Abstract
Introduction
To describe the epidemiology of acute appendicitis in the Province of Ontario, we carried out a retrospective population-based cohort study of all patients with acute appendicitis.
Methods
Using hospital discharge abstracts of patients with acute appendicitis from all acute care hospitals in Ontario for the fiscal years 1991–1998 coded for the Canadian Institute for Health Information, we studied the demographic features, particularly age and sex, length of hospital stay (LOS), incidence, and seasonal variation of acute appendicitis.
Results
During the observation period, 65 675 cases of acute appendicitis occurred in Ontario. Of these, 58% of the patients were male and 35.5% had perforation. The mean (and standard deviation [SD]) LOS for patients with perforation was 6.2 (5.3) days versus 3 (1.8) days for patients with no perforation (p < 0.001). The age-specific incidence of acute appendicitis followed a similar pattern for males and females, but males had higher rates in all age groups. The incidence was highest in those aged 10–19 years. The annual age and sex-adjusted incidence of acute appendicitis was 75 per 100 000 population. The female:male age-adjusted rate ratio was 1:1.4. During the study period, the rate of acute appendicitis decreased by 5.1%, but the rate of appendicitis with perforation increased by 13%. A significant seasonal effect was also observed, with the rate of acute appendicitis being higher in the summer months.
Conclusions
Appendicitis is more common in males, in those aged 10–19 years, and during the summer months. The frequency of acute appendicitis appears to be decreasing whereas the proportion of cases with perforation appears to be increasing. This may reflect a change in the population structure in Ontario and restrictions placed on the patient access to the health care system.
Abstract
Introduction
Pour décrire l'épidémiologie de l'appendicite aiguë en Ontario, nous avons réalisé une étude rétrospective stratifiée représentative par cohorte qui a porté sur tous les patients atteints d'appendicite aiguë.
Méthodes
Dans tous les hôpitaux de soins actifs de l'Ontario, pour les exercices 1991 à 1998 codés selon l'Institut canadien d'information sur la santé, nous avons utilisé les résumés de congé d'hôpital des patients qui ont eu une appendicite aiguë et nous avons étudié les caractéristiques démographiques, particulièrement l'âge et le sexe, la durée du séjour à l'hôpital (DSH), l'incidence et la variation saisonnière de l'appendicite aiguë.
Résultats
Au cours de la période d'observation, il y a eu 65 675 cas d'appendicite aiguë en Ontario. De ce total, 58 % des patients étaient des hommes et 35,5 % avaient subi une perforation. La DSH moyenne (et l'écart type [ET]) chez les patients victimes d'une perforation s'est établie à 6,2 (5,3) jours par rapport à 3 (1,8) jours dans le cas des patients qui n'avaient pas eu de perforation (p < 0,001). L'incidence selon l'âge de l'appendicite aiguë a suivi une tendance semblable chez les hommes et les femmes, mais les hommes présentaient des taux plus élevés dans tous les groupes d'âge. L'incidence était la plus élevée chez les 10 à 19 ans. L'incidence annuelle comparative de l'appendicite aiguë selon l'âge ou le sexe s'établissait à 75 pour 100 000 habitants. Le ratio femme:homme comparatif selon l'âge s'établissait à 1:1,4. Pendant la période visée par l'étude, le taux d'appendicite aiguë a diminué de 5,1 %, mais celui des cas d'appendicite avec perforation a augmenté de 13 %. On a aussi observé un effet saisonnier important : le taux d'appendicite aiguë était plus élevé l'été.
Conclusions
L'appendicite est plus répandue chez les hommes, chez les 10 à 19 ans et pendant les mois d'été. La fréquence de l'appendicite aiguë semble à la baisse tandis que la proportion des cas de perforation semble augmenter. Ces statistiques peuvent refléter un changement de la structure démographique de l'Ontario et des restrictions imposées sur l'accès au système de santé pour les patients.
Appendicitis is the most common acute surgical condition of the abdomen.1 The rate of acute appendicitis varies among countries. Declining rates of acute appendicitis have been reported in the United States and Europe.2,3,4 However, the frequency appears to be increasing in the developing countries.5,6 Age, sex and seasonal variations of acute appendicitis have been observed in many studies, but the reasons for these variations are not clear.
