Abstract
Introduction
There is controversy as to whether continuous passive motion (CPM) after total knee arthroplasty (TKA), which is the standard treatment, confers significant benefit with respect to outcome. The primary purpose of this study was to determine if CPM or slider-board (SB) therapy, used as adjuncts to standardized exercises (SEs) during the acute-care hospital stay, resulted in a reduced total length of hospitalization and post-discharge rehabilitation in patients who underwent primary TKA.
Methods
We carried out a randomized, clinical trial on 120 patients who received a TKA at the University of Alberta Hospital, Edmonton, a tertiary care institution. The study horizon began at the point of discharge from the hospital and continued up to 6 months after operation. Postoperatively, patients (40 in each group) received CPM and SEs, SB therapy and SEs or SEs alone while in the tertiary centre. Health service use was compared using transfer institution length of stay (LOS), post-discharge rehabilitation, readmission and complication rates and their associated costs.
Results
There were no differences in health service use or costs among the 3 groups over the 6-month study. The rates of postoperative complications and readmissions also were similar among the groups. Increased health service use was associated with knee flexion that was less than 60° at discharge, but similar proportions of patients with poor knee range of movement (ROM) at discharge were found in each group.
Conclusions
This finding suggests that adjunctive ROM therapy, as used in this study, does not reduce health service use. Further research is required to determine if adjunctive ROM therapy after discharge from the surgical hospital decreases health service utilization in those patients who have poor knee ROM at the time of discharge.
Abstract
Introduction
La question de savoir si les mouvements passifs continus (MPC) après une arthroplastie totale du genou (ATG), qui constituent le traitement standard, entraÎnent des avantages importants sur le plan des résultats soulève la controverse. Cette étude visait principalement à déterminer si les traitements par MPC ou tapis de glissements latéraux (TGL), utilisés comme ajouts aux exercices normalisés (EN) pendant le séjour à l'hôpital de soins actifs, ont réduit la durée totale de l'hospitalisation et de la réadaptation après le congé chez les patients qui ont subi une ATG de première intervention.
Méthodes
Nous avons procédé à un essai clinique randomisé portant sur 120 patients ayant subi une ATG à l'Hôpital de l'Université de l'Alberta à Edmonton, établissement de soins tertiaires. L'étude a commencé au moment où le sujet a reçu son congé de l'hôpital et a duré jusqu'à six moins après l'intervention. Après l'intervention, les patients (40 de chaque groupe) ont fait des MPC et des EN, ont suivi une thérapie au TGL et aux EN, ou ont fait des EN seulement pendant leur séjour au centre de soins tertiaires. On a comparé l'utilisation des services de santé en se fondant sur la durée du séjour dans l'établissement de transfert, la réadaptation après le congé, les taux de réadmission et de complications et leurs coûts connexes.
Résultats
On n'a constaté aucune différence au niveau de l'utilisation des services de santé ou des coûts entre les trois groupes pendant l'étude de six mois. Les taux de complications postopératoires et de réadmission se ressemblaient aussi entre les groupes. On a établi un lien entre l'utilisation accrue des services de santé et la flexion du genou qui n'atteignait pas 60 degrés au moment du congé, mais on a constaté dans chaque groupe des pourcentages semblables de patients dont l'amplitude du mouvement (ADM) au genou était médiocre.
Conclusions
Ces résultats indiquent qu'une thérapie d'appoint pour améliorer l'ADM, comme celle qu'on a utilisée dans le contexte de la présente étude, ne réduit pas le recours aux services de santé. Des recherches plus poussées s'imposent pour déterminer si une thérapie d'appoint pour améliorer l'ADM après le congé de l'hôpital chirurgical réduit le recours aux services de santé par les patients dont l'ADM au genou est médiocre au moment du congé.
