Abstract
Background
Seat-belt compliance in trauma patients involved in motor vehicle collisions (MVCs) appears low when compared with compliance of the general public. In this study we wished to define the relative frequency of seat-belt use in injured Canadian drivers and passengers and to determine if there are risk factors particular to seat-belt noncompliance in this cohort.
Methods
We identified trauma patients who were involved in MVCs over a 24-month period and contacted them 2–4 years after the injury by telephone to administer a standardized survey. Potential determinants of seat-belt noncompliance were compared with the occurrence of an MVC by multiple logistic regression.
Results
Seat-belt noncompliance in 386 MVC patients was associated with drinking and driving, youth, speeding, male sex, being a passenger, smoking, secondary roads, rural residence, low level of education, overnight driving, having no dependents, licence demerit points, previous collisions, unemployment and short journeys. There was an increase in seat-belt awareness and a decrease in self-rated driving ability after the MVC.
Conclusions
Factors that indicate poor driving habits (alcohol, speeding, previous MVCs and driving offences) also predict seat-belt noncompliance. Injury prevention programs should selectively target these high-risk drivers to improve seat-belt compliance and limit associated injury and consumption of health care resources.
Abstract
Contexte
Le port de la ceinture de sécurité chez les patients traumatisés suite à une collision de véhicules à moteur (CVM) semble faible comparativement à celui de la population en général. Dans cette étude, nous voulions définir la fréquence du port de la ceinture de sécurité chez les conducteurs et les passagers canadiens blessés et déterminer s'il y des facteurs de risque particuliers à l'inobservation du port de la ceinture de sécurité dans cette cohorte.
Méthodes
Nous avons identifié des patients traumatisés victimes d'une CVM au cours d'une période de 24 mois et nous avons communiqué avec eux par téléphone de deux à quatre ans après le traumatisme pour leur administrer un questionnaire normalisé. Nous avons comparé au moyen d'une régression logistique multiple les déterminants possibles de l'inobservation du port de la ceinture de sécurité à l'occurrence d'une CVM.
Résultats
On a établi un lien entre l'inobservation du port de la ceinture de sécurité chez 386 patients victimes d'une CVM et la conduite en état d'ébriété, la jeunesse, la vitesse, le fait d'être de sexe masculin, le fait d'être passager, le tabagisme, les routes secondaires, une résidence rurale, un faible niveau d'instruction, la conduite pendant la nuit, le fait de ne pas avoir de personne à charge, la présence de points d'inaptitude sur le permis, des collisions antérieures, le chômage et les déplacements sur de courtes distances. La sensibilisation au port de la ceinture de sécurité a augmenté et l'habileté au volant autoévaluée a diminué après la CVM.
Conclusions
Les facteurs qui révèlent de mauvaises habitudes au volant (alcool, vitesse, CVM antérieures et infractions au code de la route) sont aussi des prédicteurs de l'inobservation du port de la ceinture de sécurité. Les programmes de prévention des blessures devraient cibler sélectivement les conducteurs à risque pour améliorer le port de la ceinture de sécurité et limiter les traumatismes et la consommation de ressources des soins de santé découlant de l'inobservation.
Use of seat belts reduces injury and saves lives in motor vehicle collisions (MVCs).1,2,3,4,5 Unbelted occupants involved in an MVC sustain significantly more trauma to the head, face, chest, abdomen and extremities.6 Unbelted motorists also have a greater hospitalization rate,7 are costly to the health care system,8 account for many lost years of productive life9 and have a higher death rate when involved in MVC trauma.10 These issues are particularly frustrating since MVC injuries are preventable.
Despite the clear effectiveness of seat belts and the knowledge that MVCs are a major cause of injury and hospital admission,10 noncompliance with seat-belt laws in trauma patients involved in MVCs is very high. The reported rate of seat-belt use in this population is only 41%–43%,11,12 a rate that is markedly lower than the overall Canadian national rate of 88%.13 The underlying reasons for this remain unclear.
There are a number of significant risk factors associated with seat-belt nonuse in the general public: male gender,14,15,16,17,18,19,20,21 young age,14,15,16,19,20,21,22 passenger status,14,16,17,21,22 risk-taking,19,21,23,24 rural living,20,21,22 low level of education,21 black or hispanic ethnicity,14,16,25,26 having few dependents or children, smoking, speeding, alcohol consumption before driving15,21 and travelling on secondary roads late in the day.15,27 However, there is a lack of comparable information pertaining specifically to the MVC trauma patient. Male sex, youth, nonwhite ethnicity and low annual income were each associated with seat-belt nonuse in these patients in one recent study.28 Because of the lack of data, seat-belt compliance intervention programs have been forced to broadly target the population as a whole, rather the group most commonly injured during a collision.
