Abstract
Introduction
To evaluate the function, radiographic results and implant survival in patients younger than 21 years at the time of operation and with at least a 10-year follow-up, we reviewed the course of young adults who underwent total hip arthroplasty at McGill University Health Centre.
Patients and methods
Twelve patients (16 hips) met the criteria for inclusion in this study. They ranged in age from 10–20 years (median 16.5 yr). One patient (1 hip) died 5 years after the index surgery and was excluded from the study. Functional results were measured by the Harris hip score, and radiographs of surviving implants were assessed for radiolucencies, osteolysis and eccentric polyethylene wear.
Results
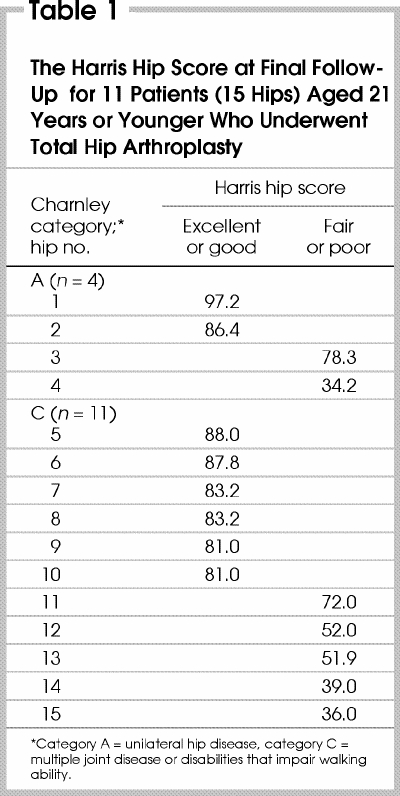
Eleven arthroplasties were cementless, 2 were hybrid and 2 were cemented. At follow-up ranging from 10 to 25 years (mean 13.6 yr), the Harris hip score ranged from 34.2–97.2 (mean 64.5). Four (26%) acetabular components were revised and (at the time of writing) 1 required revision. Only 1 (7%) femoral stem was revised. Radiographically, there was a high prevalence of eccentric polyethylene wear, but none of the surviving implants were found to be loose. Overall, 67% (10 of 15) of the total hip arthroplasties continued to function well at a mean of 13.6 years postoperatively.
Conclusions
Total hip arthroplasty remains a reasonable option in adolescence and early adulthood in selected patients with severe debility from multiple joint disease. Polyethylene wear is a particularly significant problem in this group of active young people.
Abstract
Introduction
En vue d'évaluer la fonction, les résultats radiographiques et la survie de l'implant chez des patients qui avaient moins de 21 ans au moment de la chirurgie et qui se sont prêtés à un suivi d'au moins 10 ans, nous avons examiné l'évolution de jeunes adultes ayant subi une arthroplastie totale de la hanche au Centre de santé de l'Université McGill.
Patients et méthodes
Douze patients (16 hanches) satisfaisaient aux critères d'inclusion de l'étude. Leur âge s'échelonnait de 10 à 20 ans (médiane, 16,5 ans). Un patient (1 hanche), qui est décédé cinq ans après la première chirurgie, a été exclu de l'étude. On a mesuré les résultats fonctionnels au moyen du score de Harris pour la hanche et on a procédé à une évaluation des radiographies des implants fonctionnels en s'attachant aux radiotransparences, à l'ostéolyse et à l'usure excentrique du polyéthylène.
Résultats
On comptait 11 arthroplasties sans ciment, 2 arthroplasties hybrides et 2 arthroplasties avec ciment. Après un suivi de 10 à 25 ans (moyenne, 13,6 ans), le score de Harris pour la hanche était de 34,2 à 97,2 (moyenne, 64,5). Quatre (26 %) composants cotyloïdiens ont été examinés et (au moment d'aller sous presse) l'un d'eux devait faire l'objet d'une révision chirurgicale. Seulement une tige fémorale (7 %) a fait l'objet d'une révision. Sur le plan radiographique, bien que la prévalence d'usure excentrique du polyéthylène soit élevée, on n'a pas observé de laxité à l'examen des implants fonctionnels. Dans l'ensemble, 67 % des arthroplasties totales de la hanche (10 des 15) fonctionnaient toujours bien après un recul postopératoire moyen de 13,6 ans.
