Abstract
Background
Ultrasonography (US) has become indispensable in assessing the status of the injured patient. Although hand-held US equipment is now commercially available and may expand the availability and speed of US in assessing the trauma patient, it has not been subjected to controlled evaluation in early trauma care.
Methods
A 2.4-kg hand-held (HH) US device was used to perform focused abdominal sonography for trauma (FAST) on blunt trauma victims at 2 centres. Results were compared with the “truth” as determined through formal FAST examinations (FFAST), CT, operative findings and serial examination. The ability of HHFAST to detect free fluid, intra-abdominal injuries and injuries requiring therapeutic interventions was assessed.
Results
HHFAST was positive in 80% of 313 patients who needed surgery or angiography. HHFAST test performances (sensitivity, specificity, positive and negative predictive values, likelihood ratios of positive and negative test results) were 77%, 99%, 96%, 94%, 95%, 95 and 0.2, respectively, for free fluid, and 64%, 99%, 96%, 89%, 90%, 74 and 0.4, respectively, for documented injuries. HHFAST missed or gave an indeterminate result in 8 (3%) of 270 patients with injuries who required therapeutic intervention and 25 (9%) of 270 patients who did not require intervention. FFAST performance was comparable.
Conclusions
HHFAST performed by clinicians detects intraperitoneal fluid with a high degree of accuracy. All FAST examinations are valuable tests when positive. They will miss some injuries, but the majority of the injuries missed do not require therapy. HHFAST provides an early extension of the physical examination but should be complemented by the selective use of CT, rather than formal repeat US.
Abstract
Contexte
L'échographie est devenue indispensable pour évaluer l'état du patient traumatisé. Même si le marché offre maintenant du matériel d'échographie portatif qui peut étendre la disponibilité de cet examen et accélérer l'évaluation du patient traumatisé, ces appareils n'ont pas été soumis à une évaluation contrôlée pour les premiers soins aux traumatisés.
Méthodes
Dans deux centres, on a utilisé un appareil d'échographie portatif de 2,4 kg pour procéder à un examen abdominal focalisé de détection de traumatisme (FAST) sur des patients atteints de traumatisme fermé. On a comparé les résultats à la «réalité», telle que déterminée par les examens FAST standards (FFAST), par tomodensitométrie, en fonction des résultats opératoires et par un examen en série. On a évalué la capacité de la technique FAST manuelle à détecter des traumatismes intra-abdominaux libres et fluides et des traumatismes exigeant des interventions thérapeutiques.
Résultats
La technique FAST manuelle s'est révélée positive chez 80 % des 313 patients qui ont eu besoin d'une intervention chirurgicale ou d'une angiographie. Les résultats de test de la technique FAST manuelle (sensibilité, spécificité, valeur prédictive positive et négative, coefficient de probabilité des résultats d'examen positifs et négatifs) se sont établis à 77 %, 99 %, 96 %, 94 %, 95 %, 95 et 0,2 respectivement dans le cas des traumatismes libres et fluides et à 64 %, 99 %, 96 %, 89 %, 90 %, 74 et 0,4 respectivement dans celui des traumatismes documentés. La technique FAST manuelle a échoué ou donné un résultat indéterminé chez 8 (3 %) des 270 patients traumatisés qui ont eu besoin d'une intervention thérapeutique et chez 25 (9 %) des 270 qui n'ont pas eu besoin d'intervention. La technique FAST standard a donné un résultat comparable.
Conclusions
La technique FAST manuelle utilisée par des cliniciens permet de détecter la présence de liquide intrapéritonéal avec beaucoup de précision. Tous les examens FAST sont valables lorsqu'ils donnent un résultat positif. Ils rateront quelques traumatismes, mais la majorité des traumatismes ratés n'ont pas besoin d'être traités. La technique FAST manuelle permet une évaluation rapide antérieure à l'examen physique, mais il faut la compléter par l'utilisation sélective de la tomodensitométrie au lieu de répéter l'échographie par la méthode standard.
Clinical abdominal examination is inaccurate for the assessment of the blunt trauma patient as there are often distracting injuries, altered levels of consciousness, nonspecific signs and symptoms and large differences in individual patient reactions to intra-abdominal injury.1,2,3,4 Thus, diagnostic tests must be selected, performed and interpreted to reliably discriminate between patients who require therapeutic intervention or further study from those who do not. Quick ultrasonographic screening to identify the presence of free intraperitoneal and intrapericardial fluid constitutes focused abdominal sonography for trauma (FAST) examination,5 which is becoming the clinical standard. The most important benefits of this technique are an earlier and portable means of confirming the presence of intracavity hemorrhage or visceral leakage. Boulanger and associates6 reported in 2000 that FAST had replaced diagnostic peritoneal lavage as the initial screening test after blunt abdominal trauma in the majority of North American trauma centres.
