Abstract
Introduction
The chronic shortage of organs for donation could be improved by increasing the numbers of potential and actual donors. Physicians can play a key role in solving this problem but may miss opportunities because they lack knowledge about organ donation to answer questions or concerns. Education of physicians early in their careers may lead to better procurement rates for donor organs. We carried out a study at Queen's University in Kingston, Ont., to determine whether medical students have sufficient knowledge of topics shown to affect organ donation rates.
Methods
Medical students from years 1–4 completed a self-administered questionnaire. Section 1 tested general knowledge about organ donation; section 2 tested the students' ability to identify potential donors; and section 3 dealt with the approach to the potential donor's family. Univariate predictors of mean test scores were assessed using the t-test.
Results
Of 322 medical students who received the questionnaire, 260 (81%) responded. The mean age of the students was 25 years and 54% were men. The mean knowledge score was 6.7 out of a possible score of 14. Third-year students had the best knowledge scores (7.6), followed by fourth- (7.4), second- (6.6) and first-year students (5.7). Teaching about organ donation and a student's comfort with approaching a family for organ donation were also predictive of higher knowledge scores. There was no correlation between knowledge score and age, gender or whether the student was carrying a signed donor card. Knowledge scores were low in all 3 sections. Thirty-six percent of students did not know that brain death means that the patient is dead rather than in a coma. Half the medical students believed that people of certain religious groups should not be approached about organ donation.
Conclusions
Medical students possess limited knowledge about organ donation topics important for maximizing procurement rates. A teaching intervention designed to target these shortcomings may be beneficial.
Abstract
Introduction
Il serait possible d'atténuer la pénurie chronique d'organes à donner en augmentant le nombre de donneurs possibles et de donneurs réels. Les médecins peuvent jouer un rôle clé dans la solution de ce problème, mais ils peuvent rater des possibilités parce qu'ils ne possèdent pas suffisamment de connaissances au sujet du don d'organe pour répondre à des questions ou à des préoccupations. L'éducation des médecins en début de carrière pourrait améliorer les taux d'acquisition d'organes de donneurs. Nous avons procédé à une étude à l'Université Queen's de Kingston (Ontario) pour déterminer si les étudiants en médecine connaissent suffisamment les sujets connus pour avoir un effet sur les taux de dons d'organe.
Méthodes
Les étudiants en médecine de la première à la quatrième année ont rempli un questionnaire autoadministré. La partie 1 vérifiait les connaissances générales sur le don d'organe, la partie 2 vérifiait la capacité des étudiants de repérer des donneurs éventuels et la partie 3 portait sur la façon d'aborder la famille du donneur éventuel. On a évalué les prédicteurs unidimensionnels des résultats moyens en utilisant le test-t.
Résultats
Sur 322 étudiants en médecine ayant reçu le questionnaire, 260 (81 %) y ont répondu. Les étudiants avaient en moyenne 25 ans et 54 % d'entre eux étaient des hommes. Le résultat moyen au niveau des connaissances a atteint 6,7 sur un total possible de 14. Les étudiants de troisième année affichaient les meilleurs résultats au niveau des connaissances (7,6), suivis de ceux de la quatrième (7,4), de la deuxième (6,6) et de la première (5,7) année. La formation au sujet du don d'organe et le confort avec lequel l'étudiant aborde une famille pour obtenir un don d'organes étaient aussi des prédicteurs de résultats plus élevés quant aux connaissances. Il n'y avait aucun lien entre le résultat relatif aux connaissances et l'âge, le sexe ou le fait que l'étudiant portait ou non une carte de don signée. Les résultats relatifs aux connaissances étaient faibles dans les trois parties. Trente-six pour cent des étudiants ne savaient pas que la mort cérébrale signifie que le patient est mort plutôt que dans le coma. La moitié des étudiants en médecine pensaient qu'il ne faudrait pas parler de don d'organe aux membres de certains groupes religieux.
Conclusions
Les étudiants en médecine ont une connaissance limitée des sujets reliés aux dons d'organe qui sont importants pour maximiser les taux d'obtention. Une intervention pédagogique conçue pour combler ces lacunes pourrait être bénéfique.
