Abstract
Introduction
Although many options exist for ligament reconstruction in knee dislocations, the optimal treatment remains controversial. Allografts and autografts have both been used to reconstruct the cruciate ligaments. We present the results of reconstruction using artificial ligaments at Hôpital du Sacré-Coeur in Montréal.
Methods
We reviewed the treatment of all patients with knee dislocations seen between June 1996 and October 1999. The Lysholm score, ACL-quality of life (QoL) questionnaire, physical examination and Telos instrumented laxity measurement were used to evaluate the results.
Results
Twenty patients (21 knees) participated in the study. The mean (and standard deviation [SD]) Lysholm score was 71.7 (18). Results from the ACL-QoL questionnaire showed a global impairment in QoL. Mean (and SD) range of motion and flexion were 118° (10.9°) and 2° (2.9°) respectively. Mean (and SD) radiologic laxity evaluated with Telos for the anterior and posterior cruciate ligaments were 6.1 (5.7) mm and 7.3 (4.5) mm respectively.
Conclusions
Knee reconstruction with artificial ligaments shows promise, but further studies are necessary before it can be recommended for widespread use. This is the first study to show specifically a severe impairment in QoL in this patient population.
Abstract
Introduction
Même s'il existe plusieurs possibilités de reconstruction ligamentaire dans les cas de luxation du genou, le traitement optimal suscite toujours la controverse. On a utilisé à la fois les allogreffes et les autogreffes pour reconstruire des ligaments croisés. Nous présentons les résultats de reconstructions au moyen de ligaments artificiels effectuées à l'Hôpital du Sacré-Cœur à Montréal.
Méthodes
Nous avons passé en revue le traitement de tous les patients ayant subi une luxation du genou et qui ont consulté entre juin 1996 et octobre 1999. On a utilisé le score de Lysholm, le questionnaire sur la qualité de vie (QdV) LCA, l'examen physique et la laxité mesurée au Telos pour évaluer les résultats.
Résultats
Vingt patients (21 genoux) ont participé à l'étude. Le score médian de Lysholm (et l'écart type [ET]) s'est établi à 71,7 (18). Les résultats du questionnaire QdV-LCA ont montré un déficit global de la QdV. L'amplitude médiane (et l'ET) du mouvement et celle de la flexion se sont établies à 118 ° (10,9 °) et 2 ° (2,9 °) respectivement. La laxité radiologique médiane (et l'ET) mesurée au Telos dans le cas des ligaments croisés antérieur et postérieur s'est établie à 6,1 (5,7) mm et 7,3 (4,5) mm respectivement.
Conclusions
La reconstruction de genou au moyen de ligaments artificiels est porteuse de promesses, mais d'autres études s'imposent avant que l'on puisse en recommander l'application générale. Il s'agit de la première étude qui montre spécifiquement un déficit grave de la QdV dans cette population de patients.
Knee dislocations are uncommon injuries resulting from both high-energy and low-energy trauma. Motor vehicle collisions, industrial accidents, falls and sports injuries are the leading causes.1,2 There is a high potential for functional impairment from the major trauma to the knee ligaments involved and from associated injuries. Traditionally, the term knee dislocation has been applied, not only to truly dislocated knees but also to knees with rupture of 2 or more of the 4 major knee ligaments, usually involving bicruciate ligament injury.1 Whereas nonoperative treatment was once deemed acceptable,3 it is now mostly reserved for patients with very low functional demands. Open or arthroscopic ligamentous reconstruction is now standard care for most patients.4 However, the optimal reconstructive procedure has yet to be defined. Some surgeons advocate early reconstruction of all ligaments,5,6,7,8 whereas others, fearing increased arthrofibrosis, limit the immediate procedure to surgical reconstruction of the posterior cruciate ligament (PCL) and repair of the posterolateral corner.9,10,11 Autografts and allografts have been used successfully in reconstruction of the cruciate ligaments.
A number of artificial ligaments have been designed for reconstruction of knee ligaments. The ligament augmentation device (LAD) is the prototype. It was designed to reinforce anterior cruciate ligament (ACL) reconstructions.12 After an initial wave of enthusiasm for these implants in the 1980s, their popularity waned owing to their poor long-term survival and their marginal benefits in supplementing autografts. The Ligament Advanced Reinforcement System (LARS; Surgical Instruments and Devices, Arc-sur-Tille, France) represents a new generation of ligament implants. Nau and colleagues13 have recently reported outcomes similar to bone–patellar tendon–bone autografts in a prospective randomized study of ACL reconstruction with 24 months of follow-up.
