Abstract
Background
Lipofibromatous harmartoma (LFH) is a rare tumour that requires early diagnosis and treatment. To alert physicians to the possibility of this tumour, we review the epidemiologic and pathological characteristics, the presentation, diagnosis and treatment of LFH in the upper extremity.
Methods
We obtained data from a MEDLINE search of the English literature from 1966 to June 2003, using the search terms “lipofibromatous,” “hamartomas of the nerve,” “macrodactyly” and “intraneural lipoma.”
Study selection
Articles that demonstrated institutional experience (epidemiologic, diagnostic and therapeutic, and complications) and those that provided general reviews were selected for inclusion. Of 501 identified articles, 42 fulfilled the review criteria.
Data extraction
Relevant clinical, diagnostic and therapeutic evaluations were extracted from the literature and synthesized.
Data synthesis
LFH is distinguished pathologically from other intraneural tumours by fibrofatty infiltration around the nerve fascicles. Typically, patients present either early with macrodactyly or later with a forearm mass lesion or symptoms consistent with a compressive neuropathy of the affected nerve. Although MRI is an important tool in the diagnosis of LFH, the diagnosis should be supported with a tissue biopsy. Treatment for patients with no neurologic deficit involves prophylactic decompression of affected nerves at all points of possible compression. Patients with macrodactyly may benefit from debulking, joint reconstruction or amputation.
Conclusions
LFH differs from other benign nerve tumours with respect to clinical presentation, pathological characteristics, MRI features and management. Because LFH is extensive and inseparable from the nerve fascicles, excision is not recommended.
Abstract
Contexte
L'hamartome lipofibromateux (HLF) est une tumeur rare qu'il faut diagnostiquer et traiter rapidement. Afin de prévenir les médecins de la présence possible de cette tumeur, nous passons en revue les caractéristiques épidémiologiques et pathologiques, la présentation, le diagnostic et le traitement de l'HLF du membre supérieur.
Méthodes
Nous avons extrait des données par recherche MEDLINE dans des publications en anglais de 1966 à juin 2003 en utilisant les termes «lipofibromatous», «hamartomas of the nerve», «macrodactyly» et «intraneural lipoma».
Sélection des études
On a choisi d'inclure les articles qui démontraient l'expérience de l'établissement (épidémiologie, diagnostic, traitement et complications) et ceux qui présentaient des analyses générales. Sur 501 articles repérés, 42 satisfaisaient aux critères d'examen.
Extraction des données
On a extrait et résumé, à partir des publications, des évaluations cliniques, diagnostiques et thérapeutiques pertinentes.
Synthèse des données
On a établi une distinction, sur le plan pathologique, entre l'HLF et d'autres tumeurs nerveuses par son infiltration de tissus fibrograisseux autour des faisceaux nerveux. Habituellement, les patients se présentent soit au début avec une macrodactylie, soit plus tard avec une masse à l'avant-bras ou des symptômes correspondant à une neuropathie compressive du nerf touché. Même si l'IRM constitue un outil important dans le diagnostic de l'HLF, il faut appuyer le diagnostic par une biopsie tissulaire. Dans le cas des patients qui n'ont pas de déficit neurologique, le traitement comporte une décompression prophylactique des nerfs atteints à tous les points de compression possibles. La chirurgie de réduction tumorale, la reconstruction de l'articulation ou l'amputation peuvent être bénéfiques pour les patients atteints de macrodactylie.
Conclusions
L'HLF diffère d'autres tumeurs nerveuses bénignes sur le plan de la présentation clinique, des caractéristiques pathologiques, des résultats de l'IRM et de la prise en charge. Comme l'HLF est étendu et inséparable des faisceaux nerveux, l'excision n'est pas recommandée.
Lipofibromatous hamartoma (LFH) is a benign, extremely rare intraneural tumour, which needs to be differentiated from other more common peripheral nerve tumours such as intraneural lipomas. It affects the peripheral nerves, most commonly in the upper extremity. Unlike other nerve tumours, LFH cannot be excised but requires early prophylactic decompression at points of potential compression in order to avoid permanent nerve damage. LFH was first reported by Mason1 in 1953 and then by several others.2,3,4 Synonyms for the condition include: fatty infiltration,3 intraneural lipofibroma,5 fibrofatty proliferation,6 lipofibroma,7 and hamartoma,8 but LFH is currently the most accepted name.9 LFH is associated with macrodactyly in more than one-third of cases.10,11 Patients present early in childhood with macrodactyly or later in adolescence with a volar forearm mass. Symptoms consistent with compressive neuropathy of affected peripheral nerves can also occur later in life. Traditionally, management has included decompression of symptomatic nerves at points of compression and debulking of soft tissues or, in patients with severe macrodactyly, amputation. Radical excision of the affected nerve is not recommended. In this review, we will alert physicians to this rare form of nerve tumour that requires early diagnosis and treatment.