Studies have shown that organ donation continues to remain a topic of debate and a high public priority.1 In 1998, 1576 transplants were performed in Canada, but 3548 patients remained on donor waiting lists. Canada's organ donation rate in 1999 was just 14.1 per million population, compared with 21.3 per million in the United States and 33.6 per million in Spain.2 The obvious solution to this problem is to decrease the disparity between the numbers of potential and actual donors. Possible donors are excluded because they do not meet eligibility requirements, usually owing to a pre-existing illness. Many potential donors are missed because physicians fail to approach family members about the possibility of donation. In Ontario, the decision to donate organs lies ultimately with family members. Physicians may miss potential donors because they falsely believe that the patient is unsuitable for donation or because they are deterred by emotional stress associated with a request for organ donation. Physicians who do approach family members often lose an opportunity to obtain an organ because they lack sufficient knowledge about organ donation to answer questions or concerns.3 Physician education has been shown to increase donation requests and procurement by addressing these problems.4,5,6 Also, the benefits of education for physicians in this area may diminish with time.4 This problem may be solved by making organ donation a key component of medical education and fostering an interest in organ donation among students. Results of a recent pilot study suggest that medical students at Queen's University in Kingston, Ont., demonstrate little knowledge of scientific and social issues related to organ donation.7 Furthermore, medical students were not shown to have any more knowledge of organ donation than their nonmedical undergraduate counterparts. This lack of knowledge may reflect the minimal time allotted to issues of organ donation in the medical curriculum. Organ donation and transplantation are important topics in surgical education. There is a growing trend for a reduced exposure to topics related to surgery in undergraduate medical curricula. This may be responsible in part for the declining number of students applying to surgery training.8 At Queen's University, 1 lecture hour is allocated to ethical issues relating to organ donation, and 1 problem-based learning case has organ donation as a learning issue. An additional immunology lecture covers topics related to the science of transplantation and graft rejection. No time is allotted to teaching the process of organ donation or how to approach a family about organ donation.
Knowledge of organ donation among medical students has not been examined in detail. A study conducted in Germany looked at the knowledge level of first-year medical students and found it to be at a level consistent with that of the lay public.9 We, therefore, sought to determine whether medical students have the knowledge needed to maximize organ donation rates and, if not, to identify areas that could be targeted by future curriculum modifications.
Method
Ethics approval was obtained, and a cross-sectional questionnaire was delivered to all medical students at Queen's University Faculty of Health Sciences. To design the questionnaire, a review of the literature determined key information needed by physicians to maximize donation rates. Three areas were identified: general knowledge of organ donation; identifying potential donors; and how to approach family members. No suitable questions were identified in the literature, so the research team developed and tested the questions used in the survey. A pilot questionnaire was administered to 8 graduate students in the Department of Community Health and Epidemiology and to 7 residents with the Department of Surgery to identify and eliminate bias in the questionnaire design. This led to changes in the wording of some questions to improve clarity and to the addition of a question about a religious topic. Age, gender, prior teaching, whether the student carries a signed organ donor card and whether the student would feel comfortable in making a request for organ donation were all considered as predictors of better test scores. The questionnaire was administered before class lectures (the lectures were on topics unrelated to organ donation) and during a student–faculty dinner. Statistical analysis was performed using SPSS version 10.0. The t-test was used to compare mean knowledge scores between 2 groups.
Results
A completed questionnaire was obtained from 260 (81%) of 322 medical students. The response rates for first-year, second-year, third-year and fourth-year classes were 92%, 72%, 86 % and 70%, respectively. The mean age of all students was 25.3 years. Of the respondents, 54% were men. The mean knowledge score was 6.7 out of a possible score of 14. The third-year students had the highest mean score (7.56) followed by fourth-year (7.35), second-year (6.55) and first-year (5.73) students. The differences among the mean scores of each of the classes in the 3 categories of general knowledge, identifying potential donors and the process of requesting a donation are shown in Fig. 1. Third- and fourth-year students appeared to possess greater knowledge in the area identifying potential donors and, to a lesser extent, in the approach to requesting donation. Third-year students appeared to have greater general knowledge about organ donation. The temporal relationship between scheduled teaching on topics related to organ donation and the mean scores for each medical class is illustrated in Fig. 2. The figure demonstrates that knowledge scores do not increase substantially after the second year, despite the scheduling of all related teaching sessions in this year.