Portable hand-held (HH) ultrasonography (US) units have recently become available to clinicians. These units were developed through a joint civilian–military initiative to provide portable US capability suitable for the battlefield or a mass casualty situation.7 A recent international consensus conference stressed the importance of examining the potential role of smaller, compact portable US machines in the early diagnosis of traumatic abdominal injury.5
We report a combined experience with a portable 2.4-kg HH US machine in the early evaluation of trauma patients at a Canadian trauma centre and an American trauma centre. We believed it was important to evaluate the effectiveness of such a unit in a setting where the relative effectiveness of a “standard” FAST examination performed using typical floor-based US machines could provide relevance. A valid examination of any diagnostic test also depends on asking appropriate questions. FAST has been defined and used most extensively to test for free intraperitoneal fluid, which is a marker for intraperitoneal injury. Numerous studies have reported that emergentologists, radiologists and surgeons can detect intraperitoneal fluid with a high degree of accuracy.8,9,10,11,12,13,14,15 However, serious intra-abdominal injuries may occur without the presence of free intraperitoneal fluid.16,17 Our study asked, How good are both examinations at finding fluid, did this fluid correlate with injuries, and did these injuries require intervention? Blunt trauma pilot cohorts of 47 patients from Vancouver and 58 patients from Detroit, as well as a separate penetrating abdominal cohort have previously been reported.18,19,20
Methods
The Detroit Receiving Hospital (DRH) is a level I urban trauma centre. The Vancouver Hospital and Health Sciences Centre (VHHSC) is a provincial trauma centre. At both institutions, critically injured patients are resuscitated by a trauma team led by an attending trauma surgeon. FAST performed with an Acuson XP128 (Acuson Corp., Mountain View, Calif.) has been the initial screening test for blunt abdominal trauma since 1996 at the VHHSC. Senior and junior radiology residents, with a later staff review, carry out this examination. At the DRH, a Toshiba SSH 140A (Toshiba American Medical Systems, Armonk, NY) is used by the resuscitating surgical team (typically a senior surgical resident) to perform FAST. For the purposes of this study, both these examinations were designated as formal FAST (FFAST) examinations.
To evaluate the potential of HH US units during acute trauma resuscitation, HHFAST examinations were performed by an attending trauma surgeon or trauma fellow using a Sonosite 180 (Sonosite, Inc., Bothell, Wash.), 2.4-kg US machine with a 5–2 MHz curved array transducer. These were performed and interpreted as part of the initial examination and were followed by other examinations as is usual practice. Whereas HHFAST was limited to ascertaining the presence or absence of free fluid as a marker of injury, FFAST would occasionally also report impressions regarding the presence or absence of specific injuries. The original FFAST diagnosis communicated to the surgical team was considered the test result, as this was what influenced clinical decisions. HHFAST results did not influence patient care, except in unusual cases in which unstable patients had positive findings and there were delays in obtaining FFAST.
This study was approved by the human ethics committees of both participating institutions.
HHFAST images were saved as representative JPEG digital images, digital video-images with use of a video recorder (GV-D800 NTSC, Sony Corp. Japan, Tokyo) and as hard-copy using a video graphic printer (UP895MD, Sony Corp. Japan). For all patients the results of HHFAST were compared with US examinations performed with the floor-based machines (i.e., FFAST), CT studies, operative findings, autopsy studies and the hospital course. Separate test performance was calculated for the ability of HHFAST to detect free intraperitoneal fluid and to detect all intra-abdominal injuries.
The standard of comparison for intraperitoneal fluid was defined as true when fluid was reported as present on CT performed within 24 hours of admission, reported in operative notes or seen on FFAST in the case of positive HHFAST. Free fluid first detected on CT performed more than 24 hours after injury in asymptomatic patients was not considered injury-related. FFAST was considered to be the accurate test in comparison with HHFAST. Intra-abdominal injury was defined as one comprising any intra-abdominal lesion of a traumatic nature as defined by Chiu and associates.16 Retroperitoneal hematoma, abdominal wall disruption and unexpected free intraperitoneal fluid seen within 24 hours of injury were also considered to be significant intra-abdominal injuries. Indeterminate studies were defined as those in which the sonographer could not definitively judge the results as either positive or negative for fluid as defined by Boulanger and colleagues.21 Indeterminate scans and cases of equipment failure were excluded from the test performance calculations of the diagnostic accuracy for free fluid and intra-abdominal injury but were considered as diagnostic failures when assessing patients requiring interventions.