At Hôpital du Sacré-Coeur in Montréal, early reconstruction of both cruciate ligaments and posterolateral corner with the use of LARS ligaments has been the practice for treating knee dislocations. In this study we wished to evaluate the outcome of our institutional protocol of immediate ligament reconstruction in knee dislocations using LARS artificial ligaments.
Patients and methods
We reviewed the charts, including operative protocols, of all patients treated for knee dislocation by the senior author (P.R.) with a follow-up of at least 1 year. These cases made up all the knee dislocations managed at our institution from June 1996 to October 1999. Data about the traumatic event, associated injuries, operative findings, surgical reconstruction and complications were collected according to a standardized protocol. Injuries were classified according to the anatomy-based Schenck classification: KD-I is a dislocation in which 1 of the cruciate ligaments is intact; KD-II is a tear of both cruciate ligaments with intact collateral ligaments; KD-III are bicruciate injuries with either an associated medial cruciate ligament tear (KD-IIIM) or lateral cruciate ligament tear (KD-IIIL); and KD-IV is a rupture of all 4 major knee ligaments.
Patients were managed initially according to advanced-trauma life support guidelines. Open dislocations were treated emergently with irrigation and debridement. All knees were provisionally stabilized with a knee immobilizer or external fixation (1 case) while awaiting recovery of the soft tissues prior to ligament reconstruction. Angiography was performed selectively depending on the physical findings and the ankle–brachial index.
A medial parapatellar arthrotomy was done in all cases. The knee joint was assessed for damage to the cruciate ligaments, cartilage and menisci. Meniscal tears were repaired when possible. The ACL and PCL stumps were sutured with heavy nonabsorbable suture. Only the anterolateral bundle of the PCL was reconstructed. Guide pins were inserted with use of PCL and ACL drill guides. A guide pin was inserted from the anterior tibia to the PCL footprint. Another guide pin was inserted at the origin of the anterolateral bundle of the PCL. This pin was driven proximally into the femur. A cannulated reamer was then used to create the bony tunnels. ACL tunnels were positioned in a standard fashion. The sutures tied to the PCL and ACL stumps were then fed through the corresponding bony tunnels to ensure realignment of the ligament stumps as described by Marshall et al.14 The LARS ligaments were inserted through the bony tunnels in the tibia and femur and positioned to lie adjacent to the native cruciate ligaments. Secure fixation was achieved with interference screws. The PCL and ACL tunnels have 6 and 7 mm diameters respectively. The interference screws are usually 8 mm in diameter, but larger screws are sometimes used when bone quality appears suboptimal. There was 1 case of bony avulsion from the tibial insertion of the ACL, which was fixed with intraosseous sutures. The collateral ligaments were approached by means of appropriate medial and lateral incisions. Posterolateral corner avulsions from bone were fixed with intraosseous sutures. Mid-substance tears were sutured and reinforced with LARS. Depending on the structures involved, LARS ligaments were positioned to reconstruct the LCL (in bony tunnels in the fibular head and distal femur) or popliteus (in the tibia and distal femur).
Postoperatively, patients followed an intense rehabilitation protocol. A hinged brace was used to protect the collateral ligaments. Patients were only allowed touch weight-bearing at first. Ice and interferential currents were employed to decrease swelling. Indomethacin (25 mg tid for 3 wk) was given to patients without contraindications. The initial phase of the program was aimed at regaining range of motion by passive and active exercises. In between physical therapy sessions, patients were prescribed at-home exercises. As soon as flexion reached 115° patients were started on low-resistance stationary cycling. When adequate muscle strength and control were regained, progressive weight-bearing was allowed. This usually took at least 6 weeks. Focus was then shifted to strengthening with closed-chain exercises, including squats and riding the exercise bicycle with increasing resistance. The next step centred on proprioceptice exercises. Once the swelling had resolved and balance, proprioception and strength had been regained, patients started jogging and moved on to sport-specific drills if jogging was well tolerated. The time of progression through this rehabilitation protocol was highly dependent on the individual patient.
Functional status was evaluated using the Lysholm score.15 Patients were also given the ACL quality of life (QoL) questionnaire.16 One of the authors was available at all times if the patients needed help answering the questionnaire.
