Abstract
Introduction
The benefits of the laparoscopic approach to colon and rectal surgery do not seem as great as for other laparoscopic procedures. To study this further we decided to review the current literature and the 10-year experience of a surgical group from university teaching hospitals in Montréal, Québec and Toronto in performing laparoscopic colon and rectal surgery.
Methods
The prospectively designed case series comprised all patients having laparoscopic colon and rectal surgery. The procedures were carried out by a group of 4 surgeons between April 1991 and November 2001. We noted intraoperative complications, any conversions to open surgery, operating time, postoperative complications and postoperative length of hospital stay.
Results
The group attempted 750 laparoscopic colon and rectal procedures of which 669 were completed laparoscopically. Malignant disease was the indication for surgery in 49.6% of cases. Right hemicolectomy and sigmoid colectomy accounted for 54.5% of procedures performed. Intraoperative complications occurred in 8.3%, with 29.0% of these resulting in conversion to open surgery. The overall rate of conversion to open surgery was 10.8%, most commonly for oncologic concerns. Median operating time was 175 minutes for all procedures. Postoperative complications occurred in 27.5% of procedures completed laparoscopically but were mostly minor wound complications. Pulmonary complications occurred in only 1.0%. The anastomotic leak rate was 2.5%. The early reoperation rate was 2.4%. Postoperative mortality was 2.2%. No port site metastases have yet been detected. The median postoperative length of stay was 5 days.
Conclusions
The clinical outcomes of laparoscopic colon and rectal surgery in this 10-year experience are consistent with numerous cohort studies and randomized clinical trials. Laparoscopic colon and rectal surgery in the hands of well-trained surgeons can be performed safely with short hospital stay, low analgesic requirements and acceptable complication rates compared with historical controls and other reports in the literature. Evidence from published randomized clinical trials is emerging that under these conditions laparoscopic resection represents the better treatment option for most benign conditions, but concerns regarding its appropriateness for malignant disease are still to be resolved.
Abstract
Introduction
La chirurgie du côlon et du rectum par laparoscopie ne semble pas offrir autant d'avantages que d'autres interventions par laparoscopie. Afin d'étudier la question plus à fond, nous avons décidé d'analyser les publications courantes et l'expérience de la chirurgie du côlon et du rectum par laparoscopie acquise en 10 ans par un groupe chirurgical d'hôpitaux d'enseignement universitaires de Montréal, Québec et Toronto.
Méthodes
L'étude de cas prospective a regroupé tous les patients ayant subi une chirurgie du côlon et du rectum par laparoscopie. Les interventions ont été réalisées par un groupe de quatre chirurgiens entre avril 1991 et novembre 2001. Nous avons pris note des complications intraopératoires, des conversions à la chirurgie ouverte, de la durée de l'intervention, des complications postopératoires et de la durée du séjour à l'hôpital après l'intervention.
Résultats
Le groupe a tenté de réaliser 750 interventions par laparoscopie au côlon et au rectum. Il en a terminé 669 par laparoscopie. Une atteinte maligne était une indication de chirurgie dans 49,6 % des cas. L'hémicolectomie droite et la colectomie sigmoïde ont représenté 54,5 % des interventions réalisées. Il s'est produit des complications intraopératoires dans 8,3 % des cas, et 29,0 % ont entraÎné une conversion à la chirurgie ouverte. Le taux global de conversion à la chirurgie ouverte s'est établi à 10,8 %, le plus souvent à cause de problèmes d'ordre oncologique. La durée médiane de l'intervention a atteint 175 minutes. Il y a eu des complications postopératoires dans 27,5 % des laparoscopies, mais il s'agissait surtout de complications mineures au niveau de la plaie. Seulement 1,0 % des patients ont eu des complications pulmonaires. Le taux de fuite à l'anastomose a atteint 2,5 %, le taux de nouvelle intervention précoce, 2,4 %, et le taux de mortalité postopératoire, 2,2 %. On n'a pas détecté jusqu'ici de métastases au site de l'orifice. La durée médiane du séjour après l'intervention s'est établie à cinq jours.
Conclusions
Les résultats cliniques de la chirurgie du côlon et du rectum par laparoscopie au cours de cette expérience d'une durée de 10 ans sont conformes aux résultats d'un grand nombre d'études de cohorte et d'études cliniques randomisées. Pratiquée par des chirurgiens ayant reçu une solide formation, la chirurgie du côlon et du rectum par laparoscopie est sans danger et entraÎne un bref séjour à l'hôpital, de faibles besoins en analgésiques et des taux de complications acceptables comparativement aux témoins historiques et à d'autres comptes rendus dans les écrits scientifiques. On commence à réunir des données probantes tirées d'essais cliniques randomisés publiés qui indiquent que dans ces conditions, la résection par laparoscopie représente le meilleur traitement possible pour la plupart des problèmes bénins, mais il reste à en déterminer la pertinence dans celui des maladies malignes.
The introduction of laparoscopic cholecystecomy in the late 1980s by Muhe and Mouret ushered in the modern era of minimally invasive surgery. The benefit to patients of reduced pain, shortened hospital stay and faster recovery along with superior cosmesis rapidly resulted in laparoscopic cholecystectomy becoming the standard of care.1,2 Similar benefits were anticipated as the laparoscopic approach was subsequently applied to nearly all aspects of abdominal surgery. In fact, in centres where the technical expertise is available, laparoscopic splenectomy, adrenalectomy and Nissen fundoplication have now become the preferred method of treatment.3,4,5
The first reports of laparoscopic colectomy were published in 1991.6,7 Although numerous large case series, cohort studies and recent randomized trials have attested to similarly improved outcomes compared to open surgery, acceptance of the laparoscopic approach for colon and rectal surgery has lagged behind other laparoscopic procedures. The reasons for this undoubtedly include the technically demanding nature of this approach, the requirement for increased operating room resources, a lack of available training opportunities and early concerns about the treatment of malignant disease. Additionally, the magnitude of improvement seems attenuated compared with other laparoscopic procedures, leaving some skepticism of the overall benefits.
