Abstract
Background
The Canadian Task Force on Preventive Health Care has recommended the use of annual or biennial fecal occult blood testing (FOBT) and flexible sigmoidoscopy in the periodic health examination of asymptomatic people over 50 years of age. Therefore, we decided to ascertain the current colorectal cancer (CRC) screening practices and attitudes of surgeons, gastroenterologists and internists.
Methods
In June 2002 (with a final mailing in December 2002), a questionnaire was sent to all gastroenterologists, internists and surgeons in Alberta. It included items on demographic and practice characteristics, CRC screening practices and opinions about CRC screening.
Results
Responses were received from 42 gastroenterologists, 83 internists and 68 surgeons. Overall, 141 of 187 respondents (75.4%, 95% confidence interval [CI] 68.6%–81.4%) recommended that average-risk adults undergo CRC screening. Internists were less likely to recommend screening than either gastroenterologists or surgeons (95% CI for the difference 7.2%–32.8%). The most commonly recommended screening test was colonoscopy (70%), followed by FOBT (65%), flexible sigmoidoscopy (47%) and air-contrast barium enema (31%). Colonoscopy was the only test recommended by 7 (22.6%) of 33 gastroenterologists, 9 (16.4%) of 59 surgeons and 3 (6.1%) of 49 internists. Respondents were more likely to list barriers to the use of colonoscopy (mean 5 barriers) for screening than for either FOBT or flexible sigmoidoscopy (mean 2 barriers for both tests). Only 3 respondents indicated that they themselves would not undergo screening. Colonoscopy was the only screening test that 135 (70.0%) of the 193 would themselves undergo.
Conclusions
The majority of Alberta specialists recommend CRC screening for average-risk adults. Colonoscopy was the most commonly recommended test, despite the perception of more barriers to that technique and the 2001 guidelines prepared by the Canadian Task Force for Preventive Health Care, which did not support colonoscopy.
Abstract
Contexte
Le Groupe d'étude canadien sur les soins de santé préventifs a recommandé l'utilisation annuelle ou bisannuelle de l'analyse du sang occulte dans les matières fécales (SOMF) et une sigmoïdoscopie flexible lors de l'examen de santé périodique de personnes asymptomatiques âgées de plus de 50 ans. Nous avons alors décidé de vérifier les pratiques actuelles de dépistage du cancer colorectal (CCR) et les attitudes des chirurgiens, des gastro-entérologues et des internistes.
Méthodes
En juin 2002, on a fait parvenir un questionnaire à tous les gastro-entérologues, internistes et chirurgiens en Alberta (avec un envoi final en décembre 2002). Il comprenait des questions sur les caractéristiques démographiques et de pratique, sur les pratiques de dépistage du CCR et sur leurs opinions à ce sujet.
Résultats
Nous avons reçu des réponses de 42 gastro-entérologues, 83 internistes et 68 chirurgiens. Dans l'ensemble, 141 des 187 répondants (75,4 %, intervalle de confiance à 95 % [IC] 68,6 %–81,4 %) ont recommandé que les adultes à risque moyen subissent un dépistage du CCR. Les internistes ont recommandé moins souvent ce dépistage que les gastro-entérologues ou les chirurgiens (IC à 95 % pour l'écart 7,2 %–32,8 %). La coloscopie a été le plus souvent recommandée (70 %), suivie par l'analyse SOMF (65 %), la sigmoïdoscopie flexible (47 %) et le lavement baryté à contraste aérique (31 %). La coloscopie a été le seul dépistage recommandé par 7 (22.6 %) des 33 gastro-entérologues, par 9 (16.4 %) des 59 chirurgiens et par 3 (6.1 %) des 49 internistes. Les répondants ont été plus nombreux à indiquer les obstacles à l'utilisation de la coloscopie (moyenne de cinq obstacles) pour le dépistage que pour l'analyse SOMF ou la sigmoïdoscopie flexible (moyenne de deux obstacles pour les deux tests). Seulement trois répondants ont indiqué qu'ils ne subiraient pas eux-mêmes un dépistage. La coloscopie a été le seul test de dépistage que 135 (70.0 %) des 193 répondants subiraient eux-mêmes.