Data on patient demographics, physiologic status and HHFAST sonographer and sonographic findings were collected prospectively with the use of standardized forms. The ultimate hospital course was determined by collating demographic information recorded in the British Columbia Trauma Registry with a complete hospital chart review. Complete data on the outcomes of the Detroit patients were available from the institutional trauma registry. Data were manually entered into an Excel database (Microsoft Corp., Redmond, Wash.). Test performance characteristics were defined as described by Sackett and colleagues.22 Statistical calculations were performed using Stata 7.0 (Stata Corp., College Station, Tex.). Group means were compared using the t test, proportions using either the χ2 or Fisher's exact test. Confidence intervals (95%) were calculated with use of exact statistics.
Results
Three hundred and twenty-eight victims of blunt trauma were examined during trauma resuscitations: 58 in Detroit and 270 in Vancouver. Although all had physical examination, 15 patients were either not examined by HHFAST because of battery exhaustion (5), a missing 5–2-MHz probe (3) or had indeterminate findings (7). In addition, 281 underwent FFAST; of these, the findings were indeterminate in 7. Of the 274 FFAST examinations interpreted, 58 were performed by surgical residents at DRH and 216 by radiology residents at VHHSC. CT was carried out according to the clinical protocol at each centre; 54% of all the HHFAST patients and 57% of all FFAST patients had thoracoabdominal CT. Overall, there was a significantly greater use of CT at VVHSC (174 of 270) than at DRH (7 of 58) (p < 0.001).
The mean age was 38.9 (standard deviation [SD] 17.5) years (ranging from 1–59 yr). The DRH patients were younger than those at the VHHSC (34.1 v. 39.9 yr, p = 0.03). The mean (SD) Injury Severity Score was 17.3 (14.7); VHHSC patients had a significantly higher score than DRH patients (19.0 v. 8.5, p < 0.001); 74% were male and 26% were female. All patients had blunt injury: motor vehicle crashes, 45%; falls, 16%; pedestrians struck by vehicles, 12%; assaults, 6%; bicycle crashes, 5%; crush injuries, 4%; motorcycle crashes, 4%; snow-boarding crashes, 3%; skiing injury, 1.5%; airplane crashes, 1%; blasts, 1%; all-terrain-vehicle crashes, 1%; and skateboarding injury, 0.3%.
Free intraperitoneal fluid
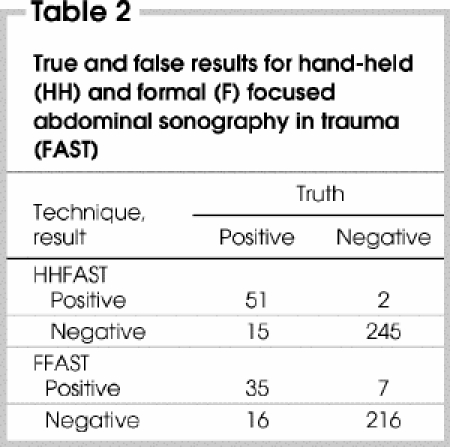
HHFAST was highly accurate for detecting intraperitoneal fluid: of 313 patients with determinate results, 296 were correctly classified. Of the 66 patients who were designated positive by FFAST, HHFAST identified 51 with intraperitoneal fluid, for a sensitivity of 77%. A positive HHFAST result was highly specific for the true presence of fluid, with only 2 of 247 (0.8%) results being false positive, and a nearly 100-fold likelihood ratio of a positive test (Table 1). Although not designed as a formal comparison between the 2 techniques, FFAST performed with accuracy comparable to HHFAST (a correct diagnosis in 251 of 274 patients tested) (Table 2). Overall, FFAST was slightly less sensitive: 35 (69%) of 51 patients were identified with free fluid according to the standard of comparison. However, a negative FFAST was highly specific for the absence of fluid: 216 (97%) of 223 patients were correctly excluded (Table 1). Significantly more diagnostic errors were made at the VHHSC using HHFAST (p = 0.031) than at the DRH, and there was a trend toward this for the FFAST (p = 0.058). There was no difference in the rate of misdiagnoses between the clinicians performing HHFAST (p = 1.0).