The purpose of this paper is to review the large experience over the past decade of a single surgical group routinely and consistently offering the laparoscopic approach to patients requiring colon and rectal surgery and to survey the contemporary literature.
Methods
Beginning with the first procedure performed, all patients scheduled to undergo attempted laparoscopic colon and rectal surgery by this group, between April 1991 and November 2001, were entered into a prospectively designed, computerized database. Data collected included patient demographics, information on comorbid conditions, indication for surgery, surgeon, procedure performed, intra- and postoperative complications, operating time (skin-to-skin), length of postoperative hospital stay and postoperative follow-up to the most recent office visit.
Patients were unselected, consecutive referrals to 1 of 4 academic surgeons (E.C.P., J.M., R.G., C.M.S.) practising in university teaching hospitals that provide resident and fellow training in advanced minimally invasive surgery. All 4 surgeons routinely offered all elective patients a laparoscopic approach with the result that there was no case selection by the surgeon. This does not account for possible case selection by referring physicians.
Fellow and resident trainees were involved in all cases and performed some or all of the procedure according to their level of experience. All patients received preoperative prophylaxis for deep venous thrombosis, broad-spectrum parenteral antibiotics and an oral bowel preparation when appropriate. All patients provided informed consent for the planned laparoscopic procedure.
Statistical analyses consisted of the Student t-test, the χ2 test or rank sum test for nonparametric data where appropriate. A p value of 0.05 was considered statistically significant.
Surgical technique
For right-side colon resections, patients are positioned supine and the bladder is catheterized. A 12-mm blunt-tipped trocar is inserted through the umbilicus using an open technique. After insufflating a carbon dioxide pneumoperitoneum to 15 mm Hg, a 30° viewing 10-mm laparoscope connected to a 1- or 3-chip charge-coupled device (CCD) camera is inserted. Two or 3 video monitors are positioned with at least 1 on each side of the patient. These are moved regularly throughout the procedure to ensure that the surgeon is always operating facing a monitor and the operating assistant has an ergonomic view of the procedure. Operating trocar placement is variable. Two or 3 additional 5-mm trocars are used, with one placed in the left lower quadrant and another suprapubically or in the epigastrium, or both. With the patient in a steep Trendelenburg position, the small bowel is extracted from the pelvis, and the cecum and ascending colon are mobilized with electrocautery. The patient is then levelled while the omentum is transected or detached from the transverse colon, and the hepatic flexure taken down. Once the colon is mobilized so that the ileocecal junction can be brought above the umbilicus, the hepatic flexure can be brought below the umbilicus and both can be brought across the midline, division of the mesentery, bowel resection and anastomosis are performed extracorporeally through a 4- to 5-cm extension of the umbilical trocar site.
For left-side colon resections and rectal resections, 3 operating trocars are used in addition to the umbilical trocar. A 12-mm trocar is placed in the right lower quadrant, and 5-mm trocars are placed in the left lower quadrant and left upper quadrant. In steep Trendelenburg position, with the small bowel out of the pelvis, the sigmoid colon and descending colon are mobilized along the white line of Toldt. The left ureter is identified. The sigmoid colon is elevated, and a window is created in the sigmoid mesocolon by identification and high ligation of the inferior mesenteric vessels, leaving 3 secure clips on the patient's side of each vessel. Proximal and distal mesenteric division is performed intracorporeally with electrocautery. For low rectal resections, with excellent visualization, the presacral space is easily entered and dissected while avoiding injury to the pelvic autonomic plexus. The bowel is divided distally with a linear endoscopic stapler and delivered though a muscle-splitting 4- to 5-cm extension of the left lower quadrant trocar site. The proximal bowel resection, sizing and insertion of the anvil of an endoluminal circular stapler are performed extracorporeally. The incision is closed before reinsufflation and stapled reanastomosis under laparoscopic visualization. The splenic flexure is mobilized as necessary for a tension-free anastomosis.
For abdominoperineal resection or proctectomy, the rectum is mobilized laparoscopically to the levator muscles before performing a standard perineal dissection. If 2 teams are used, care is taken not to enter the pelvis and release the pneumoperitoneum before full laparoscopic rectal mobilization is complete. Ileal pelvic pouches were fashioned extracorporeally through a Pfannenstiel incision before stapled anastomosis under laparoscopic visualization.
Results
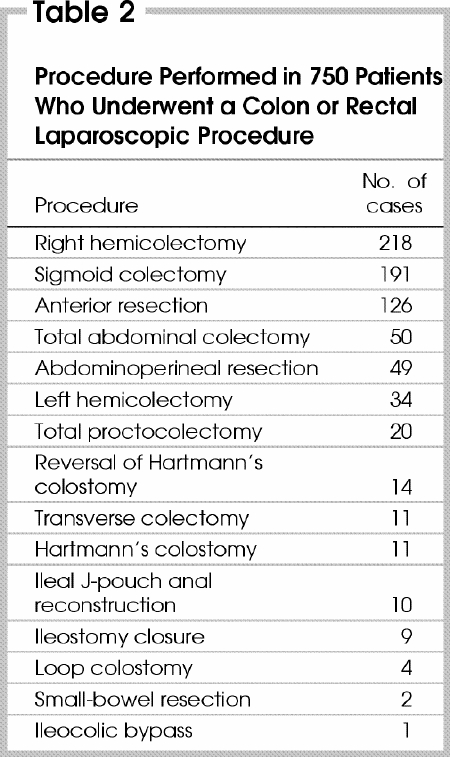
A total of 750 laparoscopic colon and rectal procedures were performed. They were fairly evenly divided among the 4 surgeons (250, 203, 197 and 100). Of the patients, 52% were female and the mean (and standard deviation [SD]) age was 59.0 (17.9) years (range from 12–94 yr) and mean (and SD) weight was 69.7 (16.4) kg (range from 36.5–150 kg). The indication for surgery was malignant disease in 372 (49.6%) cases (Table 1). Right hemicolectomy and sigmoid colectomy accounted for 409 (54.5%) of all procedures performed (Table 2).
