Abstract
Background
The introduction of noninvasive laparoscopic surgery has raised concerns about appropriate teaching techniques for medical students considering surgery as a specialization. The principal aim of this study was to determine the effect, between the sexes, of cognitive imaging as a teaching method in the context of learning a surgical technique.
Methods
A randomized treatment-control sample of 42 medical student volunteers was used to test the effect of cognitive imaging on performance and on traditional instructional techniques to help medical students acquire suturing skills specific to laparoscopic surgery.
Results
Repeated-measures analysis of variance showed no significant effect for the use of cognitive imaging (F 1,40 = 0.97, p > 0.05). Males tended to perform better than females in completing tasks that required the use of visual-spatial manipulation of the instruments within a simulated laparoscopic environment (F 1,40 = 5.08, p < 0.05).
Conclusions
These results, which are in concordance with other research findings, indicate that females generally have lower visual-spatial abilities than males. Enhanced performance for both sexes, however, increases rapidly with practice. Other than verbal one-on-one instruction, males on average rank instructional approaches that are applied and visual higher than do females.
Abstract
Contexte
L'avènement de la chirurgie par laparoscopie non effractive soulève des préoccupations au sujet des techniques appropriées d'enseignement aux étudiants en médecine qui envisagent de se spécialiser en chirurgie. Cette étude visait principalement à comparer l'effet, entre les sexes, de l'imagerie cognitive comme méthode d'enseignement dans le contexte de l'apprentissage d'une technique chirurgicale.
Méthodes
On a utilisé un échantillon témoin de traitement randomisé constitué de 42 étudiants en médecine qui se sont portés volontaires pour tester l'effet de l'imagerie cognitive sur la performance et sur les techniques traditionnelles d'enseignement afin d'aider les étudiants en médecine à apprendre à poser des sutures spécifiques à la chirurgie laparoscopique.
Résultats
L'analyse de variance par mesures répétées n'a montré aucun effet important dans le cas de l'utilisation de l'imagerie cognitive (F1,40 = 0,97, p > 0.05). Les hommes ont eu tendance à produire de meilleurs résultats que les femmes dans l'exécution des tâches exigeant l'utilisation de la manipulation visuospatiale des instruments dans un environnement laparoscopique simulé (F1,40 = 5,08, p < 0,05).
Conclusions
Ces résultats, qui concordent avec ceux d'autres recherches, indiquent que les femmes ont en général des habiletés visuospatiales moindres que les hommes. La performance s'améliore toutefois rapidement avec la pratique chez les deux sexes. Mis à part l'enseignement verbal individualisé, les hommes classent en moyenne les méthodes pédagogiques appliquées visuelles à un niveau plus élevé que les femmes.
The introduction of noninvasive laparoscopic surgery1 has raised concerns about whether such procedures can be simulated or if learning strategies can be identified that will provide appropriate surgical skill training to medical students considering surgery as their specialty. As laparoscopic surgery relies on the use of video or camera images to complete procedures, surgeons must rely heavily on their visual-spatial skills. Risucci and colleagues2 concluded that the development of visual-spatial perception should be incorporated into the instructional component of teaching surgical technical skills. The ability to manipulate instruments within the abdomen of a patient during laparoscopic surgery requires that the operator can clearly envision a 3-dimensional situation. Suturing in laparoscopic surgery is one of the more advanced technical skills to be acquired by a surgeon.3 The main purpose of our study was to determine the effect of cognitive imaging (which can be defined as a cognitively imaged symbolic rehearsal of a physical activity with the intent of learning and improving the task in the absence of any gross muscular movements4) as a teaching method that supports the cognitive component of motor skill acquisition in learning a surgical technique.