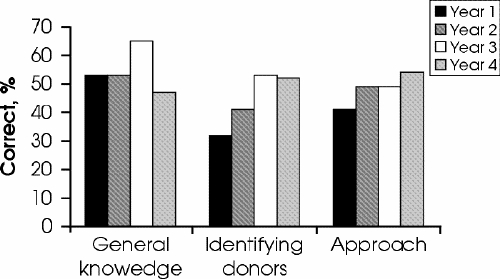
FIG. 1. Knowledge scores by test category for medical students who responded to the questionnaire in the 4 classes.
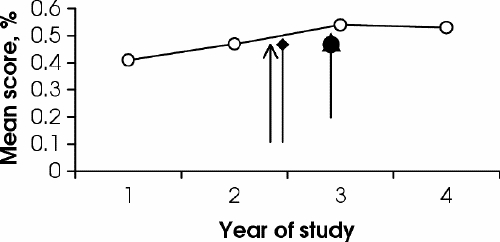
FIG. 2. Knowledge score and curriculum milestones for medical students who responded to the questionnaire Indicated are the timing of the problem-based learning case on organ donation (arrow), the lecture on criteria of brain death (diamond) and the ethics lecture on organ allocation (circle).
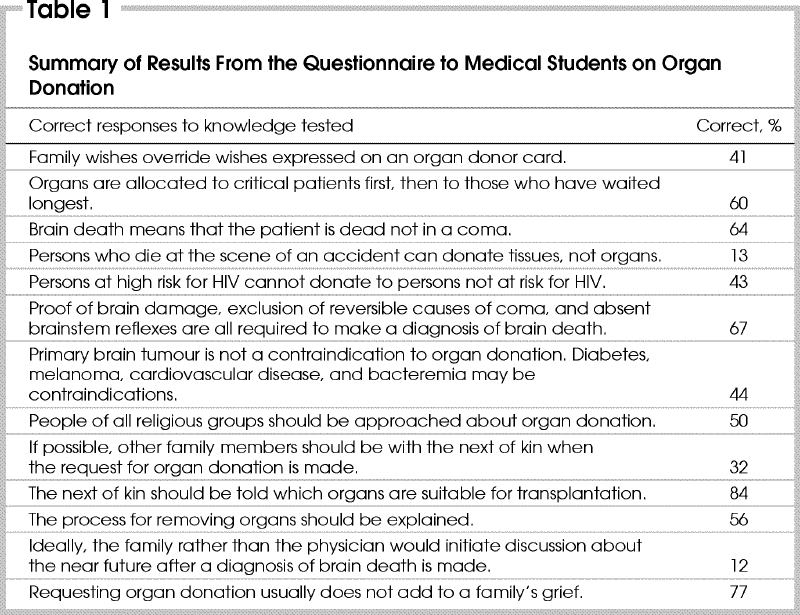
Students scored poorly in all 3 categories. For example, in the general knowledge section, 41% of students correctly believed that in practice the wishes of a family override those expressed on an organ donor card. In the identifying potential donors category, only 13% of students knew that individuals who die at the scene of an accident can only donate tissues such as corneas and not vital organs such as the heart or kidneys. In the process of requesting organ donation section, only 12% of students thought that discussions about the near future would be ideally initiated by the family of the deceased rather than being brought up by the physician. A comprehensive list of student responses by question can be seen in Table 1. Just 64% of students knew that a diagnosis of brain death means that a patient is dead and not in a coma. Fifty percent of students believed that people of all religious groups should be approached about organ donation. Few students recognized that a separate consultation would be more appropriate for making a request for donation, after giving the diagnosis of brain death.10
Table 1
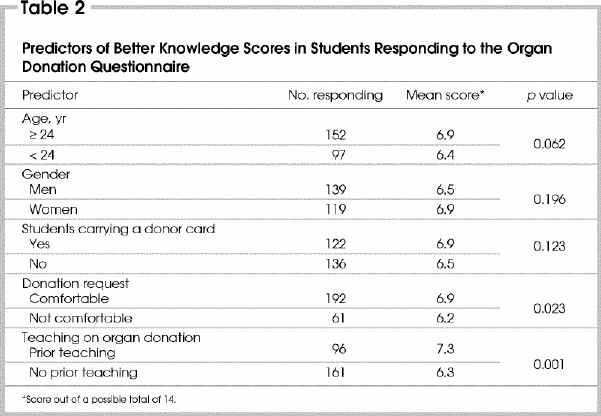
Prior teaching on organ donation and comfort in approaching potential donor's families were predictive of better knowledge scores. Age, sex and whether the student carried a signed donor card were not predictive of better scores (Table 2).