Our objective was to define the relative frequency of seat-belt use in injured Canadian drivers and to determine if risk factors particular to seat-belt noncompliance exist in this cohort. The findings could enhance injury prevention strategies for seat-belt promotion by documenting the problem and potentially offering an improved means to target distinct populations.
Methods
Sunnybrook & Women's College Health Sciences Centre is an adult regional trauma centre serving metropolitan Toronto and surrounding areas within Ontario. Most patients (90%) are victims of blunt trauma, with MVCs acting as the primary mechanism (61%).
Data on patients involved in MVCs who presented to the Sunnybrook Regional Trauma Unit between Jan. 1, 1996, and Dec. 31, 1997, and survived to the time of hospital discharge, were analyzed with use of a standardized telephone survey. There was no survey pretest, but each question was founded on associations from the literature and a set of plausible influences from the MVC environment, vehicle and driver. All study patients were contacted at home by the same researcher (C.G.B.). Approval from the institutional ethics review board was obtained before patient contact. The survey consisted of informed consent followed by 34 questions relating to demographics, driving habits, driving history, driving attitudes and seat-belt use.
Independent variables included the following: age; sex; time of day; patient position in the vehicle; type of road; rural residence; educational level; marital status; number of dependents under 18 years of age; licence demerit points; number of previous collisions; alcohol intake; speeding; smoking; income; length of trip; number of passengers in the vehicle; typical seat-belt use as a driver and passenger before the MVC; employment status; employment type; housing tenure; use of an airbag; how the seat belt was used; cellular phone use; self-reporting of driving skills relative to the general public before and after the collision; and the make, model and year of the vehicle. Finally, a question outlining change in driver attitude toward seat-belt use after the MVC was also included. Patient responses were limited to defined choices (e.g., “always,” “mostly,” “sometimes,” “rarely,” “never”).
All supplementary data, including patient age, sex, Injury Severity Score (ISS), Abbreviated Injury Scale (head) (HAIS) score, length of hospitalization and amount of blood transfused were obtained from the Sunnybrook Trauma Program Registry. This database is a concurrent record of all trauma patients, documenting their injuries and trauma associated factors.
To address the possibility of biased survey responses, alternate questionnaires were used to interview 30 of the patients. This survey included 2 unique forms of questions regarding alcohol use before driving and speeding behaviour. The response rate for those who answered “yes” to consuming alcohol before driving was similar in the standard and the modified surveys. Comparable results were also noted for self-reported speeding activity (61.9% v. 60.0%, respectively).
Continuous and categorical variables were compared using the t and χ2 tests. Multiple logistic regression defined the predictive ability of risk factors for seat-belt noncompliance in MVC trauma patients, while controlling for confounding covariates. Stepwise logistic regression analysis was employed with a p value less than 0.05 determining significance. Adjusted and unadjusted odds ratios with 95% confidence intervals were obtained. Within subgroups of independent variables, odds ratios were estimated from logistic regression. No interactions within subgroups were evident.
Results
During the 24-month study period, 567 trauma patients who were involved in MVCs were admitted to the Sunnybrook Trauma Unit; 386 (68%) completed the telephone questionnaire. Of those who did not participate, 142 (25%) could not be located, 34 (6%) refused to participate, and 5 (1%) had died at the time of follow-up.
The average study participant was 38.5 years old, male (64%) and a driver (70%) (Table 1). A mean ISS of 23 with an associated length of hospitalization of 16.2 days, an HAIS of 2 and the need for 2.2 units of blood transfused during hospitalization also characterized the typical respondent. Overall, the patients complied with seat-belt regulations in 52% (201 of 386) of collisions.
