Abstract
Introduction
Discoid meniscus is an atavistic anomaly in which the meniscus of the knee, predominantly the lateral meniscus, is discoid rather than semilunar in shape. The abnormality is diagnosed relatively infrequently and may even go unrecognized or be untreated. Treatment has consisted of either partial or complete meniscectomy performed either arthroscopically or by open arthrotomy. Our purpose was to examine the outcome of treatment for discoid meniscus in children.
Methods
Since 1974, 34 children, including 2 with bilateral involvement, have been treated for discoid meniscus at the Children's Hospital of Eastern Ontario, a major pediatric referral centre. The average age of the children at the time of surgery was 11 years 4 months (range from 6 yr 2 mo–18 yr 6 mo). The average follow-up was 3 years (range from 1 mo–22 yr). The lateral meniscus was affected in 35 of the 36 knees. Treatment consisted of partial resection in 19 cases, complete resection in 13; 4 did not undergo resection.
Results
There were 16 excellent, 10 good, 6 fair and 4 poor results at the time of most recent follow-up. In 2 cases degenerative changes were evident radiologically.
Conclusion
Partial resection of discoid menisci is preferable in children, but in complete dislocation of the entire menisci, total removal is necessary.
Abstract
Introduction
Le ménisque discoïde est une anomalie atavique en raison de laquelle le ménisque du genou, et surtout le ménisque latéral, prend une forme discoïde plutôt que semi-lunaire. Ce diagnostic est relativement rare et il arrive même que l'anomalie ne soit pas identifiée ou traitée. Le traitement a consisté en une méniscectomie partielle ou complète réalisée par arthroscopie ou par athrotomie ouverte. Nous voulions analyser le résultat du traitement du ménisque discoïde chez les enfants.
Méthodes
Depuis 1974, 34 enfants, dont 2 étaient atteints des deux côtés, ont été traités pour un ménisque discoïde au Centre hospitalier pour enfants de l'est de l'Ontario, grand centre de référence pédiatrique. Au moment de l'intervention chirurgicale, les enfants avaient en moyenne 11 ans et 4 mois (intervalle de 6 ans et 2 mois à 18 ans et 6 mois). Le suivi moyen s'est établi à 3 ans (intervalle d'un mois à 22 ans). Le ménisque latéral était atteint dans 35 des 36 genoux. Le traitement a consisté en une résection partielle dans 19 cas, une résection complète dans 13 et 4 sujets n'ont pas subi de résection.
Résultats
Il y avait 16 résultats excellents, 10 bons, 6 moyens et 4 médiocres au moment du suivi le plus récent. Dans deux cas, l'examen radiologique a révélé la présence de changements dégénératifs évidents.
Conclusion
La résection partielle des ménisques discoïdes est préférable chez les enfants, mais dans un cas de luxation complète de tout le ménisque, la résection totale s'impose.
Discoid meniscus is an abnormality of the fibrocartilaginous meniscus of the knee in which the meniscus is discoid rather than semilunar in shape. The condition was first reported by Young1 in 1889 when he dissected an anatomical specimen with a lateral discoid meniscus. Although most discoid menisci involve the lateral meniscus, the first cases of symptomatic discoid medial meniscus were reported by Watson-Jones2 in 1930 and subsequently by Cave and Staples3 in 1941.
Bilateral involvement of the lateral menisci is not uncommon. No sex preponderance has been reported. Discoid meniscus is classified into 3 types, according to the Watanabe system as follows: complete type — characterized by a discoid lateral meniscus, covering the entire lateral tibial plateau and attached to the tibial plateau; incomplete type — attached to but not covering the entire lateral tibial plateau; Wrisberg-ligament type — a discoid lateral meniscus, covering the entire lateral tibial plateau but attachment only to the posterior meniscofemoral ligament not the tibial plateau.
The reported prevalence of discoid meniscus is between 0.4% and 17%.4,5 In the Caucasian population, it is less than 5%,6,7 rising to 12.5% in the Korean population8 and 17% in the Japanese population.5 The reason for this prevalence distribution is unknown.
The principal diagnostic feature of discoid meniscus has been a history of snapping or clicking in the knee;9 however, recent studies have reported that pain is a more common preoperative complaint.10,11,12 Several studies have reported that radiography is noncontributory in establishing the diagnosis, whereas arthrography and arthroscopy are helpful.3,10,13,14,15,16,17 Magnetic resonance imaging has also been used for diagnosis, with the added advantage of an increased sensitivity in detecting meniscal tears.18,19,20
For symptomatic discoid meniscus, nonoperative treatment consisting of a short-course of knee immobilization, restricted activities and strengthening exercises of the quadriceps muscles is recommended. Surgical intervention should be reserved for symptomatic cases with recurrent locking or persistent pain. Options for surgical management include partial removal of the torn portion, restoring the anatomical configuration of the meniscus or complete resection of the meniscus, which should be avoided because of the potential for degenerative change.
In this study we review the experience and results of the management of discoid meniscus at the Children's Hospital of Eastern Ontario, Ottawa, a major pediatric referral centre. We also wished to compare the results of management by the type of surgical procedure and resection.