Conclusions
L'arthroplastie totale de la hanche demeure une option raisonnable chez certains adolescents et jeunes adultes qui souffrent d'une grave incapacité découlant d'une maladie touchant de multiples articulations. L'usure du polyéthylène est un problème particulièrement important dans ce groupe de jeunes actifs.
The effect of hip joint disease, especially when it affects multiple other joints, is known to have a greater impact on mobility than disease of joints other than the hip in the lower extremity.1 The benefits of regaining mobility in young patients can have a tremendous impact on their social and personal development in this particularly important phase of life.
In adolescents and young adults, the indications for total hip arthroplasty (THA) are limited. Most commonly it is reserved for patients who are significantly debilitated by systemic disease like juvenile rheumatoid arthritis or who have multiple joint involvement.
Numerous problems may be encountered when performing THA in this patient group. Poor bone stock secondary to systemic disease or medications, as well as osseous deformities can render the procedure technically difficult. Postoperatively, poor compliance with activity restriction in these young patients makes early loosening a significant problem. Nevertheless, recent encouraging long-term results in older patients and improvements in surgical technique, implant materials and prosthetic design have broadened the indications for THA in young people.2
We undertook a study to evaluate the function, radiographic results and implant survival in patients younger than 21 years old at the time of their THA, who had at least a 10-year follow-up.
Patients and methods
All primary THAs performed by the senior authors (C.E.B. and F.F.) between 1975 and 1990 were reviewed. Twelve patients (8 female, 4 male, 16 hips) were younger than 21 years at the time of surgery. They ranged in age from 10–20 years (mean 16.5 yr).
One patient with Down's syndrome died of respiratory complications after a revision THA, 5 years after the primary procedure, and was excluded, leaving 15 hips for the study. Clinical examination and a Harris hip score3 was obtained on 9 patients (12 hips); in 2 patients (3 hips) a Harris hip score was obtained by telephone interview. Radiographic analysis was carried out on 14 of 15 hips (1 patient refused radiography, but a Harris hip score was obtained). Follow-up ranged from 10–25 years (mean 13.6 yr). Radiographs of surviving implants were studied for radiolucencies, osteolysis, eccentric polyethylene wear and loosening. Areas of radiolucency and osteolysis were assessed according to the zones described by Gruen and associates4 and those described by Delee and Charnley.5 Polyethylene wear was estimated using the technique described by Charnley and Cupic,6 where the width of the narrowest part of the socket in the weight- bearing area was subtracted from the width of the widest part in the non-weight-bearing area and the difference halved. Definite loosening was determined by evidence of migration as described by Harris and associates.7,8 Probable loosening was applied in the presence of a continuous radiolucent line at the bone–cement interface surrounding the entire mantle. In cementless implants, the femoral component was determined to be loose if it met the criteria for unstable fibrous fixation as described by Engh and associates.9 Loosening of a cementless acetabular cup was diagnosed if there was migration of the cup (when serial radiographs were available) or presence of a continuous radiolucent line wider than 2 mm on both anteroposterior and lateral radiographs. The implant was considered to have failed if it required revision or was loose radiographically.
Four patients (4 hips) were classified in Charnley category A (unilateral hip disease) and 7 patients (11 hips) in Charnley category C (multiple joint disease or other disabilities impairing walking ability).10 There were no patients in Charnley category B (bilateral hip disease). Of the 4 hips in Charnley category A, the diagnosis was avascular necrosis in 3 and developmental dysplasia of the hip in 1. In the 11 hips in Charnley category C, 9 were affected by juvenile rheumatoid arthritis and 2 by multiple epiphyseal dysplasia.
Eleven of the THAs were performed using a cementless technique with AML components (DePuy, Warsaw, Ind.) in 7 hips, HG components (Zimmer, Warsaw, Ind.) in 3 hips, and PCA components (Howmedica, Rutherford, NJ) in 1 hip. Two arthroplasties were hybrids, with HG cups and Harris precoat stems (Zimmer), and 2 were cemented: 1 with HD-2 (Howmedica) and the other with Aufranc-Turner (Howmedica) components. The patient who died after revision had a cemented cup with a cementless AML stem.
