Abstract
Introduction
Hydatid disease, a clinical entity endemic in many sheep- and cattle-raising areas, is still an important health problem in the world. Extrapulmonary location of cysts in the thorax is rare. We report our experience with intrathoracic but extrapulmonary hydatid cysts and discuss concepts of treatment.
Method
In our Thoracic and Cardiovascular Surgery Department at the Dicle University School of Medicine, 133 patients with thoracic hydatid cysts were managed surgically between January 1990 and October 2002. In 14 (10.5%), the cysts were extrapulmonary but within the thorax, located in the pleural cavity, mediastinum, pericardium and diaphragm, or in pleural fissures. Cysts were intact in 12 patients and ruptured in 2. Radiographs of the chest were the main means of diagnosis; all patients with mediastinal and diaphragmatic cysts and some with pleural cysts were also scanned with computed tomography. All patients were managed surgically.
Results
We operated on 3 mediastinal, 2 diapragmatic and 1 pericardial hydatid cyst, as well as 6 in pleural fissures and 2 in the pleural space. Lateral thoracotomy was chosen as the surgical incision in all patients except 1 (7% of the 14), who had median sternotomy for a pericardial hydatid cyst. Empyema developed in 2 patients (morbidity, 14%). No patient died perioperatively.
Conclusions
Hydatid cysts may be found in many different sites. Surgery to obtain a complete cure is the treatment of choice for most patients with intrathoracic but extrapulmonary cysts; excision must be done without delay to avoid or relieve compression of surrounding vital structures.
Abstract
Introduction
L'hydatidose, entité clinique endémique dans de nombreuses régions d'élevage de moutons et de bovins, demeure un important problème de santé dans le monde. La localisation extrapulmonaire des kystes dans le thorax est rare. Nous présentons un compte rendu de notre expérience des kystes hydatiques intrathoraciques mais extrapulmonaires et discutons de concepts de traitement.
Méthode
Au département de chirurgie thoracique et cardiovasculaire de la Faculté de médecine de l'Université Dicle, 133 patients ayant des kystes hydatiques thoraciques ont été traités chirurgicalement entre janvier 1990 et octobre 2002. Dans 14 (10,5 %) des cas, les kystes étaient extrapulmonaires mais intrathoraciques, situés dans la cavité pleurale, sur le médiastin, le péricarde et le diaphragme, ou dans les fissures pleurales. Les kystes étaient intacts chez 12 patients et rupturés dans 2 cas. La radiographie thoracique a constitué le principal moyen de diagnostic. On a soumis à une tomodensitométrie tous les patients ayant des kystes au médiastin et au diaphragme et certains de ceux ayant des kystes pleuraux. Tous les patients ont été traités par chirurgie.
Résultats
Nous avons excisé chirurgicalement 3 kystes au médiastin, 2 au diaphragme et 1 au péricarde, ainsi que 6 autres dans les fissures pleurales et 2 dans la cavité pleurale. On a choisi la thoracotomie latérale comme incision chirurgicale sur tous les patients sauf un (7 % des 14), qui a subi une sternotomie médiane à cause d'un kyste hydatique au péricarde. Deux patients ont été atteints d'empyème (morbidité, 14 %). Aucun patient n'est mort pendant la période périopératoire.
Conclusions
Des kystes hydatiques peuvent se former à divers endroits. La chirurgie visant à produire une guérison complète est le traitement privilégié chez la plupart des patients ayant des kystes intrathoraciques mais extrapulmonaires. Il faut procéder à l'excision sans tarder afin d'éviter la compression des structures vitales voisines, ou de la soulager.
Hydatid disease is a parasitosis caused by Taenia echinococcus. It is common in many sheep- and cattle-raising areas, notably the Mediterranean countries, South America, the Middle East, New Zealand and Australia.1,2 In Turkey, the prevalence of hydatid disease is said to be 20 in one million.3
Echinococcal cysts may develop in almost any part of the body except the hair, teeth and fingernails.4 Extrapulmonary location of a cyst in the thorax is very rare. Enlarged cysts can produce compression symptoms. The most serious complication is cyst rupture, which can cause anaphylactic shock and even death.
Here we present our experience and the diagnostic methods in 14 patients with hydatid cysts in extrapulmonary sites within the thorax, and options for their surgical treatment.
Material and methods
Between January 1990 and October 2002, we reviewed 14 cases of hydatid disease located in the thorax but not involving the lung. During the same period 119 patients with pulmonary hydatid disease were also treated surgically in our centre.
Preoperative diagnosis was based primarily on chest radiography (Fig. 1), along with computed tomography (CT), magnetic resonance imaging (MRI) and echocardiography.
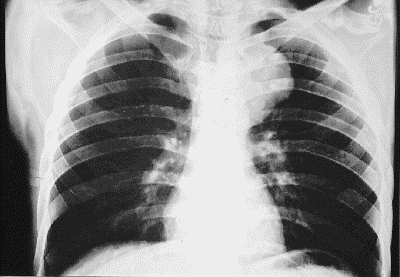
FIG. 1. Chest radiograph showing a hydatid cyst located in the mediastinum.
Posterolateral thoracotomy or median sternotomy were standard approaches in all patients. When a hydatid cyst was identified during surgery, the surgical wound and adjacent tissue were covered with gauze soaked in 10% povidone–iodine. Hydatid fluid was aspirated from the cyst through a 20-gauge needle connected to a 50-mL glass syringe. Following this, the same volume of 10% povidone–iodine was injected into the cyst. After 10–15 minutes this solution was aspirated and a total excision performed. After resection of a mediastinal cyst, the mediastinal pleura was repaired. In 1 patient the diaphragm was repaired by an interrupted suture technique using nonabsorbable sutures.
