Abstract
Introduction
Since the introduction of a regionalized trauma system in Quebec in 1993, patient loads at level I trauma centres have been increasing gradually. We aimed to investigate the type of patient presenting to 4 tertiary trauma centres in Quebec, the nature of their injuries and whether there was a need to modify triage protocols.
Methods
The study consisted of a review of major trauma patients entered into a regional trauma registry between Apr. 7, 1993, and Mar. 31, 2000. A total of 29 669 patients fulfilled the eligibility criteria. We compared patient demographics, injury type and severity and mechanism of injury.
Results
During the 7 years of the study, there was an increase in the volume and presentation of patients injured in falls (p < 0.01), patients with extremity injuries (p < 0.01), single injuries (p < 0.01) and injuries to single body regions (p < 0.01). Young patients were mostly injured in motor vehicle collisions and had multiple injuries of high severity whereas elderly patients were mostly injured in falls and experienced isolated extremity injuries of low severity.
Conclusions
The proportion of elderly patients injured in falls, experiencing isolated extremity injuries of low severity and being treated at tertiary trauma centres in Quebec is overwhelmingly high. Revision of pre-hospital triage protocols should be considered and studied in order to transport trauma patients to appropriate facilities.
Abstract
Introduction
Depuis l'implantation d'un système régionalisé de traumatologie au Québec en 1993, la charge de patients aux centres de traumatologie de niveau I a augmenté progressivement. Nous voulions étudier le type de patients qui se présentent à quatre centres tertiaires de traumatologie du Québec, la nature de leurs traumatismes, et déterminer s'il faudrait modifier les protocoles de triage.
Méthodes
L'étude a consisté en une analyse des cas de grands traumatisés inscrits dans un registre régional de traumatologie entre le 7 avril 1993 et le 31 mars 2000. Au total, 29 669 patients satisfaisaient aux critères d'admissibilité. Nous avons comparé les caractéristiques démographiques des patients, le type de traumatisme, sa gravité et le mécanisme traumatisant.
Résultats
Au cours des sept années visées par l'étude, le volume et le nombre de références de patients ayant subi un traumatisme à la suite d'une chute (p < 0,01), une blessure aux membres (p < 0,01), un seul traumatisme (p < 0,01) et des traumatismes à une seule région du corps, (p < 0,01) ont augmenté. Les jeunes patients ont été blessés principalement dans des accidents de véhicule automobile et ont subi des traumatismes multiples très graves, tandis que les patients âgés s'étaient blessés principalement à la suite d'une chute et ont subi des traumatismes isolés et moins graves aux membres.
Conclusions
La proportion des patients âgés qui subissent une blessure à la suite d'une chute, subissent une blessure isolée et moins grave des membres et sont traités aux centres tertiaires de traumatologie du Québec est excessivement élevée. Il faudrait envisager de réviser les protocoles de triage préhospitalier et les étudier afin de transporter les patients traumatisés vers les établissements appropriés.
Tertiary trauma centres aim to provide comprehensive multidisciplinary care to the severely injured trauma patient. As a consequence of the large amount of specialized in-house staff and specialty equipment required at tertiary trauma centres as well as overcrowding, costs are high and beds are in great demand. Regionalization of trauma care has been shown to decrease the death rate after trauma,1,2,3,4 and the “trauma centre” approach to the care of the injured patient has been widely accepted as being superior to the treatment of severely injured patients at the closest hospital.
Regionalization of trauma care was initiated in Quebec in 1993 to improve quality of care and decrease morbidity and mortality. Since then, the volume of patients transported to tertiary trauma centres has been rising steadily. We undertook this study to find the causes of increased patient loads at tertiary trauma centres in Quebec and to study the demographics of these patients with the intention of identifying ways to improve the efficiency of our trauma program.
Methods
This retrospective study comprised patients entered in the Quebec Trauma Registry from the 4 provincial tertiary trauma centres (Montreal General Hospital, Hôpital Sacré-Coeur, Hôpital Charles-Lemoyne and Hôpital Enfant-Jésus) between Apr. 7, 1993, and Mar. 31, 2000. All data were prospectively collected at the tertiary trauma centres, then entered into the registry by designated trauma registry personnel. These hospitals are compatible with the American College of Surgeons (ACS) criteria for level I trauma centres and have been accredited by the Trauma Association of Canada as tertiary trauma centres.