Results
Clinical results
Preoperatively, 6 of 11 patients (55%) could walk 2 blocks or less or could only walk indoors (limited community ambulators) and 5 (45%) were nonambulatory. All nonambulatory patients had multiple joint involvement (Charnley category C). At the final follow-up, 9 patients (82%) were able to walk 3 blocks or more (community ambulators) and 2 (18%) were limited community ambulators. The latter were not limited by their hips but by multiple other joint problems. One patient was waiting for bilateral THAs, and the other had multiple epiphyseal dysplasia and was limited by severe bilateral knee and ankle pain.
Preoperatively, all patients required aids to walk. Five patients (45%) were wheelchair bound, 4 (36%) used a cane at all times, and 2 patients (18%) used a walker. At the final follow-up, 6 patients (54%) did not need any aids for walking, 2 (18%) used a cane at all times, 2 (18%) used a walker and 1 (9%) used a cane for long walks.
The mean Harris hip score was 64.5 (range from 34.2–97.2) at an average follow-up of 13.6 years (Table 1). Only 8 (54%) hips had an excellent or good result and the remaining 7 (46%) hips had a fair or poor score. However, 12 of 15 (80%) hips had no or only slight and occasional pain. Two hips in the Charnley A category had an excellent or good Harris Hip Score and 2 hips had a fair or poor score. Only 1 of these hips had more than slight or occasional hip pain. This patient had a failed acetabular component and at the time of writing was awaiting revision surgery. Six (55%) of 11 hips in the Charnley C category had an excellent or good score and 5 (45%) had a fair or poor score. Only 2 of these hips were mildly painful. All hips of patients of the Charnley category C with a fair or poor score, scored especially low in the functional component of the Harris Hip Score questionnaire because of knee or ankle pain. None of the unrevised hips of the Charnley C category were loose at the most recent follow-up.
Table 1
Overall, 9 (82%) of 11 patients reported increased function, all patients stated they had less pain and 9 were satisfied with the result of their THA.
Radiographic results
Follow-up radiographs were available in 10 of 11 hips in which the acetabular component had survived. One cup will require revision because of severe pelvic osteolysis and symptomatic failure. None of the other surviving acetabular implants showed radiologic evidence of loosening. Seven acetabular cups had osteolytic areas in 2 zones or less (Fig. 1). One cup had a noncontinuous radiolucent line (in a single zone). Eccentric polyethylene wear was noted in 9 of the 10 remaining implants.
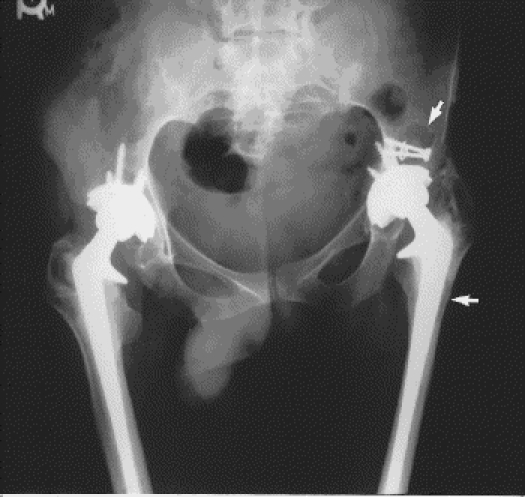
FIG. 1. Total hip arthroplasty 11 years after the index surgery. Arrows show areas of osteolysis. Note the eccentric polyethylene wear on the left side.
Thirteen (2 cemented, 11 cementless) of 14 hips in which the femoral component survived were available for follow-up radiologic examination. Six (54%) of the 11 cementless hips were not associated with any radiolucencies or areas of osteolysis (Fig. 2). One cementless hip showed continuous parallel radiolucent lines around the implant and was therefore felt to have a stable fibrous interface; the 10 remaining cementless femoral stems displayed stable bony ingrowth. The 2 cemented hips had noncontinuous radiolucencies at the cement–bone interface in 3 or fewer Gruen zones. Areas of osteolysis were noted in a single zone of 1 cemented femoral component (Fig. 1). None of the surviving femoral implants were found radiographically to be loose.