Table 1
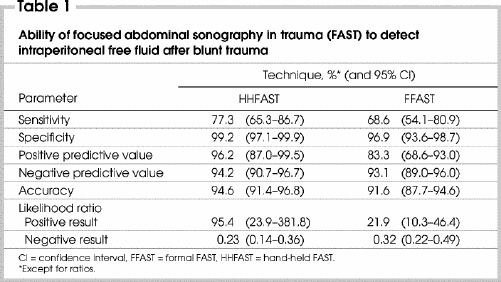
Table 2
In 2 patients, CT revealed small amounts of free fluid, despite negative HHFAST and FFAST findings, and the results in these patients were thus considered as false negative. One 37-year-old woman, who was struck by a car, had a small amount of periportal edema that was officially reported to be “consistent with fluid resuscitation” on CT performed 13 hours after HHFAST and FFAST gave negative results. Another 21-year-old woman involved in a motor vehicle collision had a small amount of fluid in the pelvis, reported as “physiologic” on CT performed 3 hours after HHFAST and FFAST were found to be negative. Both patients were managed successfully with serial examination and had an uncomplicated hospital stay.
Intraperitoneal injuries
The sensitivity was markedly decreased when FAST was asked to detect all intraperitoneal injuries. HHFAST had an overall sensitivity of 64% for detecting injuries (51 of 80 patients) and an overall accuracy of 90% (282 of 313 patients) (Table 3). Positive HHFAST examinations were still highly predictive of intra-abdominal injuries, with a positive predictive value of 96% (51 of 53 positive results being true [Table 4]), and a likelihood ratio of a positive test being 74. Likewise, FFAST also had a reduced sensitivity of 52% in detecting positive cases (35 of 67 cases) and an overall accuracy of 86% (235 of 274). A positive test carried a positive predictive value of 83% (35 of 42 cases being true [Table 4]) and a likelihood ratio of a positive test of 15 (Table 3). There were more missed injuries at the VHHSC than at the DRH (p = 0.015). There was no significant difference in the missed injuries between clinicians performing HHFAST (p = 0.3). However, there were significantly more misdiagnoses by FFAST at the VVHSC than at the DRH (p < 0.01).
Table 3
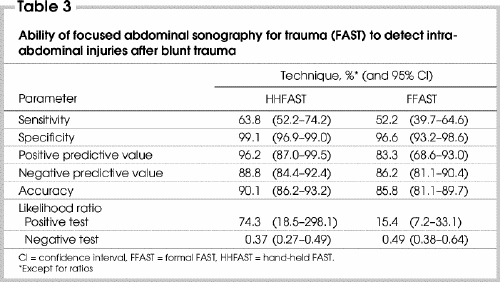
Table 4

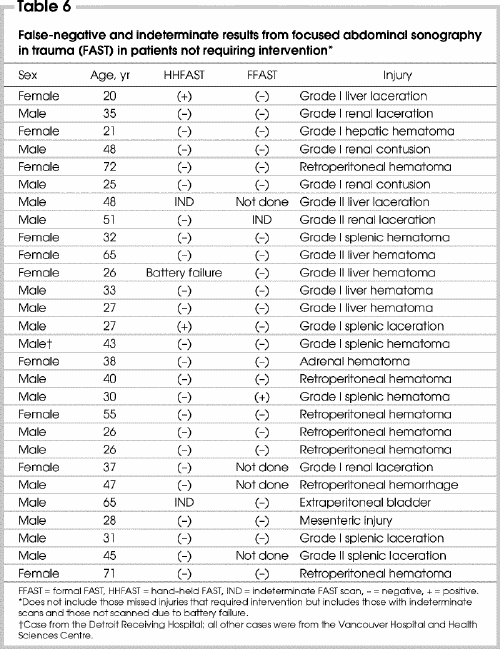
Patients requiring therapeutic intervention
Of the 270 patients who had HHFAST, 40 required therapeutic interventions: 37 laparotomies and 4 angioembolizations (1 patient requiring both). In 32 patients, HHFAST detected the complication leading to the intervention, for a detection rate of 80%. Of the remaining 8 (20%, including indeterminate) in which HHFAST did not detect the complication, only 1 was from the DRH (Table 5). There were 31 cases in the FFAST cohort who required a therapeutic intervention: 29 laparotomies and 3 angioembolizations (1 patient requiring both). FFAST detected the condition in 20 patients (64%), but did not detect the condition in 11 patients (36%). In 26 patients, despite a “negative” or indeterminate FAST scan, intra-abdominal injuries were found that did not require therapeutic intervention. Only 1 of these patients was from the DRH (Table 6).