Findings from neuropsychological testing of surgeons have demonstrated that visual-spatial perception — the ability to represent in one's mind the physical environment and the movement to be performed — is the major determinant of technical performance in laparoscopic surgery.5,6,7 In particular, surgical proficiency has been purported to be related to a collection of nonverbal cognitive and psychomotor abilities that encompass complex visual-spatial organization.8,9 Studies of surgical trainees have showed that visual-spatial representation (e.g., ability to represent cognitively a 3- dimensional situation) and somatosensory memory (the ability to remember object shapes and their relationships by feel) are key components of surgical proficiency.3,8 Other researchers have demonstrated the importance of cognitive functions in executing motor skills, particularly in sport psychology.10,11 On the basis of these findings, strategies to support the cognitive phase of learning, such as cognitive imaging, have been studied and have shown sex differences in visual-spatial abilities12 and potential benefit to improved performance13,14,15,16,17,18 and motor-skill acquisition.8,19 The process of cognitive imaging promotes the development of a cognitive image and facilitates the coordination of movements required to perform the task proficiently.
In an extensive review of research into sex differences, Maccoby and Jacklin20 reported that males generally perform better on spatial ability tasks than do females. Linn and Petersen21 conducted a meta-analysis of research studies whose results used a cognitive and psychometric rationale to separate studies into 3 relatively homogeneous spatial task categories. Tests of spatial perception, defined as the ability to determine spatial relations despite distracting information, yielded a mean effect size of d = 0.44 (95% confidence interval [CI] 0.04–0.84, p < 0.05). Tests of mental rotation, defined as the ability to rotate quickly and accurately 2- or 3-dimensional figures in imagination, showed a mean test effect size of d = 0.73 (95% CI 0.50–0.96, p < 0.05). Tests of spatial visualization, defined as the ability to manipulate complex spatial information when several stages are needed to produce the correct solution, yielded a mean effect size of d = 0.13 (95% CI –0.24 to 0.50, p > 0.05). A subsequent meta-analysis of 286 studies of sex differences on spatial abilities showed that males outperformed females with an overall mean weighted d = 0.37 (z = 2.61, p < 0.01).22 With use of the same criteria to differentiate tests, results by age showed that effect sizes increased with the age of the study participants sampled in all 3 categories of spatial abilities. In particular, sex differences in children under 13 years of age had the smallest effect sizes and those over 18 years old had the largest effect sizes for spatial perception ([d = 0.33, p > 0.05; d = 0.48, p < 0.05], mental rotation [d = 0.33, p < 0.05; d = 0.66, p < 0.05] and spatial visualization [d = 0.02, p > 0.05; d = 0.23, p < 0.05]). Conversely, females excel in the acquisition of literacy skills from early childhood23 and the differences continue to widen on verbal tasks into adolescence.20 The sex differences in verbal tasks vary from large to small, but the greatest advantage is found in specific executive speech abilities related to speed of articulation, and accuracy of speech production and fluency. Although these findings indicate that males perform better on average than females on specific spatial tasks, these differences are assumed to reflect variations in patterns of abilities rather than a connection to overall intellectual functioning.24
Since the introduction of the laparoscopic approach, there has been an ongoing continuing education movement among practising surgeons to become familiar with minimally invasive surgical techniques.25 Although the relationship between performance in a simulated environment and the ability to complete the same procedure in actual surgery is inconclusive, the ability to complete a task improves with repeated practice.26,27,28,29 Moreover, increased experience with laparoscopic surgery is related to a reduction in operative time and complication rates.25 In support of motor skill performance, Meehan and Georgeson30 describe a surgical performance curve that improves substantially during the initial phase of skill acquisition development. Subsequently, the initial part of the performance curve is very steep, then flattens until improvement levels out with each completed surgical procedure.
The complexity of laparoscopic surgery is reflected in practice and is acknowledged as an advanced skill usually performed by highly trained, experienced surgeons. Laparoscopic suturing differs largely in the level of difficulty when compared with a traditional suturing of skin through direct visualization. In laparoscopic suturing, long thin instruments (graspers) are inserted through very small incisions into the abdomen. A camera introduced through a separate incision projects an image on a television monitor that guides the surgeon. The image, however, only provides a magnified 2-dimensional image of the 3-dimensional structures within the abdomen. The absence of a direct line of vision into the suturing area distorts depth perception and substantially increases the level of difficulty in performing such tasks.