Table 1
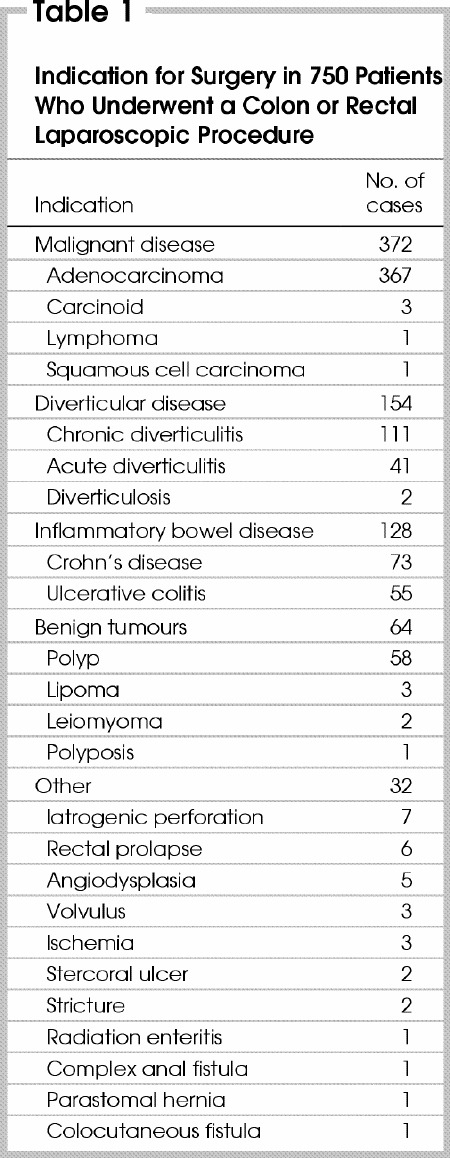
Table 2
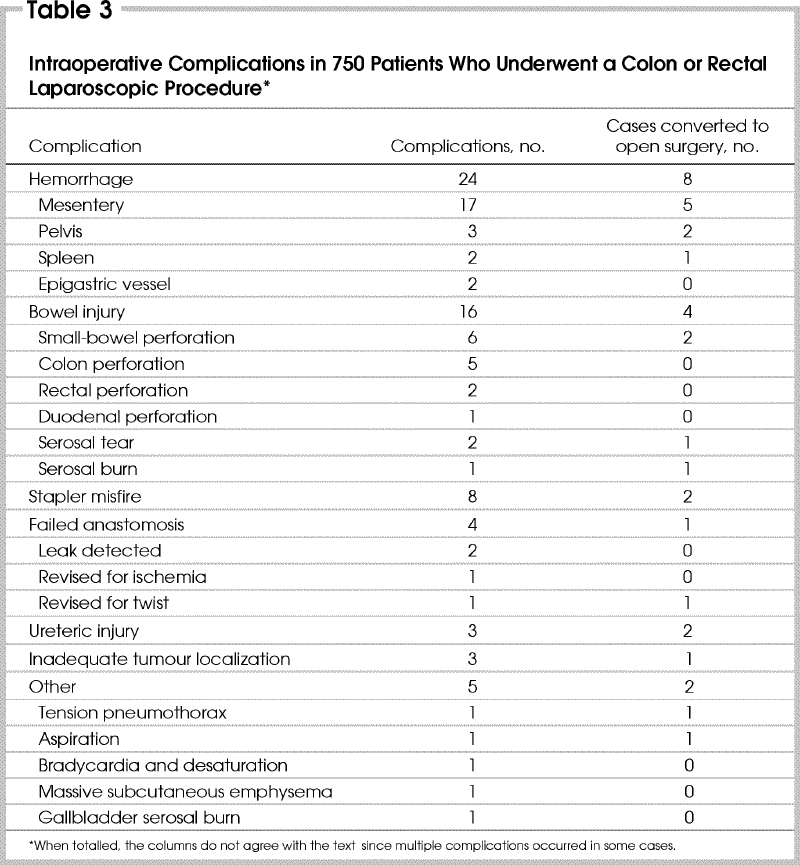
Intraoperative complications (Table 3) occurred in 62 (8.3%) patients. Most intraoperative complications were managed laparoscopically, with 18 (29.0%) patients requiring conversion to open surgery. The complication was not always the cause of conversion.