Patients and methods
The clinical, radiologic and operative records of all children treated at our institution since 1974 for meniscal disorders were retrospectively reviewed. Thirty-four children (12 boys, 22 girls) were treated for discoid meniscus, 2 bilaterally, making a total of 36 knees. Each discoid meniscus was classified according to the Watanabe classification on the basis of its appearance on magnetic resonance imaging or at the time of surgery. The initial treatment was nonoperative in all cases (restricted activity, immobilization or bracing with subsequent physiotherapy to increase knee range of motion and strength).
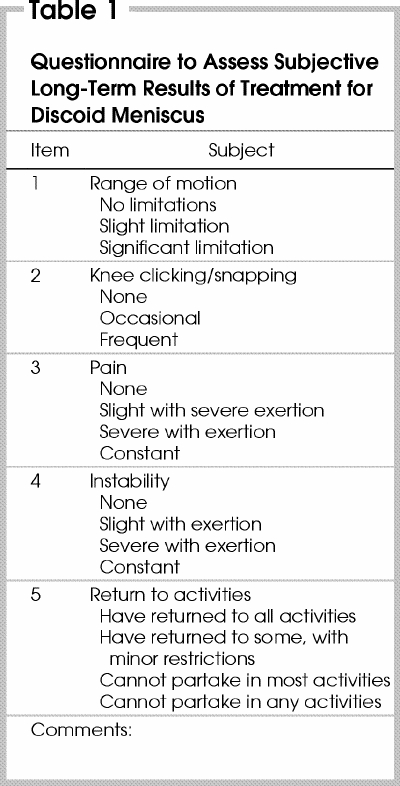
Results were classified according to the criteria proposed by Ikeuchi:5 excellent — full range of motion, no knee snapping and no pain; good — infrequent pain with exertion and full range of motion; fair — slight pain, knee snapping on motion and full range of knee motion; poor — constant pain or recurrent locking of the knee, or both. A questionnaire was developed to assess the subjective long-term results of treatment (Table 1).
Table 1
Results
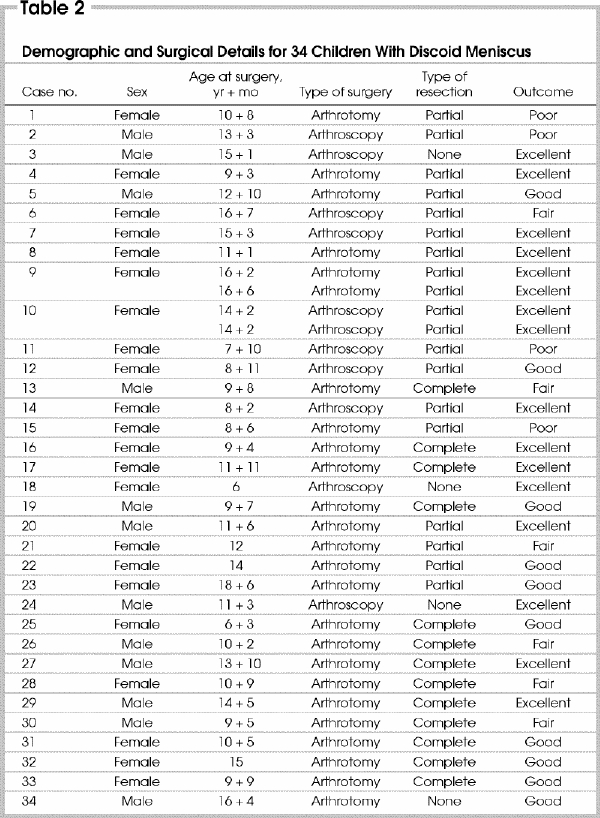
Details concerning sex, age at surgery, surgical procedure and outcome of the study group are shown in Table 2. The average age at the time of initial presentation was 10 years 5 months (range from 5 yr 3 mo–17 yr 7 mo) and at the time of surgery was 11 years 4 months (range from 6 yr 2 mo–18 yr 6 mo). The average length of follow-up was 3 years (range from 1 mo–22 yr). The right knee was involved in 12 cases (33%) and the left knee in 24 (67%). The medial meniscus was affected in 1 knee (3%) and the lateral meniscus in the remaining 35 knees (97%). There were 30 complete (83%), 3 incomplete (8%) and 3 Wrisberg-ligament (8%) type discoid menisci.
Table 2
The duration of symptoms before surgery ranged from 1 month to 6 years (average 1 yr 7 mo). Clicking, snapping or clunking of the affected knee was reported in 19 cases (53%), pain in 19 (53%), “giving way” in 9 (25%), locking in 9 (25%) and decreased range of motion in 4 (11%). There was a history of trauma in 8 cases (22%). On clinical examination, the McMurray test for meniscal injury was positive in 19 knees (53%). There was a positive pivot shift in 2 knees (6%). Effusion of the knee joint was evident in 5 (14%). Lateral joint tenderness was present in 8 cases (22%). There was a decrease in knee flexion greater than 10° in 5 cases (14%) and a decrease in knee extension greater than 10° in 2 (6%).