Methods
For this review we selected articles from a MEDLINE search of the English language literature from 1966 to June 2003. Further references from the bibliographies of these articles were identified and reviewed. The search terms used were “lipofibromatous,” “hamartomas of the nerve,” “macrodactyly” and “intraneural lipoma.”
Study selection
We identified 501 articles; of these, 42 articles and selected reviews demonstrated institutional experience (epidemiology, diagnosis, treatment, complications) or were general reviews.
Data extraction
From these 42 articles and reviews, we extracted all relevant etiologic, epidemiologic, pathological, diagnostic and therapeutic information and synthesized the data.
Data synthesis
Etiology and epidemiology
The etiology of LFH is unclear, although several potential etiologic factors have been described, including abnormal development of flexor retinaculum in children,7 antecedent trauma12 and chronic nerve irritation.6 Many authors believe that LFH is a congenital condition.3,10 It most commonly manifests well before the third decade, although several reports have described patients who first presented past the fifth decade.13,14,15,16,17 The condition is most common among white people. It occurs sporadically across populations and has no association with neurofibromatosis.18 LFH commonly results in digital enlargement due to an increase in perineural soft tissue and skin. When accompanied by true macrodactyly, the tumour is referred to as macrodystrophia lipomatosa. More than one-third of LFHs are associated with macrodactyly.10,11 Females are more commonly affected when macrodactyly is present;10,11 when LFH is not associated with macrodactyly, both males and females are equally affected.
The distal peripheral nerves are most often affected in LFH; cranial nerve involvement is rare.19 LFH involves the upper extremities 3 times more frequently than the lower extremities, and specifically the median nerve.20,21,22,23,24,25,26,27 Cases of LFH affecting the entire brachial plexus,28 proximal ulnar nerve,14,29 distal ulnar nerve,10 superficial branch of the radial nerve,15,30 superficial peroneal nerve31 and the medial plantar nerve of the foot32 have also been reported.
Pathological findings
Gross findings
On gross pathological examination, LFH consists of lobulated, soft, grey-yellow, sausage-shaped masses within the epineural sheath (Fig. 1). Nerves may be markedly increased in length and diameter in the involved area (Fig. 2); indeed, cases of fusiform median nerve enlargement of up to 17 cm in length and 30 mm in diameter have been reported.17,33 LFH can be extensive and follow nerves even up the brachial plexus. Along their course, the affected peripheral nerves do not adhere to surrounding tissue.12,17,22,34,35 In some instances, hypertrophy of surrounding skin and soft tissue is associated with the enlargement of the bone (macrodystrophia lipomatosa).12

FIG. 1. The typical gross appearance of lipofibromatous hamartoma. This 45-year-old man's right index finger contains multiple soft, grey-yellow, sausage-shaped masses within the epineural sheath of the radial digital nerve. The epineurium of the digital nerve had extensive perineural fibrosis.
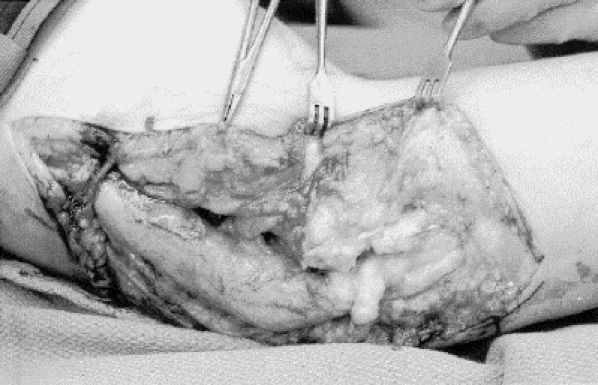
FIG. 2. Significant enlargement can occur in a peripheral nerve affected by lipofibromatous hamartoma. In this 29-year-old man with advanced cubital tunnel syndrome, the ulnar nerve was more than 10 times larger than a typical ulnar nerve, both proximal and distal to the cubital tunnel. The ulnar nerve was slightly enlarged within the cubital tunnel and showed signs of advanced compression.