Continuous passive motion (CPM) is the standard treatment after knee arthroplasty in many institutions. It is controversial, however, as to whether significant benefits can be ascribed to its use after total knee arthroplasty (TKA). Several studies have reported that 6 months after TKA, patients who received CPM immediately postoperatively had the same clinical outcome as patients who did not receive CPM.1,2,3,4,5 Some have suggested, however, that use of health services is reduced because of earlier return of knee range of motion (ROM), fewer manipulations under anesthesia and a reduction in the need for early pain medication when CPM is utilized in the initial postoperative period.6,7,8,9,10 Little quantitative evidence exists to support this premise. Thus, it is unclear whether the use of adjunctive ROM therapy postoperatively ultimately affects knee ROM and the ensuing use of health services during the patient's recovery from primary TKA.
Because we believed that ROM therapy in addition to physical therapy would be beneficial to the patient's recovery but did not want the costs incurred through the use of CPM therapy, an alternative form of ROM mobilization was introduced at our site in 1995. The slider board (SB) is a simple device, consisting of a movable heel-cup fixed to a low friction sliding mechanism, that allows the patient to actively flex and extend the knee with minimal active quadriceps and hamstring movement. This device can be purchased for Can$50–$200 and can be set up independently by the patient or with minimal nursing assistance. The CPM machines for knee joints, conversely, vary in initial purchase cost between Can$2500 and Can$9700 and require nursing and technical support to set up and maintain.
It was not known if either of these devices, used during the acute care hospital stay, would facilitate a more rapid functional recovery than the standardized daily physical therapy sessions alone. Thus, patients were randomly allocated to 1 of 3 groups to receive CPM as an adjunct to standardized exercise (SE), SB therapy as an adjunct to SE, or SE alone. The functional outcomes and health- related quality of life among the 3 groups have been reported previously.11 The purpose of this paper is to compare health services utilization and the associated costs among the 3 groups of patients after discharge from the acute care hospital. To assess for potential confounding, we verified that the acute care hospital length of stay and the amount of pain medication used as measured by the Medication Quantification Scale12 were similar in all 3 groups, as predicated by the hospital caremap, and that the complication rate also did not differ among groups during the acute care hospital stay. Finally, we examined the relationship between knee ROM regained at the time of hospital discharge and the amount and cost of health services used after discharge from the acute care hospital.
We hypothesized that patients in the SE group would be more likely to be transferred for further rehabilitation, require longer secondary hospitalization and use more rehabilitation services after discharge than the ROM intervention groups. We did not anticipate finding a difference in the complication or readmission rates among the 3 groups nor did we expect to see a difference between the 2 ROM groups in any of the variables measured.
Methods
Design
This randomized, controlled clinical trial was performed at a single tertiary care hospital that utilized a standardized clinical pathway for treatment of patients who underwent TKA. Because pain medication use and length of stay was predicated on the use of the pathway, the study horizon for health service use and costing began at the time of discharge from the tertiary care hospital.
Subjects
One hundred and twenty subjects who were scheduled for primary TKA between June 5, 1997, and July 17, 1998, were recruited consecutively from 12 surgeons' practices. Subjects were eligible for the study if they would be undergoing primary TKA, were willing to return for the required visits and gave informed consent. Subjects receiving a unicondylar knee replacement were ineligible for the trial.