Table 5
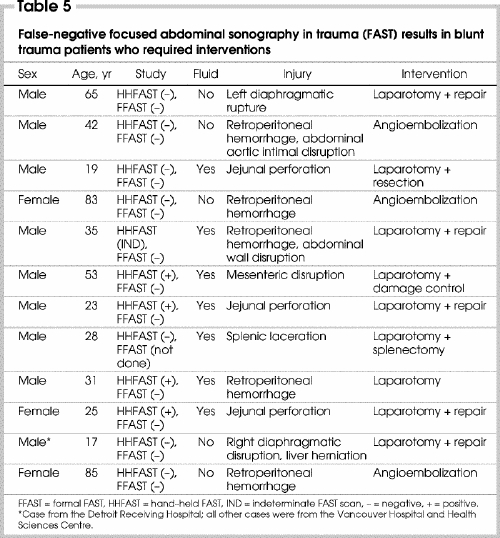
Table 6
Discussion
The goal of FAST examination, as defined by a recent international consensus conference, is to detect free intraperitoneal fluid as a marker of injury.5 In current practice, trauma US has taken on 2 congruous yet distinct roles. One is the early identification of unstable trauma victims requiring urgent surgical intervention,23,24 and the other newer, potentially controversial, role is that of excluding stable patients from further abdominal imaging.9,15,25,26,27 Institutional trauma protocols at both the DRH and the VHHSC have accepted FAST's ability to do both; thus, unstable patients with positive FAST results are operated on, and stable patients with negative FAST results tend to be observed, depending on the US findings and clinical examination. In our study, we examined the validity of this practice and evaluated the role of HHFAST.
Whether used to detect intraperitoneal fluid or as a screening test for all intra-abdominal injuries, the likelihood ratios indicated that both HHFAST and FFAST were valuable tests when the result was positive. Likelihood ratios are thought to give a better assessment of the value of a diagnostic test than the sensitivity, specificity, positive and negative predictive value, and accuracy.28 As a rough guide, likelihood ratios greater than 10 or less than 0.1 typically generate large and often conclusive changes from pre-test to post-test probability.28,29 HHFAST could quickly confirm the presence of intraperitoneal fluid in the majority (80%) of those who required therapeutic intervention. After a patient was examined with this portable device, the examiner had correctly classified the patient into a group with or without free fluid in 95% of cases, and into one with or without injury in 90% of cases. Likelihood ratios of a positive test of 95 and 83, and a positive predictive values of 96%, respectively, for fluid and injury, using HHFAST as a continuation of the physical examination, extend the clinician's diagnostic power. Further, HHFAST can be repeated on any subsequent examination, without side effects, contrast, transport or interference with other clinical activities. Simply, when the examiners saw fluid they could be very confident that it was present, and thus triage the patient toward either surgery or CT depending on the patient's status.
This study was hospital based, but the technology could easily be carried to the scene of the trauma. Hemorrhage accounts for approximately 40% of all deaths in trauma patients30,31 and is the greatest cause of post-traumatic operating room deaths.32 The risk of victims dying from injuries sustained in vehicular collisions is much greater for those injured in rural as opposed to urban settings,33,34 sometimes by more than 50%.35 A larger proportion of fatalities occur outside the hospital and within the first hour after injury in rural areas.34 The diagnosis of such injuries is time-dependent and critical. HHFAST is extremely portable and has been tested in prehospital settings, including air transport systems36 and on a commercial ski hill.37 Prehospital transport should never be unnecessarily delayed, but a prehospital HHFAST might provide important triage information. A massive hemoperitoneum can quickly be detected with a single view of Morrison's pouch in 82%–90% of hypotensive patients with an abdominal source,23,24 requiring on average 19 seconds to determine.23 This might differentiate a patient with a massive hemoperitoneum who might respond to a damage control intervention at a smaller sending site from one with a severe retroperitoneal hemorrhage that will require angiography at a referral centre. Such an image might be locally or remotely interpreted, yet be critically important in triage and transport decisions.
Clinicians need to be keenly aware of the limitations of trauma sonography. It is a very user dependant technique. FAST may miss injuries that are not associated with free intraperitoneal fluid, no matter who performs it, or with which device (HHFAST or FFAST). The sensitivities for detecting all intraperitoneal injuries were 65% and 52%, respectively, for both examinations. As a test that looks for free intraperitoneal fluid, this is a known limitation of the FAST technique. FAST is not expected to detect injuries that may not be associated with intraperitoneal fluid, such as hollow viscus, mesenteric, intraparenchymal, solid or retroperitoneal injuries.12,16,17,38 There were 12 patients in the group requiring intervention who did not have their injuries detected by FAST. The causes included diaphragmatic and hollow viscus injuries, injuries that are also often missed on CT.
