. [DOI] [PubMed]
- 14.Vanderpool DM, O'Leary JP. Primary tuberculous enteritis [review]. Surg Gynecol Obstet 1988;167:167-73. [PubMed]
- 15.Chen WS, Su WJ, Wang HS, Jiang JK, Lin JK, Lin TC. Large bowel tuberculosis and possible influencing factors for surgical prognosis: 30 years experience. World J Surg 1997;21:500-4. [DOI] [PubMed]
- 16.Ko CY, Schmit PJ, Petrie B, Thompson JE. Abdominal tuberculosis: the surgical perspective. Am Surg 1996;62:865-8. [PubMed]
- 17.Sherman S, Rohwedder JJ, Ravikrishnan KP, Weg JG. Tuberculous enteritis and peritonitis. Arch Intern Med 1980;140:506-8. [PubMed]
- 18.Bhargava DK, Shriniwas, Chopra P, Nijhawan S, Dasarathy S, Kushwaha AKS. Peritoneal tuberculosis: laparoscopic patterns and its diagnostic accuracy. Am J Gastroenterol 1992;87:109-12. [PubMed]
- 19.Talwar S, Talwar R, Prasad P. Tuberculous perforations of small intestine. Int J Clin Pract 1999;53:514-8. [PubMed]
- 20.Misra SP, Misra V, Dwivedi M, Gupta SC. Colonic tuberculosis: clinical features, endoscopic appearance and management. J Gastroenterol Hepatol 1999;14:723-8. [DOI] [PubMed]
- 21.Ihekwaba FN. Abdominal tuberculosis: a study of 881 cases. J R Coll Surg Edinb 1993;38:293-5. [PubMed]
- 22.Lisehora GB, Peters CC, Lee YT, Barcia PJ. Tuberculous peritonitis — do not miss it. Dis Colon Rectum 1996;39:394-9. [DOI] [PubMed]
- 23.Apaydin B, Paksoy M, Bilir M, Zengin K, Saribeyoglu K, Taskin M. Value of diagnostic laparoscopy in tuberculous peritonitis. Eur J Surg 1999;165:158-63. [DOI] [PubMed]