Microscopic findings
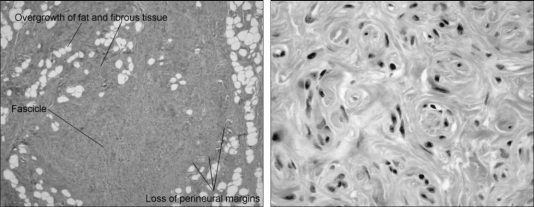
In LFH, the diffuse involvement of the nerve showing relatively bland histologic changes is consistent with a hamartomatous rather than a neoplastic tumour. The lesion is described as a hamartoma because of the overgrowth of the normal connective tissue constituents: fat and fibrous tissue (Fig. 3, left).11,23 Histopathological examination shows infiltration of the epineurium by fibrofatty tissue, which separates and compresses the nerve fascicles. This infiltration causes atrophy of the neural elements,30 often accompanied by extensive perineural fibrosis.10,21,23 Axonal loss and collagen deposition add further chronic changes. In one case reported by Louis and Dick,25 a biopsy specimen of the median nerve showed the presence of fat and heterotopic bone, an occurrence that is very uncommon. The affected nerve may display other features in addition to adipose tissue, such as perineural septation of nerve fascicles and microfascicle formation. Pseudo-onion bulb-like hypertrophic change is an effect of the increase in perineural cells. Although this condition resembles intraneural perineuroma, it should not be misdiagnosed as such (Fig. 3, right).
FIG. 3. Left: characteristic histologic findings in lipofibromatous hamartoma. There is overgrowth of fat and fibrous tissue within the substance of the nerve. Note the fibrofatty infiltration around the nerve fascicles (arrows) with loss of perineural margins (trichrome stain; original magnification х2.5). Right: characteristic pseudo-onion bulb change that may be seen due to an increase in perineural cells. Such changes should not be misdiagnosed as intraneural perineuroma (trichrome stain; original magnification х63).
Histologic differential diagnosis
Other benign soft-tissue tumours in the upper extremity need to be distinguished from LFH; these include neurilemmomas, neurofibromas and intraneural lipomas. LFH differs from other intraneural tumours by its characteristic fibrofatty infiltration around the nerve fascicles. Neurilemmomas and neurofibromas arise from Schwann cells. Neurilemmomas are encapsulated tumours, extrinsic to the nerve fibres and easily separated from the nerve fascicles. Neurofibromas are not encapsulated and show intermingling with the nerve fascicles. Intraneural lipomas arise from normally occurring adipose cells within the nerve; like neurilemmomas, they are encapsulated and easily detached from the nerve fascicles. Finally, intraneural ganglia have been described in the histologic differential diagnosis.36 Unlike LFH, neurilemmomas, intraneural lipomas and intraneural ganglia do not intermingle with nerve fascicles.12,13,36,37,38,39
Clinical presentation
The most frequent presentation of LFH is a swelling or mass on the volar aspect of the wrist or distal forearm. The mass usually appears several years before the onset of neurologic symptoms.26 Neurologic deterioration ensues after some years.36 Associated clinical symptoms include pain and numbness, along with motor and sensory deficits in the median nerve distribution.12,23,36,40 Since most of these tumours involve the median nerve, the symptoms are caused by the compression of this nerve in the carpal tunnel.
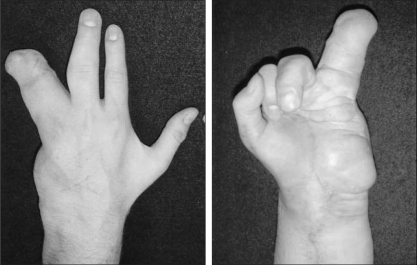
The macrodactyly with which LFH is commonly associated can be present at birth or can be diagnosed during early childhood.39 When present, macrodactyly can be symmetric — involving equally the radial or ulnar sides of the same digit — or asymmetric. Although the phalanges are usually affected, the metacarpals are involved inconsistently. According to Dell,39the involvement of metacarpals often occurs in older patients and is a manifestation of the severity of the disorder. Macrodactyly is unilateral 90% of the time. The majority of patients with macrodactyly present in their first to third decades because of aesthetic concerns (Fig. 4).17
FIG. 4. Left: macrodactyly in the left hand of a 29-year-old man with lipofibromatous hamartoma of the ulnar nerve. Note the massive overgrowth of the ring finger of the left hand and the fullness along the ulnar aspect of the forearm owing to increased size of the ulnar nerve and overlying soft tissues. A ray amputation of the small finger was performed at an early age. Right: the palmar fullness along the hypothenar eminence is also caused by the increased size of the ulnar nerve and overlying soft tissues. Typically, macrodactyly is seen only in the sensory distribution of affected nerve.
