Abstract
Introduction
Obesity has been described as a risk factor for the development of coronary artery disease, but it has not been determined whether obesity is associated with adverse outcomes after cardiac surgery. Therefore, we analyzed a large cohort of patients who had undergone cardiac surgery to determine whether obesity is a predictor of mortality, morbidity or early readmission to hospital.
Methods
At the London Health Sciences Centre, an academic tertiary care centre, we prospectively entered data from the cardiac surgical database from July 1999 to April 2002. We collected data on 1310 consecutive, unselected patients who underwent cardiac surgery during that time. We assessed the degree of obesity using the body mass index (BMI), and we prospectively documented the occurrence of 10 major complications after surgery. They included stroke, reoperation for bleeding, life-threatening cardiac arrest or arrhythmia, new renal failure requiring dialysis, septicemia, mediastinitis, sternal dehiscence, respiratory failure, postoperative myocardial infarction and low cardiac output necessitating intra-aortic balloon pump use. Univariable and multivariable analyses were conducted to determine the factors associated with and predictive of postoperative death and major complications.
Results
An increased BMI did not increase the risk of early postoperative death. Furthermore, increased BMI was not a predictor of a patient experiencing any of the major complications, except sternal dehiscence. An increased BMI was associated with a higher likelihood of readmission to hospital within 30 days of discharge.
Conclusion
Obesity was not associated with adverse outcomes after cardiac operations, aside from the increased risks of sternal dehiscence and early hospital readmission.
Abstract
Introduction
On a décrit l'obésité comme un facteur de risque d'apparition de coronaropathie, mais on n'a pas déterminé s'il y a un lien entre l'obésité et des résultats indésirables après une chirurgie cardiaque. C'est pourquoi nous avons analysé une cohorte importante de patients qui avaient subi une chirurgie cardiaque afin de déterminer si l'obésité est un prédicteur de mortalité, de morbidité ou de réhospitalisation précoce.
Méthodes
Au Centre des sciences de la santé de London, centre universitaire de soins tertiaires, nous avons entré de façon prospective des données tirées de la base de données sur les chirurgies cardiaques de juillet 1999 à avril 2002. Nous avons recueilli des données sur 1310 patients consécutifs non sélectionnés qui ont subi une chirurgie cardiaque au cours de cette période. Nous avons évalué le degré d'obésité au moyen de l'indice de masse corporelle (IMC) et nous avons documenté de façon prospective l'occurrence de 10 complications principales après la chirurgie, notamment les suivantes : accident vasculaire cérébral, nouvelle intervention pour saignement, arrêt ou arythmie cardiaque menaçant la vie, nouvelle insuffisance rénale exigeant une dialyse, septicémie, médiastinite, déhiscence du sternum, insuffisance respiratoire, infarctus du myocarde après l'intervention et faible débit cardiaque obligeant à utiliser la contrepulsion intra-aortique. On a procédé à des analyses à variable unique et à variables multiples pour déterminer les facteurs prédicteurs de la mort postopératoire et de complications majeures associées à ces problèmes.
Résultats
Une élévation de l'IMC n'a pas augmenté le risque de mortalité postopératoire précoce. De plus, une élévation de l'IMC ne permettait pas de prédire qu'un patient aurait une des complications majeures, sauf dans le cas de la déhiscence du sternum. On a établi un lien entre une élévation de l'IMC et une probabilité plus élevée de réhospitalisation dans les 30 jours suivant le congé.
Conclusion
On n'a pas établi de lien entre l'obésité et des résultats indésirables après des interventions de chirurgie cardiaque, sauf dans le cas du risque accru de déhiscence du sternum et de réhospitalisation précoce.
It is commonly thought that obesity has a negative impact on surgical outcomes, but there is little supporting evidence. Obesity has been described as a risk factor for coronary artery disease, but several studies have demonstrated that obesity may not be a risk factor for significant adverse outcomes after cardiac surgery.1,2,3
We analyzed the findings in a large cohort of patients after cardiac surgery to determine whether obesity is a risk factor for mortality, morbidity, length of stay in hospital, or readmission.