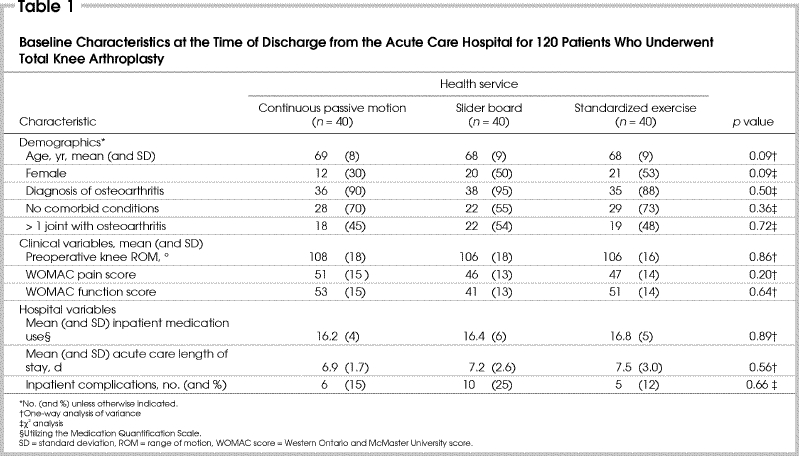
Earlier findings determined that there were no differences in knee ROM, pain and function assessed at discharge from hospital and at 3 and 6 months after surgery among these 3 randomly allocated intervention groups.11 Patients were assessed at all intervals by a physical therapist blinded to group allocation. All 3 groups were similar in baseline characteristics including demographic, clinical and acute hospital care variables (Table 1). The detailed study methodology has been reported elsewhere.11 Subsets were randomized using consecutively numbered, sealed, opaque envolopes following the patients' enrolement visit.
Table 1
Intervention
After TKA, the mean (± standard deviation) length of stay (LOS) in the acute care hospital was 7(2) days as per the clinical pathway and then, barring complications, patients were discharged home or transferred to another facility for further rehabilitation.
Postoperative management
All patients followed the institution's standardized clinical pathway for TKA that included medical, pharmaceutical and rehabilitation care during the acute care hospital stay. The goal of the clinical pathway is to prepare patients for discharge from the hospital 5–7 days after operation. Early mobility is encouraged. Immediately after the operation, a Jones bandage, which maintained the lower extremity in extension, was applied to the knee and remained in situ until the second postoperative day when the Hemovac drain was removed from the knee joint. Patients were allowed to sit during the first postoperative day, and they progressed to walking short distances on the second postoperative day.
Daily SE sessions with the physical therapist, typically 30 minutes per session, began on the third postoperative day for all 120 patients. They all used the SB for one 10-minute session during their SE period. For the CPM treatment group, CPM began on the second postoperative day with the patients instructed to receive three 2-hour CPM sessions, each day until discharge. The starting range was 0°–30° and was progressed daily as tolerated. For the SB treatment group, the use of the SB began on the second postoperative day with the patients asked to perform a minimum of two 10-minute sessions daily independently, in addition to the SE session. Active knee flexion and extension in both sitting and lying positions were performed independently to patient tolerance, both at the therapy session and during the 2 patient-directed sessions.
Use of health services
Chart reviews were completed by trained research assistants to record inpatient use of pain medication, place of discharge, LOS at acute care and transfer institutions, complications during the hospital stay and readmissions over the 6-month study period. Data were also collected from the patients at each follow-up visit to ascertain whether they had been admitted to any other hospital or had any complications after discharge home during the 6 months after operation.
Data on the use and cost of institutional care and rehabilitation, for the 6 months after operation, were obtained from the regional health authorities' (RHAs) administrative database. Institutional services in the analysis included transfers to a rehabilitation subacute care program within a continuing care facility, a rehabilitation hospital or a rural acute care hospital immediately after the initial surgical inpatient stay. Rehabilitation services included physical and occupational therapy related to direct care or case management in both home care (HC) and outpatient therapy (OPT) programs. Readmissions to acute care hospitals during the study period were also included.
Knee ROM is one of the criteria used in determining when a patient may be discharged home. If a patient is independent in gait and transfers, but has poor knee ROM, the patient may still be discharged home with physical therapy. All patients discharged from the hospital to the community had physical therapy appointments arranged with either HC or community rehabilitation programs before discharge regardless of knee ROM. Patients were expected to attend these programs until their knee ROM exceeded 90°. Those patients who did not attain 90° ROM were instructed to return to their surgeon for further consultation.
The place of discharge is primarily indicated by the patient's ability to ambulate and transfer independently. Patients who could manage activities of daily living independently were discharged home 7 days postoperatively. Those who still required assistance were transferred to other facilities for further rehabilitation.