Acquisition of motor skills has been described as occurring in 3 phases: a cognitive phase where the steps of procedures are learned; an associative phase where the tasks are completed with continuous reference to the steps (executive routine); and an autonomous phase where execution is smooth and devoid of extensive reference to the executive routine.31,32,33 Supporting the cognitive phase of the learning process has been shown to have an impact on student performance.32,34 Multiple modalities of providing feedback — visual, perceptual and cognitive — have been shown to be effective. Teaching surgical skills usually follows this model piece by piece until the learner can assemble each component into more free-flowing performance. On the other hand, this model does not explain very well the refinements of surgical skills and the quality differences in the execution.
Current findings offer little information about specific techniques that may facilitate learning medical or surgical technical skills.35,36 This learning of technical skills is usually completed with use of the apprenticeship model, through which the learner is exposed to surgical procedures and over the course of a few years is given the opportunity to practise components of these interventions until they are mastered. The learner then progresses to more complicated procedures that are usually composed of previously acquired skills.37,38 In 2002, Seymour and colleagues39 demonstrated the benefit of using simulation training sessions with residents to reduce error risk on a subsequent assisted laparoscopic surgery dissection. The execution of the fine motor skills necessary in the visually and spatially limited field of laparoscopic surgery make cognitive imaging a potential learning strategy for trainees. In this study, therefore, we evaluated the effectiveness of cognitive imaging for the acquisition of laparoscopic surgical skills. Specifically, we examined the use of a variety of formal learning strategies (i.e., one-on-one instruction, schematic diagrams, previewing of suture and graspers, video demonstration and practice) that focus on the cognitive process of imaging. The emphasis was on understanding the importance of various instructional strategies that may facilitate medical students' learning performance in a simulated laparoscopic surgery exercise.
Method
Participants
Forty-two first- and second-year undergraduate medical students (mean age 24.2 yr, standard deviation [SD] 3.0) voluntarily participated in the completion of 2 laparoscopic suturing training sessions (each 1 h long and separated by a 1-wk interval). Students were randomly assigned to either the control (n = 22) or intervention (n = 20) groups (an equal number of males and females were assigned within each of the 2 groups). The average age of students in each group was 24.3 and 24.0 years respectively. Sex differences in average ages were 24.9 years for males and 23.4 years for females. Any student with previous experience in microscopic or video-assisted surgical techniques was excluded from the study.
Procedures
The laparoscopic suturing procedure was conducted through a simulated model (laparoscopic training apparatus) of a patient's abdominal cavity. Suturing instruments (needle drivers) are inserted through separate incisions that can manipulate abdominal contents while the medical student visualizes the process using the image projected from a camera onto a television monitor. This study also focused on the use of learning methods and strategies to help medical students acquire suturing skills (consisting of suturing and knot tying) specific to video-assisted laparoscopic surgical procedures.
All participants were provided with the following instructional strategies or techniques:
One-on-one instruction was provided consistently throughout each session
Schematic diagrams were used to illustrate how the procedure should be completed
Previewing was provided of suture thread and needle and graspers before the trials began
Video demonstration (approximately 2 min long) was given of initial suturing tasks to be replicated (i.e., cam recorder at 0°)
Suturing was to be practised through direct visualization
Suturing was to be practised with a television monitor view or cam recorder set at 0°
Suturing was to be practised with a television monitor view or cam recorder set at 45°
A bead manipulation task was given using the laparoscopic training apparatus
During the first session of practice trials, each participant received initially one-on-one instruction by the facilitator, a video demonstration of the expected suturing task, and descriptions of the process, procedures and equipment used in the simulated laparoscopic suturing study. This was followed by 5 separate trial attempts by the participant to replicate the suturing process in the laparoscopic training apparatus while supervised by the facilitator (consistent verbal instructions were provided through each of the attempted suturing trials). The first 2 trials were performed through direct visualization (looking directly into the simulated open body cavity) and the remaining 3 trials involved the use of the television monitor with a cam recorder positioned between the graspers (referred to as cam @ 0°). All of the suturing trials used a preset silk thread, suture needle (0 Silk on FSL needle) to suture a small incision made in a piece of latex that was repositioned consistently for each attempted trial. Once the suture needle was passed through both sides of the incision, the student was required to complete a knot by manipulating the thread to tie 3 half-hitches.