Patients and method
Between July 1999 and April 2002, data entered prospectively into the London Health Sciences Centre cardiac surgical database were collected for 1310 consecutive, unselected patients who underwent cardiac surgery, excluding patients who received a transplant. The degree of obesity was assessed from the body mass index (BMI), which is a well-validated measurement of percent body fat. The common definition of obesity is a BMI greater than 30.1
We documented 10 major complications after cardiac surgery: low cardiac output requiring intra-aortic balloon pumping postoperatively, neurologic complications, reoperation for bleeding, life-threatening arrest or arrhythmia, renal failure requiring dialysis, septicemia, mediastinitis, sternal dehiscence, respiratory failure and myocardial infarction. Operational definitions of these complications have been listed in a recent publication from our centre.4
Both univariable and multivariable analyses were employed to determine the factors associated with and independently predictive of the occurrence of death or any of the major complications, the postoperative length of hospital stay and readmission rates. Linear regression was used to model length of hospital stay, and logistic regression was used to model the occurrence of death or one of the major complications and readmission rates. The C index and Hosmer–Lemeshow goodness-of-fit p values were calculated for all multivariable logistic regression models. Continuous data were presented as means (and standard deviations) and categorical data as incidence rates. The level of significance was set at 5% (p < 0.05).
Results
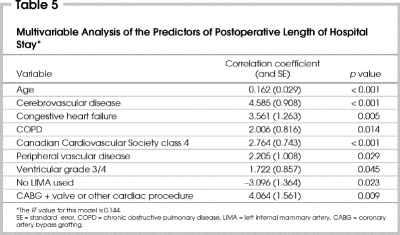
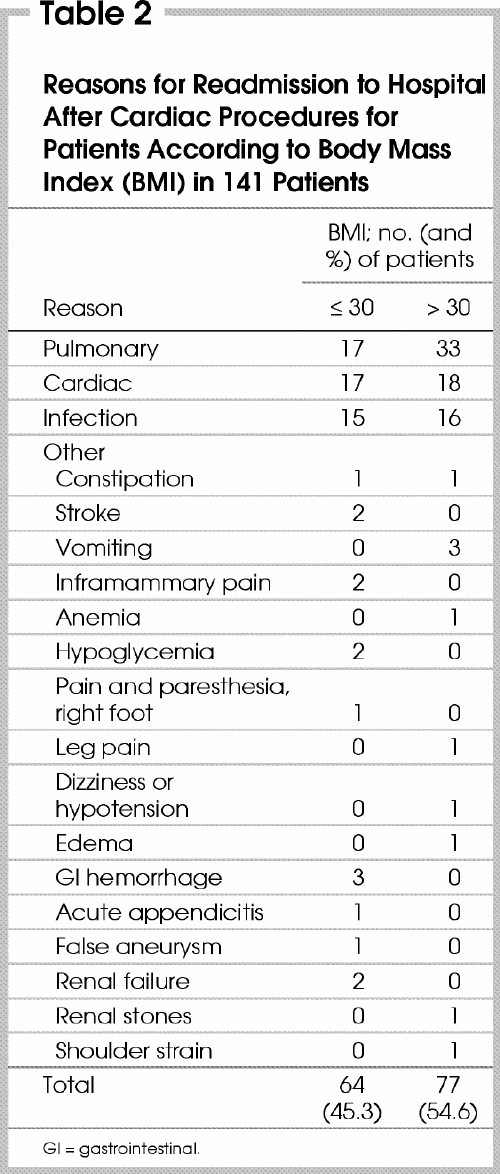
The study cohort included 1310 patients (958 men and 352 women), with a median age of 66.7 years (range 26.3–86.9 yr). To determine the univariable association of obesity with postoperative outcomes, the patients were divided into 2 groups: BMI of 30 or less (846 patients) and BMI greater than 30 (464 patients). The latter group had a significantly higher rate of sternal dehiscence and readmission within 30 days of discharge (Table 1), whereas the former group had a significantly higher rate of arrest or arrhythmia. There were no significant differences during the study period in the incidence of death or any of the 10 major complications aside from sternal dehiscence (Table 1). Furthermore, postoperative lengths of stay were almost identical in the 2 groups. A total of 141 patients (10.8%) were readmitted to hospital within 30 days of discharge. The reasons for readmission (Table 2) were pulmonary (50 patients), cardiac (35), infection (31) and other (25).