Inclusion criteria for severely injured patients were as follows: death after arrival at hospital; admission with hospital stay longer than 3 days; or admission with surgery or intensive care unit stay. The calendar year Jan. 1 to Dec. 31 was used to define the year.
Patients were identified from emergency room records on the basis of ICD-9 E-codes, which indicate external cause of injury or any evidence of injury. Patients admitted to hospital for treatment of burns, asphyxiation, drowning and poisoning were excluded. All records were subjected to routine edit checks. No attempt was made to substitute missing values for any data elements. The Injury Severity Score (ISS) was calculated from patient admission variables prospectively entered into the database. Patients with a mechanism of injury consistent with a fall were included in the study regardless of the height from which the patient fell, as long as the patient fulfilled the inclusion criteria.
Quebec Trauma Registry software developed in Paradox for Windows was used to collect the data and the SPSS, version 11 for Windows, was used to analyze the findings. Differences between groups were evaluated for statistical significance with the appropriate bivariate tests including the χ2 test and ANOVA for categorical and continuous variables respectively. Because of the large sample size, the significance level was set at 0.01 to prevent overpowered analysis from highlighting nonclinically significant differences between groups.
Results
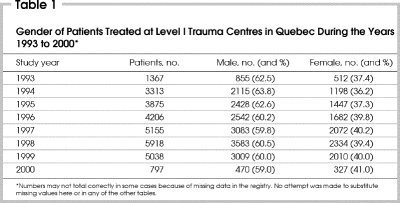
Between Apr. 1, 1993, and Mar. 31, 2000, there were 29 669 patients who fulfilled the eligibility criteria for inclusion in the study (Table 1). During the earlier years of the study, compliance with trauma registry patient entry was low, so the numbers of patients included for these years are smaller than those included in later years. The number of patients in the year 2000 is low because only 3 months were included (January– March inclusive).
Table 1
The mean age of the patients in this study was 47.4 years (range from 46–49 yr) (Table 2). The largest portion of patients were younger than 25 years of age and the majority were younger than 45 years. The gender distribution by year is outlined in Table 1; 60.9% of patients were male. The median ISS remained constant at 9.0 for the study period. The mean ISS increased slightly but not significantly (Table 3).
Table 2
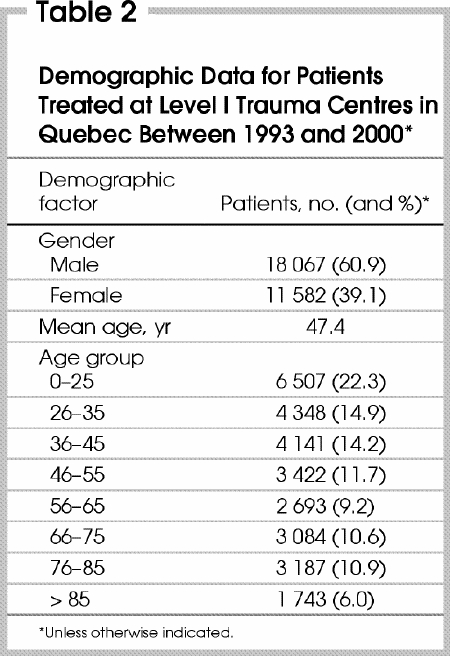
Table 3
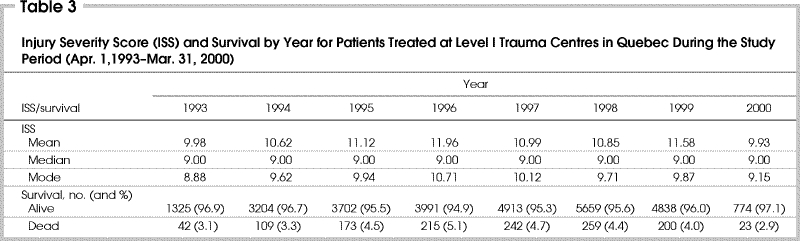
Of the 29 669 patients treated at tertiary trauma centres in Quebec over study period, 28 406 (95.7%) were discharged from hospital. The discharge status among survivors is outlined in Fig. 1. Survival rates by year are shown in Table 3.