Conclusions
La majorité des spécialistes albertains recommandent le dépistage du CCR pour les adultes à risque moyen. La coloscopie a été le test le plus souvent recommandé malgré l'impression d'un plus grand nombre d'obstacles pour cette technique et les lignes directrices générales de 2001 du Groupe d'étude canadien sur les soins de santé préventifs, qui n'appuient pas la coloscopie.
There is growing emphasis on colorectal cancer (CRC) screening. In 2001, the Canadian Task Force on Preventive Health Care concluded that there is good evidence to include annual or biennial fecal occult blood testing (FOBT) and fair evidence to include flexible sigmoidoscopy in the periodic health examination of asymptomatic people over 50 years of age.1 This followed the lead set by other professional societies, organizations and cancer agencies.2,3,4,5,6 However, the Canadian guidelines differed from many others,2,3 in not including colonoscopy as an option for primary screening of average-risk people. Subsequently, the National Committee on Colorectal Cancer, constituted by Health Canada, recommended a population-based screening program using FOBT in Canada.7
Despite guidelines since the mid-1990s that have recommended CRC screening, screening rates for CRC have changed little and lag behind other established cancer screening tests.8,9,10,11 Physician recommendation is a strong predictor of the acceptance of mammography, the Papanicolaou test and prostate-specific-antigen testing12,13,14 and is the strongest predictor of patient acceptance of CRC screening, regardless of patient preference for a particular screening modality.15 Specialists play an important role as opinion leaders and as providers of most flexible sigmoidoscopy and colonoscopy services for either primary screening or diagnostic follow-up.
The purpose of this study was to determine current screening practices of specialists relevant to CRC screening, including gastroenterologists, other internists and surgeons. An important current debate is between those who favour screening by colonoscopy to ensure complete visualization of the colon versus those who favour more limited evaluation by FOBT or flexible sigmoidoscopy. Therefore, we focused on specialists' use of and attitudes toward these 3 screening tests. We were especially interested in how specialists' screening practices were influenced by their attitudes toward CRC screening and the 2001 Canadian Task Force guidelines. Finally, we wished to understand what barriers they perceived to CRC screening using the different tests.
The study was approved by the Conjoint Health Research Ethics Board of the University of Calgary.
Methods
Survey sample
All gastroenterologists, other internists, and surgeons were selected from the list of physicians licensed by the College of Physicians and Surgeons of Alberta in April 2002. The database included physician practice addresses, telephone and fax numbers and up to 3 medical specialties. All specialists (internal medicine, general surgery) in Canada have been certified as such by the Royal College of Physicians and Surgeons of Canada. Subspecialty designation within the College of Physicians and Surgeons' list can be incomplete. Therefore, a manual search of the list was performed by one of us (R.J.H.), and those who were known to be gastroenterologists but were classified by the College only as internists were reclassified as gastroenterologists for the purpose of this study. To establish the relevance of CRC screening to each of the subspecialty groups, we initially included all internal medicine specialists. Subsequently, we excluded subspecialties for which respondents indicated that CRC screening was not relevant. Subspecialties excluded in this way included cardiology, endocrinology and metabolism, clinical immunology and neurology.
Survey process and content
The initial mailing was sent in June 2002, with follow-up in December 2002. Each mailing included a coded survey, cover letter and stamped return envelope. The Clinical Practice Guideline (CPG) Program of the Alberta Medical Association endorsed the survey and signed a joint cover letter with the investigators encouraging physicians to participate. Three follow-up mailings were sent to non-respondents. For the final mailing, we enclosed an abbreviated questionnaire that included 7 key questions about screening practices, attitudes and perceived barriers to CRC screening.
The questionnaire included items on demographic and practice characteristics, CRC screening practices and knowledge and opinions about CRC screening. We provided definitions of average risk and screening. Average risk was defined as referring “to a person without a personal or family history of adenomatous polyps or colorectal cancer and without a condition (i.e., ulcerative colitis) that would predispose them to the development of colorectal cancer.” Screening was defined as “the use of a test for a person without symptoms or signs of colorectal cancer.”