Diagnosis
A carefully taken history and physical examination are the cornerstones of the correct diagnosis of LFH. Plain radiographs are valuable for assessing changes in the underlying skeleton when macrodactyly is present (Fig. 5). In some cases, a biopsy of the palmar cutaneous branch or the dorsal ulnar portion of the median nerve has been obtained to confirm the diagnosis. When this is done, the biopsy should be studied by an experienced neuropathologist so that malignant lesions such as neurofibrosarcomas can be ruled out.20,21,36,41

FIG. 5. Characteristic radiologic features associated with macrodactyly in lipofibromatous hamartoma include symmetric overgrowth of the affected phalanges and metacarpal of the thumb and index finger with bony overgrowth concentrated around the metacarpophalangeal and interphalangeal joints.
MRI plays a major role in confirming the diagnosis of LFH. It is now being recommended for all patients suspected of having the condition. Cases are being identified more frequently as the use of MRI increases.17 MRI not only confirms the diagnosis, it also provides a detailed assessment of nerve involvement preoperatively. A characteristic feature on MRI is the appearance of serpentiform nerve fascicles surrounded by fibrofatty tissue within the expanded nerve sheath.29 Distribution of fat between fascicles is asymmetric. On coronal images, the nerve has a spaghetti-like appearance that is pathognomonic for LFH (Fig. 6).17,42 Although MRI is an important tool in the diagnosis of LFH, the diagnosis should be supported with a tissue biopsy, particularly in cases presenting as an asymptomatic mass lesion or in centres without a large clinical experience in dealing with rare peripheral nerve tumours.

FIG. 6. Characteristic features of lipofibromatous hamartoma seen on MRI. This axial image shows serpentiform nerve fascicles (arrows) surrounded by fibrofatty tissue within the expanded nerve sheath. Distribution of fat between fascicles is asymmetric. The nerve has a spaghetti-like appearance that is considered to be pathognomonic for lipofibromatous hamartoma.
Electromyography and nerve conduction studies (EMG-NC) can also provide valuable information needed to confirm a diagnosis of LFH. EMG-NC can show prolonged distal latency of sensory or motor innervation and fibrillations in distal muscles to confirm a compressive neuropathy.11,26,29
Treatment
Surgical excision of LFH is not recommended for several reasons. First, the effects of excision are devastating in terms of motor and sensory function.10,12,21 Second, patients may suffer neurogenic pain after resection. Third, LFH can involve the entire nerve all the way up to the plexus, making the resection margins difficult if not impossible to identify.
In cases of LFH without macrodactyly, most authors agree with a conservative approach that includes decompression of all compromised peripheral nerves to help alleviate pain and paresthesia to reduce the likelihood of permanent motor and sensory sequelae.6,9,12,21,22,41 If the disease is extensive — with marked enlargement of the peripheral nerves as determined by MRI — consideration should be given to prophylactic decompression, even in the absence of motor or sensory symptoms. If LFH is associated with gross macrodactyly in an adult, the preferred procedure is either debulking or amputation of the finger. Amputation of the finger is less frequently indicated in childhood.39 In selected patients, other reconstructive procedures aimed at improving hand function include joint debridement, excision of osseous overgrowth and tendon transfers (i.e., opponensplasty).
Conclusions
Our understanding of this rare benign tumour of the peripheral nerves remains limited. LFH differs from other intraneural tumours owing to its characteristic fibrofatty infiltration around the nerve fascicles, which, unlike other nerve tumours, rules out excision. LFH requires early prophylactic decompression at points of potential compression in order to avoid permanent nerve damage. Patients with significant macrodactyly may benefit from debulking, joint reconstruction or amputation. Patients who present late with advanced disease may benefit from reconstructive procedures aimed at improving hand function. Radical excision of these tumours is not recommended.
Presented in part at the annual meeting of the British Society of Hand Surgery, London, UK, October 2003.
Competing interests: None declared.