Table 1
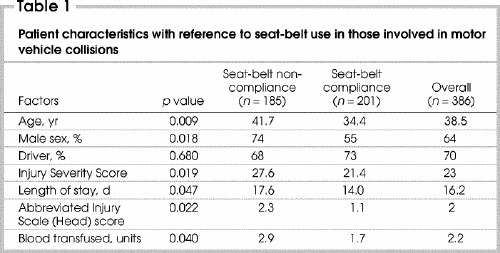
Unbelted patients had a significantly (p = 0.019) higher mean ISS, a longer hospitalization (p = 0.047), an increased HAIS (p = 0.022) and a greater volume of blood transfused (p = 0.040) than patients who had used their seat belts (Table 1).
Specific seat-belt noncompliance rates for each demographic factor in all 386 patients can be reviewed on the Trauma Association of Canada Web site (www.tac.medical.org/videolinks.htm).
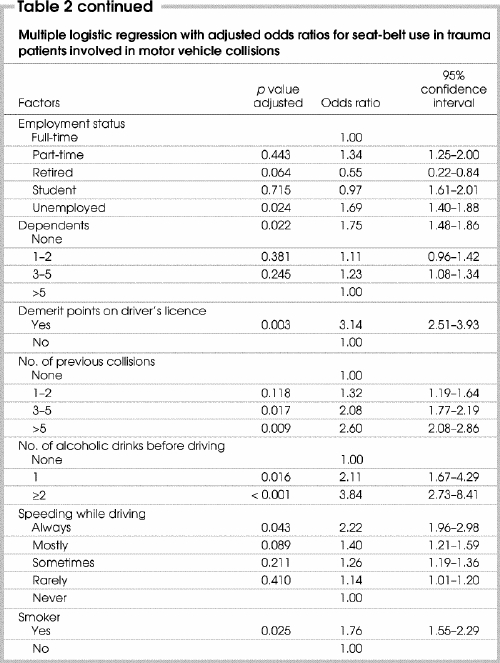
Multivariate analysis (Table 2) indicated that younger age, male sex, low level of education, unemployment, rural residence, rear passenger status and having no dependents under 18 years of age were each predictive of seat-belt noncompliance in MVC trauma. Environmental factors such as driving on smaller, secondary roads, trips of short duration and late at night were also predictive of seat-belt noncompliance, as were factors involving high-risk driving behaviour such as having licence demerit points, previous collisions, drinking alcohol before driving, speeding and smoking. We found that 55.4% of all MVC trauma patients in our study admitted to consuming alcohol before driving. A patient's typical pattern of seat-belt use in the months leading up to the MVC, as either a driver or a passenger, was consistent with seat-belt use at the time of the crash (p = 0.029). Proper seat-belt use (i.e., both lap and shoulder belts) was correlated with seat-belt compliance at the MVC (p = 0.008). Finally, there was an increase in the awareness of seat-belt use (p = 0.021), as well as a decrease in self-rated driving ability (i.e., from “above average” to “average”) (p = 0.040) after an MVC.
Table 2
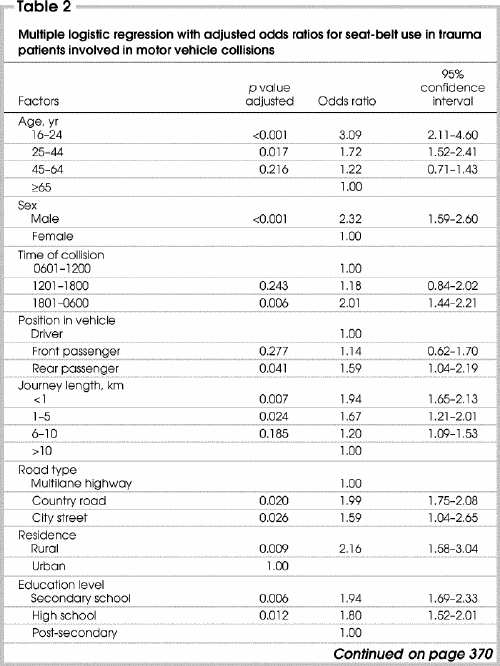
Table 2 continued
Discussion
The findings from our study confirm Porter and Zhao's11 assertion that MVC trauma patients comply with seat-belt regulations less often than those in the general population. It also draws a direct link between seat-belt noncompliance and a significantly increased demand for health resources in this Canadian patient cohort (increased ISS, HAIS, transfusion requirements and longer hospital stays). Furthermore, this study also identified a diverse set of associated factors for seat-belt noncompliance in the specific subset of MVC-related Canadians who are injured. Although some risk factors may not be directly amenable to change, they are crucial to identify and better understand so as to direct future injury prevention strategies.