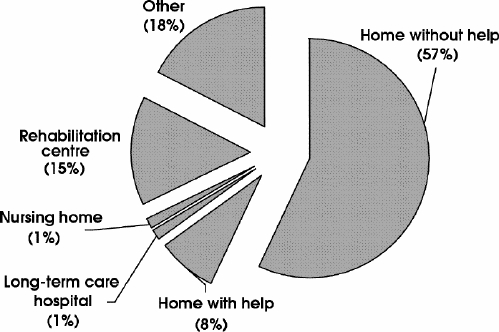
FIG. 1. Discharge status among the 28 406 study trauma patients surviving to discharge.
In regard to the mechanism of injury, falls were the commonest mechanism (49.2%), followed by motor vehicle collisions (MVCs) (27.3%) (Table 4). Fig. 2 demonstrates the increasing number of patients admitted for the treatment of falls, which was significant (p < 0.01).
Table 4
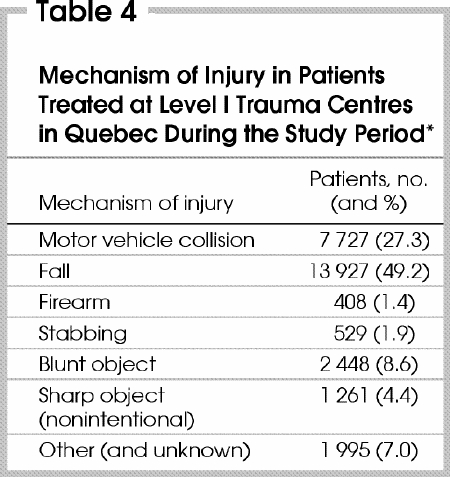
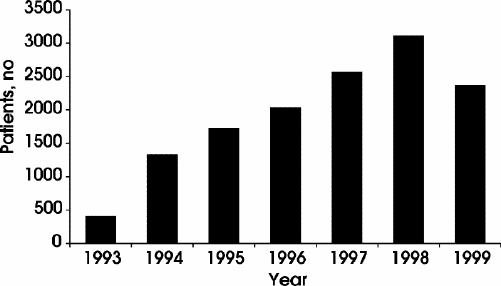
FIG. 2. Number of fall injuries treated at tertiary trauma centres in Quebec by year. Increase in number of falls from one year to the next was significant (p < 0.01).
The 29 669 patients included in this study sustained over 75 000 injuries, and 45.3% of patients had injury to an extremity (Table 5). Fig. 3 shows the number of body regions injured by year. Note the increasing number of extremity injuries treated at tertiary trauma centres since 1993 (410 in 1993, 3116 in 1998 and 2378 in 1999 [p < 0.01]).
Table 5
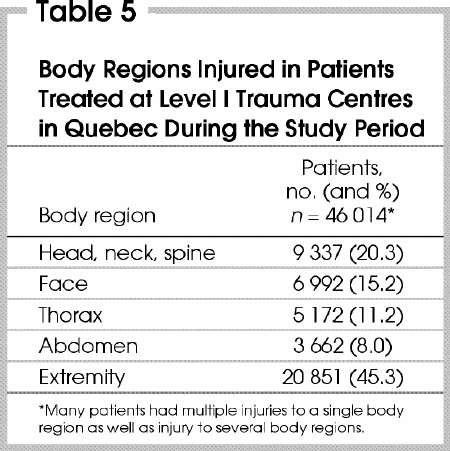
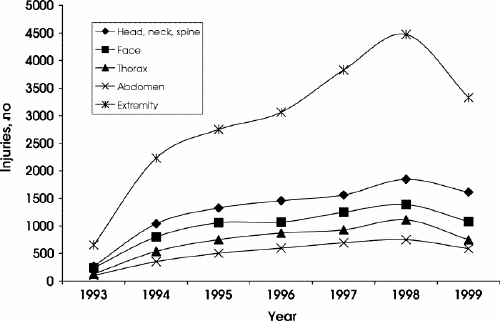
FIG. 3. Body regions injured by year. Increasing numbers of extremity injuries were significant (p < 0.01).
Table 6 shows the number of injuries experienced per patient and Table 7 the number of body regions injured per patient. Single injuries accounted for the highest proportion (36.0%), followed by 2 to 3 injuries (30.5%). Fig. 4 and Fig. 5 describe the number of injuries sustained and the number of body regions injured by year respectively. Significantly more patients sustained single injuries (p < 0.01) and injuries to isolated body regions (p < 0.01) during the later years of the study.