Health service costing
For each HC and OPT service event (visit), standard 1997/98 unit costs were used to value services. The costs of institutional care stays were valued by applying a standard 1997/98 per diem cost to the length of hospital stay for each admission during the follow-up period. The per diem cost of the rehabilitation subacute program was used as the standard for all transferred cases. For readmission cases, the average per diem cost of the 3 hospitals that readmitted study patients was used. All costs were valued in Canadian dollars. Standard unit and per diem costs were used to avoid the confounding effects of cost variation among programs and institutions. Since all resources were valued using 1997/98 unit and per diem costs, adjustment for price changes over the study period was not required.
As there was no difference in the clinical outcome or complication rates among the 3 groups at 6 months, a cost minimization analysis to determine the most economic intervention was completed on the rehabilitation and institutional costs (excluding the initial surgical stay) for 6 months after the operation.
Analysis
Descriptive statistics were performed on all variables. χ2 tests were used for analyses of categorical data, and a one-way analysis of variance (ANOVA) was used for continuous data to determine differences among the 3 treatment groups. All analyses were performed on an “intent-to-treat” basis, that is, all subjects were analyzed in their assigned group. All statistical tests were 2-tailed at a level of significance of α = 0.05. Statistical analyses were performed using the SPSS software version 10.05.
The perspective of the cost minimization analysis was that of the RHAs, which are both a third party payer and a provider. The standard per diem costs used to value the transfer and readmission institutional stays were the only assumptions that may have had a significant impact on the overall results. Therefore, a sensitivity analysis was performed using an alternative set of per diem hospital costs. For transfer and readmission cases, actual 1997/98 costs of the subacute care program or rehabilitation hospital, and the 3 hospitals that readmitted study patients were used as for the previous analysis. For the rural hospitals, however, the 1997/98 average per diem rate of all rural hospitals utilized was applied in the sensitivity analysis.
As health service use was a secondary question of this study, the power analysis was based upon the knee ROM. The study was powered to determine a difference of 5° of knee ROM among the 3 intervention groups (β = 0.20; effect size = 0.3).11 The mean knee ROM among the 3 groups at all assessment intervals did not differ more than 3°, thus we were unable to distinguish any ROM differences among the groups. Three degrees of knee ROM cannot be considered clinically important in terms of altering function. To achieve statistical significance with these differences among groups, a very large sample size would have been required, and the results would likely not be clinically meaningful.
Results
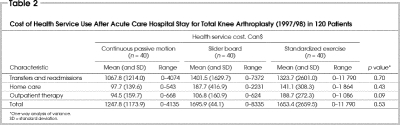
Cost of health service use after discharge from the acute care hospital
Differences in the average cost of health services use among the study groups were not significant (Table 2). All patients are included in this analysis regardless of whether they were transferred to another hospital or received any postdischarge rehabilitation. Two patients in the total cost analysis were deemed outliers (defined as a value greater than 3 standard deviations from the population mean). Both of these patients had complicated postoperative courses unrelated to their knee ROM and are included in the data in Table 2. As the results are not significantly different among the groups with the outlying values included, and the CPM group reported the lowest costs, exclusion of the patients with outlying values would cause the means among groups to become more, not less, similar, so we kept these 2 patients in the analyses to represent the complete data obtained for the study cohort.
Table 2
The institutional costs include both the transfer LOS as well as the readmissions. Because there were only 6 readmissions (1 CPM, 2 SE, 3 SB) over the entire study period, it was not feasible to analyze their costs separately. Patients were readmitted either for infection, including cellulitis (n = 3) or manipulation (n = 3). All of the patients who underwent manipulation had knee ROM greater than 100° preoperatively (range 103°–132°).
The sensitivity analysis showed no differences, by one-way ANOVA, among the 3 groups when the actual per diem costs from the rural institutions were used in place of the subacute per diem costs (p = 0.89).