Table 1
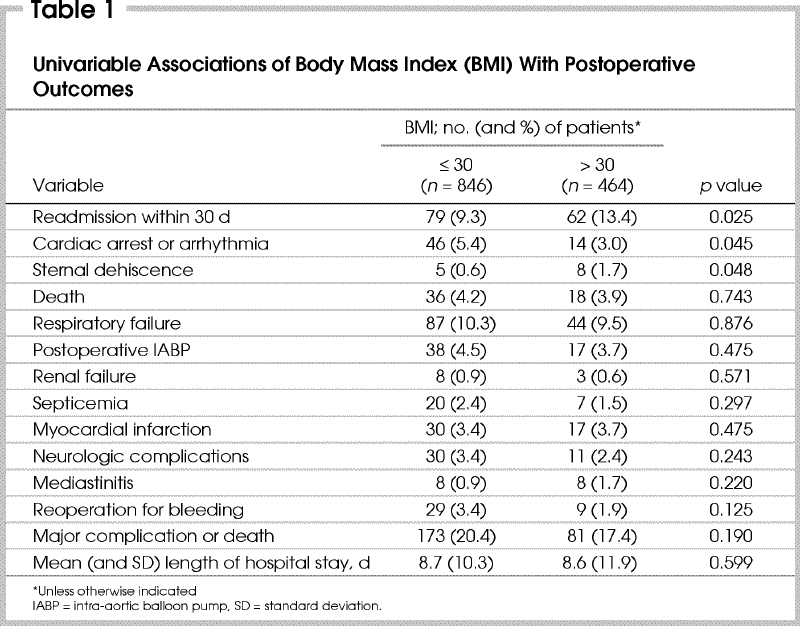
Table 2
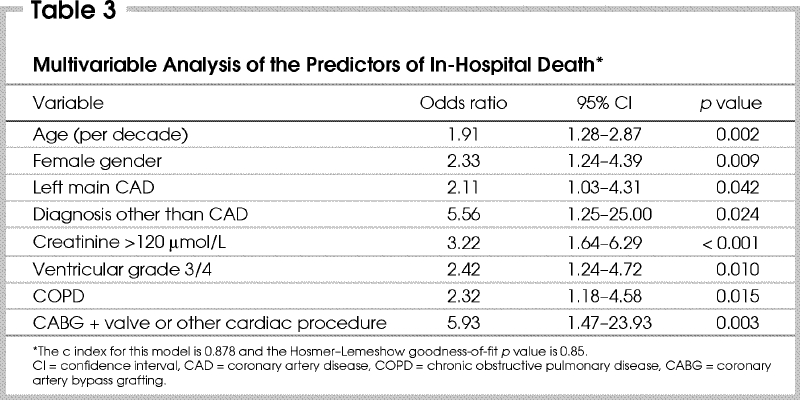
A BMI greater than 30 was not associated with postoperative death (Table 3). The variables that predicted significantly higher rates of death on multivariable analysis were increasing age, female gender, ventricular grade 3 or 4, a diagnosis other than coronary artery disease, combined coronary artery bypass grafting and a valve or other cardiac operation, left main disease, chronic obstructive pulmonary disease and a serum creatinine level greater than 120 μmol/L.
Table 3
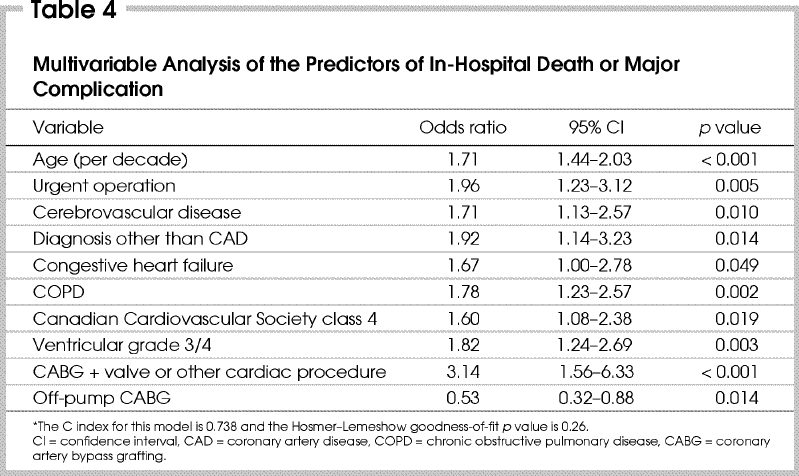
A logistic regression analysis for the composite outcome of any of the 10 major complications or death (Table 4) also revealed no significant influence by BMI greater than 30 as a predictive variable. The variables that predicted a significantly higher rate of major complications or death were increasing age, combined coronary artery bypass grafting and valve or other cardiac operation, chronic obstructive pulmonary disease, left ventricular grade 3 or 4, urgent operation, cerebrovascular disease, diagnosis of other than coronary artery disease, Canadian Cardiovascular Society (CCS) class 4 status and congestive heart failure (Table 4). Off-pump coronary bypass grafting was predictive of a lower risk of this composite outcome in our study (Table 4).
