Abstract
Background
Injury to the physis of the distal tibia in children can lead to subsequent growth arrest. This can result in physeal bars, leg-length discrepancies and angular deformities.
Method
The cases of 12 children with distal tibial growth arrest due to ankle trauma were reviewed. All were treated at a tertiary care institution between 1990 and 2002.
Results
The average age at initial injury was 9.7 years (range 5–13 yr). Salter–Harris classifications (SH) of their injuries were SH2 in 4 children, SH3 in 1, SH4 in 6 and SH5 in 1 child. Four involved open fractures; 5 were high-energy injuries. Six of the injuries resulted in simple physeal bars, 4 caused pure angular deformities and 2 resulted in leg-length discrepancies > 2 cm. Eight of the physeal arrests were treated either with bar excision, selective epiphysiodesis or osteotomy for angular correction.
Conclusion
This series reinforces the importance of frequent follow-up of distal tibial physeal injuries in order to detect growth arrest early, thus facilitating corrective surgery.
Abstract
Contexte
Les lésions de la plaque cartilagineuse du tibia distal chez l'enfant peuvent conduire à un arrêt de croissance subséquent. Il peut en résulter l'apparition d'une bande de tissu conjonctif au niveau de l'épiphyse, une inégalité de longueur des membres et des difformités angulaires.
Méthode
On a étudié le cas de 12 enfants présentant un arrêt de croissance du tibia distal consécutif à un traumatisme de la cheville. Tous les enfants ont reçu un traitement dans un établissement de soins tertiaires entre 1990 et 2002.
Résultats
L'âge moyen lors de la première blessure s'établissait à 9,7 ans (intervalle de 5 à 13 ans). Selon la classification de Salter–Harris (SH), les lésions se classaient comme suit : catégorie SH2 chez quatre enfants, catégorie SH3 chez un enfant, catégorie SH4 chez six enfants et catégorie SH5 chez un enfant. Quatre cas comprenaient une fracture ouverte et il y avait cinq cas de blessure à haute énergie. Six des blessures ont entraÎné des bandes simples au niveau de l'épiphyse, quatre ont provoqué des difformités angulaires nettes et deux ont entraÎné des différences de longueur > 2 cm. Huit des cas d'arrêt de croissance de l'épiphyse ont fait l'objet d'un traitement faisant appel soit à l'excision de la bande, soit à une épiphysiodèse spécifique, soit à une ostéotomie pour la correction angulaire.
Conclusion
Cette série réitère l'importance d'assurer un suivi fréquent des lésions de l'épiphyse du tibia distal afin de détecter rapidement les arrêts de croissance et, par conséquent, de favoriser la chirurgie corrective.
The distal tibial physis contributes 40% of the longitudinal growth of the tibia, compared with 60% in the proximal physis.1,2 During the years of most rapid growth in childhood, the distal physis contributes about 6 mm/yr.
Physeal ankle injuries are the second most common growth-plate injuries, after those of the distal radius.3 They can occasionally cause physeal growth arrest of the distal tibia, with subsequent bony bar, angular deformity or leg length discrepancy.
Despite the frequency of ankle injuries, few recent studies have addressed the treatment of growth arrest of the distal tibia. Among the existing reports,4,5 treatment options include shoe lifts, bony bar excision, contralateral and ipsilateral epiphysiodeses, leg lengthening, corrective angular osteotomy and Ilizarov corrective procedures.
The purpose of this paper was to review posttraumatic distal tibial growth arrests treated at our institution; to characterize the original (index) injuries, subsequent deformities and treatments required; and to propose principles for the treatment of distal tibial physeal fractures and subsequent deformities.
Method
All cases of children with distal tibial growth arrest treated at our tertiary care pediatric institution from January 1990 through December 2002 were studied retrospectively. Pediatric patients with triplane or Tillaux fractures tend to be older, and their limited remaining growth makes their case progression different. These cases were therefore excluded.