Table 2
Discussion
Limitations
The present study was limited in that not all medical students responded to the questionnaire, allowing the possibility of response bias. Although the overall response rate was 81%, only 72% of fourth-year students responded, as a number of them were away on elective rotations. A pilot study was employed in an attempt to minimize bias in the questionnaire design, but this scoring instrument was not tested for validity or reliability.
Interpretation
The limited knowledge of medical students about organ donation is likely a result of a paucity of teaching on the subject of organ donation in the undergraduate medical curriculum. At our institution, organ donation is identified as a learning issue in 1 problem-based learning case, brain death criteria are taught during the neurosciences section of the curriculum, and the ethics of organ allocation are discussed during the nephrology section of the curriculum. There is no formal teaching directed at such issues as how to identify potential donors or how to approach a potential donor family. The finding that only a slight increase in knowledge is observed from first to fourth year supports this conclusion (Fig. 2).
Fourth-year students, with almost a year of clinical experience, did not demonstrate better knowledge scores than third-year students. There are 3 possible explanations for the finding that third-year students had the highest scores: the result may be spurious; third-year students may recall more from lectures, as lectures that are given on topics pertaining to organ donation all occur during the second year of study (Fig. 2); and this finding may be the result of a previous intervention, as the cohort of students now in their third year of study were investigated in a previous study that compared general knowledge of organ donation between medical and nonmedical university students.7
The only predictors of better test scores were comfort with requesting donation and recollection of prior teaching on the subject of organ donation. Perhaps the students who have more knowledge about organ donation are more comfortable discussing the subject because of their better knowledge. This has been found previously in studies of both physicians and nurses.11 Only 37% of students could recall having had prior teaching on organ donation, while all but the first-year students should have had teaching at some point in the undergraduate curriculum.
Implications
There is a trend in medical schools to devote less time to surgical topics, a trend that may be responsible in part for the decline in applications to surgical residency programs.8 Organ transplantation is an exciting part of surgery that is at the forefront of medical advancement, and exposure to this discipline may encourage more future physicians to pursue a career in surgery. This important issue aside, the results of this study suggest that students at 1 Canadian medical school are not receiving adequate teaching on organ donation. For example, the task of explaining to families that a diagnosis of brain death means the patient is truly dead will be difficult, considering that 36% of medical students did not believe this to be the case. With only half of medical students believing that people of all religious groups should be approached for donation, the potential for missed donors is great. A future physician could wrongly assume that certain religious groups do not support organ donation. Furthermore, many people do not follow all of the tenets of their religion, or may not be practising their faith at all. All families should be presented with the option of organ donation. Many people find that organ donation helps with the grieving process.12
With limited teaching on organ donation in the undergraduate medical curriculum, design and testing of an educational intervention for medical students on how to identify potential donors and how to approach the potential donor's family may be useful. Without such teaching, it is unclear where future physicians will acquire this knowledge. It should be noted that physician knowledge on the subject of organ donation is just one of many requirements for maximizing organ donation rates. A sensitive approach and good communication are also important skills. Nevertheless, undergraduate medical education committees at other universities should consider curriculum review in view of our results. Time and resources for undergraduate teaching are limited, yet organ donation is not a topic better reserved for the training of neurosurgeons and intensive care specialists. Studies have shown that emergency department physicians and consultants to the emergency department from various specialties can influence organ procurement rates.4,13 An important barrier to organ donation is that few people discuss the topic of organ donation with their families. Future family physicians will be ideally situated to foster this discussion.14
Conclusions
We have demonstrated shortcomings in medical student knowledge about organ donation at 1 Canadian medical school. These findings highlight a need to review medical school curricula to ensure that they contain sufficient teaching on organ donation, with a focus on information needed by physicians to maximize donation rates. This strategy may be part of a solution to the chronic shortage of donor organs for transplantation.
