Wrong-side surgery is probably the most dramatic, visible and devastating of all surgical errors. It is arguably the error most feared by surgeons. Recently, there was a prominently profiled neurosurgical case that received a lot of publicity, perhaps more than it might have because it occurred in a highly renowned medical institution in the United States.1 In this paper I describe a case of a wrong-sided surgery as a platform to summarize the available literature with an emphasis on strategies to prevent such errors from harming patients.
Case report
A healthy 71-year-old man presented with a subacute history of confusion and right hemiparesis. Computed tomography showed a large, chronic subdural hematoma in the left frontal region (Fig. 1). The patient was placed on the after-hours operating room waiting list and was called for around 1 am. An experienced senior resident initiated the operation with a junior resident without notifying the neurosurgery staff. With the patient under neuroleptanalgesia supplemented with regional local anesthesia a frontal burr hole was drilled and the dura opened. When no subdural blood was found, the resident realized he had opened the wrong (i.e., right) side and proceed to do the operation on the correct (i.e., left) side. The operating-room charge nurse called the staff neurosurgeon to inform him of the error. When the staff neurosurgeon arrived at the hospital 15 minutes later, the patient was in the recovery room and the error was immediately and fully disclosed to the patent's family by the surgeon and the resident.

FIG. 1. Computed tomography scan demonstrating large, left frontal, isodense, chronic subdural hematoma (arrow).
The patient was noted to be deeply obtunded and hemiplegic on the right side; an urgent CT demonstrated a large acute hemorrhage into the left subdural space (i.e., the correct side) (Fig. 2). Urgent craniotomy on the left was performed to evacuate the clot. Postoperatively, the staff neurosurgeon had a long conversation with the family about the error and informed them that it would not likely have an impact on the patient's outcome. The complication was also discussed in detail. The patient's son specifically asked if the staff neurosurgeon was in the operating room at the time of the error. This question was answered honestly, and the nature of graded responsibility and delegation of responsibility within teaching hospitals was discussed. In a detailed discussion, the neurosurgeon, the senior resident and the junior resident dissected the possible causes of the error (and the complication) and considered potential methods of preventing such errors.
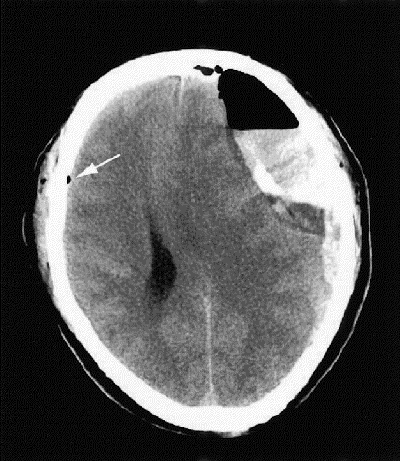
FIG. 2. Computed tomography scan 1 hour after creation of a burr hole on the wrong side and a burr hole made on the correct side to drain a left subdural hematoma. Blood and air are visible in the left subdural space. The arrow points to a residual drop of subdural air at the site of the wrong-sided (right) burr hole.
The patient recovered fully and 2 months after admission was neurologically intact and had a normal CT (Fig. 3). He was well 1 year later. At the time of this writing, neither the patient nor his family have initiated medicolegal action or made any formal complaint.
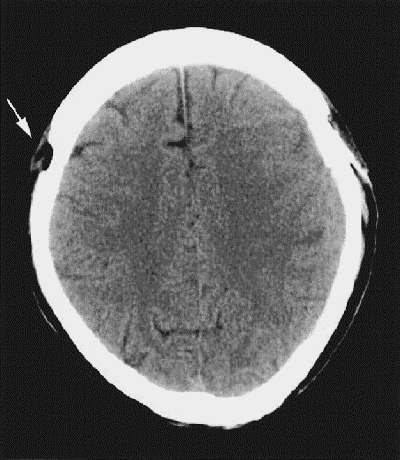
FIG. 3. Two months after the initial surgery, when the patient had fully recovered, the left side appears normal. The arrow points to the wrong-side (right) burr hole in the skull.
Error analysis
At least 3 distinct task steps were errors in the management of this patient: (1) the patient was taken to the operating room without the neurosurgeon being informed; (2) the first burr hole was placed on the normal (i.e., incorrect) side; (3) the neurosurgeon was not immediately notified of the error by the resident, but the operating-room charge nurse ultimately informed the staff surgeon. The main error of wrong-sided burr hole placement was a purely human one, likely the result of a brief lapse in concentration.