Although Lerner and associates28 reported independent associations between older age, female sex and driver status with seat-belt use in the injured adult population, others have reported younger age,14,15,16,20,21,22,27,28,29,30 male sex,14,15,16,17,18,19,20,27 passenger status,14,16,17,21,22 living in a rural community,21 low level of education21 and having a limited number of children or dependents21 as risk factors predictive of seat-belt nonuse in the general public only. Our study is the first to confirm that these risk factors retain validity and apply to the MVC trauma population as well. Furthermore, we present unemployment as a previously unidentified nonmodifiable risk factor for seat-belt noncompliance in any population.
This study confirms that driving on secondary roads and travelling late at night15,27 are environmental factors predictive of seat-belt noncompliance in the MVC trauma population. Our data also showed that a short journey (<5 km) was positively associated with seat-belt noncompliance in this population. These findings highlight the need for seat-belt compliance strategies to target the often-neglected motorists from rural communities, travelling short distances on slower secondary roads close to home. Serious MVC injuries may carry a greater than 50% risk of death in rural as opposed to urban settings,31 although these are the same conditions in which seat-belt use is especially effective.27,32 Specific strategies may include increasing public awareness and surveillance in rural settings, as both interventions are often limited outside of large urban centres.
Modifiable risk factors predictive of seat-belt noncompliance in the general population include consuming alcohol before driving,19,21,23,24,33 smoking21,34 and speeding.21,29 We confirmed that these same factors are also predictive in MVC trauma patients. Possessing driver's licence demerit points and a history of 3 or more previous collisions before the MVC are previously unreported risk factors for seat-belt nonuse. Alcohol is a particularly serious factor, as 55.4% of our patients admitted to consuming alcohol before driving. These driver-related factors are the most helpful components for increasing seat-belt compliance and hence directing injury prevention programs. Having license demerit points and previous MVCs represent a window of opportunity where drivers at risk of not wearing seat belts, and hence at risk for injury, can be identified for education.
Although we found no association between seat-belt use in MVC trauma patients and self-reported driving skills, there was a significant change in our study patients' perception of the quality of their driving skills, decreasing from “above average” to “average” after the collision. This group also reported increased awareness of the importance and value of seat belts after their MVC. When coupled with previous data suggesting that MVC involvement increases seat-belt use35 as well as examples of other successful interventions,14,25,36,37,38,39 the potential impact of a well-directed prevention campaign may be significant.
This study has several potential limitations and can be considered a “snap-shot” measure of seat-belt use at the time of injury. First, this study relied on the single-dependent variable of seat-belt use during the MVC. For successful MVC injury prevention, this data point should convey mean seat-belt use on a daily basis for this high-risk population. The observed correlation between typical seat-belt use as a driver or passenger before the MVC and compliance during the crash supports this assumption (p = 0.008 and p = 0.011, respectively). Second, because patient behaviours were reported and not observed, some responses may be biased.19 This is especially relevant for the ethically charged questions where legislation or guilt may have influenced responses. Although this risk cannot be eliminated, it was tempered by a known correlation between seat-belt self-reporting and observed compliance,40,41 the use of bias-reducing terms41 in the survey itself and the statistically similar results of our alternative surveys. Finally, our study only had a moderate response rate. Although the rate is comparable to that for other telephone surveys using similar time frames31,35,42 and was not unexpected in this population, the possibility of excluding a unique subgroup of patients or a unique risk factor exists. It is important that these results, specific to the injured MVC patient, be confirmed in other trauma centres to determine their accuracy.
Despite the enormous discrepancy in seat-belt compliance rates between the general public and MVC trauma patients, documented predictive factors specific to this group have been limited. By increasing seat-belt use in the population with a high likelihood of MVC trauma,43 the tremendous economic1,28 and medical resources required for the treatment of these injured patients may be reduced. Factors that indicate poor driving habits (alcohol, speeding, previous MVC or driving offences) also predict seat-belt noncompliance. Injury prevention programs should selectively target these high-risk drivers to improve seat-belt compliance. These programs may include seat-belt education in demerit reduction programs, increased alcohol roadside checks and stricter penalties in the legal arena.
Presented at the annual meeting of the Trauma Association of Canada, Banff, Alta., Mar. 27–29, 2003.
Competing interests: None declared.