Each child had radiography, and the diagnosis was apparent in 7 of the 34 children, with a squared-off appearance of the distal femur in 1 and increased joint space in 6 (Fig. 1). Radiography were noncontributory in 27 children. Magnetic resonance imaging was diagnostic in each of the 7 children in whom it was performed (Fig. 2). Arthrography was diagnostic in each of the 4 children in whom it was performed (Fig. 3). The remaining cases were diagnosed by arthroscopy.
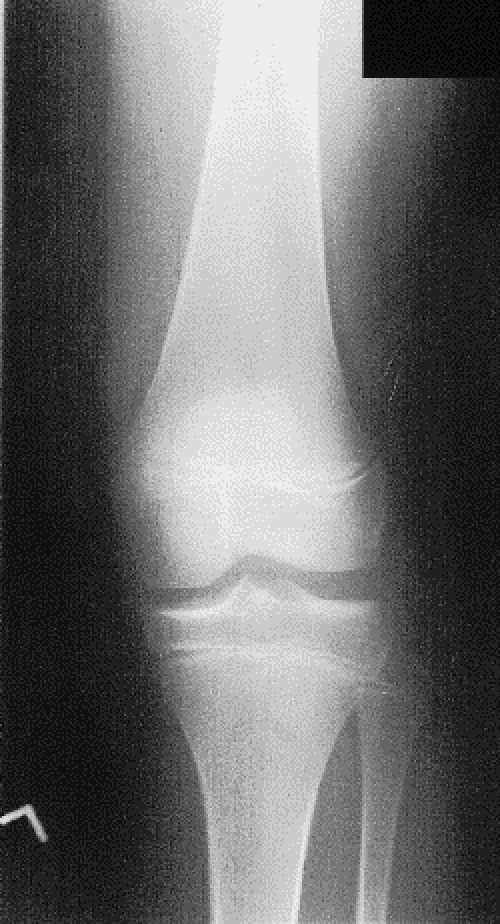
FIG. 1. Radiograph of the left knee in case 8 (a girl aged 10 yr 10 mo) revealing a squared-off appearance of the lateral femoral condyle and increased lateral joint space, indicative of discoid meniscus.
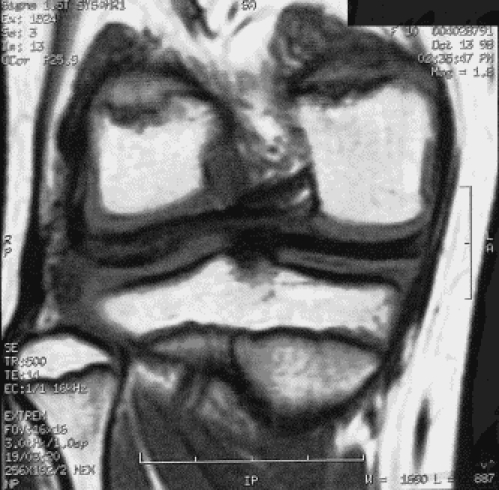
FIG. 2. Left: a coronal T 1 -weighted magnetic resonance image in case 1 (a girl aged 10 yr 6 mo) indicating increased thickness of the right lateral meniscus, consistent with discoid meniscus, and no other pathologic condition. Right: a sagittal T 2 -weighted magnetic resonance image further demonstrating the discoid meniscus and lack of any other abnormality.

Figure 2. Continued.

FIG. 3. Arthrogram of the left knee in case 14 (a girl aged 7 yr 6 mo), demonstrating left lateral discoid meniscus with no additional abnormality.
There were no associated injuries or meniscal tears in 24 knees (67%), but a lateral meniscal tear was present in 7 (19%). There was 1 case of an associated tibial spine fracture, 1 proliferation of the plica, 1 meniscal cyst, 1 case of excessive laxity of the medial collateral ligament, and 1 associated chondromalacia of the lateral femoral condyle.
Of the 36 knees, complete or partial resection was done in 32 (89%). The time from initial presentation until surgery averaged 11 months (range from 1 mo–5 yr 9 mo). Arthrotomy was performed in 25 (69%) cases, involving complete resection in 13 and partial resection in 11; no resection was done in 1 case. Arthroscopic partial resection was performed in 8 (22%) cases, and a diagnostic arthroscopy in 3 (8%). Arthroscopy was converted to arthrotomy with subsequent meniscal resection in 15 knees. Of the 4 children who did not undergo resection, there was no significant abnormality at the time of arthroscopy in 1 (case 24, Table 2), the knee joint was too small for resection in 1 (case 18), there was a concomitant medial meniscal tear requiring medial meniscectomy in 1 (case 34), and in 1 the family declined resection (case 3).
