Abstract
Objective
To determine parents' attitudes toward and acceptance of waiting times for their child's operation.
Design
Waiting times were measured by a cross-sectional method. A descriptive survey was conducted of families with a child waiting for a non-urgent operation.
Setting
A university teaching hospital.
Subjects
Parents of children (age < 20 yr) waiting for non-urgent pediatric general-surgery operations.
Main outcome measures
Parents' concerns and attitudes about waiting for their child's operation, how it was affecting the child and family, how urgent they felt the need for surgery was, and what they thought was a reasonable maximum waiting period.
Results
Of 89 patients waiting for non-urgent pediatric general-surgery operations at the time of the survey, 61% had been waiting > 6 months and 30% > 12 months. Of the 57 families (64%) who returned completed surveys, 94% reported the wait to be emotionally stressful for the family; 81.5% expected their child's quality of life would improve after the operation. As for length of wait, 83% felt that > 3 months was unacceptable, and 98% > 6 months.
Conclusions
Parents of children waiting for pediatric general surgery operations thought that the need for the operation was significantly more urgent then their classification of elective. They felt that waiting periods should not exceed 3 months. Long waiting periods are stressful for both family and child. Parental perceptions are important when considering strategies for wait-list management.
Abstract
Objectif
Déterminer les attitudes de parents à l'égard des périodes d'attente pour l'opération de leur enfant et leur acceptation de celles-ci.
Conception
On a mesuré les temps d'attente par une méthode transversale. On a procédé à une enquête descriptive auprès de familles dont un enfant attendait une intervention non urgente.
Contexte
Hôpital universitaire.
Sujets
Parents d'enfants (âgés de moins de 20 ans) en attente d'une intervention de chirurgie générale pédiatrique non urgente.
Principales mesures de résultats
Préoccupations et attitudes des parents face à l'obligation d'attendre pour l'intervention de leur enfant, répercussions sur l'enfant et la famille, urgence qu'ils attribuaient au besoin de l'intervention chirurgicale et période d'attente maximale qu'ils jugeaient raisonnable.
Résultats
Sur 89 patients qui attendaient une intervention de chirurgie générale pédiatrique non urgente au moment de l'enquête, 61 % attendaient depuis plus de six mois et 30 %, depuis plus de douze mois. Des 57 familles (64 %) qui ont renvoyé les questionnaires remplis, 94 % ont déclaré que l'attente était une cause de stress émotionnel pour la famille et 81,5 % s'attendaient à ce que la qualité de vie de leur enfant s'améliore après l'intervention. Quant à la durée de l'attente, 83 % étaient d'avis qu'il était inacceptable d'attendre trois mois, et 98 %, d'attendre plus de six mois.
Conclusions
Les parents d'enfants qui attendaient une intervention en chirurgie générale pédiatrique étaient d'avis que le besoin de l'intervention était beaucoup plus urgent que ne l'établissait son classement parmi les chirurgies électives. Les périodes d'attente ne devraient pas dépasser trois mois selon eux. Les longues périodes d'attente sont une cause de stress à la fois pour la famille et pour l'enfant. Les perceptions des parents sont des facteurs importants lorsqu'on envisage des stratégies de gestion des listes d'attente.
Waiting for an operation is an emotionally charged issue for Canadians, and this is reflected in their declining approval of the health care system. Their dissatisfaction is due, in no small part, to their frustration with the perception of excessively long waiting times for surgical operations. Physicians share the public's perception. Providers attribute problems to the general lack of accurate and reliable information about waiting lists and wait-list management systems that are woefully inadequate.
Major changes in prioritizing patients for surgical operations and allocation of resources are needed to ensure that patients with the greatest need receive the highest priority. While providers' perceptions and input are the cornerstone to most wait list systems, public perception is important. There has been little published about patients' perspectives on waiting for surgical operations, and no reports of parents waiting on behalf of their children.1,2,3
The success of new wait-list management strategies will depend, in part, on public acceptance. The purpose of this study was to determine parents' concerns and the acceptability of waiting times for non-urgent pediatric general surgery procedures.
Methods
This study is based on a pediatric general surgery service in an urban health region with a referral population base of about 500 000 covering a vast, sparsely populated area. For this study, waiting period was defined as starting when the patient's family and the surgeon (GGM) agreed on the treatment plan. The wait list is created and maintained in cooperation with the regional health authority; it is not audited. A cross-sectional measurement method was used to determine how long respondents had been waiting for operative procedures at the time of the survey.