Analysis
Missing values have been excluded from the analysis in all percentages reported. Responses to opinion questions were collapsed into agree (strongly agree and agree), uncertain and disagree (disagree, strongly disagree). Associations between categorical variables were tested using Fisher's exact test.
Results
Sample
The response rate for gastroenterologists, internists and surgeons was 83.3%, 35.1% and 57.4%, respectively, after excluding those who were unreachable, retired or dead or for whom the topic was not relevant. Of the returned and completed surveys, 186 (96%) were the full questionnaire and 7 (4%) were the abbreviated questionnaire. The final sample comprised 42 gastroenterologists, 83 internists and 68 surgeons. The demographic and practice characteristics of the sample are shown in Table 1. Flexible sigmoidoscopy (at least 1/wk over the past 12 mo) was performed by 83.3% of gastroenterologists, 60.9% of surgeons but only 7.2% of internists. Of those performing flexible sigmoidoscopy, 79.5% performed 1–5/wk. None reported performing more than 15/wk. Colonoscopy (at least 1/wk over the past 12 mo) was performed by 95.2% of gastroenterologists, 57.8% of surgeons and 6.0% of internists. Of those performing colonoscopy, 22.5% performed 1–5/wk, 18.8% performed more than 15/wk and the remainder performed 6–15/wk. Of those performing more than 15/wk, 80% were gastroenterologists and 20% were surgeons. Only 12.5% of those who performed flexible sigmoidoscopy did not also perform colonoscopy.
Table 1

Familiarity with the 2001 Canadian Task Force guidelines
Overall, 108 of 190 (56.8%, 95% confidence interval [CI] 49.5%–64.0%) specialists who responded indicated that they were familiar with the 2001 Canadian Task Force for Preventive Health Care guidelines on CRC screening. Eighty-four specialists rated the guidelines as not useful, useful or very useful. Of these, only 11 (13.1%) found them very useful (95% CI 6.7%–22.2%); 35% of gastroenterologists found the guidelines not useful compared with 8% and 9% of internists and surgeons, respectively.
Attitudes toward CRC screening
Only 7 (3.6%) of the 193 specialists disagreed with the statement that CRC screening was beneficial. Thirty (15.5%) were uncertain about the benefit. Although 97 (50.5%) of 192 who responded believed CRC screening was cost-effective, 81 (42.2%) were uncertain. A majority (75.3%) believed that inconsistent guidelines about CRC screening made it difficult to decide which tests patients should undergo. Furthermore, 109 (59.6%) of 183 who responded did not believe that resources were adequate in their health region for the implementation of CRC screening (item included in full questionnaire only).
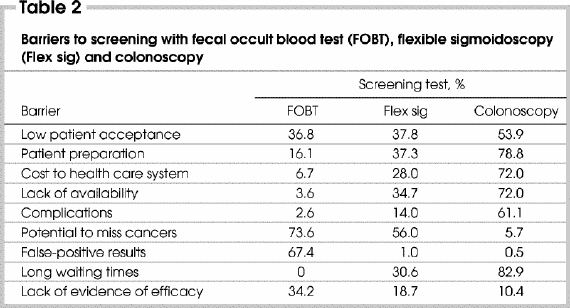
Potential barriers to the use of the screening tests are shown in Table 2. The median number of barriers respondents indicated for FOBT was 2 (range from 0–6), for flexible sigmoidoscopy was 2 (range from 0–8) and for colonoscopy was 5 (range from 0–8). Only 22 (11.6%) of 190 specialists who responded rated the FOBT as a very good or excellent screening test. The respondents rarely used FOBT, as 72% indicated that they did not order any FOBT in an average week.
Table 2
Screening of average-risk people for CRC
Fig. 1 shows the proportion for each specialty of those who recommended that average-risk adults undergo CRC screening. Internists were less likely to recommend screening than the other 2 groups (63.6%, 95% CI for the difference 7.2%–32.8%, p = 0.003).