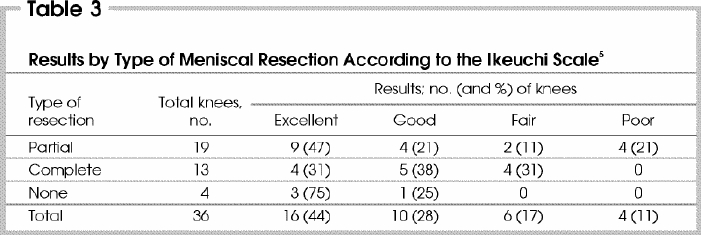
Overall, according to the Ikeuchi scale,5 the outcome was excellent in 16 (44%) cases, good in 10 (28%), fair in 6 (17%) and poor in 4 (11%) at the time of most recent follow-up. Of the 19 children treated with a partial resection, the results were good to excellent in 13 (68%), and of the 13 children treated with complete resection, the results were good to excellent in 9 (69%) (Table 3).
Table 3
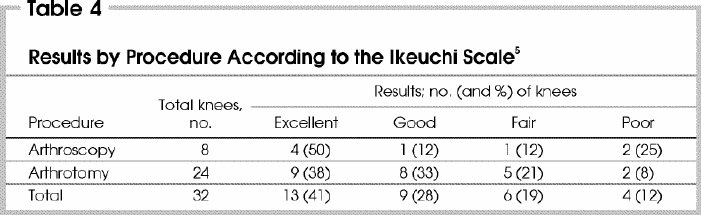
Of the 8 children who underwent arthroscopic resection, the results were good to excellent in 5 (63%), and of the 24 knees treated by arthrotomy, the results were good to excellent in 17 (71%) (Table 4). Of the 4 children who did not undergo resection of the discoid meniscus, 3 had an excellent results and 1 a good result. In this subgroup, there were 3 complete discoid menisci and 1 incomplete discoid meniscus.
Table 4
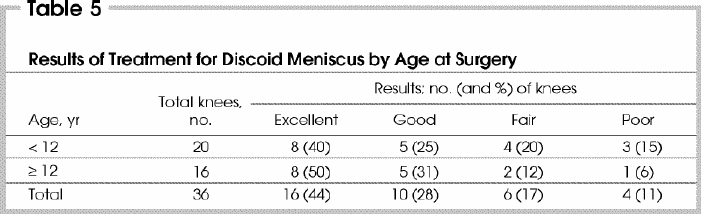
Results were also determined by age at the time of surgery (Table 5). Among 20 knees treated in children younger than 12 years, there were 13 (65%) good to excellent results, and among the 16 knees treated in children, 12 years of age or older there were 13 (81%) good to excellent results.
Table 5
The questionnaire (Table 1) was returned by 10 (29%) of the 34 children. Analysis of the questionnaires revealed improvement in outcome in 2 and deterioration in 4, while the remaining children reported no change from the last clinical evaluation.
Of the 34 children in this series, 20 (22 knees) were followed up for longer than 1 year, including both children with bilateral involvement. The average length of follow-up among these children was 4 years 10 months (range from 1–22 yr). This group contained 16 (73%) complete, 3 (14%) incomplete and 3 (14%) Wrisberg-ligament type discoid menisci. There were no associated injuries in 17 (77%), a tear of the discoid meniscus in 3 (14%), osteochondritis dissecans of the lateral femoral condyle in 1 (4%) and medial collateral ligament laxity in 1 (4%). In this group of 22 knees, there were 11 (50%) excellent, 4 (18%) good, 5 (23%) fair and 2 poor (9%) results, compared with 5 (36%) excellent, 6 (43%) good, 1 (7%) fair and 2 (14%) poor outcomes for the knees of the 14 children who were followed up for 1 year or less. Partial resection was performed on 13 of the 22 knees (through an arthrotomy in 10 cases), with 8 excellent, 2 good, 1 fair result and 2 poor results. Complete resection by arthrotomy was performed in 8 knees, with 2 excellent, 2 good and 4 fair results. In 1 child the meniscus was not resected. In the younger age group (< 12 yr at the time of surgery), there were good to excellent results in 7 (54%), fair in 4 (31%) and poor in 2 (15%) of the 13 knees. In the older age group (≥ 12 yr) there were good to excellent results in 8 knees and a fair result in 1 of the 9 knees.
In total, there were 15 complications in the 36 knees (42%). In 2 knees (6%) there was a persistent decrease in knee range of motion of greater than 10°. In 4 (11%) knees the child reported persistent pain. Persistent knee joint effusion was evident in 3 (8%) cases and patellofemoral syndrome in 3 (8%). One child sustained a tear of the residual meniscus after partial resection. There were 2 cases of postoperative degenerative knee-joint changes (6%). In both cases the knee had been treated with an arthrotomy: by complete resection in 1 case (case 26 Table 2) (Fig. 4) and by partial resection in the other (case 15, Table 2). In both cases, the child complained of pain, and radiographs demonstrated degenerative changes at 5 and 8 years postoperatively respectively. In 1 case (case 7, Table 2) osteochondritis dissecans of the lateral femoral condyle developed, and the osteochondral fragment required pinning (Fig. 5).

FIG. 4. Anteroposterior (left) and lateral (right) radiographs of the left knee in case 26 (a boy aged 18 yr 4 mo) 8 years after arthrotomy and complete resection of the left lateral discoid meniscus. Early degenerative changes are revealed, including subchondral sclerosis and early subchondral cyst formation.

Figure 4. Continued.