Table 3
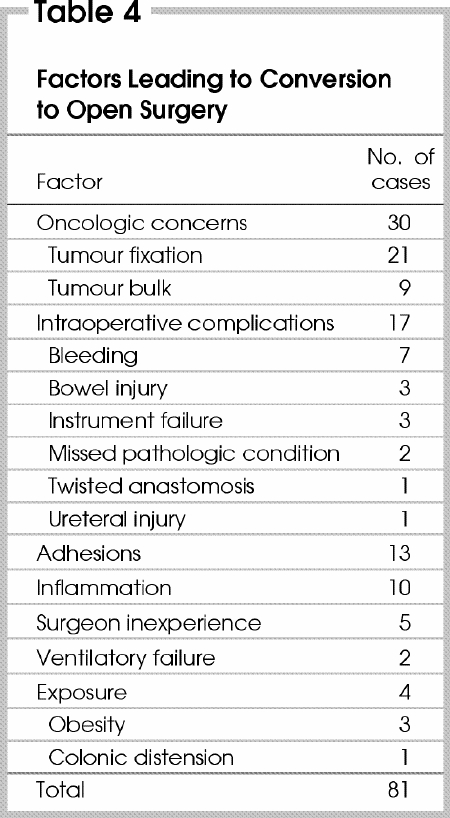
Conversion to open surgery was required in 81 (10.8%) cases overall (Table 4). The most common reasons for conversion were oncologic concerns in 30 (37%) cases. Compared with benign disease, patients were more likely to require conversion to open surgery if they underwent a laparoscopic procedure for malignant disease (13.4% v. 8.2%, p = 0.028). Patients requiring conversion to open surgery weighed significantly more than those having procedures completed laparoscopically (median 75.0 v. 67.6 kg, p < 0.001). There was a nonsignificant trend toward a higher conversion rate when we compared the first 50 procedures performed by each surgeon with subsequent procedures (12% v. 10.4%, p = 0.613). The conversion rate for the laparoscopic fellowship-trained surgeon's first 50 cases was 8%. Excluding the fellowship-trained surgeon's experience, the gap in conversion rates between each surgeon's first 50 cases and subsequent cases was wider (13.4% v. 9.4%) but still not significant (p = 0.216). Adhesions from previous surgery was the stated cause in 13 (16%) conversions.
Table 4
Median operating time was 175 (range from 50–450) minutes overall. For segmental resections only, the operating time was longer for procedures converted to open surgery than those completed laparoscopically (median 212 v. 165 min, p < 0.001).
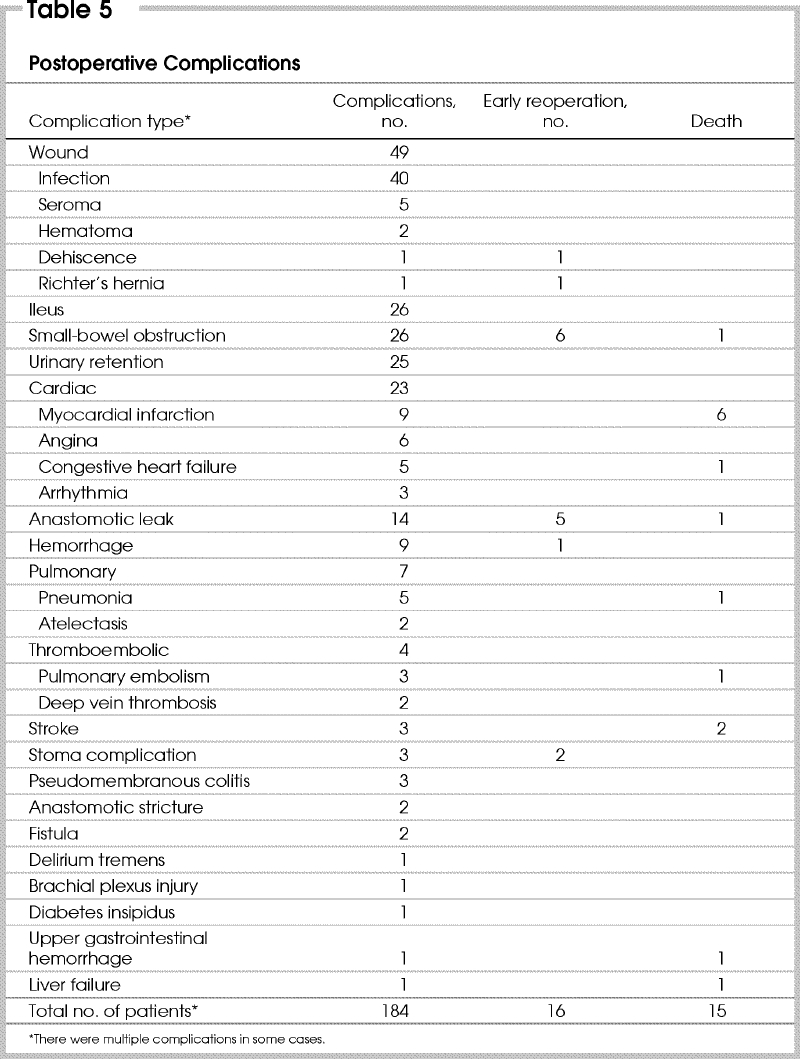
Of 669 procedures completed laparoscopically, postoperative complications occurred in 184 (27.5%). Most common were minor wound complications (Table 5). Twenty percent of wound infections occurred in a perineal wound and not at abdominal sites. There were only 7 pulmonary complications (1.0%). Postoperative ileus and small-bowel obstruction occurred with equal frequency (3.9%). The anastomotic leak rate was 2.5% (14 of the 555 laparoscopic procedures in which an anastomosis was performed). Sixteen patients (2.4%) required early reoperation for complications. Postoperative mortality was 2.2%. No recurrence of malignant disease at port sites has yet been detected.
Table 5
The median postoperative hospital stay for all procedures was 5 (range from 1–72) days with a mode of 4 days. Postoperative length of stay was longer if conversion to open surgery was required than if the laparoscopic approach was successful (median 7 v. 5 d, p < 0.001). Of the 669 patients having successful laparoscopic procedures, 114 (17%) were discharged home within 3 days of surgery, 241 (39%) within 4 days, and 381 (57%) within 5 days. One hundred and fifty-three (23%) patients stayed longer than 7 days, 104 (68%) of whom had postoperative complications. Patients having a postoperative complication had a significantly longer hospital stay than those without complications (median 9 v. 5 d, p < 0.001). Median time to resumption of full diet was 3 (range from 1–25) days. Twenty-seven (4.0%) of the 669 patients were discharged home on oral fluids. Median length of postoperative hospital stay declined from 6 days in the first half of the series to 5 days in the second half (p < 0.001).