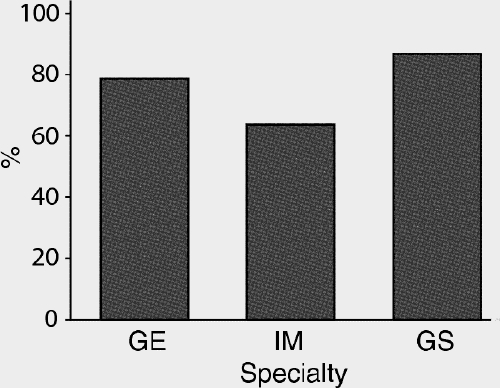
FIG. 1. Proportion of respondents for each of the 3 specialties who recommended screening for colorectal cancer in asymptomatic average-risk people over 50 years of age. GE = gastroenterology, IM = internal medicine, GS = general surgery.
Not surprisingly, those who agreed or strongly agreed that CRC screening was beneficial were more likely to recommend screening than those who did not agree or were uncertain (88.6% v. 21.6%, 95% CI for the difference 52.8%–81.2%, p < 0.001). A belief in the cost-effectiveness of CRC screening was also associated with screening recommendation, but the absolute difference between screeners and non-screeners was not as marked (89.0% v. 62.1%, 95% CI for the difference 15.2%–38.6%, p < 0.001). Other factors, including the age, sex and health region of the specialist, familiarity with the Canadian Task Force guidelines and rating of FOBT as a screening test were not associated with a screening recommendation.
Most specialists (internists 83.7%, surgeons 82.8%, gastroenterologists 93.9%) recommended screening begin at age 50–59 years. However, 14.3% of internists and 17.2% of surgeons recommended starting screening at age 40–49 years.
Recommended screening tests for average-risk people are shown in Table 3. FOBT only was recommended most frequently by internists, and gastroenterologists recommended colonoscopy only most often (Fig. 2). No specialist recommended only flexible sigmoidoscopy for screening and only 1 recommended only air-contrast barium enema.
Table 3
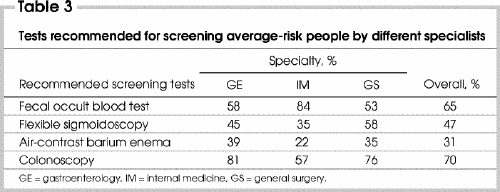
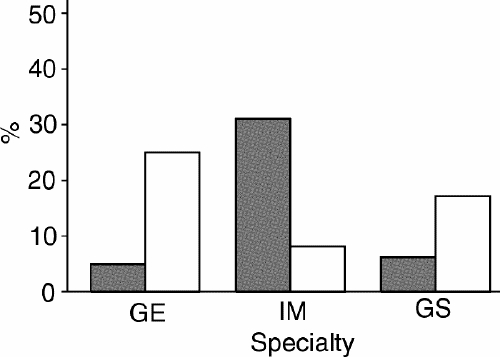
FIG. 2. Proportion of specialists recommending only colonoscopy (white columns) or only fecal occult blood testing (black columns) for colorectal cancer screening of asymptomatic average-risk people. GE = gastroenterology, IM = internal medicine, GS = general surgery.
Of those who recommended FOBT, 74 (72.6%) recommended annual testing and 18 (17.7%) recommended biennial testing. Flexible sigmoidoscopy was most commonly recommended to be repeated every 5 years. Colonoscopy was recommended to be repeated every 10 years by 82.8% of gastroenterologists, whereas internists and surgeons were more likely to recommend testing every 5 years (62.5% and 56.5%, respectively).
Colonoscopy was given as the only option for the ideal follow-up testing of a positive FOBT by 38 (90.5%) of 42 responding gastroenterologists, 46 (55.4%) of 83 internists and 44 (64.7%) of 68 responding surgeons. No gastroenterologists listed repeat FOBT as the only option for the ideal follow-up, but this was the only option given by 9 (10.8%) internists and 5 (7.4%) surgeons. Eighty-three percent of specialists routinely recommended what they considered the ideal follow-up of a positive FOBT, including those who only recommended a follow-up colonoscopy. The most common barriers given by those who did not routinely recommend their ideal follow-up up was a lack of local resources (30%) and long waiting times (37%).
