Abstract
Background
Laparoscopic splenectomy has become an important therapeutic option in the management of diverse hematologic disorders. However, the incidence of important complications, such as portal vein thrombosis, remains poorly understood. We set out to study the incidence of this complication over a 14-month period.
Methods
All adult patients who underwent laparoscopic splenectomy between July 2001 and April 2002 at McMaster University Medical Centre in Hamilton, Ont., were approached postoperatively and offered duplex ultrasonography of the portal vein to look for thrombosis.
Results
During the study period 17 patients underwent laparoscopic splenectomy. Two patients declined to participate, and in 1 patient the ultrasonography was technically inadequate. Of the 14 remaining patients, 2 (14%) were found to have portal vein thrombosis. In 1 other patient, the investigation was suggestive, but not conclusive, of a clot in the portal system.
Conclusions
Portal vein thrombosis in this series was a relatively common complication of laparoscopic splenectomy. Further research is needed to confirm our findings.
Abstract
Contexte
La splénectomie par laparoscopie est devenue une option thérapeutique importante pour la prise en charge de divers troubles hématologiques. On comprend toutefois encore mal l'incidence de complications importantes comme la thrombose de la veine porte. Nous avons étudié l'incidence de cette complication au cours d'une période de 14 mois.
Méthodes
On a communiqué avec tous les patients adultes ayant subi une splénectomie par laparoscopie entre juillet 2001 et avril 2002 au Centre médical de l'Université McMaster à Hamilton (Ontario) pour leur offrir de se soumettre à une échographie duplex de la veine porte afin de détecter la présence d'une thrombose.
Résultats
Au cours de la période de l'étude, 17 patients ont subi une splénectomie par laparoscopie. Deux patients ont refusé de participer et dans un cas, l'échographie était inadéquate sur le plan technique. On a constaté la présence d'une thrombose de la veine porte chez deux (14 %) des 14 patients restants. Chez un autre patient, l'investigation a indiqué de façon non concluante la présence d'un caillot dans le système porte.
Conclusions
La thrombose de la veine porte dans cette série a constitué une complication relativement courante de la splénectomie par laparoscopie. Une recherche plus poussée s'impose pour confirmer ces constatations.
Laparoscopic splenectomy is less morbid than open splenectomy.1,2 Consequently, acceptance of elective splenectomy to treat hematologic and metabolic disorders has grown. Between Apr. 1, 1998, and Apr. 1, 1999, 32 laparoscopic splenectomies and 13 open splenectomies were performed at McMaster University Medical Centre in Hamilton, Ont. Given this volume of splenic surgery and a shift toward the laparoscopic procedure, it is imperative to further our knowledge concerning the complications of the laparoscopic procedure.
Portal vein thrombosis is a recognized complication of splenectomy.3,4,5,6,7 Studies have suggested that portal vein thrombosis occurs most commonly after splenectomy for myeloproliferative disorders, and rarely after splenectomy for trauma.5,6 Prospective trials on the subject are lacking. Most trials focus on open splenectomy4 or on patients with preexisting portal hypertension.3
Historically, portal vein thrombosis has been considered a potentially catastrophic complication. Acute portal vein thrombosis can cause intestinal infarction secondary to portal hypertension.4,7 Chronic thrombosis can lead to portal hypertension and variceal hemorrhage.4,7 Portal vein thrombosis is usually diagnosed in symptomatic patients. Because screening for clinically occult portal vein thrombosis is not routine, it has been suggested that its true incidence is underestimated.4,5,7 The recommendation to perform routine screening remains controversial,8 and at McMaster University Medical Centre, patients are not routinely screened by ultrasonography after splenectomy.
The rate of portal vein thrombosis after open or laparoscopic splenectomy is not well established. However, in a study of 12 patients who had laparoscopic splenectomy, 1 patient had portal vein thrombosis.9 Because the acceptance of laparoscopic splenectomy is growing, it is important to understand if the unique technical aspects of laparoscopic splenectomy have an impact on the rate of portal vein thrombosis.
Methods
Approval for this trial was obtained from the Hamilton Health Sciences Institutional Review Board. All patients who underwent laparoscopic splenectomy between July 2001 and April 2002, performed by a single surgeon at McMaster University Medical Centre, were asked to participate. Patients were approached at the time of discharge from hospital. The nature of the study and the potential consequences of discovering portal vein thrombosis were explained to the patients. Informed consent was obtained and documented on the chart.
The ideal time to identify portal vein thrombosis by ultrasonography is unknown. In the immediate postoperative period, it has been suggested that visualization may be limited.4 Furthermore, portal vein thrombosis may not occur in the immediate postoperative period.7 Petit and colleagues7 suggested that screening 2 weeks postoperatively may be preferable. To minimize inconvenience for patients, and to allow time to elapse, ultrasonography was coordinated with routine outpatient follow-up.
Patients who agreed to participate underwent duplex ultrasonography of their portal and splenic veins. This investigation has been shown to be highly sensitive and specific for thrombus within the portal system.10,11,12,13,14,15 The presence or absence of thrombus within the splenic and portal venous system was documented, and the results were shared with the attending surgeon.