All patients underwent clinical examination of the knees by 3 of the 4 authors. Knees were evaluated for ligamentous laxity and range of motion. Neurovascular status of the injured leg was evaluated. Ligament stability was compared to the uninjured knee. It was graded as normal, grade 1 (0–5 mm side-to-side difference), grade 2 (5–10 mm) and grade 3 (> 10 mm) for all knee ligaments. At the time of examination, the examiner was unaware of the results obtained by the other examiners. Range of motion was assessed in a standardized fashion with a goniometer.
Anterior and posterior laxity was also evaluated radiologically with Telos (Telos, Marburg, Germany). A standardized protocol was used. The readings were all done by the same experienced bone radiologist. The ACL was evaluated at 25° of flexion with an anteriorly directed force of 20 kPa. For the PCL, a posteriorly directed force of 15 kPa was used with the knee at 90° of flexion. The same protocol was carried out on the normal side and results of ligamentous laxity were expressed as side-to-side difference. Clinical and radiologic laxities were graded in the same manner.
For statistical analysis, the unpaired t test was used to compare different groups of patients. A p value less than 0.05 was considered statistically significant.
Results
From July 1996 to October 1999, 22 patients were admitted to our institution because of a knee dislocation. Two were lost to follow-up. The other 20 patients (4 female, 16 male; 21 injured knees) made up the study group. The mean age was 28.5 years (range, 15–73 yr). Fourteen dislocations were the result of high-energy trauma.
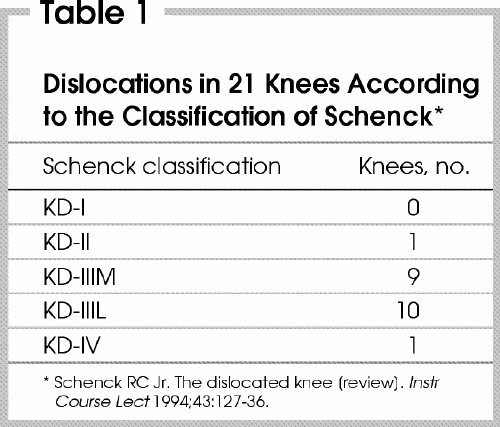
On average, surgery took place 11 days after injury. All patients underwent definitive surgery by 3 weeks after their injuries. The dislocated knees were categorized according to the Schenck classification (Table 1).9 All patients had bicruciate injury. Mean follow-up was 27.4 months; for 13 patients the follow-up was longer than 2 years.
Table 1
There was 1 open dislocation. The knee was debrided on an emergent basis followed by a delayed ligament reconstruction. Two knees had vascular compromise requiring vascular reconstruction; 1 of these 2 patients had a compartment syndrome postoperatively, which was treated by prompt fasciotomy. Eight patients had some degree of peroneal nerve injury. Two (10% of the 22 patients) had complete peroneal nerve palsy; neither recovered. Six presented with incomplete peroneal nerve palsy: 4 recovered completely, 1 was left with an isolated sensory deficit and 1 with weakness (Medical Research Council grade 3) of ankle eversion and dorsiflexion without footdrop. Associated fractures (ipsilateral) included the lateral femoral condyle in 1, medial femoral condyle in 2, tibial plateau in 4 and peroneal head in 2. All were fixed anatomically, and uncomplicated union was achieved. One patient had a deep infection that was sucessfully treated with antibiotics and multiple debridements, allowing retention of the LARS ligaments. Thirteen patients had a meniscal injury. There were 11 tears of the medial meniscus and 9 of the lateral meniscus. Only 2 meniscal injuries were unrepairable and the patient underwent partial menisectomy.
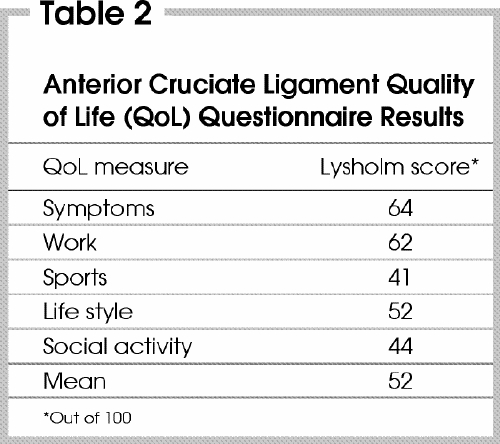
The mean (and standard deviation [SD]) Lysholm score was 71.7 (18). Results of the ACL-QoL questionnaire are shown in Table 2. Mean (and SD) range of motion was 118° (10.9°); mean flexion, 2° (2.9°). To regain a functional range of motion, 2 patients required an arthrolysis. Increased length of follow-up made no statistically significant change in the Lysholm score or range of motion. Mean (and SD) radiologic laxity evaluated with Telos for the ACL was 6.1 (5.7) mm; mean PCL, 7.3 (4.5) mm. There was no statistically significant difference in cruciate laxity between patients with less than 24 months of follow-up and those with more than 24 months. Ten knees had a torn posterolateral corner; 4 were repaired primarily, and 6 reinforced with LARS ligaments. No knees had clinically detectable laxity of the posterolateral corner manifested by increased external rotation of the tibia at both 90° and 45° of knee flexion.