In addition to receiving the same learning components as the control group, the intervention (cognitive imaging) participants were provided with formal instruction in the use of cognitive imaging on the completion of the television monitor with cam recorder trials (3–5). During the 1-week interval, the intervention participants were asked to use cognitive imaging as a learning strategy to assist them in visualizing the suturing task as completed in the last 3 video-assisted suturing tasks from the first session. A 1-page journal record was given to the students to complete and return to ensure that the recommended minimum of 2 cognitive imaging sessions was attempted each day during the interval period.
One week later, both groups of participants were asked to return to complete the final 6 trials; 2 trials (6 and 7) with the cam recorder again set initially at 0°, 2 trials (8 and 9) with the cam recorder set at 45° (altering the visual perception of the same suturing task), and the last 2 trials (10 and 11) with the cam recorder set again at 0° but involving a complex bead manipulation task that used the same instruments and trainer apparatus as the suturing tasks (i.e., transfer of skills to new tasks). Participants in the intervention group were asked to return their journal record sheet and use the same cognitive imaging strategy that they used during the 1-week interval before attempting suturing trials 6–9.
The medical students were informed that the principal outcome measure (dependent variable) was the time (seconds) it took them to complete the suturing and bead manipulation tasks. The quality of the performance was not assessed because the previous piloted trials with the trainer apparatus showed that any qualitative differences in the participants' ability to complete the task was reflected in their recorded times. An exit questionnaire was completed by the participants at the end of the second session. All participants were asked to provide their perceptions of the instructional strategies, difficulty of tasks and ability to visualize an image on a 5-point Likert scale (strongly disagree–strongly agree). In addition, participants in the intervention group were asked if they found the use of cognitive imaging useful between trials and during the 1-week interval.
Results
Cognitive imaging
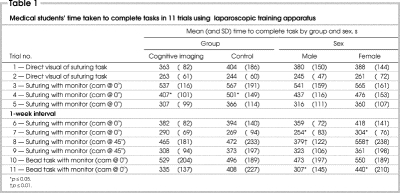
The use of cognitive imaging over the 1-week interval did not show any measurable benefit to the intervention group's performance in the second session (Table 1). Although the intervention participants appeared to benefit initially from the introduction of cognitive imaging after trial 2 (Fig. 1), a 1-way repeated-measures analysis of variance (ANOVA) showed no significant performance differences between the 2 groups on the trials that followed 1-week later (F 1,40 = 0.97, p > 0.05).
Table 1
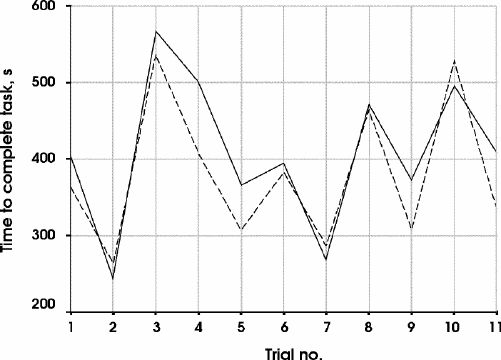
FIG. 1. Average trial times (see Table 1 for description of trials) for cognitive imaging (dashed line) and control (solid line) groups.
Sex differences
Males consistently demonstrated better performance overall and, in particular, in those trials that required the use of camera-assisted tasks (Table 1). Over progressive trials requiring the visual-spatial manipulation of instruments (Fig. 2), a repeated-measures ANOVA revealed that males performed better than females on the completion of tasks (F 1,40 = 5.08, p < 0.05). This trend was apparent during the second session as significant differences between the sexes were shown for half of the trials and on each of the 3 different tasks presented to the medical students. The overall mean average effect size of the combined trials was d = 0.42 (p < 0.05).