Although acute appendicitis is a common surgical condition, little is known about its epidemiology in Canada. Therefore, this study was conducted to explore the demographic characteristics, incidence, seasonal variation and trends of acute appendicitis in the Province of Ontario from 1991 to 1998.
Methods
Study design
We conducted a retrospective population-based study to assess the demographic features, length of stay (LOS) in hospital, incidence and seasonal variation of acute appendicitis in Ontario for the fiscal years 1991–1998 (Apr. 1 of the indicated year to Mar. 31 of the following year).
Data source
Cases of acute appendicitis were obtained from the Canadian Institute for Health Information (CIHI) Discharge Abstract Database. This database records discharges from all Ontario acute care hospitals. The information is abstracted from patient charts, coded and inserted locally into hospital databases by trained personnel, then included in summaries sent to various central CIHI databases. The diagnosis codes are based on the International Classification of Diseases, 9th Revision (Clinical Modification) (ICD-9-CM), and the treatment codes are based on the Canadian Classification of Diagnostic, Therapeutic and Surgical Procedures (CCP).7 The main data elements include 4 types of information. The first is demographic information on age, sex and area of residence. The second type focuses on disease, both the primary diagnosis (most responsible diagnosis) and the secondary diagnosis and complications (up to 16 diagnoses). The third type of information specifies the procedures provided by the physician (up to 10 procedures). The fourth type specifies hospital services provided — information on admission category, LOS and special care unit stay.
These records are very complete. Studies have shown that less than 3% of the records from Ontario are missing demographic data.8 A study of Ontario data on most responsible diagnosis and principal procedures revealed an 81% level of agreement for most responsible diagnosis and 88% for primary procedures between the database and patients' charts.9
The CIHI coding of appendicitis is based on the discharge diagnosis, which itself is based on the surgical report (intraoperative diagnosis of appendicitis) or radiology report (if the patient has perforated appendicitis and percutaneous drainage under radiologic guidance without surgical intervention). Coding personnel use ICD-9-CM 540.0 and 541.1 to code cases with perforation and 540.9 to code cases without perforation. These discharge diagnosis codes should be used only if the patient has a positive appendectomy or radiologically proven perforation treated conservatively, or both. ICD-9-CM 541 (appendicitis, unqualified) is used sometimes as the discharge diagnosis for a patient who was admitted with questionable appendicitis and who underwent appendectomy that proved negative. ICD-9-CM 542 (other appendicitis) is used as the discharge diagnosis for a patient who underwent an elective appendectomy. Using the CIHI database, discharge abstracts for all patients who were discharged between Apr. 1, 1991, and Mar. 31, 1998, with a principal diagnosis of acute appendicitis with generalized peritonitis (ICD-9-CM code 540.0), acute appendicitis with peritoneal abscess (code 540.1) or acute appendicitis without mention of peritonitis (code 540.9) were included in the study. Cases with code 540.9 are referred to as “nonperforating” acute appendicitis.Cases with codes 540.0 or code 540.1 are referred to as perforated acute appendicitis. Cases with missing information on age or gender were excluded.
Statistics Canada census data provided the number of residents in Ontario and their gender and age category on July 1 of each year.
Statistical analysis
Differences among groups in demographic variables were assessed by means of the t-test for continuous variables. The age, sex and population adjusted incidence rates of appendicitis for each month and year were calculated by use of the Ontario population for the relevant month and year (obtained from Statistics Canada) as the denominator. Rates were standardized to the Ontario 1996 population by sex and 6 age groups (0–9, 10–19, 20–29, 30–39, 40–49, and ≥ 50 yr). Ordinary least-square linear regression was used to examine changes in rates of appendicitis over time.
Spectral analysis10 was conducted to assess cyclical patterns in event occurrence on a monthly basis to identify the seasonal variation. The data series was detrended using ordinary least-square regression before conducting spectral analysis.
Fisher's kappa (Fκ) test is designed to detect one major sinusoidal component buried in white noise whereas the Bartlett Kolmogorov– Smirnov (BKS) test accumulates departures from the white noise hypothesis over all frequencies.10
Results
Basic data
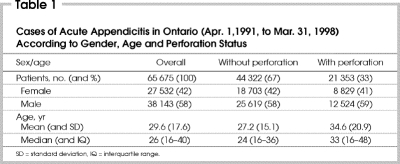
The study comprised 65 675 patients (58% were men) with acute appendicitis. Of these, 32.5% had perforation. The median age for patients with acute appendicitis was 26 years (range from 16–40 yr). The median age for patients with nonperforated appendicitis was 24 years (16–36 yr) compared with 33 years (16–48 yr) for patients with perforated appendicitis (p < 0.001) (Table 1).