Table 2
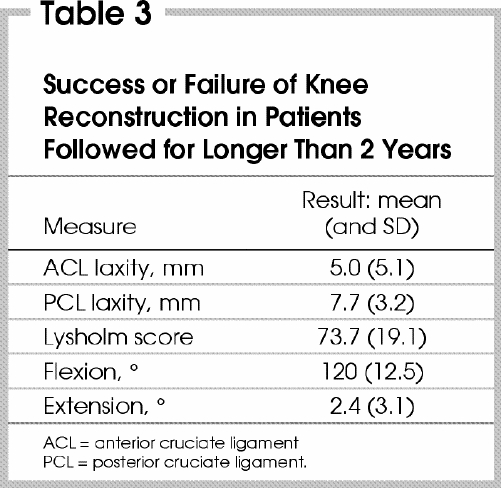
Results for patients with a follow-up longer than 2 years are shown in Table 3.
Table 3
Discussion
The management of knee dislocations remains a challenge even for experienced surgeons, and the optimal reconstructive procedure for the ligamentous component has yet to be decided. Associated injuries can contribute to long-term disability. Popliteal artery involvement and peroneal nerve injury occur in approximately one-third of cases,2,3,17 whereas injury to the tibial nerve occurs less often. In our series, 10% of patients had a permanent footdrop, 45% had associated fractures of the ipsilateral extremity, and 62% had a meniscal injury. These are all confounding variables that complicated the assessment of the surgical results.
The literature on knee dislocations consists mainly of cohort studies. In many cases the results of different types of operative treatment are pooled together. In this study, all patients received uniform treatment. A recent meta-analysis by Dedmond and Almekinders4 compared conservative and surgical treatment. In their study, the Lysholm score, range of motion and flexion contracture were improved by surgical treatment. Richter and colleagues18 also found that surgical treatment yielded better results. However, defining the optimal surgical procedure remains elusive. Some authors advocate early reconstruction of all ligaments whereas others opt for a more conservative approach and in the acute setting reconstruct only the PCL.
Both allografts and autografts have been used to reconstruct the cruciate ligaments in knee dislocations and have advantages and disadvantages. Autografts are familiar to most surgeons, have no potential for disease transmission and do not elicit an immune reaction, but their harvest adds further trauma to the injured knee. Allografts have no donor-site morbidity, are readily available and provide a versatile graft source useful in multiligament-injured knees.19 The potential for disease transmission and their limited availability are, however, potential drawbacks. For knee dislocations treated early, most surgeons will use 1 autograft at most and will resort to allografts if other grafts are needed. Some use allografts exclusively. Artificial ligaments have the same advantages as allografts without the risk of disease tranmission or availability problems; however, previous generations of artificial ligaments have been shown to fail eventually since they have no healing potential.
The goal of this study was to assess the results of a standardized treatment protocol, including early reconstruction of both cruciate ligaments with LARS and to compare our results to those published for autografts and allografts. The Lysholm score, range of motion and cruciate ligament laxity were used for this purpose.
We adopted the Lysholm score to evaluate the functional status of the injured knees. Despite its development for sports injuries this score has been used extensively, allowing easy comparison among studies. A recent study has shown that the Lysholm score is a valid and reliable measure.20 Mean scores ranging from 74.7 to 91.3 have been reported for knee dislocations treated with surgery. The highest score comes from Fanelli's study where bicruciate reconstruction was performed early. Our mean score of 71.7 is lower than other reported scores. However, in one of our patients, rheumatoid arthritis developed postoperatively and severely affected her knee; another had a very painful neurofibroma in the popliteal fossa (present preoperatively) that severely affected her functional status. Excluding these 2 patients raises the average Lysholm score to 74.4.