Table 6
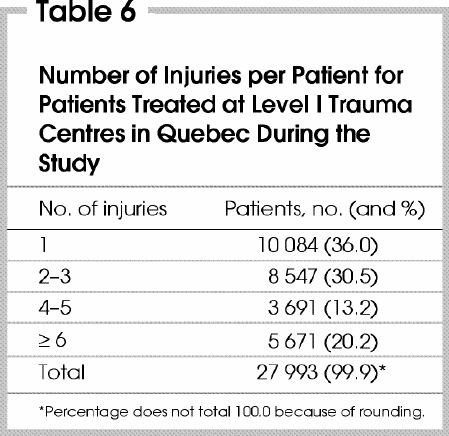
Table 7
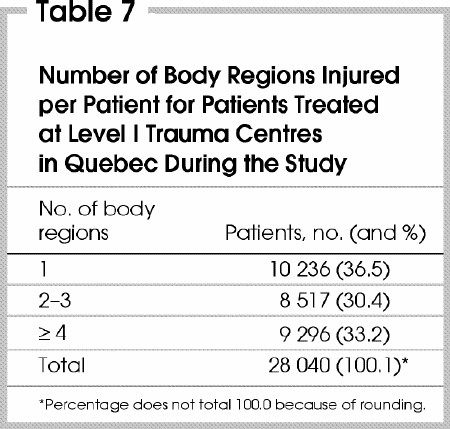
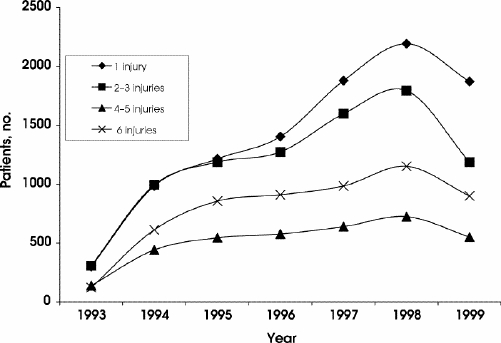
FIG. 4. Number of injuries per patient by year. Increase in single-region injuries was significant (p < 0.01).
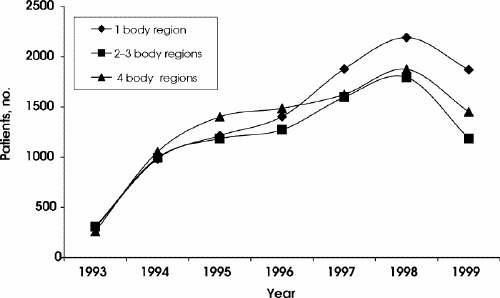
FIG. 5. Number of body regions injured per patient by year. Increase in number of patients with injuries to single-body regions was significant (p < 0.01).
The number of injuries sustained by each patient according to the mechanism of injury is described in Table 8. Those sustaining falls made up the majority of patients with single injuries (69.8%) and those involved in MVCs sustained the largest proportion of multiple injuries (≥ 6, 63.5%). Fig. 6 outlines the proportion of patients with each mechanism of injury according to the total number of injuries experienced by each patient. With the progression from single injury to 6 or more injuries per patient, the number of patients experiencing falls decreased from 7042 patients to 1197 patients (p < 0.01) and the number of patients injured in MVCs rose from 785 patients to 3600 (p < 0.01).