Table 1
Length of hospital stay
The mean (and standard deviation [SD]) LOS was 4 (3.7) days. The mean LOS for patients with perforation was 6.2 (5.3) days versus 3 (1.8) days for patients with no perforation (p < 0.001). There was no difference in LOS between males and females.
Incidence and temporal trends
Between fiscal years 1991 and 1998, the average age and sex-adjusted incidence of acute appendicitis annually was 75 per 100 000 population. The female:male average age-adjusted rate ratio was 1:1.4 (62 per 100 000 females/yr v. 88 per 100 000 males/yr). When patients were subdivided into nonperforated and perforated groups, the age and sex-adjusted rates were 50 and 24 per 100 000/yr, respectively. The female:male average age-adjusted rate ratio was 1:1.4 (42 per 100 000 females/yr v. 59 per 100 000 males/yr) for patients without perforation and 1:1.45 (19 per 100 000 females/yr v. 29 per 100 000 males/yr) for patients with perforation.
The annual acute appendicitis rate decreased over time between fiscal years 1991 and 1998: by 5.1% (from 78 to 74 cases per 100 000 population, R 2[coefficient of determination] = 0.51, p = 0.05 [linear regression analysis]). In females, the decrease was 3.1% (from 64 to 62 cases per 100 000, R 2 = 0.40, p = 0.09) and in males 6.5% (from 93 to 87 cases per 100 000, R 2 = 0.56, p = 0.03) (Fig. 1). Similarly, for nonperforated appendicitis the annual rate decreased over time by 12.7% (from 55 to 48 cases per 100 000 population, R 2 = 0.84, p = 0.002). In females, the decrease was 11% (from 45 to 40 cases per 100 000, R 2 = 0.80, p = 0.003) and in males 13.9% (from 65 to 56 cases per 100 000, R 2 = 0.78, p = 0.004) (Fig. 2).
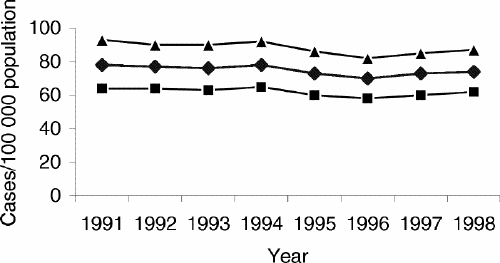
FIG. 1. Trends in acute appendicitis in Ontario per 100 000 population for the fiscal years 1991–1998 by year and sex. Diamonds = age- and sex-adjusted rate, squares = age- adjusted rate in females, triangles = age-adjusted rate in males (applies also to Figs. 2 and 3).
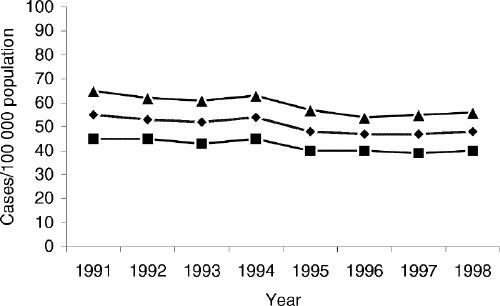
FIG. 2. Trends in acute appendicitis without perforation in Ontario per 100 000 population for the fiscal years 1991–1998 by year and sex.
However, for perforated appendicitis the annual rate increased over time by 13% overall (from 23 to 26 cases per 100 000 population, R 2 = 0.63, p = 0.02). In females, the increase was 22.2% (from 18 to 22 cases per 100 000 population, R 2 = 0.60, p = 0.03) and in males 10.7% (from 28 to 31 cases per 100 000, R 2 = 0.66, p = 0.01) (Fig. 3).
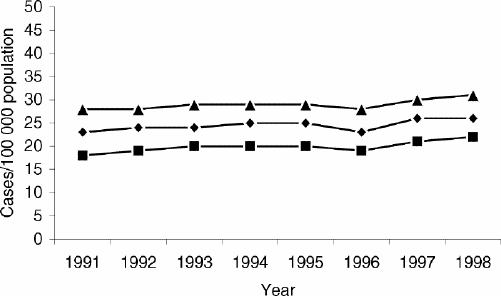
FIG. 3. Trends in acute appendicitis with perforation in Ontario per 100 000 population for the fiscal years 1991–1998 by year and sex.