Discussion
Whether laparoscopic colon and rectal surgery should become a standard or even a routine option for patients depends on a number of key factors. The approach must be technically feasible. The benefits must outweigh any potential disadvantages. Concerns regarding appropriateness for cure of malignant disease must be assuaged. It must be practically feasible, particularly with respect to resources and training.
From this review and others it is clear that with varying degrees of difficulty, colon and rectal procedures ranging from simple segmental resections to restorative proctocolectomy can be accomplished laparoscopically. The technical feasibility has been demonstrated. It remains the responsibility of the operating surgeon to ensure that established surgical principles are applied and that no “shortcuts” are taken simply to complete a procedure laparoscopically. A properly performed open procedure is always preferable to a poor laparoscopic attempt.
Conversion to open surgery is not a complication. It is a wise decision when the technical limitations of an attempted laparoscopic procedure exceed a surgeon's ability to ensure that sound surgical principles are applied. However, the effectiveness of the laparoscopic approach will depend on compliance. The anticipated benefits of the laparoscopic surgery will decline as conversion rates increase. Surgeons acquiring new experience with laparoscopic colon and rectal surgery may wish to select their patients and procedures based on anticipated difficulty and risk of conversion. From our own experience, we have developed a simple model for predicting conversion to open surgery. Our findings logically suggest that the risk of conversion rises with obesity, the presence of malignant disease and surgeon inexperience.8
The overall rates of intraoperative and postoperative complications in this series are well within the range reported in other large case series of laparoscopic colon resections (Table 6 9,10,11,12,13), even given that the data were collected prospectively with the attendant heightened sensitivity to outcomes. The recent 3-year audit of 15 427 open segmental colon resections in Illinois reported a rate of postoperative complications of 24.2% and 4.4% mortality,14 with which the present series compares favourably.
Table 6
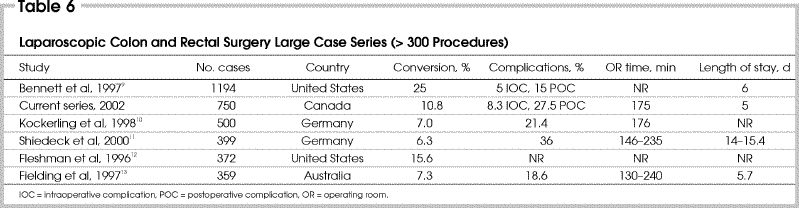
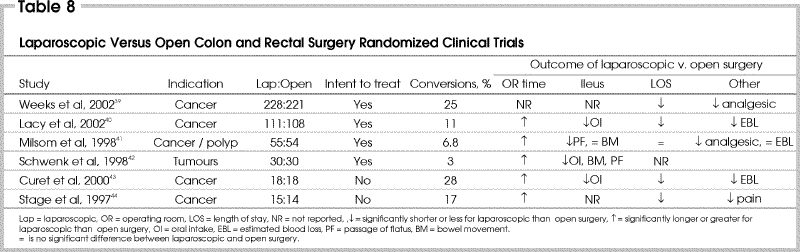
The short-term benefits of the laparoscopic approach have been suggested repeatedly but inconsistently in retrospective cohort studies (Table 7 15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38). The evidence is demonstrated more clearly in prospective randomized trials (Table 8 39,40,41,42,43,44). Excluding the voluntary registry of the American Society of Colon and Rectal Surgeons,9 the present study is the largest prospective case series yet published. Our own outcomes are in accordance with most published reports (Table 6). Although the improvement in recovery does not seem as dramatic as with end organ surgery, there should be little doubt that laparoscopic colon and rectal surgery results in less pain, less ileus and shorter hospital stay. The recent preliminary report of the multicentre, prospective, randomized trial by Weeks and associates,39 despite suspect quality-of-life assessments,45 clearly demonstrated a reduction in analgesic requirements and postoperative length of stay with laparoscopic surgery that is consistent with the findings of other reports. The improvement in outcomes was statistically significant even when analyzed on the basis of intent-to-treat. This is particularly impressive given the reported 25% rate of conversion to open surgery.
Table 7
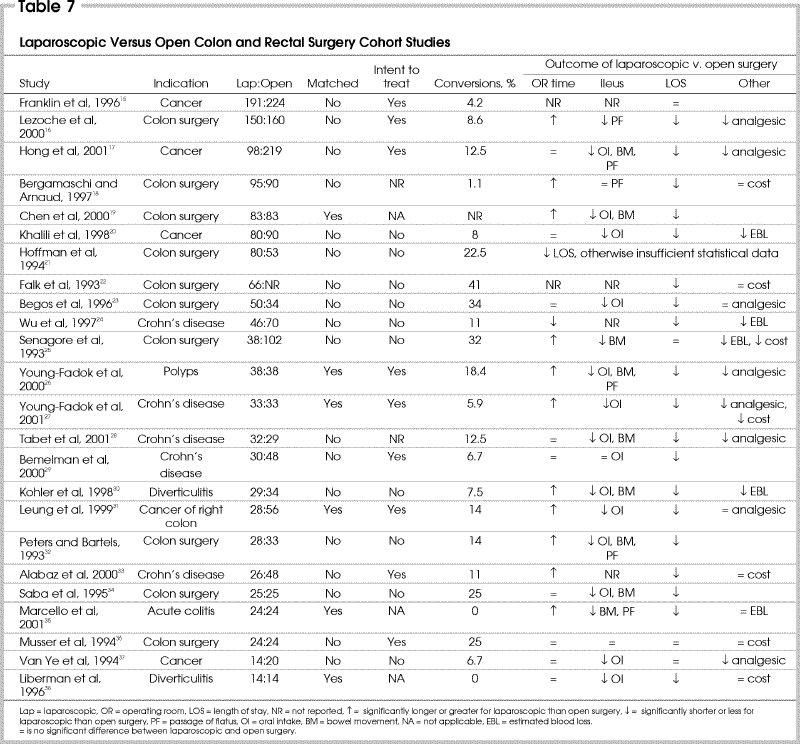
Table 8
No discussion on the presumed advantages of laparoscopic surgery would be complete without acknowledging the work of Holte and Kehlet on “fast track surgery,”46 who clearly demonstrated that whereas laparoscopic surgery may be an important way of reducing postoperative pain and ileus, it is not the only means of doing so. A multimodal approach of opioid-sparing analgesia, early enteral feeding and laparoscopy may have synergistic benefits that are greater than laparoscopy alone.