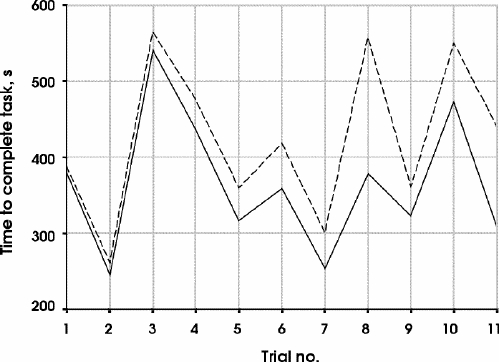
FIG. 2. Average trial times (see Table 1 for description of trials) by sex. Solid line = male, dashed line = female.
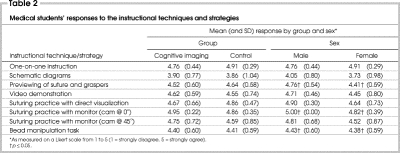
With respect to the instructional approaches used during the course of this study, participants were asked to recommend each technique on a scale of 1 (strongly disagree) to 5 (strongly agree). On average, suturing practice with the cam @ 0° and one-on-one instruction were considered to be the most important teaching strategies (Table 2). The use of a video demonstration of the suturing task and previewing of the equipment were considered to be less important, and the bead manipulation task and the use of schematic diagrams were considered to be least important by both groups. By sex, one-on-one instruction was the preferred and only instructional technique ranked higher by female than male medical students. On average, males scored the use of cognitive imaging between trials (M = 4.30, SD = 0.82) and during the 1-week interval (M = 4.05, SD = 0.67) higher than females (M = 3.82, SD = 0.98; and M = 4.00, SD = 1.10 respectively).
Table 2
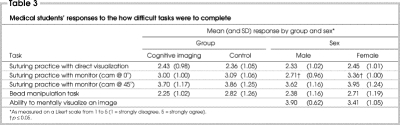
Females usually found the camera-assisted suturing tasks more difficult than males (Table 3), these results being significant only with the cam @ 0°. When the medical students were asked to rank their ability to mentally visualize an image from 1 (impoverished image lacking colour and detail) to 5 (extremely vivid and detailed coloured image), males reported better mental visualization than females (F 1,40 = 3.75, p = 0.06).
Table 3
Discussion
The main findings of our study are as follows: there may be a marginal benefit from cognitive imaging in the early stages of skill acquisition of video-assisted surgical tasks; although the treatment group appeared to benefit initially from the introduction of cognitive imaging, no effect was observed on the remaining trials 1 week later; a comparison of the 4 separate groupings showed that potential benefits from cognitive imaging are inconclusive; and finally there are sex differences in performance (time) of video-assisted suturing and bead manipulation tasks on the completion of initial trial procedures. These results are in concordance with other research that suggests males perform better on visual-spatial representation.
The importance of psychomotor practice was shown to be a vital learning strategy for medical educators in developing better teaching or facilitation methods for surgery. In our study, for both sexes each progressive practice of any particular task reduced the time to complete the procedure by minutes in most cases. In that practice enhances the surgical learning or performance curve of medical students, the use of simulated laparoscopic procedures to enhance motor skills development is important to promote early in medical school. Although females recommended one-on-one instruction as the most important strategy (verbal feedback) and males placed greater emphasis on the suturing practice as a whole (stressing the task-oriented and problem-solving component of completing the procedure itself), on average participants agreed that all of the teaching strategies used in the study were effective for learning laparoscopic surgical techniques.
Although the results of this study did not provide support for the cognitive imaging techniques used, there are a number of potential limitations that may have impeded our efforts to demonstrate the effectiveness of this approach. First, training in the use of cognitive imaging is relatively new to this discipline and will benefit from future testing and articulation of “best” practice techniques. Second, the effect size differences anticipated in this cognitive imaging procedure may have actually required a substantially large sample of medical students to achieve any level of significance. Third, the independent outcome measure used in this study may have benefited from a more rigorous list of criteria that would have incorporated both quantitative and qualitative measures of successful performance outcomes. As such, the use of cognitive imaging in the context of learning a surgical technique will need to be validated by further research by experts in the medical education and surgical community.