Personal preferences for screening
When asked what screening method they would choose if they were to undergo CRC screening, only 3 (1.6%) of 192 responding indicated that they would not undergo screening. Colonoscopy was the only test that 135 (70.3%) of the 192 respondents would undergo, whereas only 32 (16.7%) of the 192 would undergo only FOBT.
Discussion
In this survey, we examined the practices and attitudes toward CRC screening of 3 groups of specialists. CRC screening is clearly relevant to 2 of these groups: gastroenterologists and general surgeons. These specialists provide the majority of specialized diagnostic testing and definitive surgical therapy for CRC. The third group, nongastroenterologist internists, is less commonly involved directly with the care of CRC patients. However, they are key providers of health care for common medical problems, such as hypertension and diabetes. Therefore, they are in a pivotal position to ensure that patients receive recommended preventive health care, and they act as opinion leaders for their general practice colleagues.
The response rate to our questionnaire varied, depending on the type of specialist, with a high response rate (83.3%) for gastroenterologists and a low response rate for internists (35.1%). CRC screening is likely to be directly relevant to only a small proportion of Canadian internists. Unfortunately, when creating our sampling frame, it was not possible to determine from the membership list of the College of Physicians and Surgeons of Alberta the internists to whom the subject matter would be relevant. Some physicians characterized only as “internal medicine” may limit their practice to specific areas, whereas some internists with a subspecialty designation may practise general internal medicine and may be involved in screening for and treatment of CRC. Therefore, we elected to initially send the questionnaire to all internists and then excluded those whose initial responses indicated that the subject was not of relevance to them. Responding internists are a select group and are likely biased in terms of being a group to whom CRC screening is relevant and of interest.
We found that most Alberta specialists believe that CRC screening is beneficial and recommend that adults without risk factors for CRC undergo screening. Most recommended starting screening at 50 years of age, consistent with existing guidelines. All available screening tests were recommended by at least some specialists, although the majority favoured FOBT or colonoscopy, or both. Although one might see in these data reasons to believe that specialists are heeding the recommendations of the Canadian Task Force for Preventive Health Care 2001 CRC screening guidelines, this is likely more coincidence than cause and effect. Only 56.8% of respondents were familiar with the guidelines, and familiarity with the guidelines was not associated with self-reported screening practices. Furthermore, few specialists found the guidelines very useful.
There is other evidence that Alberta specialists do not consistently follow the Canadian Task Force guidelines. The guidelines only endorsed the use of FOBT and flexible sigmoidoscopy. However, Alberta specialists also reported recommending air-contrast barium enema and colonoscopy for screening. In fact, colonoscopy was the most commonly recommended screening test. In this way, the practices of Alberta specialists are much more in keeping with the American Consortium guidelines, which support the use of all of these screening tests.2,3
The Canadian Task Force guidelines are based on the strength of existing evidence. Therefore, in the absence of randomized controlled trials or well-designed observational studies evaluating the efficacy of colonoscopy, the Canadian Task Force will not categorize colonoscopy as either an effective or ineffective screening test. In contrast the American Consortium guidelines take a much broader approach, using not only existing clinical trials but other types of evidence, including cost-effectiveness analyses.
Why is the practice of Alberta specialists not in keeping with Canadian guidelines? First, they could be unaware of current evidence supporting different screening modalities. Although knowledge about existing evidence likely varies among specialties and specialists, it is unlikely that those most involved in CRC screening, gastroenterologists and surgeons, are completely ignorant of the clinical trials supporting FOBT and the lack of clinical trials on colonoscopy. It is certainly possible that these specialists lack an appreciation of problems inherent in developing mass screening programs and are more focused on screening within their own practice rather than screening a population. On the other hand, these specialists may be willing to accept a broader range of evidence than that used by the Canadian Task Force. They may recognize that evidence from randomized controlled trials supporting colonoscopy will either not be available for many years or may never be available. This is a common problem encountered by physicians who must frequently act in the absence of this level of evidence in their clinical practice.