FIG. 2. Cementless total hip arthroplasty 14 years after the index surgery.
Complications
There were 2 hip dislocations, both treated successfully by nonoperative management. One hybrid THA was complicated by an intraoperative longitudinal fracture of the femoral shaft, which healed with conservative measures without further consequences. On the same side, this THA was also complicated by a dropfoot from a sciatic nerve injury attributed to lengthening for correction of an acetabular protrusio. This was eventually treated with a triple arthrodesis.
Revisions
At the most recent follow-up, 4 (27%) of 15 acetabular components were revised. Three of these were in the Charnley A category (1 cementless, 2 cemented cups) and the other in Charnley C category (cementless cup). The patient with severe osteolysis and symptomatic failure (Charnley A, cementless cup) was scheduled for an acetabular revision. Only 1 (7%) of 15 femoral stems was revised. This was a Charnley A category hip with a cemented femoral stem. All revisions performed were required because of aseptic loosening.
Discussion
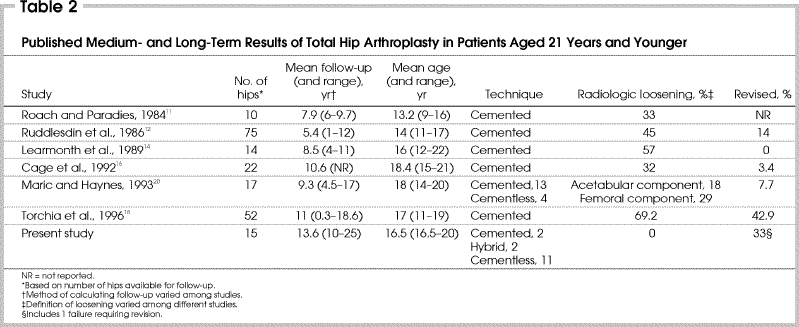
There are few reports on the long-term results of THA performed in adolescents or very young adults. In our study, at a mean follow-up of 13.6 years, 67% (10 of 15) of the protheses continued to function well; 4 hips had been revised and at the time of writing 1 hip required revision; overall, 67% of acetabular components and 93% of the femoral components had not failed; and 1 of the 2 cemented acetabular components and 10 (77%) 13 noncemented acetabular components were still functioning well. On the femoral side, 3 of 4 (75%) of cemented components and all of the cementless femoral components survived, and 10 (90%) of 11 prostheses in Charnley category C patients did not loosen, whereas the prostheses in all of the 4 Charnley category A patients were revised or required revision.
Roach and Paradies11 reported on 10 cemented THAs in patients ranging in age from 9 to 16 years. Thirty-three percent of the cups but no stems required revision at an average 13.2-year follow-up. Ruddlesdin and colleagues12 evaluated the results of 75 hips in young patients who received a cemented total hip replacement between the ages of 11 and 17 years (mean 14 yr). At a mean follow-up of 5.4 years, 45% of the prostheses were radiographically loose, and 14% had been revised. Halley and Wroblewski13 reviewed 49 cemented THAs in patients under the age of 30 years with a 10-year mean follow-up. Radiologic loosening was seen in 47% of cups and 20.4% of stems, whereas 14.3% of the acetabula and 4% of the femora were revised. Learmonth and associates14 reported on 14 cemented THAs in patients with an average age of 16 years. At a mean follow-up of 8.5 years, 8 (57%) hips showed radiologic loosening but none had been revised. Witt and colleagues15 reviewed 96 hips with cemented THAs in patients between the ages of 11 and 26 years. At a mean 9.5-year follow-up, 41 hips showed radiologic loosening and 34 were revised. Cage and associates16 published a review of 29 cemented THAs in patients who were 21 years old or younger. At an average 11-year follow-up, 7 (32%) of the 22 hips that were available for evaluation showed radiologic loosening and 1 hip required revision. Chmell and associates17 reviewed the results of 55 cemented arthroplasties in 33 patients under the age of 30 years and with a diagnosis of rheumatoid arthritis. The 15-year survival rate for the femoral component with revision or radiographic loosening as an end point was 85%. The 15-year survival rate for the acetabular components with revision as an end point was 70% and with revision or radiographic loosening as an end point 61%. Torchia and colleagues18 reported on 52 hips in patients who were younger than 20 years at the time of their cemented THA. They determined that the probability of radiologic loosening after 15 years was 60% for the acetabular component and 20% for the femoral component. In the German literature, Porsch and Siegel19 reported on 27 cemented hip arthroplasties for developmental dysplasia of the hip in 18 patients under the age of 20 years. The overall revision rate at an average 10 years and 8 months was 41% with acetabular loosening occurring 3 times as often as femoral loosening. These findings in the English literature are summarized in Table 2.11,12,14,16,18,20