All clinical charts and accompanying radiographic studies were reviewed. Data recorded from charts included patient demographics; the mechanism, classification and treatment of the original injury; characteristics of the physeal growth arrest and accompanying deformity; and subsequent treatment of the physeal arrest. The images reviewed included all x-ray, CT and MRI studies available from the time of original injury until the latest follow-up.
Injuries were classified according to their Salter– Harris (SH) pattern;6 injury mechanisms, as high-energy (involving motor vehicles) or low-energy (falls, sports activities).4
Results
A total of 12 cases were identified that fit the inclusion criteria: 6 male and 6 female patients who averaged 9.7 years of age (range 5–13 yr) at the time of original injury. Mean interval from that index injury to corrective procedure was 29 months.
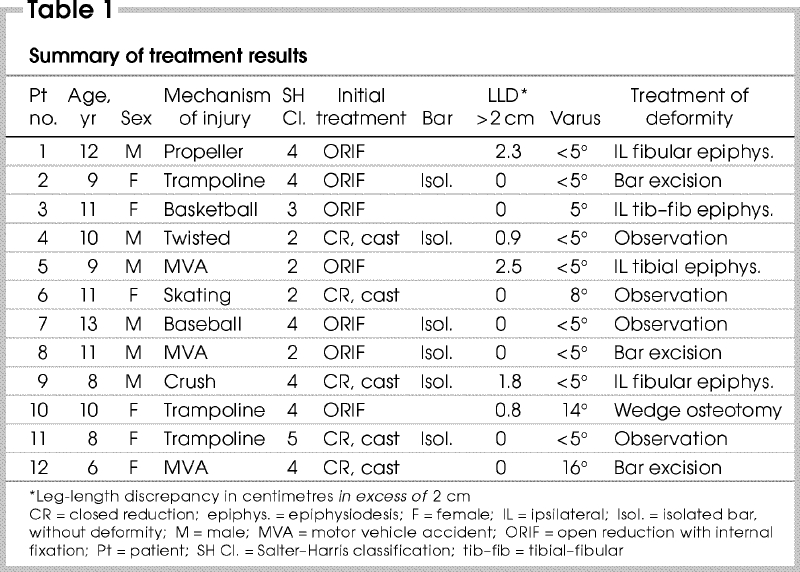
When index injuries were classified (Table 1), SH2 and SH4 categories (4 and 6 fractures, respectively) predominated over other SH patterns. Mechanisms of injury were high- energy in 5 cases and low in 7. Similarly, 4 fractures were open injuries and 7, closed. Treatment of the index injury was closed reduction and casting in 5 children; the other 7 required operative management.
Table 1
All patients were followed closely after the initial injury. They were typically seen every 3–4 months after the fracture was healed, so that any subsequent growth arrest could be detected early.
Of the 12 patients, 2 developed growth arrest with leg-length discrepancies of note: 2.3 and 2.5 cm. Four other patients developed angular deformities of 5° or more; the largest was 16°. The remaining 6 children developed a physeal bar but (to date) no deformity. This absence of deformity was attributed in some cases to the site and limited extent of the bar, but in others to early diagnosis of the growth arrest. None of the patients had simultaneous length and angular deformities of clinical significance.
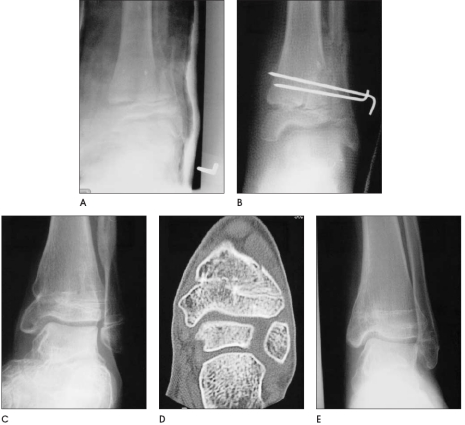
Bar excisions were performed in 3 children (Fig. 1); all resulted in continued symmetrical growth of the distal tibial physis. Epiphysiodeses were performed in 4 cases; specifics are given in Table 1. One child underwent osteotomy and epiphysiodesis (Fig. 2). The remaining 4 patients were treated conservatively, either with a shoe lift or with observation. Because these children are not yet skeletally mature, they may require surgical intervention in future; but at their most recent follow-ups, all appeared to be free of deleterious effects from the bar.