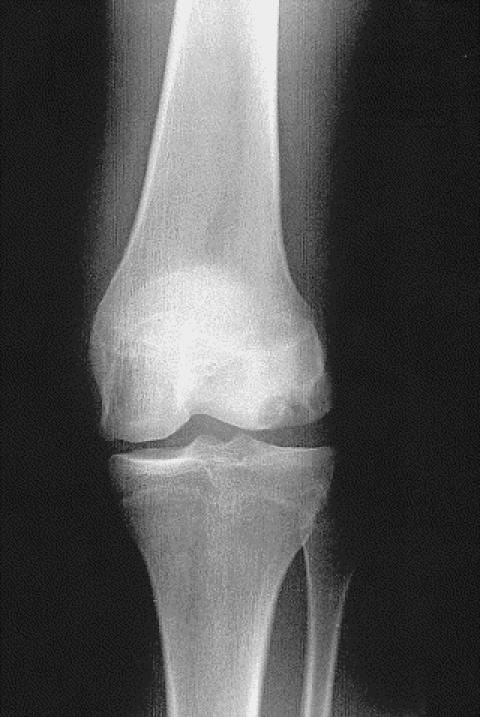
FIG. 5. Left: a radiograph of the left knee in case 7 (a girl aged 15 yr 3 mo), revealing increased lateral joint-space widening, indicative of discoid meniscus, as well as osteochondritis dissecans of the lateral femoral condyle. Right: 3 years postoperatively, the radiograph reveals healing of the osteochondritis dissecans and improvement in lateral joint-space width.

Figure 5. continued
Discussion
Bilateral involvement in discoid meniscus is not uncommon. In this series, 2 children presented with symptomatic bilateral discoid meniscus, an incidence of 6% in our series. No sex predilection has been reported, but in this series of 34 children, 22 were girls, representing a 2 to 1 female to male preponderance. The reason for this female predilection is unclear and further studies are warranted to determine if it truly exists.
Symptoms have been reported most frequently during adolescence, although cases have been reported in children as young as 47 and 8 months11 of age. In this series, the youngest child at the time of presentation was 5 years 3 months, although 1 child described symptoms developing at 4 years 10 months of age. The majority of children reported in the literature have presented between 10 and 15 years of age.10,21 Other studies have noted an average age at onset of symptoms of 9 years.12,22 In this series, the majority of children presented before adolescence (average age at the time of initial presentation 10 yr 5 mo). Typically the average duration of symptoms reported in the literature has been between 17 and 21 months.12,21 This was also our experience (average duration of symptoms 19 mo). On the basis of the results in this series and in the literature, presentation before adolescence appears to be most common.
The lateral meniscus is more commonly affected than the medial meniscus. In a review by Dickason and associates,23 the incidence of discoid medial meniscus was 0.12% and of discoid lateral meniscus was 1.5%. In addition to the existence of lateral discoid meniscus, associated abnormalities have been reported. An anomalous insertion of the anterior horn of the medial meniscus into the anterior cruciate ligament has been reported in cases of lateral discoid meniscus in up to 7.5% of cases in the Korean population.8,24 Meniscal tears have also been frequently reported in association with discoid meniscus.10,12,21,23,25 Hayashi and associates21 reported a series of lateral discoid meniscus in 53 knees, all of which had a tear of the affected meniscus. The majority of meniscal tears, in as many as 75% of cases, have been encountered in the posterior or middle aspect of the discoid meniscus.12,21 It has been postulated that the increased thickness of the discoid meniscus, its unstable attachment to the tibial plateau and its poor vascularization increase susceptibility to mechanical stress.26 In our series, 7 (19%) knees had associated meniscal tears at the time of presentation. The reason for this decreased rate compared with that reported in the literature is unknown.
The most common type of discoid meniscus is reportedly the complete type, in up to 87% of cases.21,24 Our findings were similar, as the complete type predominated in 83% of cases. There was, however, an equal distribution between the incomplete and Wrisberg-ligament types of discoid meniscus.
Although the classical clinical finding associated with discoid meniscus has been a snapping or clicking knee,9 recent studies have reported that pain is a more common presenting complaint.10,11,12 Pain was a presenting complaint in 19 (53%) cases in our serie. Smillie27 reported snapping knee as a presenting complaint in only 4 (14%) of 29 children, but Nathan and Cole7 noted that 20 (77%) of 26 patients presented with snapping knee. In our study, snapping, clicking or clunking of the affected knee was reported in 19 cases (53%). According to Woods and Whelan20 snapping knee was associated with the Wrisberg-ligament type of discoid meniscus, whereas an absence of snapping knee was encountered in the complete and incomplete types of discoid meniscus. This was not our experience.