Correspondence to: Dr. Dimitri J. Anastakis, Divisions of Plastic and Orthopaedic Surgery, Department of Surgery, University of Toronto, Toronto Western Hospital, University Health Network, 2 East Wing, 399 Bathurst St., Toronto ON M5T 2S8; fax 416 603-6189; dimitri.anastakis@uhn.on.ca
Accepted for publication July 7, 2004.
References
- 1.Mason ML. Presentation of cases: Proceedings of the American Society for Surgery of the Hand. J Bone Joint Surg Am 1953;35:273-4.
- 2.Pulvertaft RG. Unusual tumours of the median nerve. J Bone Joint Surg Br 1964;46:731-3. [PubMed]
- 3.Yeoman PM. Fatty infiltration of the median nerve. J Bone Joint Surg Br 1964;46:737-9. [PubMed]
- 4.Mikhail IK. Median nerve lipoma in the hand. J Bone Joint Surg Br 1964;46:726-30. [PubMed]
- 5.Houpt P, Storm van Leeuwen JB, Van den Bergen HA. Intraneural lipofibroma of the median nerve. J Hand Surg [Am] 1989;14:706-9. [DOI] [PubMed]
- 6.Callison JR, Thoms OJ, White WL. Fibro-fatty proliferation of the median nerve. Plast Reconstr Surg 1968;42:403-13. [PubMed]
- 7.Rowland SA. Case report: ten year follow-up of lipofibroma of the median nerve in the palm. J Hand Surg [Am] 1977;2:316-7. [DOI] [PubMed]
- 8.Paletta FX, Rybka FJ. Treatment of hamartomas of the median nerve. Ann Surg 1972;176:217-22. [DOI] [PMC free article] [PubMed]
- 9.Johnson RJ, Bonfiglio M. Lipofibromatous hamartoma of the median nerve. J Bone Joint Surg Am 1969;51:984-90. [PubMed]
- 10.Silverman TA, Enzinger FM. Fibrolipomatous hamartoma of nerve: a clinicopathologic analysis of 26 cases. Am J Surg Pathol 1985;9:7-14. [DOI] [PubMed]
- 11.Amadio PC, Reiman HM, Dobyns JH. Lipofibromatous hamartoma of nerve. J Hand Surg [Am] 1988;13:65-75. [DOI] [PubMed]
- 12.Guthikonda M, Rengachary SS, Balko MG, Van Loveren H. Lipofibromatous hamartoma of the median nerve: case report with magnetic resonance imaging correlation. Neurosurgery 1994;35:127-32. [DOI] [PubMed]
- 13.Rusko RA, Larsen RD. Intraneural lipoma of the median nerve: case report and literature review. J Hand Surg [Am] 1981;6:388-91. [DOI] [PubMed]
- 14.Gouldesbrough DR, Kinny SJ. Lipofibromatous hamartoma of the ulnar nerve at the elbow: brief report. J Bone Joint Surg Br 1989;71:331-2. [DOI] [PubMed]
- 15.Herrick RT, Godsil RD Jr, Widener JH. Lipofibromatous hamartoma of the radial nerve: a case report. J Hand Surg [Am] 1980;5:211-3. [DOI] [PubMed]
- 16.Kernohan J, Dakin PK, Quain JS, Helal B. An unusual “giant” lipofibroma in the palm. J Hand Surg [Br] 1984;9:347-8. [DOI] [PubMed]
- 17.Marom EM, Helms CA. Fibrolipomatous hamartoma: pathognomonic on MR imaging. Skeletal Radiol 1999;28: 260-4. [DOI] [PubMed]
- 18.Scheithauer BW, Woodruff JM, Erlandson RA. Tumors of the peripheral nervous system. In: Atlas of tumor pathology. Washington: Armed Forces Institute of Pathology; 1997. p. 95-7.