Our review does not specifically address the appropriateness of laparoscopic surgery for malignant disease except to demonstrate that we have not yet identified a single port-site recurrence. This is in keeping with the findings of other large series, suggesting the port-site recurrence rate in experienced hands should be around 1%,11,12,47,48 a rate that is similar to the experience with open surgery.49,50 Our own patients are followed closely, and favourable Kaplan–Meier survival curves from our experience have been published previously.51 The National Cancer Institute trial has completed accrual, and these findings along with other international prospective trials are anxiously anticipated. The one such study so far concluded is from Spain.40 This potentially landmark study has not only confirmed significant advantages with regard to improved recovery after laparoscopic surgery, but in a subgroup analysis has demonstrated that the laparoscopic approach is associated with a survival advantage for stage III colon cancers. It remains to be seen whether other studies confirm this finding. This could have significant implications for the value of the laparoscopic approach.
One of the largest stumbling blocks that remains for laparoscopic colon and rectal surgery is the issue of practical feasibility. There currently exist many barriers to the widespread introduction of this approach. Although most studies have suggested equivalent or reduced overall cost with laparoscopic surgery,18,22,25,27,33,36,38 there is clearly an increased cost when focusing on equipment and operating room resources. In the current health care environment, it is difficult to advocate for more operating room expenditure even if there may be a clear saving in inpatients beds.
Possibly a larger obstacle is the lack of available training opportunities. It is still debated whether a weekend course was ever sufficient instruction for laparoscopic cholecystectomy. Fortunately, the majority of surgeons now learning laparoscopic cholecystectomy are residents acquiring this skill through repeated exposure as a routine part of their general surgery residency program. This has only become possible because most university surgeons have acquired the necessary skills to teach this procedure. With laparoscopic colon and rectal surgery this is not yet the case. There are still only a few university instructors who can themselves perform these procedures, severely limiting exposure for trainees.
This issue is further complicated by surgical subspecialization. Any who have previously chosen to avoid laparoscopy by voluntarily leaving cholecystectomies to their general surgery colleagues have by now incurred a 10-year debt of experience with advanced laparoscopy. This adds another barrier to the acceptance and expansion of laparoscopic colon and rectal surgery within teaching centres.
Finally, under the current fee-for-service system, what is good for the patient is not necessarily good for the surgeon. Remuneration for laparoscopic procedures in Canada has traditionally been no different from that for open surgery. This holds for colon and rectal surgery, despite advanced training requirements, greater technical demands and necessarily longer operating times. This effectively creates a financial disincentive to perform this surgery, which will have to be addressed if surgeons are to voluntarily retrain for these procedures. In Ontario, a new fee code has recently been introduced for laparoscopic prostatectomy52 that may herald progress against this inequity.
Conclusions
We have demonstrated the safety, feasibility and good outcomes that can be achieved with laparoscopic colon and rectal surgery when performed by a small group of surgeons with sufficient technical expertise. We are currently at a cusp in the direction this approach will take. With adequate training and good judgement it is clear that recovery after laparoscopic surgery is improved. There should be no question of the appropriateness and value of this technique for benign disease. The evidence of superior short-term outcomes is available. The issue of suitability for cure of malignant disease will soon be resolved and may produce striking findings. Although laparoscopic colon and rectal surgery is still currently not the standard procedure, if outcomes with respect to malignant disease are equivalent or possibly superior to open surgery, then the last barriers to acceptance will fall. The demand for this approach may well overwhelm available resources and training opportunities.
Competing interests: None declared.
Correspondence to: Dr. Christopher M. Schlachta, Head, Division of General Surgery, 16-046CC, St. Michael's Hospital, 30 Bond St., Toronto ON M5B 1W8; fax 416 864-6006; christopher.schlachta@utoronto.ca
Accepted for publication May 13, 2003.