Parents (a term we use here to include primary caregivers) of patients on the waiting list were surveyed by a postal questionnaire to determine their concerns and attitudes about waiting and how it affects their child and family. There was a single mailing of the survey, without telephone follow-up. Using a 5-point Likert response scale, parents were asked to indicate their level of agreement or disagreement with statements related to their duration of waiting for an operation; the changing status of their child's health; the perceived emotional stress in the child and family; their participation in usual activities; and the improvement anticipated in the child's quality of life.
All patients were entered into the waiting list under the regional health authority category of “elective” surgery, defined by the regional health authority as “patients [who] require surgery, but their condition is not considered to pose an immediate threat to their health or life.” This determination was based on the author's judgement that at the time of assessment the risk of an adverse event while waiting was not greater then those already on the waiting list. Families were asked to rate how urgent they felt the need was for the procedure, using a visual analog scale ranging from not urgent to extremely urgent (just short of an emergency). Additionally, they were asked to judge what maximum waiting time they thought was reasonable for their child's operation.
Results
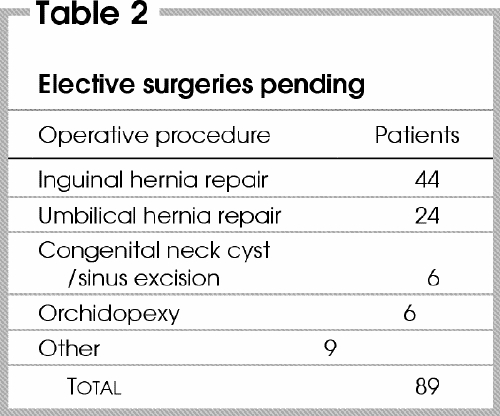
Fifty-seven of 89 surveys (64%) were completed and returned. At the time of the survey, the mean wait for all patients surveyed was 39.2 weeks (95% confidence interval [CI] 4.45 wk) and the median 40 weeks, with a range of 5–72 weeks. Table 1 portrays by 3-month interval the number of patients waiting. The types of operations pending are presented in Table 2.
Table 1
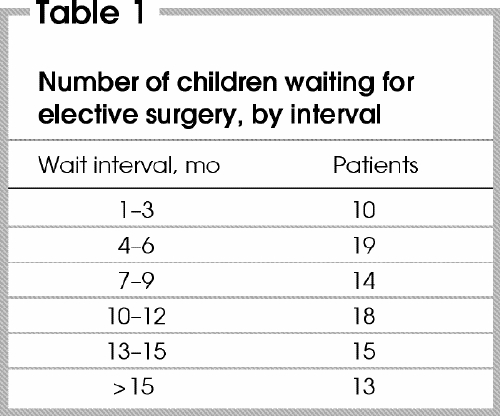
Table 2
Twenty-seven respondents (47%) felt their child's physical health was getting worse while waiting. Waiting was felt to be emotionally stressful for the child in 63%, and for the family in 95% of respondents. Twenty-one respondents (37%) reported that their child's condition prevented them from participating in their usual activities. Improvement in the child's quality of life after the operation was anticipated by 48 (84%).
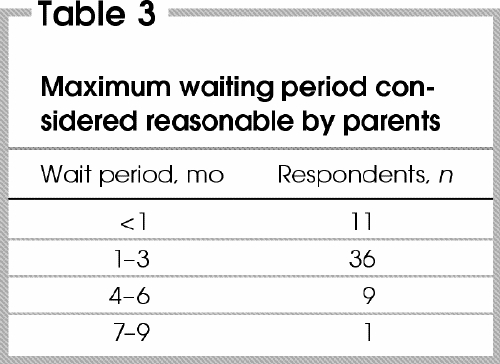
Parents perceived the urgency for their child's operation to be greater than the defined category (Fig. 1). When asked about maximum tolerable wait times, 82% of respondents felt that 3 months or less was reasonable (Table 3).
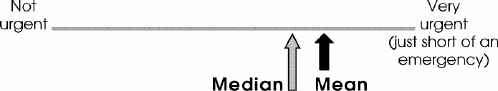
FIG. 1. Visual analog scale showing mean and median scores of parents' evaluations of the urgency of the need for their children's surgery.
Table 3
Discussion
Few studies have been published that evaluate patients' perception of waiting for non-urgent surgical procedures. This is the first report from the perspective of parents whose children are waiting for an operation.
Long waiting periods engender strong emotional responses from parents, as evinced by the large number of respondents in this study who felt waiting was emotionally stressful. Half of the respondents felt that their child's health was adversely affected by waiting, and more than three-quarters felt their child's quality of life would improve once his or her problem was treated. While the procedures were considered by the author and the local health authority to be of a non-urgent nature, the parents had a very different perspective.