Correspondence to: Dr. Fred D. Brenneman, Trauma Program, Departments of Surgery and Medicine, Sunnybrook and Women's College Health Sciences Centre, C-135,2075 Bayview Ave., Toronto ON M4N 3M5; fax 416 480-4225; Fred.Brenneman@sw.ca
Accepted for publication June 2, 2004.
References
- 1.Marine W, Kerwin E, Moore E. Mandatory seat belts: epidemiologic, financial, and medical rationale from the Colorado matched pairs study. J Trauma 1994;36:96-100. [PubMed]
- 2.Swierzewski M, Feliciano D, Lillis P. Deaths from motor vehicle crashes: patterns of injury in restrained and unrestrained victims. J Trauma 1994;37:404-7. [PubMed]
- 3.Viano D. Restraint effectiveness, availability and use in fatal crashes: implications for injury control. J Trauma 1995;38:538-46. [DOI] [PubMed]
- 4.Evans L. Safety-belt effectiveness: the influence of crash severity and selective recruitment. Accid Anal Prev 1996;28:423-33. [DOI] [PubMed]
- 5.U.S. Department of Transportation National Highway Traffic Safety Administration National Centre for Statistics and Analysis. Traffic safety facts. Washington: Department of Transportation; 1997.
- 6.Orsay E, Dunne M, Turnbull T. Prospective study of the effect of seatbelts in motor vehicle crashes. Ann Emerg Med 1990;19:258-61. [DOI] [PubMed]
- 7.Peterson T. Trauma prevention from the use of seatbelts. Iowa Med 1987;77:233-6. [PubMed]
- 8.Runge J. The cost of injury. Emerg Med Clin North Am 1993;11:241-53. [PubMed]
- 9.Centers for Disease Control and Prevention (CDC). Systematic review of strategies to prevent motor vehicle injuries. Atlanta: CDC; 1999. # 099-5928.
- 10.Millar W, Last J. Motor vehicle traffic accident mortality in Canada. Am J Prev Med 1988;4:220-30. [PubMed]
- 11.Porter R, Zhao N. Patterns of injury in belted and unbelted individuals presenting to a trauma center after a motor vehicle crash: seat belt syndrome revisited. Ann Emerg Med 1998;32:418-24. [DOI] [PubMed]
- 12.Sunnybrook & Women's College Health Sciences Centre Trauma Unit Web site Available: www.sunnybrookandwomens.on.ca/programs/trauma/factsandstats 2003 (accessed 2004 July 1.).
- 13.Transport Canada. Seat belt use in Canada survey results. November 21, 2002. Available: www.tc.gc.ca/mediaroom/releases/nat/2004/04-h107e.htm (accessed 2004 Nov 25).
- 14.Eby DW, Vivoda JM, Fordyce TA. The effects of standard enforcement on Michigan safety belt use. Accid Anal Prev 2002;34:815-23. [DOI] [PubMed]
- 15.Baker DR, Clarke SR, Brandt EN. An analysis of factors associated with seatbelt use: prevention opportunities for the medical community. J Okla State Med Assoc 2000;93:496-500. [PubMed]
- 16.Mayrose J, Jehle DV. An analysis of race and demographic factors among motor vehicle fatalities. J Trauma 2002;52:752-5. [DOI] [PubMed]
- 17.Crandon I, Brandy J, Simeon D. The prevention of seatbelt use in trauma. An observational study. West Indian Med J 1996; 45:31-3. [PubMed]
- 18.Reinfurt D, St. Cyr C, Hunter W. Usage patterns and misuse rates of automatic seatbelts by system type. Accid Anal Prev 1991;23:521-30. [DOI] [PubMed]
- 19.Preusser D, Williams A, Ludn A. Characterization of belted and unbelted drivers. Accid Anal Prev 1991;23:475-82. [DOI] [PubMed]
- 20.Thompson E, Russel M. Risk factors for non-use of seatbelts in rural and urban Alberta. Can J Public Health 1994;85:304-6. [PubMed]
- 21.Sahai V, Pitblado R, Bota G, Rowe B. Factors associated with seat belt use: an evaluation from the Ontario Health Survey. Can J Public Health 1998;89:320-4. [DOI] [PMC free article] [PubMed]
- 22.Shinar D. Demographic and sociomedical correlates with safety belt use. Accid Anal Prev 1993;25:745-55. [DOI] [PubMed]
- 23.Hunt D, Lowestein S, Badgett R, Steiner J. Safety belt nonuse by internal medicine patients: a missed opportunity in clinical preventive medicine. Am J Med 1995;98:343-8. [DOI] [PubMed]
- 24.Wasielewski P. Speed as a measure of driver risk: observed speed versus driver and vehicle characteristics. Accid Anal Prev 1984;16:89-103.