Table 4
A linear regression model of the independent predictors of postoperative length of hospital stay showed no significant impact of BMI (Table 5). The factors that predicted an increased length of hospital stay included increasing age, CCS class 4 status, cerebrovascular disease, congestive heart failure diagnosed within 30 days before the operation, combined coronary artery bypass grafting and valve or other cardiac operation, chronic obstructive pulmonary disease, non-use of the left internal mammary artery as a bypass graft, peripheral vascular disease and a left ventricular grade of 3 or 4.
Table 5
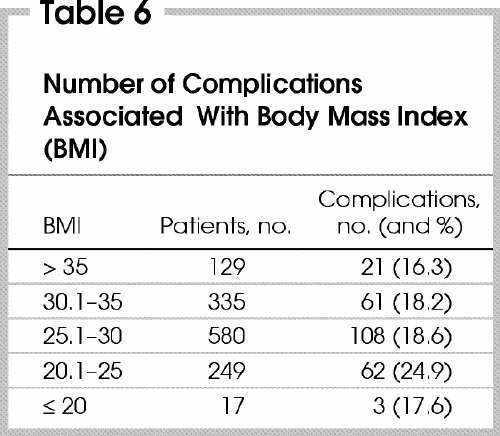
When the patients were divided into 5 groups according to BMI, the number of patients with postoperative complications was similar in those with a BMI of 30 or less and greater than 35 but was highest in those with a BMI between 20.1 and 25 (Table 6). There were no significant differences among groups with respect to the incidence of major complications (p = 0.16).
Table 6
Discussion
This study demonstrated that a high BMI does not increase the risk of death and most complications after cardiac surgery. Though some studies have found evidence that a BMI above 30 is predictive of an increased chance of morbidity,1,3,4,5 we demonstrated that increased BMI was not a predictor of any of the 10 major complications (except sternal dehiscence) but was associated with an increased rate of readmission to hospital within 30 days of discharge. Other studies1,2,3,5 have found that obesity increases the risk of sternal wound infection and leg infections but not in-hospital death. Quoted risk factors for sternal wound infection, which included diabetes mellitus, bilateral internal mammary artery bypass grafting, time on bypass, postoperative hemorrhage, age, renal failure and chronic obstructive pulmonary disease,2 were similar to many of our study's risk factors for increased morbidity. The significance of sternal dehiscence and mediastinitis should not be underestimated, as there is a much greater inconvenience to the patient in regard to long-term consequences such as reoperation and graft patency. Prasad and associates3 concluded that in patients with diabetes, obesity added to the risk of wound infection.
Although obesity is a well recognized risk factor for the development of coronary artery disease, Fasol and colleagues6 found it a risk factor for only certain complications after coronary artery bypass grafting. Theories as to why obese patients may incur select postoperative complications include a greater myocardial workload, inadequate myocardial protection of a hypertrophied heart, an imbalance in myocardial oxygen demand and supply, and decreased respiratory muscle reserve.3 Another study postulated that the problems with wound surveillance, the large, poorly vascularized panniculus and the higher incidence of hyperglycemia in the obese patient contributed to postoperative complications.1 Many obese patients are diabetic, and diabetes mellitus itself confers an added risk of impaired wound healing and heart disease. Nonetheless, our data did not show that diabetes was an independent predictor of major postoperative complications.
Obesity has been commonly thought to affect the risk of heart disease indirectly, but a recent study has demonstrated an increased BMI as a significant independent predictor for the development of heart failure.7 Although the mechanism remains unknown, this study emphasizes the importance of lifestyle modification in reducing the risk of cardiac morbidity and mortality.