Table 2
At the time of writing, there were no published long-term results (more than 10 years) of cementless THA in the under-21-years age group. This is likely because most THAs were performed on young patients with juvenile rheumatoid arthritis and other systemic disease in whom poor bone stock has convinced many surgeons to perform cemented or hybrid THAs. Maric and Haynes20 reported on 17 hips with an average follow-up of 9.3 years in patients with an average age of 18 years. Excellent results were noted in their 4 cementless THAs, whereas 5 of their 13 cemented components were definitely loose. However, the average follow-up of the noncemented hips was 5 years compared with 11 years for the cemented hips.
An important concern in all of our patients was the high prevalence (90% of surviving acetabular cups) of eccentric polyethylene wear. The relationship of acetabular wear to osteolysis and loosening in THA is well established. Sochart21 showed that the prevalence of osteolysis and acetabular and femoral component loosening and revision rose significantly with increasing wear. Moreover, Kobayashi and associates22 in a comparative study of THA between younger and older patients showed greater radiologic evidence of loosening of the acetabular cup (including revision cases) in younger (29.1%) than in older patients (14.3%) at an average follow-up of 14 years. The revision rate for aseptic loosening of the socket was higher in the younger (20%) than the older group (4%). The loosening rates for the femoral prostheses were similar for both groups. Perhaps alternative bearing surfaces, such as metal-on-metal, ceramic-on-ceramic or cross-linked polyethylene will reduce the problems related to wear and the associated high rates of loosening and revision in younger more active people. Nevertheless, careful selection of patients is important in considering THA in this age group. Torchia and colleagues18 reported that favourable candidates for THA during adolescence are patients who have a more sedentary lifestyle because of some other musculoskeletal disease, who have bilateral hip involvement not treatable by osteotomy and weigh less than 60 kg. Less favourable candidates are those who are high-demand patients and typically have unilateral hip disease, do not have any other form of musculoskeletal disease, often have a history of post-traumatic avascular necrosis with multiple previous operative procedures and weigh more than 60 kg. This is well reflected in the results of our study, which reveal a significant discrepancy in the success of total hip replacement between patients in Charnley category A versus category C. Therefore, these risk factors should be taken into account in the decision-making process when choosing treatment options in adolescents and very young patients with debilitating hip disease.
Conclusions
THA remains a reasonable option when arthrodesis or osteotomy are not possible in adolescents and in very young adults who are debilitated by hip disease. This is particularly true with bilateral or multiple joint involvement. Cementless THA may be a good choice despite the common problem of poor bone stock in this age group. THA with alternative bearing surfaces also may provide improved results in the future for patients in this age group.
Competing interests: None declared.
Correspondence to: Dr. François Fassier, Division of Pediatric Orthopedic Surgery, McGill University Health Centre, Montreal Children's Hospital, 2300 Tupper St., Montréal QC H3H 1P3; fax 514 862-8664; francois.fassier@muhc.mcgill.ca
Accepted for publication Mar. 5, 2003.