References
- 1.Litwin D, Girotti M, Poulin E, Mamazza J, Nagy AG. Laparoscopic cholecystectomy: trans-Canada experience with 2201 cases. Can J Surg 1992;35:291-6. [PubMed]
- 2.Soper NJ, Stockmann PT, Dunnegan DL, Ashley SW. Laparoscopic cholecystectomy. The new ‘gold standard’? Arch Surg 1992;127:917-21. [DOI] [PubMed]
- 3.Chekan EG, Pappas TN. The laparoscopic management of gastroesophageal reflux disease. Adv Surg 1999;32:305-30. [PubMed]
- 4.Friedman RL, Fallas MJ, Carroll BJ, Hiatt JR, Phillips EH. Laparoscopic splenectomy for ITP. The gold standard. Surg Endosc 1996;10:991-5. [DOI] [PubMed]
- 5.Smith CD, Weber CJ, Amerson JR. Laparoscopic adrenalectomy: new gold standard. World J Surg 1999;23:389-96. [DOI] [PubMed]
- 6.Fowler DL, White SA. Laparoscopy-assisted sigmoid resection. Surg Laparosc Endosc 1991;1:183-8. [PubMed]
- 7.Jacobs M, Verdeja JC, Goldstein HS. Minimally invasive colon resection (laparoscopic colectomy). Surg Laparosc Endosc 1991;1:144-50. [PubMed]
- 8.Schlachta CM, Mamazza J, Seshadri PA, Cadeddu MO, Poulin EC. Predicting conversions to open surgery in laparoscopic colorectal resections: a simple clinical model. Surg Endosc 2000;14:1114-7. [DOI] [PubMed]
- 9.Bennett CL, Stryker SJ, Ferreira MR, Adams J, Beart RW. The learning curve for laparoscopic colorectal surgery. Preliminary results from a prospective analysis of 1194 laparoscopic-assisted colectomies. Arch Surg 1997;132:41-4. [DOI] [PubMed]
- 10.Kockerling F, Schneider C, Reymond MA, Scheidbach H, Konradt J, Barlehner E, et al. Early results of a prospective multicenter study on 500 consecutive cases of laparoscopic colorectal surgery. Surg Endosc 1998;12:37-41. [DOI] [PubMed]
- 11.Schiedeck TH, Schwandner O, Baca I, Baehrlehner E, Konradt J, Kockerling F, et al. Laparoscopic surgery for the cure of colorectal cancer: results of a German five-center study. Dis Colon Rectum 2000;43:1-8. [DOI] [PubMed]
- 12.Fleshman JW, Nelson H, Peters WR, Kim HC, Larach S, Boorse RR, et al. Early results of laparoscopic surgery for colorectal cancer. Retrospective analysis of 372 patients treated by Clinical Outcomes of Surgical Therapy (COST) Study Group. Dis Colon Rectum 1996;39(10 Suppl):S53-8. [DOI] [PubMed]
- 13.Fielding GA, Lumley J, Nathanson L, Hewett P, Rhodes M, Stitz R. Laparoscopic colectomy. Surg Endosc 1997;11:745-9. [DOI] [PubMed]
- 14.Prystowski JB, Bordage G, Feinglass JM. Patient outcomes for segmental colon resection according to surgeon's training, certification, and experience. Surgery 2002;132:663-70. [DOI] [PubMed]
- 15.Franklin ME Jr, Rosenthal D, Abrego-Medina D, Dorman JP, Glass JL, Norem R, et al. Prospective comparison of open vs. laparoscopic colon surgery for carcinoma. Five-year results. Dis Colon Rectum 1996;39(10 Suppl):S35-46. [DOI] [PubMed]
- 16.Lezoche E, Feliciotti F, Paganini AM, Guerrieri M, Campagnacci R, De SA. Laparoscopic colonic resections versus open surgery: a prospective non-randomized study on 310 unselected cases. Hepatogastroenterology 2000;47:697-708. [PubMed]
- 17.Hong D, Tabet J, Anvari M. Laparoscopic vs. open resection for colorectal adenocarcinoma. Dis Colon Rectum 2001;44:10-8. [DOI] [PubMed]
- 18.Bergamaschi R, Arnaud JP. Immediately recognizable benefits and drawbacks after laparoscopic colon resection for benign disease. Surg Endosc 1997;11:802-4. [DOI] [PubMed]
- 19.Chen HH, Wexner SD, Iroatulam AJ, Pikarsky AJ, Alabaz O, Nogueras JJ, et al. Laparoscopic colectomy compares favorably with colectomy by laparotomy for reduction of postoperative ileus. Dis Colon Rectum 2000;43:61-5. [DOI] [PubMed]
- 20.Khalili TM, Fleshner PR, Hiatt JR, Sokol TP, Manookian C, Tsushima G, et al. Colorectal cancer: comparison of laparoscopic with open approaches. Dis Colon Rectum 1998;41:832-8. [DOI] [PubMed]
- 21.Hoffman GC, Baker JW, Fitchett CW, Vansant JH. Laparoscopic-assisted colectomy. Initial experience. Ann Surg 1994;219:732-40. [DOI] [PMC free article] [PubMed]
- 22.Falk PM, Beart RW Jr, Wexner SD, Thorson AG, Jagelman DG, Lavery IC, et al. Laparoscopic colectomy: a critical appraisal. Dis Colon Rectum 1993;36:28-34. [DOI] [PubMed]
- 23.Begos DG, Arsenault J, Ballantyne GH. Laparoscopic colon and rectal surgery at a VA hospital. Analysis of the first 50 cases. Surg Endosc 1996;10:1050-6. [DOI] [PubMed]
- 24.Wu JS, Birnbaum EH, Kodner IJ, Fry RD, Read TE, Fleshman JW. Laparoscopic-assisted ileocolic resections in patients with Crohn's disease: Are abscesses, phlegmons, or recurrent disease contraindications? Surgery 1997;122:682-8. [DOI] [PubMed]
- 25.Senagore AJ, Luchtefeld MA, Mackeigan JM, Mazier WP. Open colectomy versus laparoscopic colectomy: Are there differences? Am Surg 1993;59:549-53. [PubMed]
- 26.Young-Fadok TM, Radice E, Nelson H, Harmsen WS. Benefits of laparoscopic-assisted colectomy for colon polyps: a case-matched series. Mayo Clinic Proc 2000;75:344-8. [DOI] [PubMed]