Transfer institution use
Patients discharged directly home accounted for 55% (22 patients) of the SE group, 48% (19 patients) of the CPM group and 40% (16 patients) of the SB group. No differences were seen among groups for those patients transferred home and patients transferred to another institution (p = 0.41) among the 3 groups as determined by a χ2 analysis. In addition, no differences were seen in the LOS at the transfer institution or for readmissions among the 3 groups (Table 3). Those who were transferred were more likely to be older (p = 0.006) or to have knee ROM less than 60° at the time of the transfer (p = 0.007).
Table 3
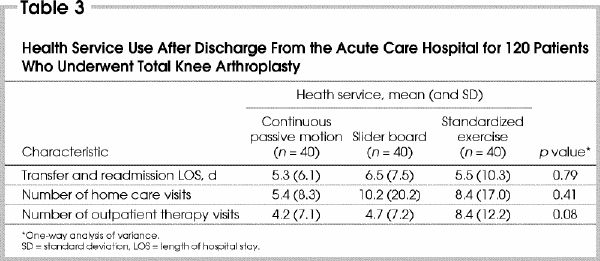
Rehabilitation after hospital discharge
Eighty-three patients (69.2%) received rehabilitation after their discharge from hospital, with no group differences seen (p = 0.45). Of these patients, 33 (40%) received HC only, 14 (17%) received OPT only and 36 (43%) received both types of hospital rehabilitation, which was similar across all 3 groups (p = 0.90). The number of visits was also similar across all 3 groups (Table 3).
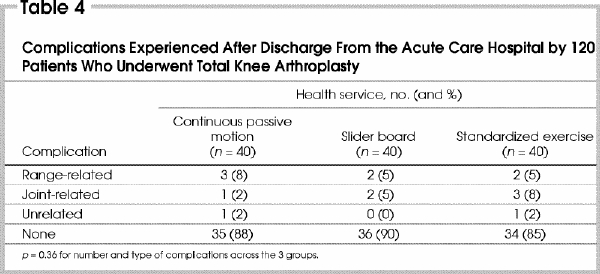
Complications
Complications after discharge from the acute care hospital are shown in Table 4. The number and type of complications were similar across all 3 groups (p = 0.36) with 105 patients (88%) having no complications. The range-related complications include 3 patients requiring manipulation, 1 in each group, and 4 patients with knee ROM less than 85°, who also had less than 90° flexion preoperatively. The joint-related complications included 5 infections and 1 deep venous thrombosis. Both superficial (wound) and deep infections were counted as complications. Four patients received antibiotic prophylaxis for cellulitis with only 1 patient (SE group) having a deep infection. Two patients had complications unrelated to either the joint or their surgery.
Table 4
Knee range of movement and health service utilization
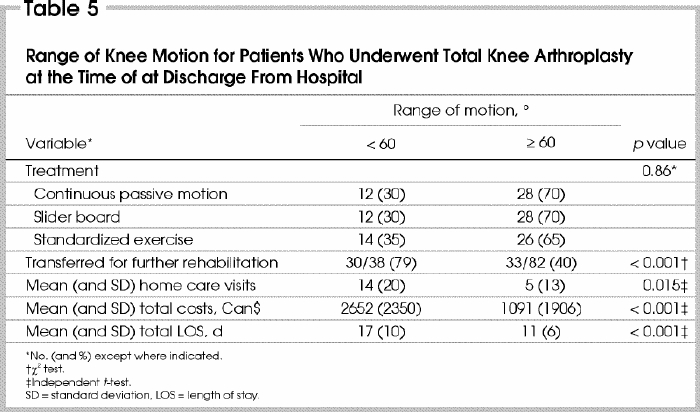
To examine the relationship between knee ROM and use of health services, the entire cohort was divided into 2 groups: those who had 60° of flexion at discharge from hospital and those who did not. The 60° of flexion was chosen because this is the knee ROM that the clinical pathway suggests patients should attain by 5 days after surgery. Table 5 demonstrates that patients with less than 60° knee flexion had a longer rehabilitation LOS and used significantly more health services than those who had attained this goal by the time of discharge from hospital. Moreover, patients who had less than 60° knee flexion were more likely to be transferred for further rehabilitation than those who had greater than 60°. Table 5 also shows that similar proportions of patients in these 2 ROM groups came from each of the 3 intervention groups (p = 0.67). Age, baseline pain, stiffness, function and preoperative knee ROM did not differ between those who attained knee flexion greater than 60° in the initial postoperative period and those who did not (p > 0.05).