The increase incidence of perforation was noted in all age groups, in both females and males, especially for the children aged 0–9 years and adults 50 years of age and older.
Age and sex differences
The age-specific incidence of acute appendicitis between fiscal years 1991 and 1998 followed a similar pattern for males and females, but males had higher rates in all age groups. The female:male rate ratio ranged from 1:1.3–1:1.5 (Fig. 4). The incidence was highest in males and females aged 10–19 years: 184 and 129 per 100 000 population per year, respectively. The incidence of acute appendicitis declined with age increment, and was lowest in young children and older adults.
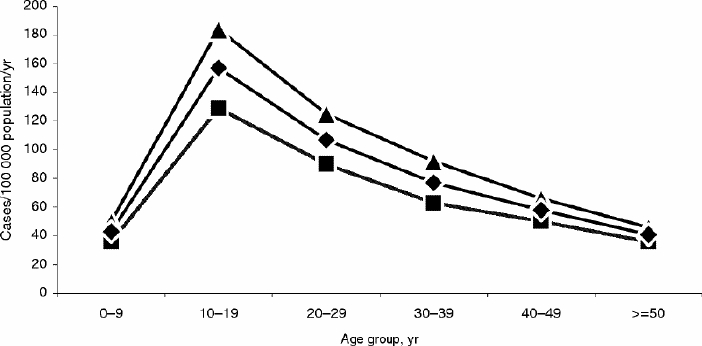
FIG. 4. Annual incidence of acute appendicitis in Ontario per 100 000 population for the fiscal years 1991–1998 by age group and sex. Diamonds = overall, squares = female, triangles = male (applies also to Figs. 5 and 6).
Similar patterns were observed for age-specific incidence when patients were subdivided into nonperforated and perforated groups. In patients without perforation, the female:male rate ratio ranged from 1:1.2–1:1.4 (Fig. 5). However, the female:male rate ratio declined with age increment and was lowest for patients who were 50 years and older (1:1.2). The incidence was highest in males and females aged 10–19 years at 136 and 98 per 100 000 population per year, respectively.
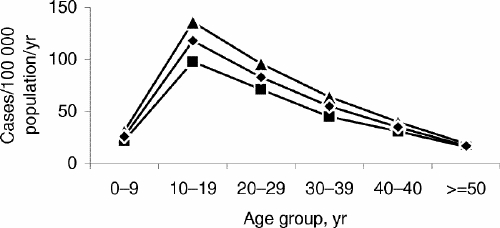
FIG. 5. Annual incidence of acute appendicitis without perforation in Ontario per 100 000 population for the fiscal years 1991–1998 by age group and sex.
In patients with perforation, the female:male rate ratio ranged from 1:1.3–1:1.6 (Fig. 6). This ratio was highest in people aged 10–19 years (1:1.6). The incidence of acute appendicitis was highest in males and females aged 10–19 years (49 and 30 per 100 000 population per year, respectively).In contrast to patients without perforation, the incidence did not decline with increasing age but increased slightly.
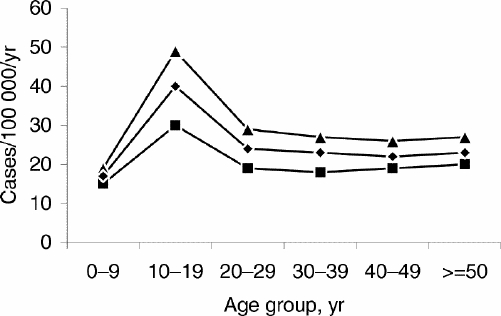
FIG. 6. Annual incidence of acute appendicitis with perforation in Ontario per 100 000 population for the fiscal years 1991–1998 by age group and sex.