Differences among patients were analyzed by the t test.
Results
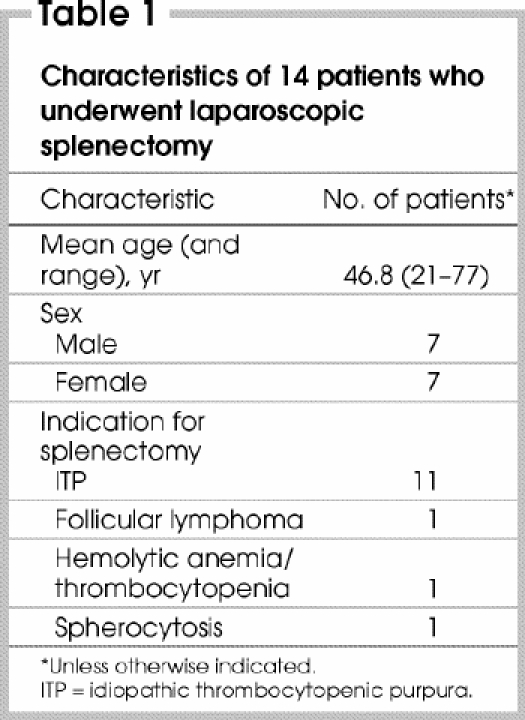
Seventeen patients underwent laparoscopic splenectomy during the study period. Two patients declined to participate. One patient agreed to participate, but the investigation was technically inadequate. This patient was excluded from further analysis. This left 14 patients (7 men, 7 women) (Table 1).
Table 1
No patients included in the study required conversion to an open procedure. The mean time in the operating room (including operative and perioperative time) was 141 minutes (range from 82–210 min). Patients who had evidence of portal vein thrombosis were in the operating room for 148 minutes, versus 139 minutes for those with no evidence of portal vein thrombosis (p = 0.69). Preoperatively, all patients received a subcutaneous injection of heparin. Pneumatic compression stockings were not routinely used. Operations were performed in the right lateral decubitus, reverse Trendeleburg position. Pneumoperitoneum was maintained between 12 and 15 mm Hg.
Ultrasonography was performed at the patients' postoperative follow-up. To accommodate patients and the availability of ultrasonography, the dates of investigation ranged from 1 week to 3 weeks postoperatively. The indication for splenectomy in 11 patients was idiopathic thrombocytopenic purpura (ITP). One patient had follicular lymphoma, 1 had hemolytic anemia and thrombocytopenia, and 1 had spherocytosis. Of the 12 patients who had splenectomy for thrombocytopenia, 10 responded in that their platelet counts rose and medical therapy for thrombocytopenia could be withdrawn.
No patient suffered complications of portal vein thrombosis during the course of study. Two patients (14%) exhibited strong evidence of portal vein thrombosis on screening ultrasonography, and in 1 patient ultrasonography was suggestive, but not conclusive, for portal vein thrombosis. The first patient had splenectomy for ITP, and subsequently symptomatic deep vein thrombosis of the leg was found. This patient received anticoagulant therapy for her thrombosis. Subsequent screening ultrasonography confirmed presence of portal vein thrombosis. Review of the patient's chart revealed that she had been taking oral contraceptives. Preoperatively, this patient's platelet counts had been normal. The indication for splenectomy was failure to stop taking steroids. This patient did not have splenomegaly (spleen weight 123 g).
In the second patient, who was 31 years old, the indication for splenectomy was ITP. Ultrasonography revealed a small amount of nonocclusive clot in the portal vein. This patient had marked preoperative thrombocytopenia. The spleen weighed 278 g.
The third patient (a 73-year-old man) had splenectomy for follicular lymphoma. Ultrasonography suggested a small clot in the superior mesenteric vein at the level of the splenoportal confluence, but the finding was not conclusive. Interestingly, this patient had a history of a pulmonary embolus and was taking coumadin perioperatively. Without preoperative imaging, it is impossible to know whether this clot (if it existed) was the result of splenectomy. The spleen in this patient was enlarged (weight 398 g).
The mean peak postoperative platelet count for the group was 345 х 109/L. The average platelet count of the 3 patients who had evidence of portal thrombosis was 426 х 109/L compared with 327 х 109/L for patients with no evidence of thrombosis. The small population and large variance limits statistical comparison between the groups. The patient who suffered deep vein thrombosis of the leg and the most significant portal vein thrombosis was 755 х 109/L. However, at least 1 patient who did not have portal vein thrombosis also had a postoperative peak platelet count greater than 700 х 109/L.
Discussion
The aim of this study was to estimate the incidence of portal vein thrombosis after laparoscopic splenectomy. We anticipated that the incidence would be approximately 10%, in keeping with studies performed on patients after open splenectomy.