FIG. 1. An 11-year-old boy suffered a Salter–Harris 2 fracture of the distal tibia (A). A closed reduction with Kirschner-wire fixation was performed (B). This injury was subsequently complicated by a partial physeal arrest and required bar resection (C, D). A good long-term result was achieved, as shown by this radiograph at age 16 years (E).
FIG. 2. A 10-year-old girl sustained a Salter–Harris 4 fracture of the distal tibia in a trampoline injury. It required open reduction and internal fixation with a cannulated screw (A, B). She subsequently developed an 8-mm leg-length discrepancy and a 16° varus deformity from a partial physeal arrest of the distal tibia (C), as also shown by MRI (D). An opening wedge supramalleolar osteotomy and a fibular shortening osteotomy was performed to correct the varus (E). Two years later, the ankle joint functions normally despite a fibrous union of the fibula (F).
Discussion
Treatment modalities
Berson and associates4 reported the results of their own treatment of distal tibial growth arrests. Their series, which was also retrospective, differed from ours in many ways. Their average length of time from original injury to presentation with deformity was 33 months, versus 9 months in ours. Four of their 24 cases required use of an Ilizarov fixator for their osteotomy; they had major deformities, with leg-length discrepancies up to 79 mm and angular deformities up to 38°. None of the deformities in our series was serious enough to require a circular external fixator, which in our opinion was largely attributable to our emphasis on close follow-up and earlier treatment. Berson's group4 did not perform any bar excisions; they had “not had great success with this form of treatment despite the presence of good reports in the literature.” Our series included 3 bar excisions, all with good results. We consider this procedure an important part of the armamentarium for certain appropriate cases. The advent of MRI may account for the improved results of bar excision.
Angular deformities
Tibial angular deformities over 4° can lead to subsequent degenerative disease of the ankle.7 Williamson and Staheli5 recommended proceeding with corrective osteotomy at the time of physeal bar resection for any deformity over 10°. We agree with these recommendations, with the exception that osteotomies may be indicated for less severe angular deformities in older children whose physes are closed.
Berson and coauthors4 also reported that angular deformities were more likely to be associated with high- energy mechanisms of injury. Based on our experience alone, 3 of 4 angular deformities were secondary in low-energy injuries. The potential for low-energy fractures to develop angular deformities must not be ignored.
Open versus closed reduction
Spiegel and colleagues8 reported on a retrospective series of ankle fractures in an attempt to identify the injuries most at risk of developing a growth deformity. They concluded that SH3 and SH4 injuries with displacements of 2 mm or more were at high risk of posttraumatic growth arrest. Kling and co workers9 also reviewed a series of growth arrests of the distal tibia, most SH3 or SH4. Care must be taken in interpreting these results, as these series are now > 20 years old. Most fractures had been treated originally with closed reduction and immobilization. Current treatment advocates anatomical reduction with internal fixation of such fractures. No relation can be deduced from our series about the incidence of growth arrests with different patterns of physeal injuries. The distribution of our cases, mostly SH2 and SH4 (totalling 10 of 12 cases), is similar to that reported by Berson's group,4 in which 19 of 24 cases were either SH2 or SH4.
The importance of anatomic reduction of these fractures to lessen the risk of physeal growth arrest remains a controversial issue. Kling and associates9 concluded that anatomic reduction of SH3 and SH4 and probably SH2 injuries, whether by open procedures or closed, decreased the incidence of physeal arrest.8 However, Ogden10 as well as Cass and Peterson11 concluded that growth disturbances may not be prevented by open reduction and internal fixation. Certainly, this debate is not resolved with our study, but it appears intuitive to use open methods with SH3 and SH4 injuries if articular congruity cannot be achieved with closed techniques. For SH2, however, the literature provides no definite answer.