Specialists may also be faced with 2 types of patients who influence their screening recommendations. First, many patients ultimately rely on their physicians to make a treatment decision. In this situation, physicians may have difficulty recommending a screening option, such as FOBT, that they themselves would be unwilling to undergo. Second, Alberta specialists may be faced by patients who, for what ever reason, prefer a specific test. It is the clinical impression of one of us (R.J.H.) and many of our clinical colleagues that average-risk people are increasingly seeking screening colonoscopy. These people who have often educated themselves about CRC screening are often unwilling to consider alternative screening methods, such as FOBT or flexible sigmoidoscopy.
Despite consistently listing more barriers to the use of colonoscopy than the use FOBT, over 65% of these Alberta specialists recommended both tests. Therefore, although more barriers are commonly listed for colonoscopy (patient preparation, cost to the system, availability, long waiting times, complications), these appear not to be perceived as important as the 2 common barriers to FOBT (the potential to miss cancers and false-positive results). In other words, the accuracy of the test seems to be perceived as the most important factor in a physician's decision to recommend a given screening test.
The disconnect between Canadian guidelines and the practices and opinions of this group of physicians suggests that merely disseminating guidelines or educational material will be ineffective in changing practice, especially if the guidelines are not congruent with the physicians' beliefs. Overall, the specialists are quite accurate in their identification of the strengths and weaknesses of the various screening options. Further education regarding the tests is therefore unlikely to alter their screening behaviours. Only 10.4% of Alberta specialists indicated that a lack of evidence of efficacy was a barrier to the use of colonoscopy. Whether this means that they do not see the lack of level 1 evidence as a barrier or they believe there is strong evidence supporting its efficacy cannot be determined from the available data. Since it is unlikely that specialists are completely unaware of the evidence supporting different screening tests, further education regarding the strength of evidence is also unlikely to significantly change screening behaviours.
Our findings suggest that a CRC screening program based on FOBT or flexible sigmoidoscopy would be difficult to implement in Alberta, as those who would be viewed by general practice physicians as key opinion leaders and who provide the majority of endoscopic services are unlikely to support such a program. Indeed, in a concomitant survey of Alberta general practitioners, we found that 66% indicated that they relied on the recommendations of local specialists regarding CRC screening.16
Although there may be a growing awareness of CRC among the general population, there will remain a large proportion of the population who will not seek screening and will only be screened if their physician raises the issue or if a population-based screening program is established. CRC is unique in that there are several potential screening modalities available with different levels of scientific evidence to support their efficacy. A clear distinction between them based on cost-effectiveness has not been established. Maximizing screening rates and thereby reducing deaths related to CRC may best be achieved through the menu approach advocated by the American Consortium guidelines by which a patient in consultation with the physician determines the best individual screening option, a decision that may often consider factors other than just the performance of the test. Hard-line stances by physicians in favour of screening only with FOBT or only with colonoscopy may have the unwanted effect of reducing public cooperation. Recommending use of several different screening tests as options appears to be the tack taken by most Alberta specialists but not by national organizations such as the Canadian Task Force on Preventive Health Care. Therefore, it may be the approach as much as the message that has been rejected by many Alberta specialists.
Conclusions
Alberta specialists believe that CRC screening is effective and recommend that average-risk adults undergo screening. Most specialists recommend more than one type of screening test, including colonoscopy, in contrast to Canadian guidelines supporting the use of only FOBT or flexible sigmoidoscopy. There is a clear need to resolve this conflict in approach before implementing population-based CRC screening, so that all stakeholders (program planners, primary care physicians, specialists) are fully supportive of a screening program.
Acknowledgments
This study was supported by an operating grant from the Alberta Cancer Board and the Medical Services Incorporated Foundation. Drs. Hilsden and McGregor were supported by Alberta Heritage Foundation for Medical Research Population Health Investigator Awards.