- 25.Davis JW, Bennink L, Kaups KL, Parks SN. Motor vehicle restraints: primary versus secondary enforcement and ethnicity. J Trauma 2002;52:225-8. [DOI] [PubMed]
- 26.Wells JK, Williams AF, Farmer CM. Seat belt use among African Americans, hispanics and whites. Accid Anal Prev 2002;34:523-9. [DOI] [PubMed]
- 27.Petridou M. Person, time and place predictors of seat belt use in Athens, Greece. J Epidemiol Community Health 1998;52:534-5. [DOI] [PMC free article] [PubMed]
- 28.Lerner EB, Jehle DV, Billittier AJ, Moscati RM, Connery CM, Stiller G. The influence of demographic factors on seatbelt use by adults injured in motor vehicle crashes. Accid Anal Prev 2001;33:659-62. [DOI] [PubMed]
- 29.Redelmeier D, Blair P. Survivors of motor vehicle trauma: an analysis of seat belt use and health care utilization. J Gen Intern Med 1993;8:199-203. [DOI] [PubMed]
- 30.Preusser D, Williams A, Ludn A. The effect of New York's seatbelt use law and teenage drivers. Accid Anal Prev 1987;19:73-80. [DOI] [PubMed]
- 31.Grossman DC, Kim A, MacDonald SC, Klein P, Copass MM, Maier RV. Urban–rural differences in prehospital care of major trauma. J Trauma 1997; 42:723-9. [DOI] [PubMed]
- 32.Peterson T, Jolly B, Runge J, Hunt R. Motor vehicle safety: current concepts and challenges for emergency physicians. Ann Emerg Med 1999;34:384-93. [DOI] [PubMed]
- 33.Waller J, editor. Injury control: a guide to the causes and prevention of trauma. Lexington (MA): D.C. Health and Company; 1985. p. 107-60.
- 34.Brison R. Risk of automobile accidents in cigarette smokers. Can J Public Health 1990;81:102-6. [PubMed]
- 35.Passman C, McGwin G, Taylor AJ, Rue LW. Seat belt use before and after motor vehicle trauma. J Trauma 2001;51:105-9. [DOI] [PubMed]
- 36.Steptoe A, Wardle J, Fuller R, Davidsdotir S, Davou B, Justo J. Seatbelt use, attitudes, and changes in legislation: an international study. Am J Prev Med 2002;23:254-9. [DOI] [PubMed]
- 37.Hanfling MJ, Mangus LG, Gill AC, Bailey R. A multifaceted approach to motor vehicle restraint compliance. Inj Prev 2000; 6:125-9. [DOI] [PMC free article] [PubMed]
- 38.Mortimer R. Extra enforcemement and the use of seatbelts by drivers in Illinois. Accid Anal Prev 1992;24:661-6. [DOI] [PubMed]
- 39.Shults RA, Elder RW, Sleet DA, Nichols JL, Alao MO, Crande-Kulis VG, et al. Reviews of evidence regarding interventions to reduce alcohol-impaired driving. Am J Prev Med 2001;21:66-88. [DOI] [PubMed]
- 40.Hunter W, Stewart J, Stutts J, Rodgman E. Observed and self-reported seatbelt wearing as related to prior traffic accidents and convictions. Accid Annal Prev 1993; 25:545-54. [DOI] [PubMed]
- 41.Nelson D. Validity of self reported data on injury prevention behavior: lessons from observational and self reported surveys of safety belt use in the US. Inj Prev 1996;2:67-9. [DOI] [PMC free article] [PubMed]
- 42.Brenneman F, Redelmeier D, Boulanger B, McLellan BA, Culhane JP. Long-term outcomes in blunt trauma: Who goes back to work? J Trauma 1997;42:778-81. [DOI] [PubMed]
- 43.Salzberg P, Yamada A, Saibel C, Moffat J. Predicting seat belt use in fatal motor vehicle crashes from observation surveys of belt use. Accid Anal Prev 2002;34:139-48. [DOI] [PubMed]