Table 8
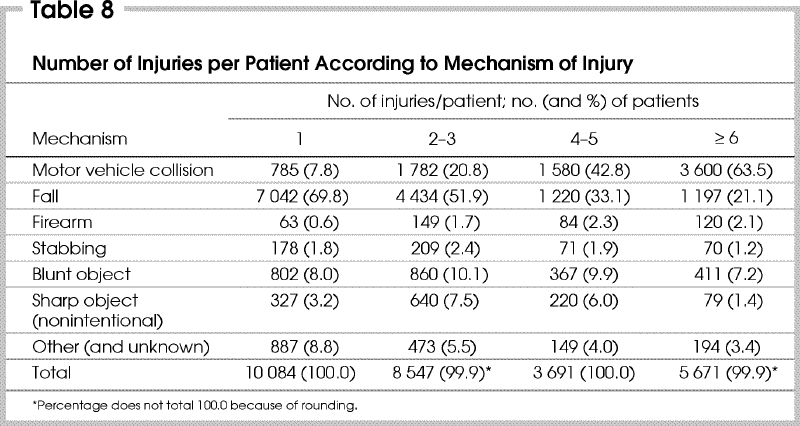
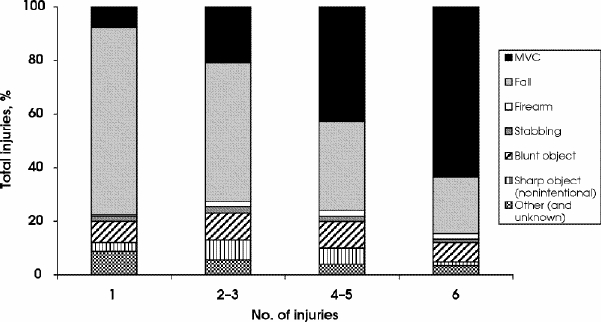
FIG. 6. Mechanism of injury as a percentage of the total according to the patient's number of injuries. MVC = motor vehicle collision.
Fig. 7 shows the proportion of patients with each mechanism of injury according to age category. Falls were prevalent in the geriatric age group (93.8% of patients over age 85 yr), and the percentage of falls as a cause of trauma increased significantly with advancing age (p < 0.01). Injuries from MVCs were more prevalent than other mechanisms of injury in younger age groups, with 40.9% of injuries in patients younger than 25 years being due to MVCs. Analysis of the ISS according to the mechanism of injury for trauma patients (Fig. 8) revealed that the proportion of MVCs was directly proportional to injury severity and the proportion of falls as a cause of trauma was inversely related to injury severity.
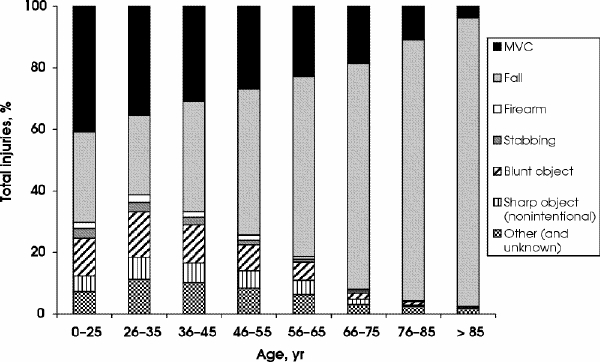
FIG. 7. Mechanism of injury as a percentage of the total according to age category. MVC = motor vehicle collision.
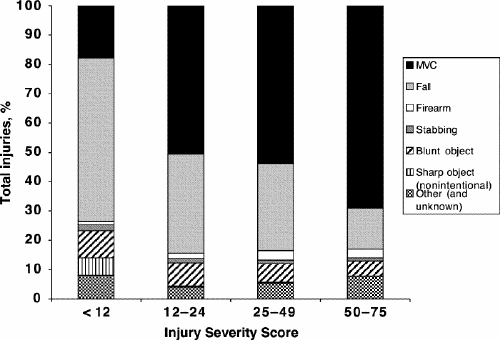
FIG. 8. Mechanism of injury as a percentage of the total according to the Injury Severity Score category. MVC = motor vehicle collision.