Presented in part at the annual meeting of the American Gastroenterology Association, Orlando, Fla., 2003.
Competing interests: None declared.
Correspondence to: Dr. Robert J. Hilsden, 3330 Hospital Dr. NW, Calgary AB T2N 4N1; fax 403 283-6151; rhilsden@ucalgary.ca
Accepted for publication July 7, 2004.
References
- 1.Canadian Task Force on Preventive Health Care. Colorectal cancer screening. Recommendation statement from the Canadian Task Force on Preventive Health Care. CMAJ 2001;165:206-8. [PMC free article] [PubMed]
- 2.Winawer SJ, Fletcher RH, Miller L, Godlee F, Stolar MH, Mulrow CD, et al. Colorectal cancer screening: clinical guidelines and rationale. Gastroenterology 1997;112:594-642. [DOI] [PubMed]
- 3.Winawer S, Fletcher R, Rex D, Bond J, Burt R, Ferrucci J, et al. Colorectal cancer screening and surveillance: clinical guidelines and rationale — update based on new evidence. Gastroenterology 2003;124:544-60. [DOI] [PubMed]
- 4.US Preventive Services Task Force. Screening for colorectal cancer: recommendation and rationale. Ann Intern Med 2002;137:129-31. [DOI] [PubMed]
- 5.American College of Radiology. ACR appropriateness criteria for screening for colorectal cancer. Radiology 2000;215 (Suppl): 231-7. [PubMed]
- 6.Ontario Expert Panel on Colorectal Cancer. Colorectal cancer screening: final report of the Ontario Expert Panel. Toronto: The Panel, Cancer Care Ontario; 1999.
- 7.National Committee on Colorectal Cancer Screening. Recommendations for population-based colorectal cancer screening. Ottawa: The Committee; 2003. Available: www.phac-aspc.gc.ca/publicat/ncccs-cndcc/ccsrec_e.html (accessed 2005 Sept 23).
- 8.Nadel MR, Blackman DK, Shapiro JA, Seeff LC. Are people being screened for colorectal cancer as recommended? Results from the National Health Interview Survey. Prev Med 2002;35:199-206. [DOI] [PubMed]
- 9.Seeff LC, Shapiro JA, Nadel MR. Are we doing enough to screen for colorectal cancer? Findings from the 1999 Behavioral Risk Factor Surveillance System. J Fam Pract 2002;51:761-6. [PubMed]
- 10.Nelson DE, Bland S, Powell-Griner E, Klein R, Wells HE, Hogelin G, et al. State trends in health risk factors and receipt of clinical preventive services among US adults during the 1990s [see comment]. JAMA 2002;287:2659-67. Comment in: JAMA 2002;288:1233. [DOI] [PubMed]
- 11.Sirovich BE, Schwartz LM, Woloshin S. Screening men for prostate and colorectal cancer in the United States: Does practice reflect the evidence? JAMA 2003;289:1414-20. [DOI] [PubMed]
- 12.McCaul KD, Tulloch HE. Cancer screening decisions. J Natl Cancer Inst Monogr 1999;(25):52-8. [DOI] [PubMed]
- 13.Slevin TJ, Donnelly N, Clarkson JP, English DR, Ward JE. Prostate cancer testing: behaviour, motivation and attitudes among Western Australian men. Med J Aust 1999;171:185-8. [DOI] [PubMed]
- 14.Cowen ME, Kattan MW, Miles BJ. A national survey of attitudes regarding participation in prostate carcinoma testing. Cancer 1996;78:1952-7. [DOI] [PubMed]
- 15.Leard LE, Savides TJ, Ganiats TG. Patient preferences for colorectal cancer screening. J Fam Pract 1997;45:211-8. [PubMed]
- 16.McGregor SE, Hilsden RJ, Murray A, Bryant HE. Colorectal cancer screening: practices and opinions of primary care physicians. Prev Med 2004;39:279-85. [DOI] [PubMed]