As indicated earlier, the 3 distinct categories relating to sex differences in spatial abilities are based on tests of spatial perception, mental rotation, and spatial visualization. Whereas general testing for these abilities are limited to singular tasks (e.g., respondents are asked to identify from 4 options a standard item that has been orientated differently), in our study the relative complexity and duration of the tasks involved several spatial abilities. In future studies, more consideration should be given to sequencing the laparoscopic suturing task to delineate and measure discrete components in relation to each spatial ability category. Accordingly, further research in the use of cognitive imaging in laparoscopic surgery should explore suturing procedures that are less ambiguous, categorized spatially and allow for numerous trials on any particular task.
A preliminary version was presented at the annual meeting of the American Education Research Association, Seattle, Wash., Apr. 10–14, 2001.
Competing interests: None declared.
Correspondence to: Dr. Tyrone Donnon, Assistant Professor, Medical Education and Research Unit, Department of Community Health Sciences, Faculty of Medicine, University of Calgary, 3330 Hospital Dr. NW, Calgary AB T2N 4N1; fax 403 270-2681; tldonnon@ucalgary.ca
Accepted for publication Aug. 3, 2004.
References
- 1.Meyer G, Hüttl TP. Laparoscopic surgery in Europe: development and education. Surg Endosc 2001;15:229-31. [DOI] [PubMed]
- 2.Risucci, DA, Tortolani, AJ, Leitman, IM, et al. Construct validation of a visual perceptual factor in surgical technical skill [abstract]. Focus on Surg Educ 1993; 10:22.
- 3.DesCôteaux JG, Leclère H. Learning surgical technical skills. Can J Surg 1995; 38:33-8. [PubMed]
- 4.Richardson A. Cognitive imaging: a review and discussion. Part I. Res Q 1976; 38:95-107.
- 5.Kaufman HH, Wiegand RL, Tunick RH. Teaching surgeons to operate — principles of psychomotor skills training. Acta Neurochir (Wien) 1987;87:1-7. [DOI] [PubMed]
- 6.Kopta JA. The development of motor skills in orthopaedic education. Clin Orthop 1971;75:80-5. [DOI] [PubMed]
- 7.Lippert FG, Spolek GA, Kirkpatrick GS, Briggs KA, Clawson DK. A psychomotor skills course for orthopaedic residents. J Med Educ 1975;50:982-3. [DOI] [PubMed]
- 8.Schueneman AL, Pickleman R, Freeark RJ. Age, sex, lateral dominance, and prediction of operative skill among general surgery residents. Surgery 1985;98:506-14. [PubMed]
- 9.Schueneman AL, Pickleman R, Hesslein MA, Freeark RJ. Neuropsychologic predictors of operative skill among general surgery residents. Surgery 1984;96:288-93. [PubMed]
- 10.Denis M. Visual imagery and the use of cognitive imaging in the development of motor skills. Can J Appl Sport Sci 1985;10:4S-16S. [PubMed]
- 11.Feltz DL, Landers DM. The effects of cognitive imaging on motor skill learning and performance: a meta-analysis. J Sports Psych 1983;5:25-7.
- 12.Weiss EW, Kemmler G, Deisenhammer EA, Fleischhacker WW, Delazer M. Sex differences in cognitive functions. Pers Individ Dif 2003;35:863-75.
- 13.Bachman K. Using mental imagery to practice a specific psychomotor skill. J Contin Educ Nurs 1990;21:125-8. [DOI] [PubMed]
- 14.Bucher L. The effects of imagery abilities and mental rehearsal on learning a nursing skill. J Nurs Educ 1993;32:318-24. [DOI] [PubMed]
- 15.Clark L. The effect of cognitive imaging on the development of a certain motor skill. Res Q 1960;31:560-9.