We advocate anatomic reduction of the articular surface of SH3 and SH4 fractures, whether achieved through open or gentle closed reduction. As for SH2 injuries, gentle closed reduction usually can provide reasonable alignment and less emphasis can be placed on obtaining anatomic reductions. The importance of follow- up every 3–4 months for 1 year after initial healing, for the early detection of any physeal arrest, cannot be overemphasized. Hynes and O'Brien12 elegantly demonstrated that growth disturbance lines can be detected as early as 3 months post-injury.
MRI is particularly useful in revealing not only the presence of a physeal arrest but also the location and extent of the bar. This is now our preferred imaging modality for assessing a physeal bar.
If a partial physeal arrest involving < 50% of the physis arises and is detected before a deformity is apparent, bar excision should be performed. If the patient is near the end of his or her growth, we proceed with an ipsilateral epiphysiodesis of the tibia and fibula. If a child still has any great degree of growth to attain and the leg-length discrepancy is predicted to exceed 5 cm, leg lengthening with an external fixator or an intramedullary device must be considered. Finally, if the angular deformity is clinically significant, supramalleolar osteotomy can be performed for angular correction.
Conclusion
The number of major deformities secondary to growth arrest was minimal in this series because of aggressive follow-up and early treatment. When compared to similar studies in the literature, this series reinforces the importance of frequent follow-up of distal tibial physeal injuries in order to detect growth arrest early; facilitating early corrective surgery decreases the need for more major corrective procedures later on.
Competing interests: None declared.
Correspondence to: Dr. Merv Letts, Department of Surgery, Shaikh Khalifa Medical Center, PO Box 51900, Abu Dhabi, United Arab Emirates; fax 011-971-2-610-3725; letmer764@skmc.gov.ae
Accepted for publication Feb. 18, 2004
References
- 1.Beaty JH, Kasser JR. Rockwood and Wilkin's fractures in children. Philadelphia: Lippincott Williams & Wilkins; 2001.
- 2.Morrissy RT, Weinstein SL. Lovell and Winter's pediatric orthopedics. Philadelphia: Lippincott Williams & Wilkins; 2001.
- 3.Peterson CA, Peterson HA. Analysis of the incidence of injuries to the epiphyseal growth plate. J Trauma 1972;12:275-81. [DOI] [PubMed]
- 4.Berson L, Davidson RS, Dormans JP, Drummond DS, Gregg JR. Growth disturbances after distal physeal fractures. Foot Ankle Int 2000;21:54-8. [DOI] [PubMed]
- 5.Williamson RV, Staheli LT. Partial physeal growth arrest: treatment by bridge resection and fat interposition. J Pediatr Orthop 1990;10:769-76. [PubMed]
- 6.Salter RB, Harris WR. Injuries involving the epiphyseal plate. J Bone Joint Surg Am 1963;45:587-622.
- 7.Puno RM, Vaughn JJ, Stetten ML, Johnson JR. Long-term effects of tibial angular malunion on the knee and ankle joints. J Orthop Trauma 1991;5:247-54. [DOI] [PubMed]
- 8.Spiegel PG, Cooperman DR, Laros GS. Epiphyseal fractures of the distal ends of the tibia and fibula. J Bone Joint Surg Am 1978;60:1046-50. [PubMed]
- 9.Kling TF, Bright RW, Hensinger RN. Distal tibial physeal fractures in children that may require open reduction. J Bone Joint Surg Am 1984;66:647-57. [PubMed]
- 10.Ogden JA. Skeletal injury in the child. Philadelphia: Lea and Febiger; 1982.
- 11.Cass JR, Peterson HA. Salter Harris type IV injuries of the distal tibial epiphyseal growth plate with emphasis on those involving the medial malleolus. J Bone Joint Surg Am 1983;65:1059-70. [PubMed]
- 12.Hynes D, O'Brien T. Growth disturbance lines after injury of the distal tibial physis. J Bone Joint Surg Br 1988;70:231-3. [DOI] [PubMed]