Advances in medicine are challenging governments to be fiscally responsible in providing comprehensive health care that meets public expectations. It has been predicted that by 2020, health care costs will increase from 31% to 42% of provincial revenues.4 New strategies or new funds sufficient to reduce waiting times dramatically are difficult to imagine. Rationalization of limited resources has become a well-entrenched part of our publicly funded health care system.
Some argue that there is no actual evidence that a wait list problem exists, and that physician-controlled wait lists may actually put the needs of patients last.5 In the absence of clinical thresholds, physicians may feel compelled to put patients on long wait lists in anticipation of future need. Studies have reported that 15% – 70% of patients are inappropriately placed on lists.6,7,8,9,10 Such rhetoric challenges surgeons to validate their wait lists to ensure best practices are employed and that the process is accountable and transparent. The results of this study have prompted me to adhere to four tasks:
To critically evaluate and apply, where appropriate, available evidence to determine appropriate entry criteria. (Unfortunately, at present, there is little such evidence.)
To ensure that those with the greatest need are treated first, by prioritizing patients with the general surgery prioritization tool being developed by the Western Canada Wait List Project11 and adapting it to the special needs of children.
To audit, by postal questionnaire, patients who have been waiting for longer than 6 months. This has been useful in identifying families that have changed their mind, moved away, or had the procedure done elsewhere.
To inform patients of the option of referral to the next nearest pediatric surgeon, 250 km away.
Immediate access is not essential for non-urgent surgery, and patients will accept some wait, but the wait must be within reason. In a study of patients who have undergone knee replacement, a wait of 8 weeks but not 32 weeks was acceptable.1 In my study, the majority of parents surveyed (83%) would accept a wait of up to 3 months, but only 2% would accept a wait exceeding 6 months.
In summary, parents find prolonged waiting for surgery stressful, and they are concerned about its effect on the well-being of their child. It is noteworthy that parents will accept wait times of 3 months but not more than 6 months. Parental perception is important to the development of wait list management strategies, the success of which will depend on public acceptance.
Competing interests: None declared.
Correspondence to: Dr. Grant G. Miller, Department of Surgery, University of Saskatchewan, Royal University Hospital, 103 Hospital Dr., Saskatoon, SK S7N 0W8; fax 306 966-7988; miller@duke.usask.ca
Accepted for publication May 22, 2003
References
- 1.Ho E, Coyte PC, Bombardier C, Hawker G, Wright JG. Ontario patients' acceptance of waiting times for knee replacements. J Rheumatol 1994;21:2101-5. [PubMed]
- 2.Kee F, McDonald P, Gaffney B. Prioritising the cardiac surgery waiting list: the angina patient's perspective. Heart 1997;7:330-2. [DOI] [PMC free article] [PubMed]
- 3.Llewellyn-Thomas HA, Arshinoff R, Bell M, Williams JI, Naylor CD. In the queue for total joint replacement: patients' perspectives on waiting times. J Eval Clin Pract 1998;1:63-74. [DOI] [PubMed]
- 4.Brimacombe GG, Antunes P, McIntyre J. The future cost of health care in Canada, 2000 to 2020: balancing affordability and sustainability. Ottawa: Conference Board of Canada; 2001.
- 5.Lewis S, Barer ML, Sanmartin C, Sheps S, Shortt SED, McDonald PW. Ending waiting-list mismanagement: principles and practice. CMAJ 2000;162:1297-300. [PMC free article] [PubMed]
- 6.Schou J, Poulsen AL, Nordling J. The anatomy of a prostate waiting list: a prospective study of 132 consecutive patients. Br J Urol 1994;74:57-60. [DOI] [PubMed]
- 7.Tomlinson MB, Cullen J. A clinical audit of patients on an orthopædic waiting list for greater than two years. N Z Med J 1992;105:266-8 [PubMed]
- 8.Barham CP, Pocock RD, James ED. Who needs a prostatectomy? Review of a waiting list. Br J Urol 1993;72:314-7. [DOI] [PubMed]
- 9.The Standards Sub-Committee of the Victoria State Committee of the Royal Australasian College of Surgeons. Surgical waiting lists in Victoria hospitals. Med J Aust 1991;154:326-8. [PubMed]
- 10.Fraser GG. An audit of surgical waiting lists. N Z Med J 1991;104:385-6. [PubMed]
- 11.Western Canada Wait List Project. General Surgery Priority Criteria, Version 1.1, January 2001. Available: http://www.wcwl.org/media/pdf/library/prioritization_tools.6.pdf (accessed 2004 Feb 23).