Further aspects of study validity relate to the question of verification bias, wherein the results of the test influence the decision to perform the standard test.29,39 Verification bias was present in this study, as well as being a general methodologic concern in other large contemporary series that have relied on clinical follow-up, and have not otherwise subjected stable patients to a standard diagnostic imaging test.9,12,14,15,25,40 Although more than one-half of the patients had CT, there were likely further missed injuries that were occult and not known about in the “true negative” patients not having CT. There were more errors at the VHHSC than at the DRH. Although this may have been related to sonographic experience, we believe it is more likely related to the higher acuity of injury at VHHSC, as well as the greater frequency of CT. Overall, other such imaging and follow-up revealed 33 “ultrasound occult” injuries in the HHFAST group, all but 2 being at the VHHSC. Eight of these injuries (including 1 indeterminate) were serious and required therapeutic intervention. Twenty-six were minor and likely would have caused no morbidity if they were not detected. In experienced hands, a US examination can identify specific parenchymal injuries,25,41,42,43,44 generally finding a greater sensitivity the higher the injury grade for both hepatic and splenic injuries.42,43 However, some of these studies have relied on the presence of a separate sonographer,25,42,43 potentially reducing the availability of the test in many clinical settings. We believe that the emphasis of the FAST technique should remain its simplicity, which as an initial screening technique is meant to be within the capabilities of an on-site clinician.
In this study we wanted to evaluate the philosophy of using hand-held US early in the resuscitation of patients with blunt trauma. With the current pace of technologic development and with commercial pressure it is almost assured that lighter and cheaper units with better batteries and greater informatic capabilities will become increasingly available. The primary benefit of these devices for trauma care providers will be earlier examinations, potentially even in the prehospital setting to expedite transport and disposition. HHFAST accurately facilitates this diagnostic algorithm, so cheaper, smaller, lighter devices should be further studied.
Conclusions
The HHFAST constitutes another dimension of the physical examination of patients with abdominal trauma. It is a very accurate test for detecting significant intraperitoneal free fluid. It can often quickly localize major intraperitoneal injury and thus expedite exploration of the abdominal cavity in unstable patients, as well as confirm serious intraperitoneal injury requiring further delineation in stable patients. It is less accurate for detecting all abdominal injuries and should be considered a complementary imaging technique for surgical decision-making when the result is positive. Negative studies should be supplemented with CT rather than relying on further US in seriously injured patients.
Acknowledgments
We thank the Heathcliffe Foundation, Vancouver, BC, for an unrestricted educational grant; the Sonosite Corporation, Bothell, Wash., for the loan of a Sonosite-180 hand-held ultrasound machine; Sharon Kasic, Manager, and Claire Adjoran-Byrne, Programmer, British Columbia Trauma Registry, Vancouver, BC; Kathy Rishell, Trauma Program Coordinator, and Karla R Price, Trauma Program Specialist, Detroit Receiving Hospital, Detroit, Mich.; and Marcia Lepore, Administrative Assistant, Trauma Services, Vancouver, BC.
Presented at the annual scientific meeting of the Trauma Association of Canada, Banff, Alta., Mar. 28, 2003.
Competing interests: None declared.
Correspondence to: Dr. Andrew W. Kirkpatrick, Foothills Medical Centre, 1403–29th St. NW, Calgary AB T2N 2T9; fax 403 944-1277; andrew.kirkpatrick@calgaryhealthregion.ca , andykirk@shaw.ca
Accepted for publication Aug. 3, 2004.
References
- 1.Fabian TC, Croce MA. Abdominal trauma, including indications for celiotomy. In: Feliciano DV, Moore EE, Mattox KL, editors. Trauma. 3rd ed. Stamford (CT): Appelton & Lange; 1996. p. 41-59.