The major complication is well recognized in this type of surgery and was not directly related to the error in this case.
In summary, this patient sustained a major, preventable error, which had transient or minimal impact on the outcome. It likely did, however, have a significant impact on the psychological comfort and confidence of the patient's family. The patient also sustained a major complication or adverse event unrelated to the error.
Discussion
Surprisingly few peer-reviewed papers on the subject of wrong-sided surgery appear in the electronically indexed medical literature. Use of the key phrases “wrong side,” “wrong sided surgery,” “incorrect side,” “erroneous side,” “sidedness error” and “right–left error” in PubMed yielded fewer than 10 English-language papers,2,3,4,5,6,7,8 1 German paper9 and 3 single case reports in Swedish with no authors listed. However, it is very likely that this type of error is underreported for obvious reasons. Of the large chart reviews that elevated the profile of error in medicine since the early 1990s, the largest to deal with primarily surgical adverse events reported on 15 000 charts, and wrong-sided surgery is not mentioned in that paper.10 The introduction of “wrong-side surgery” in most popular search engines on the Internet yields on the other hand about 288 000 Web sites, some of which are quite useful, focusing on prevention of this error.11
Of the few reports available, 2 described erroneous laterality marking on CT scans2,9 and 1 on chest films.4 At least 2 others report wrong-sided chest tube placement.3,6 Another chronicles a small number of wrong-sided anesthesia blocks in a series of 2000 incident reports regarding regional anesthesia in an incidence-monitoring study.5 The 3 Swedish papers are 25 years old and apparently described reports of surgery on the wrong femur, hip and ureter. Some papers address policies used to safeguard against this preventable adverse event and record the usefulness of the simple act of marking sides.6,8
Human error is an inherent part of human behaviour and will always be present. Certain factors may predispose to increased frequency of human error in surgery, such as fatigue, which is common in surgeons and their housestaff and has been shown to increase error.12 Distractions and competing responsibilities to other patients with more urgent conditions may also contribute to errors13,14 as may imperfect communication in the operating room.15 However, the modern approach to patient safety and error prevention focuses on a systems approach as opposed to human error.16,17 If systems are in place that make it impossible for human error to reach the patient and cause harm, patient safety will be markedly improved.
If one examines the error of wrong-side surgery from a systems approach, simple, commonsense low-technology strategies to put systems in place could start with preoperative discussion between the surgeon and the family or patient, review of the patient's chart, and then side-marking on the appropriate body part. For example, for lumbar discectomy, the author marks the correct side with a large black marker on the ipsilateral buttock. This is not visible after the patient is draped, but the surgeon and the surgical team have had to think about and discuss the correct side before the mark can be placed. Such a policy has already been demonstrated to reduce the incidence of wrong-side knee surgery.18 These systems are not fail-safe since poor communication can occur between surgeon and patient, and the surgeon can still have a lapse in concentration when marking the side or when the surgical drapes are placed. A simple back-up would be for the charge nurse in the operating room or the anesthetist, or both, to discuss the side with the surgeon and fill out a check-list before the incision is made.
More high-technology and fail-safe systems for preventing wrong-side error exist. In cranial neurosurgery, if every craniotomy were done with the aid of a surgical navigation system registered to current imaging19 or in an intraoperative magnetic resonance imaging unit,20 the occurrence of wrong-side craniotomy would be decreased from rare to almost never. These surgical adjuncts are commonplace in most modern neurosurgical units, but they are often not available after hours and therefore they may not prevent an error like the one described here.
Systems must be developed to ensure maximum patient safety and minimize preventable adverse events. Widespread attention to medical error and its prevention is becoming part of the culture in most health care organizations. Wrong-sided surgery is fortunately rare, but when it does happen it is devastating for the patient and the care-givers, and should almost be considered the archetypal surgical error type in which simple but intelligent systems approaches should be able to reduce its incidence to zero in all types of surgery.
Correspondence to: Dr. Mark Bernstein, Division of Neurosurgery, Toronto Western Hospital, West Wing 4W451, 399 Bathurst St., Toronto ON M5T 2S8; fax 416 603-5298; mark.bernstein@uhn.on.ca
Accepted for publication Oct. 22, 2002.