Discussion
Between 1992 and 1995, 147 million injury-related visits were made to emergency departments in the United States. Twenty-four percent of the visits were due to falls, making them the principal cause of external injury.5 Patients injured in falls are more often elderly and require longer hospital stays than younger patients.6,7 These patients also have been reported to have lower death rates because of lower injury severity.2 However, many studies have shown a correlation between high death rates in geriatric patients and comorbid conditions as well as in-hospital complications.7,8,9,10
Surgical and emergency room costs in trauma centres are primarily related to the length of patient stay.11 Geriatric patients experiencing traumatic injury have an increased length of hospital stay and hence increased direct health care utilization,7,10,12,13 likely due to increased rehabilitation needs and waiting time for convalescence placement.7 The increasing numbers of patients treated for isolated orthopedic injuries after falls at tertiary trauma centres in Quebec is important in terms of both allocation of resources and quality of care. In most cases, falls associated with older age involve single injuries to extremities14 as well as low ISSs, as demonstrated in this study. The majority of these injuries are isolated long bone or pelvic fractures, requiring the care of an orthopedic surgeon and not a level I trauma centre with specialized general surgeons, neurosurgeons, nursing and intensive care resources. Finelli and associates10 showed that mortality in geriatric patients increases with age for all injuries, with the exception of falls.10
Forty-five percent of patients treated at tertiary trauma centres in Quebec had injuries to the extremities. This is consistent with the prevalence of injuries due to falls and the age profile of this cohort. The proportion of patients having isolated injuries increased significantly during the last 2 years (p = 0.001) of the study. There were comparable decreases in the proportion of patients having multiple injuries. This important observation is consistent with the increase in the proportion of patients injured in falls. Similar observations were made for the number of body regions injured, raising concern that patients with injuries of moderate severity and single-body-region injuries are being treated at tertiary trauma centres, when they could have been managed in secondary centres or other acute care hospitals.
The ISS profile of the patients treated in tertiary trauma centres in Quebec was somewhat lower than expected, likely owing to the increased number and proportion of fall-injury patients treated at these centres. The majority of these (69.8%) had only one injury, and, as expected, were significantly older than for other mechanisms of injury. The majority of patients (56%) with ISSs of less than 12 (low injury severity) had falls as their mechanism of injury.
The numbers of trauma patients treated at tertiary trauma centres in Quebec decreased in 1999, after a sustained yearly increase over the preceding years. We have no single explanation for this phenomenon; however, this may be the result of improved triage and transfer protocols as well as adherence to changes made in the prehospital protocols in Quebec during the later years of the study.
One of the major limitations of this study is the inability to distinguish patients transported directly to level I trauma centres from those transferred to level I centres from lower-level centres. This knowledge is important, particularly with respect to patients with isolated extremity injuries. This could be because of an inability or unwillingness of surgeons to treat these patients at level II and III centres. However, as a regionalized trauma system matures, increasing proportions of patients are transported directly to tertiary centres. In Quebec, the proportion of patients transported directly from the scene to a tertiary centre has increased consistently and significantly from 56% in 1993 to 73% in 2000.
The geriatric patient who suffers any injury is at increased risk of mortality and requires prompt specialized care because of lower physiologic reserves and a decreased ability to handle physiologic stress. Patients injured in falls tend to be older and have fewer and less severe injuries. However, because of comorbid conditions, the risk of complications and mortality is high in this population. These patients consume a significant proportion of the resources available at tertiary trauma centres because they need specialized care, rehabilitation and have a longer hospital stay.7,10,12,13,15,16 The issue is whether these patients require treatment at a tertiary trauma centre or a secondary or less specialized one.
In a study by Oreskovich and colleagues,16 only 7 of 100 consecutive trauma patients over 70 years of age were independent for their activities of daily living at 1 year after injury, compared with 96 before their trauma. Seventeen (20%) of these patients required home assistance after discharge from hospital, and 61 patients (72%) required full nursing home care. The low functional outcome for elderly patients admitted to trauma centres contributes to the increased length of stay while they await beds in rehabilitation centres and nursing homes and consequently inappropriate use of acute care beds in tertiary trauma centres.
In Quebec, prehospital trauma triage protocols are based on the American College of Surgeons Triage Decision Scheme. However, no medical control is available for decision-making at the scene. In Montréal, there are a small number of physicians who can be dispatched to trauma patients based on severity and availability. These physicians may aid in triage decisions. In spite of this, triage is extremely operator-dependent, and the ambulance technicians are instructed to overtriage patients in order to reduce false-negative rates.
In view of the higher requirements in our study population for specialized geriatric care, longer hospital stay and prevalence of pre-existing chronic comorbid conditions, the resource allocation of a tertiary trauma centre for the post-acute-care management of these patients may be counter cost-effective. Trauma care at tertiary trauma centres would be more efficient, and the multiple resources that constitute a regional trauma program would be best used if hemodynamically stable patients with isolated orthopedic injuries of low injury severity could be treated at secondary centres or at secondary centres specializing in the care of the elderly. At this point, a more extensive analysis of the geriatric population is warranted to verify if these patients could be treated without the multidisciplinary resources of a tertiary trauma centre while ensuring an adequate level of care.