For ease of analysis we calculated the average range of motion and flexion contracture in the 8 series.5,6,7,8,10,11,21,22,23 In all, there were 109 patients. The average range of motion was 123°; the average fixed flexion contracture, 1.4°. Our results were 118° and 2° respectively. We performed arthrolysis in 2 patients when they failed to reach 90° of flexion at 4 weeks. This was an open procedure with release of all intra-articular adhesions. This rate is similar to that of manipulation under anesthesia or arthrolysis reported by Walker (23%)24, Wascher (15%),8 Yeh (12%)11 and their respective colleagues; Shapiro and Freedman (57%)7; and Noyes and Barber-Westin (18%).6
We assessed cruciate laxity using Telos, whereas previous studies have used the KT-1000 arthrometer for this purpose. Only 3 articles previously reported objective measurements of laxity.5,8,11 All had used the KT-1000 arthrometer (Medmetric, San Diego, Calif.). A recent study comparing the KT-1000 with Telos showed that Telos was more reliable in the evaluation of ACL reconstruction.25 In that study, laxity measured by Telos was on average 3 mm greater than that measured by the KT-1000. This difference between measurement techniques may partly account for the greater ACL laxity in our study compared with others. Wascher and coauthors,8 Yeh and colleagues11 and Fanelli and associates5 reported ACL laxity of 4.6 mm, 4.5 mm and 0.9 mm, respectively, after surgically treated knee dislocations. They reported PCL laxity of 5.1 mm, 4.5 mm and 0.9 mm, respectively. Unfortunately, data comparing Telos and the KT-1000 for PCL reconstruction are lacking. It is therefore diffcult to compare our results for PCL laxity to those of others.
We also evaluated QoL using the ACL-QoL questionnaire. This is an outcome assessment tool designed to study patients with ACL-deficient knees. We opted to use this tool instead of the more general scales such as the 36-item short form survey (SF-36) and EuroQol EQ-5D health outcome measure. The rationale is that the concerns of patients with knee dislocations are probably similar to those with ACL-deficient knees. The ACL-QoL questionnaire evaluates 5 areas relevant to patients with ACL deficiency: symptoms and physical complaints, work-related issues, recreation and sports, lifestyle, and social and emotional issues. In the case of knee dislocations immediately operated upon, it is impossible to evalute the effect of surgery since a preoperative score cannot be obtained. However, to the best of our knowledge these patients all had normal knees preoperatively. The low scores in all 5 areas show the dramatic effect this injury can have on QoL. Ours is the first study to look specifically at this aspect of knee dislocations.
Conclusions
In this short-term study, the use of LARS artificial ligaments for cruciate reconstruction in knees with multiligament injuries seems to give acceptable results. There are many potential advantages to the use of artificial ligaments. However, further research is needed to determine the role of these implants in cruciate ligament reconstruction. Concerns over the risk of rupture must be addressed through long-term studies. To improve management of these injuries studies comparing different treatment options are also needed. We believe that our results warrant further study of LARS ligaments in the context of knees with multiligament injuries. The ACL-QoL questionnaire results confirm the significant impairment in QoL after knee dislocation, and its use should be considered in future studies to allow comparison among studies.
Competing interests: None declared for Drs. Talbot, Berry and Fernandes. Dr. Ranger received travel expenses from J.K. Orthomedic Ltd. to present the preliminary results of this study at a convention related to the subject area of this article.
Correspondence to: Dr. Greg Berry, McGill University Health Centre, Room B5 159.4, Division of Orthopædic Surgery, Montréal General Hospital, 1650 Cedar Ave., Montréal QC H3G 1A4; fax 514 934-8394; greg.berry@muhc.mcgill.ca
Accepted for publication Oct. 16, 2003.