References
- 1.Altman LK. State issues scathing report on error at Sloan-Kettering. The New York Times 1995 Nov 16; sect A:1, A:16.
- 2.Altinors N. Erroneous placement of side indicators of brain CT. Am J Neuroradiol 1994;15:197. [PMC free article] [PubMed]
- 3.Brasel KJ, Layde PM, Hargarten S. Evaluation of error in medicine: application of a public health model. Acad Emerg Med 2000;7:1298-302. [DOI] [PubMed]
- 4.Finnbogason T, Bremmer S, Ringertz H. Side markings of the neonatal chest X-ray: two legal cases of pneumothorax side mix up. Eur Radiol 2002;12:938-41. [DOI] [PubMed]
- 5.Fox MA, Webb RK, Singleton R, Ludbrook G, Runciman WB. The Australian Incident Monitoring Study. Problems with regional anesthesia: an analysis of 2000 incident reports. Anaesth Intensive Care 1993;21:646-9. [DOI] [PubMed]
- 6.Shapiro MJ, Croskerry P, Fisher S. Profiles in patient safety: sidedness error. Acad Emerg Med 2002;4:326-9. [DOI] [PubMed]
- 7.Wender SS. Operation on the wrong side. An avoidable adverse event. J Fla Med Assoc 1990;77:585-6. [PubMed]
- 8.Mawji Z, Stillman P, Laskowski R, Lawrence S, Karoly E, Capuano TA, et al. First do no harm: integrating patient safety and quality improvement. Jt Comm J Qual Improv 2002;28:373-86. [DOI] [PubMed]
- 9.Warnke JP, Kose A, Schniewind F, Zierski J. [Erroneous laterality marking in CT of the head. A case report.] Zentralbl Neurochir 1989;50:190-2. [PubMed]
- 10.Gawande AA, Thomas EJ, Zinner MJ, Brennan TA. The incidence and nature of surgical adverse events in Colorado and Utah in 1992. Surgery 1999;126:66-75. [DOI] [PubMed]
- 11.Oregon Association of Hospitals and Health Care Systems. Hints on preventing surgery on the wrong site. Available: www.aracnet.com/~oahhs/issues/safety/surgery.htm (accessed 2003 Feb 03).
- 12.Wesnes KA, Walker MB, Walker LG, Heys SD, White L, Warren R, et al. Cognitive performance and mood after a weekend on call in a surgical unit. Br J Surg 1997;84:493-5. [PubMed]
- 13.Boutros F, Redelmeier DA. Effects of trauma cases on the care of patients who have chest pain in an emergency department. J Trauma 2000;48:649-53. [DOI] [PubMed]
- 14.Flynn EA, Barker KN, Gibson JT, Peterson RE, Berger BA, et al. Impact of interruptions and distractions on dispensing errors in an ambulatory care pharmacy. Am J Health Syst Pharm 1999;56:1319-25. [DOI] [PubMed]
- 15.Lingard L, Reznick R, Espin S, Regehr G, DeVito I. Team communications in the operating room: talk patterns, sites of tension, and implications for novices. Acad Med 2002;77:232-7. [DOI] [PubMed]
- 16.Bernstein M, Hebert PC, Etchells E. Patient safety in neurosurgery: detection of errors, prevention of errors, and disclosure of errors. Neurosurg Q 2003;13(2). In press.
- 17.Kohn LT, Corrigan JM, Donaldson MS, editors. To err is human. Building a safer health system. Washington: National Academy Press; 2000. [PubMed]
- 18.McDermott MW. Image-guided surgery. In: Bernstein M, Berger MS, editors. Neuro-oncology: the essentials. New York: Thieme Medical Publishers; 2000.
- 19.Bernstein M, Al-Anazi AR, Kucharczyk W, Manninen P, Bronskill M, Henkelman M. Brain tumor surgery with the Toronto open magnetic resonance imaging system: preliminary results for 36 patients and analysis of advantages, disadvantages, and future prospects. Neurosurgery 2000;46:900-9. [DOI] [PubMed]
- 20.Bernstein M, Al-Anazi AR, Kucharczyk W, Manninen P, Bronskill M, Henkelman M. Brain tumor surgery with the Toronto open magnetic resonance imaging system. Preliminary results for 36 patients and analysis of advantages, disadvantages, and future prospects. Neurosurgery 2000;46:900-9. [DOI] [PubMed]