Seasonal variation (Fig. 7)
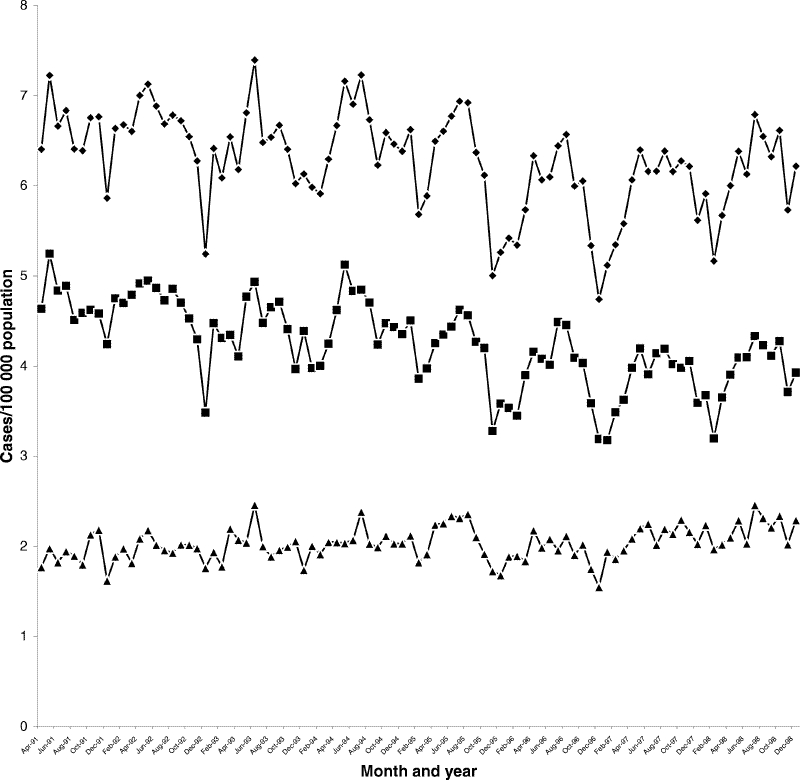
FIG. 7. Age and sex-adjusted rates of acute appendicitis in Ontario per 100 000 population by month for the fiscal years 1991–1998. Diamonds = acute appendicitis, squares = nonperforated, triangles = perforated.
The monthly series of acute appendicitis showed a major seasonal component (Fκ= 20.8, p < 0.05) and several small components that may lead to overall departures from the white-noise hypothesis (BKS = 0.53, p < 0.05). This would imply significant seasonal variations in the data. The spectral density estimates for the monthly series suggest a monthly cycle occurring approximately every 6 months. The peaks of these cycles would occur in the summer months and the troughs in the winter months.
A similar pattern of seasonal variation was found when the analysis was done for cases of nonperforated and perforated acute appendicitis. Patients with nonperforated appendicitis showed a major seasonal component (Fκ= 21.8, p < 0.05) and several small components that may lead to overall departures from the white-noise hypothesis (BKS = 0.53, p < 0.05). The seasonal variations appeared to be less pronounced but still significant in the perforated cases series, which showed a major seasonal component (Fκ= 10.0, p < 0.05) and several small components that may lead to overall departures from the white noise hypothesis (BKS = 0.32, p < 0.05). Similar pattern of seasonal variations were observed when the data were analyzed separately for females and males.
Discussion
One of the most striking epidemiologic features of appendicitis is the marked variation in incidence by age and sex. In this study, the highest incidence of appendicitis was observed in people aged 10–19 years, both males and females. This observation is consistent with the findings in other studies.2,11 Males had a higher incidence of appendicitis than females in all age groups. This finding also has been reported previously.2,12
A seasonal pattern of incidence for acute appendicitis has also been reported, with a low incidence in the winter and a higher incidence in the summer.2,12 With more sophisticated statistical analysis, we confirmed this finding. The reasons for age, sex and seasonal variations in the occurrence of acute appendicitis are not clear.
Over the study period, the overall incidence of acute appendicitis declined by 5%, consistent with the declining incidence reported in both the US and Europe.2,3,4 This observation may, in part, be related to the decline in the number of nonperforated cases, which has declined by 13%. However, the incidence of perforated cases has increased by 13%, mostly in people in the 0–9-year age group and those older than 50 years. We speculate that the increased incidence of perforation may result from 2 factors: a delay in the presentation of patients with perforated appendicitis, especially among elderly people or a delay in diagnosis owing to increased waiting time in the emergency department or delay in reaching the operating room once a diagnosis has been made. These speculations are partly supported by an aging population in Ontario and ongoing delays in health care accessibility in the province because of resource limitations.