- 27.Young-Fadok TM, HallLong K, McConnell EJ, Gomez Rey G, Cabanela RL. Advantages of laparoscopic resection for ileocolic Crohn's disease. Improved outcomes and reduced costs. Surg Endosc 2001;15:450-4. [DOI] [PubMed]
- 28.Tabet J, Hong D, Kim CW, Wong J, Goodacre R, Anvari M. Laparoscopic versus open bowel resection for Crohn's disease. Can J Gastroenterol 2001;15:237-42. [DOI] [PubMed]
- 29.Bemelman WA, Slors JF, Dunker MS, van Hogezand RA, van Deventer SJ, Ringers J, et al. Laparoscopic-assisted vs. open ileocolic resection for Crohn's disease. A comparative study. Surg Endosc 2000;14:721-5. [DOI] [PubMed]
- 30.Kohler L, Rixen D, Troidl H. Laparoscopic colorectal resection for diverticulitis. Int J Colorectal Dis 1998;13:43-7. [DOI] [PubMed]
- 31.Leung KL, Meng WC, Lee JF, Thung KH, Lai PB, Lau WY. Laparoscopic-assisted resection of right-sided colonic carcinoma: a case-control study. J Surg Oncol 1999;71:97-100. [DOI] [PubMed]
- 32.Peters WR, Bartels TL. Minimally invasive colectomy: Are the potential benefits realized? Dis Colon Rectum 1993;36:751-6. [DOI] [PubMed]
- 33.Alabaz O, Iroatulam AJ, Nessim A, Weiss EG, Nogueras JJ, Wexner SD. Comparison of laparoscopically assisted and conventional ileocolic resection for Crohn's disease. Eur J Surg 2000;166:213-7. [DOI] [PubMed]
- 34.Saba AK, Kerlakian GM, Kasper GC, Hearn AT. Laparoscopic assisted colectomies versus open colectomy. J Laparoendosc Surg 1995;5:1-6. [DOI] [PubMed]
- 35.Marcello PW, Milsom JW, Wong SK, Brady K, Goormastic M, Fazio VW. Laparoscopic total colectomy for acute colitis: a case-control study. Dis Colon Rectum 2001;44:1441-5. [DOI] [PubMed]
- 36.Musser DJ, Boorse RC, Madera F, Reed JF 3rd. Laparoscopic colectomy: At what cost? Surg Laparosc Endosc 1994;4:1-5. [PubMed]
- 37.Van Ye TM, Cattey RP, Henry LG. Laparoscopically assisted colon resections compare favorably with open technique. Surg Laparosc Endosc 1994;4:25-31. [PubMed]
- 38.Liberman MA, Phillips EH, Carroll BJ, Fallas M, Rosenthal R. Laparoscopic colectomy vs traditional colectomy for diverticulitis. Outcome and costs. Surg Endosc 1996;10:15-8. [DOI] [PubMed]
- 39.Weeks JC, Nelson H, Gelber S, Sargent D, Schroeder G. Clinical outcomes of surgical therapy. Short-term quality-of-life outcomes following laparoscopic-assisted colectomy vs open colectomy for colon cancer: a randomized trial. JAMA 2002;287:321-8. [DOI] [PubMed]
- 40.Lacy AM, Garcia-Valdecasas JC, Delgado S, Castells A, Taura P, Pique JM, et al. Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet 2002;359:2224-9. [DOI] [PubMed]
- 41.Milsom JW, Bohm B, Hammerhofer KA, Fazio V, Steiger E, Elson P. A prospective, randomized trial comparing laparoscopic versus conventional techniques in colorectal cancer surgery: a preliminary report. J Am Coll Surg 1998;187:46-54. [DOI] [PubMed]
- 42.Schwenk W, Bohm B, Haase O, Junghans T, Muller JM. Laparoscopic versus conventional colorectal resection: a prospective randomised study of postoperative ileus and early postoperative feeding. Langenbecks Arch Surg 1998;383:49-55. [DOI] [PubMed]
- 43.Curet MJ, Putrakul K, Pitcher DE, Josloff RK, Zucker KA. Laparoscopically assisted colon resection for colon carcinoma: perioperative results and long-term outcome. Surg Endosc 2000;14:1062-6. [DOI] [PubMed]
- 44.Stage JG, Schulze S, Moller P, Overgaard H, Andersen M, Rebsdorf-Pedersen VB, et al. Prospective randomized study of laparoscopic versus open colonic resection for adenocarcinoma. Br J Surg 1997;84:391-6. [PubMed]
- 45.Urbach DR. Laparoscopic-assisted surgery for colon cancer [letter] [see comment]. JAMA 2002;287:1938. Comment on: JAMA 2002;287:321-8.11960530
- 46.Holte K, Kehlet H. Postoperative ileus: a preventable event. Br J Surg 2000;87: 1480-93. [DOI] [PubMed]
- 47.Vukasin P, Ortega AE, Greene FL, Steele GD, Simons AJ, Anthone GJ, et al. Wound recurrence following laparoscopic colon cancer resection. Results of the American Society of Colon and Rectal Surgeons Laparoscopic Registry. Dis Colon Rectum 1996;39(10 Suppl):S20-3. [DOI] [PubMed]
- 48.Zmora O, Weiss EG. Trocar site recurrence in laparoscopic surgery for colorectal cancer. Myth or real concern? [review] Surg Oncol Clin N Am 2001;10:625-38/ [PubMed]
- 49.Reilly WT, Nelson H, Schroeder G, Wieand HS, Bolton J, O'Connell MJ. Wound recurrence following conventional treatment of colorectal cancer. A rare but perhaps underestimated problem. Dis Colon Rectum 1996;39:200-7. [DOI] [PubMed]
- 50.Hughes ES, McDermott FT, Polglase AL, Johnson WR. Tumor recurrence in the abdominal wall scar tissue after large-bowel cancer surgery. Dis Colon Rectum 1983;26:571-2. [DOI] [PubMed]
- 51.Poulin EC, Mamazza J, Schlachta CM, Gregoire R, Roy N. Laparoscopic resection does not adversely affect early survival curves in patients undergoing surgery for colorectal adenocarcinoma. Ann Surg 1999;229:487-92. [DOI] [PMC free article] [PubMed]
- 52. Schedule of benefits: physician services under the Health Insurance Act. Toronto: Ontario Ministry of Health and Long-Term Care; 2002.