- 2.Boulanger BR, McLellan BA. Blunt abdominal trauma. Emerg Med Clin North Am 1996;14:151-71. [DOI] [PubMed]
- 3.Wilson CB, Vidrine A, Rives JD. Unrecognized abdominal trauma in patients with head injuries. Ann Surg 1965;161:608-13. [DOI] [PMC free article] [PubMed]
- 4.Rodriguez A, DuPriest RW Jr, Shatney CH. Recognition on intra-abdominal injury in blunt trauma victims. A prospective study comparing physical examination with peritoneal lavage. Am Surg 1982;48:457-9. [PubMed]
- 5.Scalea TM, Rodriguez A, Chiu WC, Brenneman FD, Fallon WF, Kato K, et al. Focused assessment with sonography for trauma (FAST): results from an international consensus conference. J Trauma 1999;46:466-72. [DOI] [PubMed]
- 6.Boulanger BR, Kearney PA, Brenneman FD, Tsuei B, Ochoa J. FAST utilization in 1999: results of a survey of North American trauma centers. Am Surg 2000;66:1049-55. [PubMed]
- 7.Wherry DC. Potential of a hand-held ultrasound in asessment of the injured patient. Cardiovasc Surg 1998;6:569-72. [DOI] [PubMed]
- 8.Ma OJ, Mateer JR, Ogata M, Kefer MP, Wittman D, Aprahamian C. Prospective analysis of a rapid trauma ultrasound examination performed by emergency physicians. J Trauma 1995;38:879-85. [DOI] [PubMed]
- 9.Lingawi SS, Buckley AR. Focused abdominal US in patients with trauma. Radiology 2000;217:426-9. [DOI] [PubMed]
- 10.Mandavia DP, Aragona J, Chan L, Chan D, Henderson SO. Ultrasound training for emergency physicians — a prospective study. Acad Emerg Med 2000;7:1008-14. [DOI] [PubMed]
- 11.Lanoix R, Leak LV, Gaeta T, Gernsheimer JR. A preliminary evaluation of emergency ultrasound in the setting of an emergency training program. Am J Emerg Med 2000;18:41-5. [DOI] [PubMed]
- 12.Hoffmann R, Nerlich M, Muggia-Sullam M, Pohlemann T, Wippermann B, Regel G, et al. Blunt abdominal trauma in cases of multiple trauma evaluated by ultrasonography: a prospective analysis of 291 patients. J Trauma 1992;32:452-8. [DOI] [PubMed]
- 13.Kimura A, Otsuka T. Emergency center ultrasonography in the evaluation of hemoperitoneum: a prospective study. J Trauma 1991;31:20-3. [DOI] [PubMed]
- 14.Rozycki GS, Ballard RB, Feliciano DV, Schmidt JA, Pennington SD. Surgeon-performed ultrasound for the assessment of truncal injuries. Ann Surg 1998;228:557-67. [DOI] [PMC free article] [PubMed]
- 15.Boulanger BR, McLellan BA, Brenneman FD, Ochoa J, Kirkpatrick AW. Prospective evidence of the superiority of a sonography-based algorithm in the assessment of blunt abdominal trauma. J Trauma 1999;47:632-7. [DOI] [PubMed]
- 16.Chiu WC, Cushing BM, Rodriguez A, Ho SM, Mirvis SE, Shanmuganathan K, et al. Abdominal injuries without hemoperitoneum: a potential limitation of focused abdominal sonography for trauma (FAST). J Trauma 1997;42:617-25. [DOI] [PubMed]
- 17.Shanmuganathan K, Mirvis SE, Sherbourne CD, Chiu WC, Rodriguez A. Hemoperitoneum as the sole indicator of abdominal visceral injuries: a potential limitation of screening abdominal US for trauma. Radiology 1999;212:423-30. [DOI] [PubMed]
- 18.Kirkpatrick AW, Simons RK, Brown DR, Ng AK, Nicolaou S. Digital hand-held sonography utilised for the focused assessment with sonography for trauma: a pilot study. Ann Acad Med Singapore 2001;30:577-81. [PubMed]
- 19.Kirkpatrick AW, Sirois M, Ball CG, Laupland KB, Goldstein L, Hameed M, et al. The hand-held ultrasound examination for penetrating abdominal trauma. Am J Surg 2004;187:660-5. [DOI] [PubMed]
- 20.Kirkpatrick AW, Simons RK, Brown DR, Nicolaou S, Dulchavsky S. The hand-held FAST: experience with hand-held trauma sonography in a level-I urban trauma center. Injury 2002;33:303-8. [DOI] [PubMed]
- 21.Boulanger BR, Brenneman FD, Kirkpatrick AW, McLellan BA, Nathens AB. The indeterminate abdominal sonogram in multisystem blunt trauma. J Trauma 1998;45:52-6. [DOI] [PubMed]
- 22.Sackett DL, Haynes RB, Guyatt GH, Tugwell P, editors. Clinical epidemiology: a basic science for clinical medicine. 2nd ed. Boston: Little, Brown and Company; 1991. p. 69-152.
- 23.Wherrett LJ, Boulanger BR, McLellan BA, Brenneman FD, Rizoli SB, Culhane J, et al. Hypotension after blunt abdominal trauma: the role of emergent abdominal sonography in surgical triage. J Trauma 1996;41:815-20. [DOI] [PubMed]
- 24.Rozycki GS, Ochsner MG, Feliciano DV, Thomas B, Boulanger BR, Davis FE, et al. Early detection of hemoperitoneum by ultrasound examination of the right upper quadrant: a multicenter study. J Trauma 1998;45:878-83. [DOI] [PubMed]
- 25.McKenney MG, Martin L, Lentz K, Lopez C, Sleeman D, Aristide G, et al. 1,000 consecutive ultrasounds for blunt abdominal trauma. J Trauma 1996;40: 607-12. [DOI] [PubMed]
- 26.McKenney MG, McKenney KL, Hong JJ, Compton R, Cohn SM, Kirton OC, et al. Evaluating blunt trauma with sonography: a cost analysis. Am Surg 2001;67:930-4. [PubMed]
- 27.Bode PJ, Edwards MJ, Kruit MC, van Vugt AB. Sonography in a clinical algorithm for early evaluation of 1671 patients with blunt abdominal trauma. AJR Am J Roentgenol 1999;172:905-11. [DOI] [PubMed]
- 28.Henteleff H, for Members of the Evidence Based Reviews in Surgery. Canadian Association of General Surgeons/L'Association Canadienne des chirurgiens généraux evidence based Reviews in Surgery. Methodological review December 2002. Toronto: Canadian Association of General Surgeons; 2002.