In this study, 2 (14%) of 14 patients had convincing evidence of portal vein thrombosis. Both patients had ITP. A third patient with follicular lymphoma had suggestive evidence of portal vein thrombosis, which would raise the rate of portal vein thrombosis to 21%. None of the patients had complications attributable to their portal vein thrombosis. However, the patient with the most significant degree of thrombosis had received anticoagulant therapy for deep vein thrombosis of the leg. Oral contraceptive use may have been an important precipitating factor in this case. Similarly, the patient with follicular lymphoma and possible portal vein thrombosis had received anticoagulant therapy for a previous pulmonary embolus. These 2 examples emphasize the importance of medical history when judging which patients may be at risk of portal vein thrombosis.
Our study suggests that the risk of portal vein thrombosis after laparoscopic splenectomy is at least as high as for open splenectomy. The small size of the study population limits the conclusions that we can draw. The heterogeneity of diagnoses also makes interpretation difficult. Unfortunately, evaluating occult portal vein thrombosis is resource intensive. In this study, preoperative ultrasonography was omitted primarily because of the increased burden on the radiology department and patient inconvenience. Furthermore, it was felt that ITP patients with a bleeding diathesis were likely at low risk of thrombosis. Certainly studies that did screen patients before open splenectomy did not find preoperative portal vein thrombosis in those with ITP.4 However, this assumption is likely not valid for hematologic malignant conditions.
Conclusions
From the findings of this study, we can conclude that further investigation is justified. Routine surveillance for portal vein thrombosis may be advisable after laparoscopic splenectomy, especially in patients with additional risk factors for thromboembolic disease.
Competing interests: None declared.
Correspondence to: Dr. William Harris, 203 Broadway Ave., Hamilton ON L8S 2W5; fax 617 266-3365; drwharris@hotmail.com
Accepted for publication June 7, 2004.
References
- 1.Schwartz SI. Splenectomy for hematologic disorders. In: Cameron JL, editor. Current surgical therapy. Toronto: Mosby; 1995. p. 545-8.
- 2.Hashizume M, Ohta M, Kishihara F, Kawanaka H. Laparoscopic splenectomy for idiopathic thrombocytopenic purpura: comparison of laparoscopic surgery and conventional open surgery. Surg Laparosc Endosc 1996;6:129-35. [PubMed]
- 3.Eguchi A, Hashizume M, Kitano S, Tanoue K, Wada H, Sugimachi K. High rate of portal thrombosis after splenectomy in patients with esophageal varices and idiopathic hypertension. Arch Surg 1991;126:752-5. [DOI] [PubMed]
- 4.Chaffanjon PC, Brichon PY, Ranchoup Y, Gressin R, Sotto JJ. Portal vein thrombosis following splenectomy for hematologic disease: prospective study with Doppler color flow imaging. World J Surg 1998;22: 1082-6. [DOI] [PubMed]
- 5.Broe PJ, Conley CL, Cameron JL. Thrombosis of the portal vein following splenectomy for myeloid metaplasia. Surg Gynecol Obstet 1981;152:488-92. [PubMed]
- 6.Rattner DW, Ellman L, Warshaw AL. Portal vein thrombosis after elective splenectomy: an underappreciated, potentially lethal syndrome. Arch Surg 1993; 128: 565-70. [DOI] [PubMed]
- 7.Petit P, Bret PM, Atri M, Hreno A, Casola G, Gianfelice D. Splenic vein thrombosis after splenectomy: frequency and role of imaging. Radiology 1994;190:65-8. [DOI] [PubMed]
- 8.Loring LA, Panicek DM, Karpeh MS. Portal system thrombosis after splenectomy for neoplasm or chronic hematologic disorder: Is routine surveillance imaging necessary? J Comput Assist Tomogr 1998;22:856-60. [DOI] [PubMed]
- 9.Valeri A, Venneri F, Presenti L, Nardi F, Grossi A, Borrelli D. Portal thrombosis. A rare complication of laparoscopic splenectomy. Surg Endosc 1998;12:1173-6. [DOI] [PubMed]
- 10.Gallix BP, Taourel P, Dauzat M, Bruel JM. Flow pulsatility in the portal venous system: a study of Doppler sonography in healthy adults. AJR Am J Roentgenol 1997;169:141-4. [DOI] [PubMed]
- 11.Bach AM, Hann LE, Brown KT, Getrajdman GI, Herman SK, Fong Y, et al. Portal vein evaluation with US: comparison to angiography combined with CT arterial portography. Radiology 1996;201:149-54. [DOI] [PubMed]
- 12.Hellinger A, Roll C, Stracke A, Erhard J, Eigler FW. Impact of colour Doppler sonography on detection of thrombosis of the hepatic artery and the portal vein after liver transplantation. Langenbecks Arch Chir 1996;381:182-5. [DOI] [PubMed]
- 13.Harkanyi Z, Temesi M, Varga G, Weszelits V. Duplex ultrasonography in portal vein thrombosis. Surg Endosc 1989;3:79-82. [DOI] [PubMed]
- 14.Alpern MB, Rubin JM, Williams DM, Capek P. Porta hepatis: duplex Doppler US with angiographic correlation. Radiology 1987;162:53-6. [DOI] [PubMed]
- 15.Van Gansbeke D, Avni EF, Delcour C, Engelholm L. Sonographic features of portal vein thrombosis. AJR Am J Roentgenol 1985;144:749-52. [DOI] [PubMed]