The diagnosis of discoid meniscus is based on the clinical and radiologic findings. Suggestive radiographic findings include a squared-off appearance of the lateral femoral condyle, widened lateral joint space, cupping of the tibial plateau, elevated fibular head, oblique orientation of the surface of the tibial plateau, hypoplasia of the tibial spine and dysmorphia of the femoral condyles.17,28,29 The majority of studies have reported that these findings did not contribute to the diagnosis because of the frequent absence of these features.3,10,13,14,17,30 In our series, the radiographic appearance was indicative of discoid meniscus in 7 cases and was noncontributory in 27, indicating a lack of efficacy of radiographic diagnosis. Hall16 advocated arthrography for diagnosis. Arthrography was used for definitive diagnosis in 4 children in our series; however, we preferred magnetic resonance imaging (MRI) because of its enhanced sensitivity to soft-tissue abnormality and its decreased invasiveness. Several studies have recommended MRI for diagnosis of discoid meniscus and have noted the advantage this technique for demonstrating associated meniscal tears.18,19,20 Blacksin and associates18 reported that sagittal magnetic resonance images demonstrated the extent of contiguity between the anterior and posterior meniscal horns whereas coronal images illustrated the degree of meniscal thickening. In our series, MRI was diagnostic in 7 cases and was effective in evaluating additional meniscal disease.
The initial treatment of discoid meniscus is nonoperative, consisting of immobilization, restricted activities and quadriceps muscle strengthening. Surgical treatment is indicated only in persistently symptomatic knees. Options for surgical intervention include either partial or complete meniscectomy performed by open arthrotomy or arthroscopy. Several concerns have been raised regarding total resection of discoid meniscus in children. Ikeuchi5 reported lateral instability in children after total resection of the lateral discoid meniscus, and others have noted an increased frequency of progressive degenerative changes in adults.31,32,33,34 Raber and colleagues22 reported osteoarthritic changes in 10 of 11 knees at an average follow-up of 19.8 years after total meniscal resection, and Zaman and Leonard35 noted a 19% incidence in 59 knees. Manzione and colleagues34 reported radiographic changes suggestive of osteoarthritis in 16 of 20 patients, and Wroble and colleagues36 noted similar changes in 37 of 41 knees. These findings have prompted several authors to recommend against complete meniscectomy in children.22,35 In our series, 13 children underwent complete resection with 4 excellent, 5 good and 4 fair results at an average follow-up of 4 years 7 months. Only 2 cases of degenerative change were encountered. Both knees were treated with arthrotomy, one by complete and the other by partial resection. These results suggest that complete resection may not be associated with as high a risk of degenerative changes in children as previously suspected. However, these results are based on short-term follow-up; the long-term function of these knees is unknown.
It has been postulated that development of osteoarthritis, after complete meniscectomy may not be as common in children because of the axial alignment of the extensor mechanism, tissue pliability and resulting knee adaptation to the new forces acting on the joint surface.21 In support of this theory, Abdon and associates37 reported that 74% of children who underwent total resection of discoid meniscus were pleased with their long-term outcome and function, even though only 58% had a clinically satisfactory result. Aichroth and colleagues10 reported osteoarthritic changes in 3 (5%) of 62 knees at 18 years after total resection. In our series, osteoarthritis was seen in only 1 of 13 knees treated with complete resection of a discoid meniscus at an average follow-up of 1 year 7 months, a rate of 8%, which is similar to results previously reported. In 1 child, however, there were degenerative changes in the knee 5 years after partial resection at the age of 13 years 6 months.
Controversy exists in the literature regarding the true risk of osteoarthritis secondary to meniscectomy in the treatment of discoid meniscus. The effects of complete meniscectomy on the long-term function and development of degenerative changes has been well established in the general population; however, there is little information regarding the long-term function of the knee with discoid meniscus, and this requires further long-term investigation.
Several authors have advocated partial meniscectomy of discoid meniscus in an attempt to preserve as much of the meniscus as possible and thereby decrease the potential for degenerative changes and instability.10,25,30,38 Fujikawa and associates38 and Washington and colleagues12 recommended partial meniscal resection by open arthrotomy with subsequent arthroscopic evaluation of the posterior rim of the residual meniscus to ensure that no degenerative changes have occurred. Several studies have reported, however, that owing to marked hypermobility associated with the Wrisberg-ligament type of discoid meniscus, partial meniscectomy is insufficient and complete resection is indicated.9,10,30,39 In our series there were 3 cases of Wrisberg-ligament-type discoid meniscus, 2 of which were treated with partial resection with 1 excellent and 1 good result. The third knee was treated with complete resection with a fair result. These results suggest that partial resection is an effective treatment for Wrisberg- ligament-type discoid meniscus, in contrast to previous findings.12,13,40 Additional long-term studies of the treatment of Wrisberg-ligament-type discoid meniscus is required to establish the most efficacious surgical management.
Using the Ikeuchi5 classification system, Aichroth and associates10 reported 37% excellent, 47% good and 16% fair results at an average follow-up of 5.5 years, in a study of 52 children treated at an average age of 10.5 years with arthroscopic partial meniscal resection. Washington and colleagues12 reported 18 cases with excellent results in 10, good outcomes in 3 and fair results in 5, in all of which the knee was treated with partial resection of the discoid meniscus by open arthrotomy. Pellacci and colleagues40 reported excellent or good outcomes in 17 of 18 knees after partial resection of discoid meniscus. Bellier and colleagues13 reported excellent results in 18 of 19 children treated with partial discoid meniscectomy at an average follow-up of 3 years. In this series, the Ikeuchi5 classification was used to determine the outcome. In our study, we found a similar rate of good to excellent results with partial and complete meniscectomy. Ikeuchi5 and Hayashi and colleagues21 reported better clinical results in patients who underwent complete meniscectomy than in those who were treated with partial resection. Longer follow-up is required to assess the long-term results. In our study, 8 children were treated by arthroscopy and 24 by arthrotomy. Of knees treated arthroscopically, there were good to excellent results in 63% of cases. Of the 24 knees treated by arthrotomy, there were good to excellent results in 71% of cases. These findings suggest that arthrotomy is associated with a better outcome, but it may result from the difficulty in resecting the meniscus arthroscopically in children, in whom the knee joint is small.