- 19.Berti E, Roncaroli F. Fibrolipomatosis hamartoma of a cranial nerve. Histopathology 1994;24:391-2. [DOI] [PubMed]
- 20.Patel ME, Silver JW, Lipton DE, Pearlman HS. Lipofibroma of the median nerve in the palm and digits of the hand. J Bone Joint Surg Am 1979;61:393-7. [PubMed]
- 21.Louis DS, Hankin FM, Greene TL, Dick HM. Lipofibromas of the median nerve: long-term follow-up of four cases. J Hand Surg [Am] 1985;10:403-8. [DOI] [PubMed]
- 22.Sondergaard G, Mikkelsen S. Fibrolipomatous hamartoma of the median nerve. J Hand Surg [Br] 1987;12:224-6. [DOI] [PubMed]
- 23.Warhold LG, Urban MA, Bora FW Jr, Brooks JS, Peters SB. Lipofibromatous hamartomas of the median nerve. J Hand Surg [Am] 1993;18:1032-7. [DOI] [PubMed]
- 24.Abu Jamra FN, Rebeiz JJ. Lipofibroma of the median nerve. J Hand Surg [Am] 1979; 4:160-3. [DOI] [PubMed]
- 25.Louis DS, Dick HM. Ossifying lipofibroma of the median nerve. J Bone Joint Surg Am 1973;55:1082-4. [PubMed]
- 26.Lowenstein J, Chandnani V, Tomaino MM. Fibrolipoma of the median nerve: a case report and review of the literature. Am J Orthop 2000;29:797-8. [PubMed]
- 27.Bergman FO, Blom SE, Stenstrom SJ. Radical excision of a fibro-fatty proliferation of the median nerve, with no neurological loss symptoms. Plast Reconstr Surg 1970;46:375-80. [DOI] [PubMed]
- 28.Price AJ, Silver JW, Pipton DE, Pearlman HS. Lipofibroma of the median nerve in the palm and digits of the hand. J Bone Joint Surg Am 1970;61:393-7. [PubMed]
- 29.Meyer BU, Roricht S. Fibrolipomatous hamartoma of the proximal ulnar nerve associated with macrodactyly and macrodystrophia lipomatosa as an unusual cause of cubital tunnel syndrome. J Neurol Neurosurg Psychiatry 1997;63:808-10. [DOI] [PMC free article] [PubMed]
- 30.Jacob RA, Buchino JJ. Lipofibroma of the superficial branch of the radial nerve. J Hand Surg [Am] 1989;14:704-6. [DOI] [PubMed]
- 31.Hirakawa E, Miki H, Kobayashi S, Ohmori M, Arima N. Lipofibromatous hamartoma of nerve in the foot. Acta Pathol Jpn 1993;43:265-7. [DOI] [PubMed]
- 32.Ogose A, Hotta T, Higuchi T, Katsumi N, Koda H, Umezu H. Fibrolipomatous hamartoma in the foot: magnetic resonance imaging and surgical treatment: a report of two cases. J Bone Joint Surg Am 2002;84:432-6. [DOI] [PubMed]
- 33.De Maeseneer M, Jaovisidha S, Lenchik L, Witte D, Schweitzer ME, Sartoris DJ, et al. Fibrolipomatous hamartoma: MR imaging findings. Skeletal Radiol 1997;26:155-60. [DOI] [PubMed]
- 34.Frykman GK, Wood VE. Peripheral nerve hamartoma with macrodactyly in the hand: report of three cases and review of the literature. J Hand Surg [Am] 1978;3:307-12. [DOI] [PubMed]
- 35.Kronberger P, Rainer C, Hittmair A, Anderl H. Lipofibromatous hamartoma (neural fibrolipoma) of a flexor nerve of the index finger. Scand J Plast Reconstr Surg Hand Surg 1998;32:237-9. [DOI] [PubMed]
- 36.Louis DS. Peripheral nerve tumors in the upper extremity. Hand Clin 1987;3:311-8. [PubMed]
- 37.Morley GH. Intraneural lipoma of the median nerve in the carpal tunnel. J Bone Joint Surg Br 1964;46:734-5. [PubMed]
- 38.Friedlander HL, Rosenberg NJ, Graubard DJ. Intraneural lipoma of the median nerve. Report of two cases and review of the literature. J Bone Joint Surg Am 1969;51:352-62. [PubMed]
- 39.Dell PC. Macrodactyly. Hand Clin 1985;1:511-24. [PubMed]
- 40.Cavallaro MC, Taylor JA, Gorman JD, Haghighi P, Resnick D. Imaging findings in a patient with fibrolipomatous hamartoma of the median nerve. AJR Am J Roentgenol 1993;161:837-8. [DOI] [PubMed]
- 41.Strickland JW, Steichen JB. Nerve tumors of the hand and forearm. J Hand Surg [Am] 1977;2:285-91. [DOI] [PubMed]
- 42.Khanna G, Sundaram M, Rotman M, Janney CG. Fibrolipomatous hamartoma of the nerve. Orthopedics 2001;24:836, 919-20. [DOI] [PubMed]