Acknowledgments
This project was supported by the Education Program of Associated Medical Services, Inc., awarded to Mr. Bardell as an AMS/Wilson student fellowship.
The results of this study were presented at the annual meeting of the Canadian Society of Transplantation, Mont-Tremblant, Que., Feb. 27–Mar. 2, 2002.
Competing interests: None declared.
Correspondence to: Dr. Minto K. Jain, Victory 3, Kingston General Hospital, 76 Stuart St., Kingston ON K7L 2V7; fax 613 548-2456; jainm@kgh.kari.net
Accepted for publication Apr. 29, 2003.
References
- 1.Sherbin P, Cormier P. MORE life. Transplant Proc 1997;29:3250-1. [DOI] [PubMed]
- 2.Cooper G, Lang J, Leman P. Organ donation Ontario 2000 annual statistics report. Toronto: Organ Donation Ontario; August 2000.
- 3.Schutt GR. True organ donor potential: a retrospective single-centre study. Transplant Proc 2000;32:66-7. [DOI] [PubMed]
- 4.Riker RR, White BW. The effect of physician education on the rates of donation request and tissue donation. Transplantation 1995;59:880-4. [PubMed]
- 5.Wamser P, Goetzinger P, Steininger M, Gnant M, Sautner T, Muhlbacher F. Discontinuing of a permanent information and education program among donor ICUS leads to a 50% decrease of organ donor rates. Transplant Proc 1993;25: 2988-9. [PubMed]
- 6.Evanisko MJ, Beasley CL, Brigham LE, Capossela C, Cosgrove GR, Light J, et al. Readiness of critical care physicians and nurses to handle requests for organ donation. Am J Crit Care 1998;7:4-12. [PubMed]
- 7.Bardell T, Childs AL, Hunter DJ. Organ donation: a pilot study of knowledge among medical and other university students. Ann R Coll Physicians Surg Can 2002;35:77-80. [PubMed]
- 8.Richardson JD. Workforce and lifestyle issues in general surgery training and practice. Arch Surg 2002;137:515-20. [DOI] [PubMed]
- 9.Laederach-Hofmannn K, Gerster BI. Knowledge, attitude and reservations of medical students about organ transplantation: results of a survey during the first year of study. Schweiz Med Wochenschr 1998;128:1840-9. [PubMed]
- 10.Randall T, Marwick C. Physicians' attitudes and approaches are pivotal in procuring organs for transplantation. JAMA 1991;265:1227-8. [DOI] [PubMed]
- 11.Blok GA, van Dalen J, Jager KJ, Ryan M, Wijnen RM, Wight C, et al. The European donor hospital education program (EDHEP): addressing the training needs of doctors and nurses who break bad news, care for the bereaved, and request donation. Transpl Int 1999;12:161-7. [DOI] [PubMed]
- 12.Norris MK. Nurses' perceptions of donor families' opinions: implications for professional education strategies. J Transpl Coord 1991;1:42-6.
- 13.Henderson SO, Chao JL, Green D, Leinen R, Mallon WK. Organ procurement in an urban level 1 emergency department. Ann Emerg Med 1998;31:466-70. [DOI] [PubMed]
- 14.Novello AC, Braslow JB. Increasing organ donations: an important issue for medical educators. Acad Med 1992;67:314-5. [DOI] [PubMed]