Age at the time of surgical treatment appears to play a role in the final outcome. The rate of excellent results was higher in children 12 years of age or older, as 50% of knees in this group had excellent results, compared with 40% among children younger than 12 years of age. Among children 12 years of age or older at the time of surgery, poor outcomes were encountered in 6% of knees compared with 15% among those younger than 12 years. Overall, good to excellent results were achieved in 81% of those 12 years of age and older versus 65% in those younger than 12 years. Furthermore, a slightly higher rate of poor results was encountered in younger children. The reason for this is open to speculation and further study is required to substantiate this finding and determine the cause.
One potential criticism of this study is the length of follow-up. Of the 34 children, 20 (59%) were available for long-term follow-up assessment. This may have biased the results in the direction of more favourable outcomes with long-term deterioration, which was not appreciated. However, the rate of good to excellent results was not substantially different between the group with follow-up less than 1 year (79%) and the group with a follow-up longer than 1 year (70%). This may indicate that results do not have a tendency to deteriorate over time, thereby reducing the potential for bias as a result of length of follow-up.
Conclusions
We have noted the first predilection of females to discoid meniscus. Children 12 years of age and older had a higher incidence of good to excellent results. The results of this study demonstrated better results than previously reported with open arthrotomy and total meniscectomy. Further long-term assessment of the effects of meniscectomy in the treatment of discoid meniscus is essential. Osteoarthritis developed in only 2 children to date, indicating a decreased risk for degenerative changes subsequent to meniscal resection in this age group. However, the effects of such a procedure once the child reaches adulthood are unknown. For this reason, in spite of the apparent good results from total meniscectomy, a partial resection of the discoid meniscus, contoured to the anatomy of a normal meniscus, is recommended for the complete and partial types in children. Although controversy exists regarding the optimal management of the hypermobile Wrisberg type, the results in this series suggest good outcomes with partial meniscectomy.
Competing interests: None declared.
Correspondence to: Dr. Mervyn Letts, Department of Surgery, Shaikh Khalifa Medical Center, PO Box 51900, Abu Dhabi, United Arab Emirates; letmer764@skmc.gov.ae
Accepted for publication Apr. 15, 2003.
References
- 1.Young RB. The external semilunar cartilage as a complete disc. In: Cleland J, MacKay JY, Young RB, editors. Memoirs and memoranda in anatomy. Vol. 1. London: Williams and Norgate; 1889. p. 179.
- 2.Watson-Jones R. Specimen of internal semilunar cartilage as a complete disc. Proc R Soc Med 1930;23:588. [PMC free article] [PubMed]
- 3.Cave EF, Staples OS. Congenital discoid meniscus of cause of internal derangement of the knee. Am J Surg 1941;54:371-6.
- 4.Barthel T, Pesch R, Lippert MJ, Lutz G. Arthroskopische Behandlung des lateralen Scheibenmeniskus.Arthroskopie 1995;8:12-8.
- 5.Ikeuchi H. Arthroscopic treatment of the discoid lateral meniscus: technique and long-term results. Clin Orthop 1982;167:19-28. [PubMed]
- 6.Clark CR, Ogden JA. Development of the menisci of the human knee joint. Morphologic changes and their potential role in childhood meniscal injuries. J Bone Joint Surg Am 1983;65:538-47. [PubMed]
- 7.Nathan PA, Cole SC. Discoid meniscus: a clinical and pathological study. Clin Orthop 1969;64:107-13. [PubMed]
- 8.Kim SJ, Kim DW, Min BH. Discoid lateral meniscus associated with anomalous insertion of the medial meniscus. Clin Orthop 1995;315:234-7. [PubMed]
- 9.Kaplan EB. Discoid lateral meniscus of the knee joint. J Bone Joint Surg Am 1957;39:77-80. [PubMed]
- 10.Aichroth PM, Patel D, Marx C. Congenital discoid lateral meniscus in children: a follow-up study and evolution of management. J Bone Joint Surg Br 1991;73:932-6. [DOI] [PubMed]
- 11.Barnes CL, McCarthy RE, Vanderschilden JL, McConnell JR, Nusbickel FR. Discoid lateral meniscus in a young child: case report and review of the literature. J Pediatr Orthop 1988;8:707-9. [DOI] [PubMed]
- 12.Washington ER, Root L, Liener UC. Discoid lateral meniscus in children: long-term follow-up after excision. J Bone Joint Surg Am 1995;77:1357-61. [DOI] [PubMed]
- 13.Bellier G, DuPont JY, Larrain M, Caudron C, Carlioz H. Lateral discoid menisci in children. Arthroscopy 1989;5:52-6. [DOI] [PubMed]
- 14.Bramson RT, Staple TW. Double contrast knee arthrography in children. Am J Roentgenol 1975;123:838-44. [DOI] [PubMed]
- 15.Chen YC. Arthroscopic meniscectomy of the discoid meniscus. Arthroscopy 1988;4:131-5.