Table 5
Discussion
No difference in the quantity or cost of health services was seen among the 3 treatment groups in the subacute recovery phase after a TKA. Although CPM does not appear to have a beneficial effect on the long-term results of knee ROM in patients undergoing primary TKA,1,2,3,4,5 few studies have reported the effect of adjunctive ROM therapy on the patient's short-term recovery, and the subsequent health service use during that period. Because our study included a large number of surgeons who all followed a postoperative clinical pathway, our results should be generalizable to other sites that follow a similar postoperative regimen. Our findings did not support the premise that the use of adjunctive ROM therapy reduced post-discharge health service use when daily, supervised SE sessions were utilized in the acute care hospital. Although the study's power was based on clinical measures, a power analysis using the cost data as presented here suggested that a minimum of 200 patients per group would have been required to attain statistical significance. As the cost data includes outlying values that increased the mean differences among groups, 200 patients per group is a conservative number of subjects required to distinguish cost differences among the different interventions. Use of such a large sample to attain significant differences would likely lack clinical importance, particularly in light of the similar clinical outcomes reported previously.11
Although we expected the 2 ROM interventions to have no impact on the LOS at the acute care facility, it was anticipated that the proportion of patients transferred, the LOS and thus the cost at the transfer institution would be greater for the SE group than for the 2 intervention groups. Instead, we found patients in each group had a very similar distribution of service use and cost at the transfer institutions regardless of postoperative intervention received. Patients who were transferred were more likely to be older or to have knee flexion less than 60°.
The utilization and cost of postdischarge rehabilitation services also did not vary among the 3 groups. We hypothesized that the 2 intervention groups would require less rehabilitation after discharge from hospital. Again, our study did not support this hypothesis. Although it appears that the CPM group had lower costs and fewer visits overall than the other 2 groups, the difference was not significant, so we cannot rule out the effect of chance. Within the other 2 treatment groups were 2 individuals who had complicated postoperative courses unrelated to the ROM therapy. Although we measured comorbidities and complications, we did not measure their severity and perhaps did not adequately assess their impact on the patient's recovery.
The short-term benefits of fewer manipulations and readmissions associated with the use of CPM as reported in previous studies were also not seen in this study.8,9 Each of our groups had 1 manipulation, suggesting that the use of additional ROM therapy did not affect manipulation rates when a standardized postoperative routine was followed. In general, readmissions for the entire cohort were low and were similarly distributed over the 3 treatment groups.
We did, however, observe a relationship between knee ROM and the amount of postoperative health services that were required after discharge. Recovery of knee ROM postoperatively was found to be an important factor in determining how long patients stayed in the rehabilitation institution and the amount of physical therapy or HC received.
It does not appear that the ROM interventions of CPM and SB therapy as delivered in our protocols affected how patients recovered their knee motion. Longer periods of use of either adjunctive motion therapies may have produced different results, but the early total mobilization regimen we used that demanded that the patient be up and out of bed as much as possible postoperatively precluded increased modality usage.
Recovery of knee ROM postoperatively, however, does affect health service use, and more research should be directed to assisting those patients who have difficulty regaining knee ROM. Adjunctive motion therapy in the form of SB therapy or the CPM for prolonged periods either in the surgical hospital or continued after discharge may have a beneficial effect for these patients. A previous study has shown that home use of the CPM machine was more cost- effective than community-based physical therapy.13 Moreover, when the number of support staff in a surgical hospital is adequate, adjunctive ROM therapy may also play a larger role than in our centre where daily physical therapy occurs after a TKA.