- 16.Maring JR. Effects of cognitive imaging on rate of skill acquisition. Phys Ther 1990;70:165-72. [DOI] [PubMed]
- 17.Richardson A. Cognitive imaging: a review and discussion. Part II. Res Q 1976; 38:262-73.
- 18.Rakestraw PG, Irby DM. The use of cognitive imaging in pelvic examination instruction. J Med Educ 1983;58:335-40. [DOI] [PubMed]
- 19.Koslow RE. Sex-related differences and visual-spatial mental imagery as factors affecting symbolic motor skill acquisition. Sex Roles 1987;17:521-7.
- 20.Maccoby E, Jacklin C. The psychology of sex differences. Stanford: Stanford Press; 1974.
- 21.Linn MC, Petersen AC. Emergence and characterization of gender differences in spatial abilities: a meta-analysis. Child Dev 1985;56:1479-98. [PubMed]
- 22.Voyer D, Voyer S, Bryden MP. Magnitude of sex differences in spatial abilities: a meta-analysis and consideration of critical variables. Psychol Bull 1995;117:250-70. [DOI] [PubMed]
- 23.Harris L. Sex differences and spatial ability: possible environmental, genetic and neurological factors. In: Kinsbourne M, editor. Asymmetrical function of the brain. London: Cambridge University Press; 1978. p. 405-522.
- 24.Halpern DF. Sex differences in cognitive abilities. 2nd ed. Hillsdale (NJ): Erlbaum; 1992.
- 25.Rogers DA, Elstein AS, Bordage G. Improving continuing medical education for surgical techniques: applying the lessons learned in the first decade of minimal access surgery. Ann Surg 2001;233:159-66. [DOI] [PMC free article] [PubMed]
- 26.Rosser JC, Rosser LE, Savalgi RS. Objective evaluation of a laparoscopic surgical skill program for residents and senior surgeons. Arch Surg 1998;133:657-61. [DOI] [PubMed]
- 27.Derossis AM, Bothwell J, Sigman HH, Fried GM. The effect of practice on performance in a laparoscopic simulator. Surg Endosc 1998;12:1117-20. [DOI] [PubMed]
- 28.Chung JY, Sackier JM. A method of objectively evaluating improvements in laparoscopic skills. Surg Endosc 1998;12:1111-6. [DOI] [PubMed]
- 29.Anastakis DJ, Regehr G, Reznick RK, Cusimano M., Murnaghan J, Brown M, et al. Assessment of technical skills transfer from the bench training model to the human model. Am J Surg 1999;177:167-70. [DOI] [PubMed]
- 30.Meehan JJ, Georgeson KE. The learning curve associated with laparoscopic antireflux surgery in infants and children. J Pediatr Surg 1997;32:426-9. [DOI] [PubMed]
- 31.Gagne RM. The conditions of learning. 4th ed. Orlando: Holt, Rinehart and Winston; 1985.
- 32.MacKay DG. The organization of perception and action. A theory for language and other cognitive skills. New York: Springer-Verlag; 1987.
- 33.Schmidt RA. A schema theory of discrete motor skill learning. Psychol Rev 1975;82: 225-60.
- 34.West CK, Farmer JA, Wolff PM. Instructional design: implications from cognitive science. Englewood Cliffs (CA): Prentice Hall; 1991.
- 35.Barnes RW. Surgical handicraft: teaching and learning surgical skills. Am J Surg 1987;153:422-7. [DOI] [PubMed]
- 36.Doheny MO. Cognitive imaging: an alternative approach to teaching motor skills. J Nurs Educ 1993;32:260-4. [DOI] [PubMed]
- 37.Reznick RK. Teaching and testing technical skills. Am J Surg 1993;165:358-61. [DOI] [PubMed]
- 38.Knowles M. The adult learner — a neglected species. 4th ed. Houston: Gulf Publishing; 1990.
- 39.Seymour NE, Gallagher AG, Roman SA, O'Brien MK, Bansal VK, Andersen DK, et al. Virtual reality training improves operating room performance: results of a randomized, double-blinded study. Ann Surg 2002; 236:458-64. [DOI] [PMC free article] [PubMed]