- 29.Jaeschke R, Guyatt GH, Sackett DL. User's guides to the medical literature. III. How to use an article about a diagnostic test. B: What are the results and will they help me in caring for my patient? JAMA 1994;271:703-7. [DOI] [PubMed]
- 30.Sauaia A, Moore FA, Moore EE, Moser KS, Brenan R, Read PA, et al. Epidemiology of trauma death: a reassessment. J Trauma 1995;38:185-93. [DOI] [PubMed]
- 31.Gofrit ON, Leibovici D, Shapira SC, Shemer J, Stein M, Michaelson M. The trimodal death distribution of trauma victims: military experience from the Lebanon War. Mil Med 1997;162:24-6. [PubMed]
- 32.Hoyt DB, Bulger EM, Knudson MM, Morris J, Ierardi R, Sugerman HJ, et al. Death in the operating room: an analysis of a multi-center experience. J Trauma 1994;37:426-32. [PubMed]
- 33.Baker SP, Whitfield RA, O'Neill B. Geographic variation in mortality from motor vehicle crashes. N Engl J Med 1987;316: 1384-7. [DOI] [PubMed]
- 34.Mueller BA, Rivara FP, Bergman AB. Urban-rural location and the risk of dying in a pedestrian-vehicle collision. J Trauma 1988;28:91-4. [DOI] [PubMed]
- 35.Grossman DC, Kim A, MacDonald SC, Klein P, Copass MM, Maier RV. Urban-rural differences in prehospital care of major trauma. J Trauma 1997;42:723-9. [DOI] [PubMed]
- 36.Price DD, Wilson SR, Murphy TG. Trauma ultrasound feasibility during helicopter transport. Air Med J 2000;19:144-6. [DOI] [PubMed]
- 37.Kirkpatrick AW, Brown DR, Crickmer S, Mohr BP, Hamilton DR, Cunningham J, et al. Hand-held portable sonography for the on-mountain exclusion of a pneumothorax. Wilderness Environ Med 2001; 12: 270-2. [DOI] [PubMed]
- 38.Miller MT, Pasquale MD, Bromberg WJ, Wasser TE, Cox J. Not so FAST. J Trauma 2003;54:52-60. [DOI] [PubMed]
- 39.Archibald S, Bhandari M, Thoma A; Evidence-Based Surgery Working Group. Users' guides to the surgical literature: how to use an article about a diagnostic test. Evidence-Based Surgery Working Group [published erratum apperars in Can J Surg 2001;44:467] [see comment] Can J Surg 2001;44:17-23. Comment in: Can J Surg 2001;44(4):247-9. [PMC free article] [PubMed]
- 40.Branney SW, Moore EE, Cantrill SV, Burch JM, Terry SJ. Ultrasound based key clinical pathway reduces the use of hospital resources for the evaluation of blunt abdominal trauma. J Trauma 1997;42: 1086-90. [DOI] [PubMed]
- 41.Ohta S, Hagiwara A, Yukikoa T, Ohta S, Ikegami K, Matsuda H, et al. Hyperechoiec appearance of hepatic parenchyma on ultrasound examination of patients with blunt hepatic injury. J Trauma 1998; 44:135-8. [DOI] [PubMed]
- 42.Richards JR, McGahan JP, Pali MJ, Bohnen PA. Sonographic detection of blunt hepatic trauma: hemoperitoneum and parenchymal patterns of injury. J Trauma 1999;47:1092-7. [DOI] [PubMed]
- 43.Richards JR, McGahan JP, Jones CD, Zhan S, Gerscovich EO. Ultrasound detection of blunt splenic injury. Injury 2001;32:95-103. [DOI] [PubMed]
- 44.Stengel D, Bauwens K, Sehouli J, Nantke J, Ekkernkamp A. Discriminatory power of 3.5 MHz convex and 7.5 MHz linear probes for the imaging of traumatic splenic lesions: a feasibility study. J Trauma 2001;51:37-43. [DOI] [PubMed]