Conclusions
From the initial 0–6 months postoperatively, the 3 treatment groups showed a very similar pattern of health services use. Neither CPM nor the SB therapy decreased transfer LOS and health service use more than SE. With the additional costs associated with adjunctive ROM therapy, in particular with use of the CPM machine, use of these devices outside the daily SE sessions is not appropriate when a patient is following a normal postoperative course and clinical personnel are available to mobilize the patient. Because rate of recovery of knee ROM does affect health service use, more research is required to determine the role of ROM therapy in the acute and rehabilitation phases for those patients who are having difficulty regaining knee flexion.
Acknowledgments
This study received financial support from the Health Research Fund, a division of the Alberta Heritage Foundation for Medical Research. The authors would like to thank Lori N. Schaump for her administrative support, Karin E. Greaves for her assistance with data collection and Maria E Suarez-Almazor for her assistance in the study design.
Competing interests: None declared.
Correspondence to: Ms. Lauren A. Beaupre, 1F1.52 WMC7, 8440-112th St., Edmonton AB T6G 2B7; fax 780 407-7534; lbeaupre@ualberta.ca
Accepted for publication Oct. 8, 2002.
References
- 1.Chen B, Zimmerman JR, Soulen L, DeLisa JA. Continuous passive motion after total knee arthroplasty: a prospective study. Am J Phys Med Rehabil 2000;79:421-6. [DOI] [PubMed]
- 2.Chiarello CM, Gundersen L, O'Halloran T. The effect of continuous passive motion duration and increment on range of motion in total knee arthroplasty patients. J Orthop Sports Phys Ther 1997;25:119-27. [DOI] [PubMed]
- 3.Pope RO, Corcoran S, McCaul K, Howie DW. Continuous passive motion after primary total knee arthroplasty. Does it offer any benefits? J Bone Joint Surg Br 1997;79:914-7. [DOI] [PubMed]
- 4.Colwell CW, Morris BA. The influence of continuous passive motion on the results of total knee arthroplasty. Clin Orthop 1992;276:225-8. [PubMed]
- 5.Johnson DP. The effect of continuous passive motion on wound-healing and joint mobility after knee arthroplasty. J Bone Joint Surg Am 1990;72:421-6. [PubMed]
- 6.Lachiewicz PF. The role of continuous passive motion after total knee arthroplasty. Clin Orthop 2000;380:144-50. [DOI] [PubMed]
- 7.Ververeli PA, Sutton DC, Hearn SL, Booth RE, Hozack WJ, Rothman RR. Continuous passive motion after total knee arthroplasty. Analysis of cost and benefits. Clin Orthop 1995;321:208-15. [PubMed]
- 8.McInnes J, Larson MG, Daltroy LH, Brown T, Fossel AH, Eaton HM, et al. A controlled evaluation of continuous passive motion in patients undergoing total knee arthroplasty. JAMA 1992;268:1423-8. [DOI] [PubMed]
- 9.Romness DW, Rand JA. The role of continuous passive motion following total knee arthroplasty. Clin Orthop 1988;226:34-7. [PubMed]
- 10.Gose JC. Continuous passive motion in the postoperative treatment of patients with total knee replacement. A retrospective study. Phys Ther 1987;67:39-42. [DOI] [PubMed]
- 11.Beaupre LA, Davies DM, Jones CA, Cinats JG. Exercise combined with continuous passive motion or slider board therapy compared with exercise only: a randomized controlled trial of patients following total knee arthroplasty. Phys Ther 2001;81:1029-37. [PubMed]
- 12.Masters Steedman S, Middaugh SJ, Kee WJ, Carson DS, Harden RN, Miller MC. Chronic-pain medications: equivalence levels and method of quantifiying usage [review]. Clin J Pain 1992;8:204-14. [PubMed]
- 13.Worland RL, Arredondo J, Angles F, Lopez-Jimenez F, Jessup DE. Home continuous passive motion machine versus professional physical therapy following total knee replacement. J Arthroplasty 1998;13: 784-7. [DOI] [PubMed]