References
- 1.Isdale IC. Hip disease in patients with juvenile rheumatoid arthritis. Ann Rheum Dis 1970;29:603-8. [DOI] [PMC free article] [PubMed]
- 2.Callaghan JJ, Albright JC, Goetz DD, Olejniczak JP, Johnston RC. Charnley total hip arthroplasty with cement. Minimum twenty-five-year follow-up. J Bone Joint Surg Am 2000;82:487-97. [DOI] [PubMed]
- 3.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 1969;51:737-55. [PubMed]
- 4.Gruen TA, McNeice GM, Amstutz HC. “Modes of failure” of cemented stem-type femoral components. A radiographic analysis of loosening. Clin Orthop 1979;141:17-27. [PubMed]
- 5.Delee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop 1976;121:20-32. [PubMed]
- 6.Charnley J, Cupic Z. Nine and ten year results of low-friction arthroplasty of the hip. Clin Orthop 1973;95:9-25. [PubMed]
- 7.Harris WH, McCarthy JC Jr, O'Neil DA. Femoral component loosening using contemporary techniques of femoral cement fixation. J Bone Joint Surg Am 1982;64:1063-7. [PubMed]
- 8.Johnston RC, Fitzgerald RH Jr, Harris WH, Poss R, Müller ME, Sledge CB. Clinical and radiological evaluation of total hip replacement. A standard system of terminology for reporting results. J Bone Joint Surg Am 1990;72:161-8. [PubMed]
- 9.Engh CA, Glassman AH, Suthers KE. The case for porous coated hip implants. The femoral side. Clin Orthop 1990;261:63-81. [PubMed]
- 10.Charnley J. The long term results of low friction arthroplasty of the hip performed as primary intervention. J Bone Joint Surg Br 1972;54:61-76. [PubMed]
- 11.Roach JW, Paradies LH. Total hip arthroplasty performed during adolescence. J Pediatr Orthop 1984;4:418-21. [DOI] [PubMed]
- 12.Ruddlesdin C, Ansell BM, Arden GP, Swann M. Total hip replacement in children with juvenile chronic arthritis. J Bone Joint Surg Br 1986;68:218-22. [DOI] [PubMed]
- 13.Halley DK, Wroblewski BM. Long term results of low friction arthroplasty in patients 30 years or younger. Clin Orthop 1986;211:43-50. [PubMed]
- 14.Learmonth ID, Heywood AW, Kaye J, Dall D. Radiological loosening after cemented hip replacement for juvenile chronic arthritis. J Bone Joint Surg Br 1989;69:45-55. [DOI] [PubMed]
- 15.Witt JD, Swann M, Ansell BM. Total hip replacement for juvenile chronic arthritis. J Bone Joint Surg Br 1991;73:770-3. [DOI] [PubMed]
- 16.Cage DJ, Granberry WM, Tullos HS. Long term results of total arthroplasty in adolescents with debilitating polyarthropathy. Clin Orthop 1992;283:156-62. [PubMed]
- 17.Chmell MJ, Scott RD, Thomas WH, Sledge CB. Total hip arthroplasty with cement for juvenile rheumatoid arthritis. Results at a minimum ten years in patients less than thirty years old. J Bone Joint Surg Am 1997;79:44-52. [DOI] [PubMed]
- 18.Torchia ME, Klassen RA, Bianco AJ. Total hip arthroplasty with cement in patients less than twenty years old. Long-term results. J Bone Joint Surg Am 1996;78:995-1003. [DOI] [PubMed]
- 19.Porsch M, Siegel A. [Artificial hip replacement in young patients with dysplasia — long-term outcome after 10 years] [review]. Z Orthop Ihre Grenzgeb 1998;136:548-53. [DOI] [PubMed]
- 20.Maric Z, Haynes RJ. Total hip arthroplasty in juvenile rheumatoid arthritis. Clin Orthop 1993;290:197-9. [PubMed]
- 21.Sochart DH. Relationship of acetabular wear to osteolysis and loosening in total hip arthroplasty. Clin Orthop 1999;363:135-50. [PubMed]
- 22.Kobayashi S, Eftekhar NS, Terayama K, Joshi RP. Comparative study of total hip arthroplasty between younger and older patients. Clin Orthop 1997;339:140-51. [DOI] [PubMed]