The overall incidence of appendicitis in Ontario was 75 per 100 000 population per year, less than that reported in the US (96–120 per 100 000)2,11,13 and in Europe (116 per 100 000)14 in the 1980s. There are a number of explanations for this: the incidence of appendicitis is declining, and these figures were reported in the 1980s whereas ours are drawn from the 1990s; variation in surgical practice among countries may result in a higher threshold for taking the patients to operating room, since some cases of appendicitis resolve without operation;15 varying definitions of acute appendicitis in different studies; and ethnic and cultural differences.
The major strength of our study is the fact that it is population-based, covering all cases of appendicitis in Ontario over a period of 8 years. However, it has several potential limitations: a lack of information on the accuracy of recording the discharge diagnosis of acute appendicitis in the database; differences in the accuracy of recording the cases over the study period and among different hospitals in Ontario; and the discharge diagnosis of appendicitis is a clinical diagnosis based on intraoperative findings or radiologic appearance rather than the pathological diagnosis.
In summary, acute appendicitis is more common in males, in people aged 10–19 years, and during the summer months. The overall incidence of appendicitis declined over the study period. However, perforated appendicitis appears to be increasing over time, which may reflect a change in the population structure in Ontario and the restrictions placed on patient access to the health care system.
Competing interests: None declared.
Correspondence to: Dr. Mohammed Al-Omran, 3403–38 Elm St., Toronto ON M5G 2K5; fax 416 598-7755; m_alomran@hotmail.com
Accepted for publication Feb. 11, 2003.
References
- 1.Liu CD, McFadden DW. Acute abdomen and appendix. In: Greenfield LJ, Mulholland MW, Zelenock GB, Oldham KT, Lillemoe KD, editors. Surgery: scientific principles and practice. 3rd ed. Philadelphia: Lippincott-Raven; 1997. p. 1246-61.
- 2.Addiss DG, Shaffer N, Fowler BS, Tauxe RV. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol 1990;132:910-25. [DOI] [PubMed]
- 3.Arnbjornsson E, Asp NG, Westin SI. Decreasing incidence of acute appendicitis, with special reference to the consumption of dietary fiber. Acta Chir Scand 1982;148:461-4. [PubMed]
- 4.McCahy P. Continuing fall in the incidence of acute appendicitis. Ann R Coll Surg Engl 1994;76:282-3. [PMC free article] [PubMed]
- 5.Osman AA. Epidemiological study of appendicitis in Khartoum. Int Surg 1974;59:218-21. [PubMed]
- 6.Ofili OP. Implications of the rising incidence of appendicitis in Africans. Cent Afr J Med 1987;33:243-6. [PubMed]
- 7. Canadian classification of diagnostic, therapeutic and surgical procedures. Ottawa: Statistics Canada; 1986. cat no 82-562-XPE.
- 8.Ontario Hospital Association, Ontario Ministry of Health, Hospital Medical Records Institute. Report of the Ontario data quality reabstracting study. Toronto: Ontario Hospital Association; 1991.
- 9.Williams JI, Young W. Inventory of studies on the accuracy of Canadian health administrative databases. Toronto: Institute of Clinical Evaluative Sciences; 1996. p. 96-03-TR.
- 10.Fuller WA. Introduction to statistical time series. New York: John Wiley; 1976.
- 11.Luckmann R. Incidence and case fatality rates for acute appendicitis in California. A population-based study of the effects of age. Am J Epidemiol 1989;129:905-18. [DOI] [PubMed]
- 12.Luckmann R, Davis P. The epidemiology of acute appendicitis in California: racial, gender, and seasonal variation. Epidemiology 1991;2:323-30. [DOI] [PubMed]
- 13.Sugimoto T, Edwards D. Incidence and costs of incidental appendectomy as a preventive measure. Am J Public Health 1987;77:471-5. [DOI] [PMC free article] [PubMed]
- 14.Andersson R, Hugander A, Thulin A, Nystrom PO, Olaison G. Indications for operation in suspected appendicitis and incidence of perforation. BMJ 1994;308: 107-10. [DOI] [PMC free article] [PubMed]
- 15.Savrin RA, Clausen K, Martin EW Jr, Cooperman M. Chronic and recurrent appendicitis. Am J Surg 1979;137:355-7. [DOI] [PubMed]