Conclusions
This study demonstrates an overwhelming high volume and proportion of elderly patients injured in falls, having isolated extremity and low-severity injuries being treated at tertiary trauma centres in Quebec. These patients require specialized geriatric care in addition to the acute care for the management of their injuries. Further studies are required to verify whether such patients who are hemodynamically and neurologically stable and have no associated injuries could be appropriately managed at secondary centres. Prehospital triage protocols need to be adjusted to have injured patients sent to appropriate centres.
Presented at the joint meeting of the Trauma Association of Canada and the Australasian Trauma Society, Sydney, Australia, Mar. 2–4, 2001.
Competing interests: None declared.
Correspondence to: Dr. Moishe Liberman, Montreal General Hospital, Department of Surgical Research, Ste. 501, 3465 Cote des Neiges, Montréal QC H3H 1T7; fax 514 934-9913; moisheliberman@sciopsis.com
Accepted for publication Mar. 19, 2003.
References
- 1.Sampalis JS, Denis R, Lavoie A, Frechette P, Boukas S, Nikolis A, et al. Trauma care regionalization: a process-outcome evaluation. J Trauma 1999;46:565-81. [DOI] [PubMed]
- 2.Cales RH, Trunkey DD. Preventable trauma deaths. A review of trauma care systems development. JAMA 1985;254:1059-63. [DOI] [PubMed]
- 3.Mullins RJ, Veum-Stone J, Helfand M, Zimmer-Gembeck M, Hedges JR, Southard PA, et al. Outcome of hospitalized injured patients after institution of a trauma system in an urban area. JAMA 1994;271:1919-24. [DOI] [PubMed]
- 4.Shackford SR, Hollingworth-Fridlund P, Cooper GF, Eastman AB. The effect of regionalization upon the quality of trauma care as assessed by concurrent audit before and after institution of a trauma system: a preliminary report. J Trauma 1986;26: 812-20. [DOI] [PubMed]
- 5.Burt CW, Fingerhut LA. Injury visits to hospital emergency departments: United States, 1992-95. Vital Health Stat 1998;13:1-76. [PubMed]
- 6.DeKeyser F, Carolan D, Trask A. Suburban geriatric trauma: the experience of a level I trauma center. Am J Crit Care 1995;4:379-82. [PubMed]
- 7.Ross N, Timberlake GA, Rubino LJ, Kerstein MD. High cost of trauma care in the elderly. South Med J 1989;82:857-9. [DOI] [PubMed]
- 8.Osler T, Hales K, Baack B, Bear K, Hsi K, Pathak D, et al. Trauma in the elderly. Am J Surg 1988;156:537-43. [DOI] [PubMed]
- 9.Copeland AR. Fatal accidental falls among the elderly — the Metro Dade County experience, 1981–83. Med Sci Law 1985;25:172-5. [DOI] [PubMed]
- 10.Finelli FC, Jonsson J, Champion HR, Morrelli S, Fouty WJ. A case control study for major trauma in geriatric patients. J Trauma 1989;29:541-8. [DOI] [PubMed]
- 11.Taheri PA, Wahl WL, Butz DA, Iteld LH, Michaels AJ, Griffes LC, et al. Trauma service cost: the real story. Ann Surg 1998;227:720-4. [DOI] [PMC free article] [PubMed]
- 12.Weingarten MS, Wainwright ST, Sacchetti AD. Trauma and aging effects on hospital costs and length of stay. Ann Emerg Med 1988;17:10-4. [DOI] [PubMed]
- 13.DeMaria EJ. Evaluation and treatment of the elderly trauma victim. Clin Geriatr Med 1993;9:461-71. [PubMed]
- 14.Tepas JJ, Veldenz HC, Lottenberg A, Romig LA, Pearman A, Hamilton B, et al. Elderly injury: a profile of trauma experience in the sunshine (retirement) state. J Trauma 2000;48:581-6. [DOI] [PubMed]
- 15.DeMaria EJ, Kenney PR, Merriam MA, Casanova LA, Gann DS. Aggressive trauma care benefits the elderly. J Trauma 1987;27:1200-6. [DOI] [PubMed]
- 16.Oreskovich MR, Howard JD, Copass MK, Carrico CJ. Geriatric trauma: injury patterns and outcome. J Trauma 1984;24:565-72. [PubMed]