- 16.Hall FM. Arthrography of the discoid lateral meniscus. Am J Roentgenol 1977;218:993-1002. [DOI] [PubMed]
- 17.Haveson SB, Rein BI. Lateral discoid meniscus of the knee: arthrographic diagnosis. Am J Roentgenol 1970;109:581-5. [DOI] [PubMed]
- 18.Blacksin MF, Greene B, Bothelho G. Bilateral diskoid medial menisci diagnosed by magnetic resonance imaging: a case report. Clin Orthop 1992;285:214-6. [PubMed]
- 19.Silverman JM, Mink JH, Deutsch AL. Discoid menisci of the knee: MR imaging appearance. Radiology 1989;173:351-4. [DOI] [PubMed]
- 20.Woods GW, Whelan JM. Discoid meniscus. Clin Sports Med 1990;9:695-706. [PubMed]
- 21.Hayashi LK, Yamaga H, Ida K, Miura T. Arthroscopic meniscectomy for discoid lateral meniscus in children. J Bone Joint Surg Am 1988;70:1495-500. [PubMed]
- 22.Raber DA, Friedrich NF, Hefti F. Discoid lateral meniscus in children: long-term follow-up after total meniscectomy. J Bone Joint Surg Am 1998;80:1579-86. [DOI] [PubMed]
- 23.Dickason JM, Del Pizzo W, Blazina ME, Fox JM, Friedman MJ, Snyder SJ. A series of ten discoid medial menisci. Clin Orthop 1982;168:75-9. [PubMed]
- 24.Kim SJ, Lee YT, Kim DW. Intraarticular anatomic variants associated with discoid meniscus in Koreans. Clin Orthop 1998;356:202-7. [DOI] [PubMed]
- 25.Dimakopoulos P, Patel D. Partial excision of discoid meniscus: arthroscopic operation of 10 patients. Acta Orthop Scand 1989;60:40-1. [DOI] [PubMed]
- 26.Danzig L, Resnick D, Gonsalves M, Akeson WH. Blood supply to the normal and abnormal menisci of the human knee. Clin Orthop 1983;172:271-6. [PubMed]
- 27.Smillie IS. The congenital discoid meniscus. J Bone Joint Surg Br 1948;30:671-7. [PubMed]
- 28.Berson BL, Hermann G. Torn discoid menisci of the knee in adults: five case reports. J Bone Joint Surg Am 1979;61:303-4. [PubMed]
- 29.Engber WD, Mickelson MR. Cupping of the lateral tibial plateau associated with a discoid meniscus. Orthopedics 1981;4:904-6. [DOI] [PubMed]
- 30.Dickhaut SC, Delee JC. The discoid lateral-meniscus syndrome. J Bone Joint Surg Am 1982;64:1068-73. [PubMed]
- 31.Fairbank TJ. Knee joint changes after meniscectomy. J Bone Joint Surg Br 1948;30:664-70. [PubMed]
- 32.Kobayashi A, Uezaki N, Mitsuyasu M. Discoid meniscus of the knee joint. Clin Orthop Surg 1975;10:10-24.
- 33.Kurozawa H, Koide K, Nakajima H. Results of meniscectomy. J Orthop Surg 1976;27:825-32.
- 34.Manzione M, Pizzutillo DD, Peoples AB, Schweizer PA. Meniscectomy in children: a long-term follow-up study. Am J Sports Med 1983;11:111-5. [DOI] [PubMed]
- 35.Zaman M, Leonard MA. Meniscectomy in children: results in 59 knees. Injury 1981;12:425-8. [DOI] [PubMed]
- 36.Wroble RR, Henderson RC, Campion ER, El-Khoury GY, Albright JP. Meniscectomy in children and adolescents: a long-term follow-up study. Clin Orthop 1992;279:180-9. [PubMed]
- 37.Abdon P, Turner MS, Pettersson H, Lindstand A, Stenstrom A, Swanson AJ. A long-term follow-up study of total meniscectomy in children. Clin Orthop 1990;257:166-70. [PubMed]
- 38.Fujikawa K, Iseki F, Mikura Y. Partial resection of the discoid meniscus in the child's knee. J Bone Joint Surg Br 1981;63:391-5. [DOI] [PubMed]
- 39.Griffin PP. The lower limb. In: Lovell WW, Winter RB, editors. Paediatric orthopaedics. 2nd ed. Philadelphia: JB Lippincott; 1986. p. 887.
- 40.Pellacci F, Montanari G, Prosperi P, Galli G, Celli V. Lateral discoid meniscus: treatment and results. Arthroscopy 1992;8:526-30. [DOI] [PubMed]