References
- 1.Brautigan B, Johnson DL. The epidemiology of knee dislocations [review]. Clin Sports Med 2000;19:387-97. [DOI] [PubMed]
- 2.Wascher DC, Dvirnak PC, DeCoster TA. Knee dislocation: initial assessment and implications for treatment. J Orthop Trauma 1997;11:525-9. [DOI] [PubMed]
- 3.Taylor AR, Arden GP, Rainey HA. Traumatic dislocation of the knee: a report of forty-three cases with special reference to conservative treatment. J Bone Joint Surg Br 1972;54:96-102. [PubMed]
- 4.Dedmond BT, Almekinders LC. Operative treatment of knee dislocations: a meta-analysis. Am J Knee Surg 2001;14:33-8. [PubMed]
- 5.Fanelli GC, Giannotti BF, Edson CJ. Arthroscopically assisted combined anterior and posterior cruciate ligament reconstruction. Arthroscopy 1996;12:5-14. [DOI] [PubMed]
- 6.Noyes FR, Barber-Westin SD. Reconstruction of the anterior and posterior cruciate ligaments after knee dislocations. Am J Sports Med 1997;25:769-78. [DOI] [PubMed]
- 7.Shapiro MS, Freedman EL. Allograft reconstruction of the anterior and posterior cruciate ligaments after traumatic knee dislocation. Am J Sports Med 1995;23:580-7. [DOI] [PubMed]
- 8.Wascher DC, Becker JR, Dexter JG, Blevins FT. Reconstruction of the anterior and posterior cruciate ligaments after knee dislocation: results using fresh-frozen nonirradiated allografts. Am J Sports Med 1999;27:189-96. [DOI] [PubMed]
- 9.Schenck RC Jr. The dislocated knee [review]. Instr Course Lect 1994;43:127-36. [PubMed]
- 10.Shelbourne KD, Porter DA, Clingman JA, McCarroll JR, Rettig AC. Low-velocity knee dislocation. Orthop Rev 1991;20:995-1004. [PubMed]
- 11.Yeh WL, Tu YK, Su JY, Hsu RW. Knee dislocation: treatment of high-velocity knee dislocation. J Trauma 1999;46:693-701. [DOI] [PubMed]
- 12.Kumar K, Maffulli N. The ligament augmentation device: a historical perspective. Arthroscopy 1999;15:422-32. [DOI] [PubMed]
- 13.Nau T, Lavoie P, Duval N. A new generation of artificial ligaments in reconstruction of the ACL. J Bone Joint Surg Br 2002:84:356-60. [DOI] [PubMed]
- 14.Marshall JL, Warren RF, Wickiewicz TL, Reider B. The anterior cruciate ligament: a technique of repair and reconstruction. Clin Orthop 1979;143:97-106. [PubMed]
- 15.Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop 1985;198:43-9. [PubMed]
- 16.Mohtadi N. Development and validation of the quality of life outcome measure (questionnaire) for chronic anterior cruciate ligament deficiency. Am J Sports Med 1998;26:350-9. [DOI] [PubMed]
- 17.Green NE, Allen BL. Vascular injuries associated with dislocation of the knee. J Bone Joint Surg Am 1977;59:236-9. [PubMed]
- 18.Richter M, Bosch U, Wippermann B, Hofmann A, Krettek C. Comparison of surgical repair or reconstruction of the cruciate ligaments versus nonsurgical treatment in patients with traumatic knee dislocations. Am J Sports Med 2002;30:718-27. [DOI] [PubMed]
- 19.Safran MR. Graft selection in knee surgery: current concepts [review]. Am J Knee Surg 1995;8:168-80. [PubMed]
- 20.Marx RG, Jones EC, Allen AA, Altchek DW, O'Brien SJ, Rodeo SA, et al. Reliability, validity, and responsiveness of four knee outcome scales for athletic patients. J Bone Joint Surg Am 2001;83:1459-69. [DOI] [PubMed]
- 21.Almekinders LC, Logan TC. Results following treatment of traumatic dislocations of the knee joint. Clin Orthop 1992;284: 203-7. [PubMed]
- 22.Montgomery TJ, Savoie FH, White JL, Roberts TS, Hughes JL. Orthopedic management of knee dislocations: comparison of surgical reconstruction and immobilization. Am J Knee Surg 1995;8:97-103. [PubMed]
- 23.Almekinders LC, Dedmond BT. Outcomes of the operatively treated knee dislocation. Clin Sports Med 2000;19:503-18. [DOI] [PubMed]
- 24.Walker DN, Hardison R, Schenck RC. A baker's dozen of knee dislocations. Am J Knee Surg 1994;7:117-24.
- 25.Jardin C, Cantelot C, Migaud H, Gougeon F, Debroucker MJ, Duquennoy A. [Reliability of the KT-1000 arthrometer in measuring anterior laxity of the knee: comparative analysis with Telos of 48 reconstructions of the anterior cruciate ligament and intra- and interobserver reproducibility.] Rev Chir Orthop Reparatrice Appar Mot 1999;85:698-707. [PubMed]