In our study, there was a significant association of patients with a BMI greater than 30 and readmission to hospital. This indicates that obese patients require more intensive postoperative follow-up to reduce the subsequent need for readmission.
A recent study of geriatric patients (mean age, 79 yr) who underwent cardiac surgery divided patients in tertiles of BMI (< 23, 23–26 and > 26), grouping all overweight (BMI > 25) and obese (BMI > 30) patients together.8 A U-shaped relationship between BMI and postoperative complications or death revealed, with the highest incidence in the first tertile, less in the last tertile and the lowest incidence in the middle tertile. Thus, in the geriatric population, patients with a low BMI have a higher risk of complications and death after cardiac surgery than those with a high BMI. These investigators also found that an increased BMI confers no increase in the risk of postoperative complications except for wound infections.8 Another study found that the thinnest patients had more risk factors for postoperative morbidity and mortality.4 The authors' hypothesis was that these patients may have less nutritional reserve, which may not allow them to handle complications well. These results did not agree with those of our study, in which patients with a BMI of 20 or less had fewer complications than those with a BMI between 30.1 and 35 (Table 6).
Although we found no association between obesity, postoperative mortality and the occurrence of most complications after surgery, it would still be advisable for patients to achieve a normal weight, since the literature has confirmed a positive correlation between BMI greater than 30 and readmission, coronary artery disease, hypercholesteremia,6 heart failure,7 type II diabetes mellitus and hypertension.1 Further research needs to be done to study the impact of obesity on the intermediate and long-term outcomes of patients after cardiac operations.
Presented at the South Western Ontario Surgeons Association meeting, London, Ont., Nov. 6, 2002.
Competing interests: None declared.
Correspondence to: Dr. Richard J. Novick, Division of Cardiac Surgery, University Campus, London Health Sciences Centre, PO Box 5339, 339 Windermere Rd., London ON N6A 5A5; fax 519 663-3182; richard.novick@lhsc.on.ca
Accepted for publication Nov. 3, 2003.
References
- 1.Moulton MJ, Creswell LL, Mackey ME, Cox JL, Rosenbloom M. Obesity is not a risk factor for significant adverse outcomes after cardiac surgery. Circulation 1996;94(9 Suppl):II87-92. [PubMed]
- 2.Birkmeyer NJ, Charlesworth DC, Hernandez F, Leavitt BJ, Marrin CA, Morton JR, et al. Obesity and risk of adverse outcomes associated with coronary artery bypass surgery. Northern New England Cardiovascular Disease Study Group. Circulation 1998;97:1689-94. [DOI] [PubMed]
- 3.Prasad US, Walker WS, Sang CT, Campanella C, Cameron EW. Influence of obesity on the early and long term results of surgery for coronary artery disease. Eur J Cardiothorac Surg 1991;5:67-73. [DOI] [PubMed]
- 4.Novick RJ, Fox SA, Stitt LW, Swinamer SA, Lehnhardt KR, Rayman R, et al. Cumulative sum failure analysis of a policy change from on-pump to off-pump coronary artery bypass grafting. Ann Thorac Surg 2001;72:S1016-21. [DOI] [PubMed]
- 5.Engelman DT, Adams DH, Byrne JG, Aranki SF, Collins JJ Jr, Couper GS, et al. Impact of body mass index and albumin on morbidity and mortality after cardiac surgery. J Thorac Cardiovasc Surg 1999;118:866-73. [DOI] [PubMed]
- 6.Fasol R, Schindler M, Schumacher B, Schlaudraff K, Hannes W, Seitelberger R, et al. The influence of obesity on perioperative morbidity: retrospective study of 502 aortocoronary bypass operations. Thorac Cardiovasc Surg 1992;40:126-9. [DOI] [PubMed]
- 7.Massie BM. Obesity and heart failure — risk factor or mechanism? N Engl J Med 2002;347:358-9. [DOI] [PubMed]
- 8.Maurer MS, Luchsinger JA, Wellner R, Kukuy E, Edwards NM. The effect of body mass index on complications from cardiac surgery in the oldest old. J Am Geriatr Soc 2002;50:988-94. [DOI] [PubMed]