Results
The series consisted of 14 patients (9 male and 5 female) aged 6–60 years (median, 27 yr). All patients were treated surgically, with no medical treatment beforehand.
For diagnosis we used chest films in all cases, thoracic ultrasonography in 9 (64%), thoracic CT in 11 (79%), MRI in 1 (7%) and echocardiography in 1 (7%).
The cysts found were most commonly pleural (8 patients, 57%; Table 1). Among these, we found 6 cysts in various fissures and 2 in the pleural space. Three patients had mediastinal echinococcal cysts (2 anterior and 1 posterior); in these patients, CT was helpful in making the preoperative diagnosis (Fig. 2). In 1 patient with a pericardial hydatid cyst (Fig. 3 and Fig. 4), we established a preoperative diagnosis with CT and echocardiography. Two hydatid cysts in the diaphragm were found; MRI was helpful in localization (Fig. 5). The diaphragm was repaired after cyst removal.
Table 1
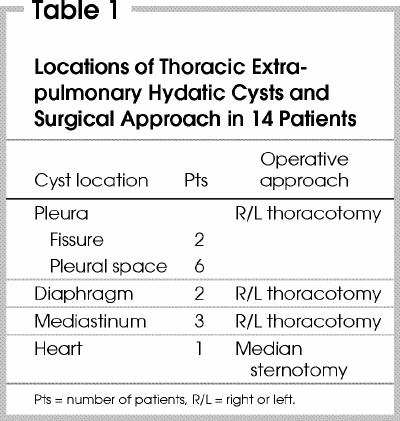
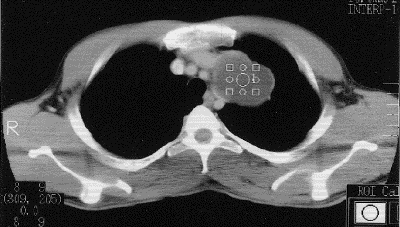
FIG. 2. The CT appearance of a mediastinal hydatid cyst.
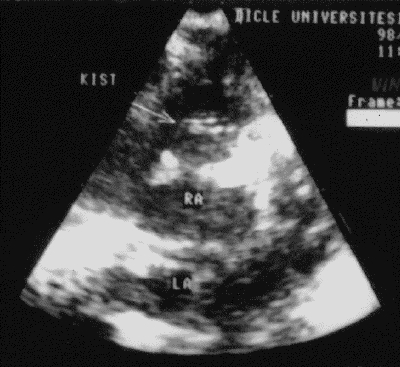
FIG 3. Echocardiographic image of a pericardial hydatid cyst.

FIG. 4. MRI of a pericardial (but extrapulmonary) hydatid cyst.
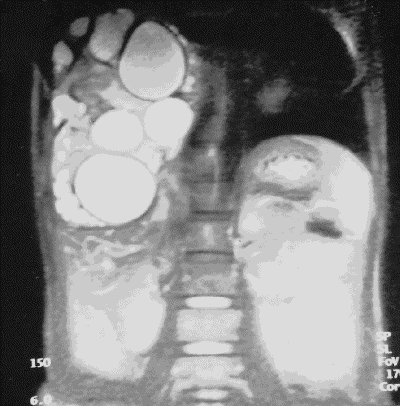
FIG. 5. MRI of a diaphragmatic hydatid cyst.
Six pleural cysts were detected in various fissures, attached by a stem to the visceral pleura. Two cysts were found in the pleural cavity, attached to both the visceral and the parietal pleura. Three cysts located in the mediastinum were close to the aorta and esophagus. Mediastinal cysts caused minimal symptoms of digestive compression. Hydatid cysts of the diaphragm showed no relationship to the lungs.
We performed a right thoracotomy in 9 patients and left thoracotomy in 4. The patient with pericardial hydatid cysts was managed by median sternotomy; cardiopulmonary bypass was not established. The radiologic and clinical diagnoses of hydatid cysts were confirmed by pathological examination.
No patients died perioperatively in our series, but there was 14% morbidity after surgery. In 2 patients who each had an infected cyst, empyema of the ipsilateral pleural cavity developed and was successfully treated with tube drainage. In these 2 patients, the hydatid cysts occurred in the right and left oblique fissures, respectively. The median postoperative hospital stay for uncomplicated cases was 10 days; for complicated cases, 17 days. In our series, there was no recurrence of disease.
Discussion
Hydatidosis is a parasitic disease caused by the larval growth of the tapeworm Echinococcus granulosus.2,5 Echinococcal cysts may develop in almost any part of body; the liver is the most commonly affected area in adults, followed by the lung. In the Turkish population, 54% of cases of hydatid disease involved the liver and 35% affected the lung.3,6
The intrathoracic location is common for hydatid cysts, usually as pulmonary cysts, whereas chest-wall, mediastinal, pericardial, myocardial, fissural and pleural-space locations have been reported for extrapulmonary intrathoracic cysts. Most of these were attached to the visceral pleura by a thin pedicle.5 In our series of extrapulmonary intrathoracic cysts, various fissures and the pleural space were the most common sites. Cysts in fissures were indeed attached by a thin pedicle to the visceral pleura.
The diaphragm is a less common area of involvement with hydatid cysts, usually needing repair after cyst removal.5 In our series, 1 of 2 patients with diapragmatic hydatid cysts required diaphragmatic repair.
Hydatid cysts are rarely present in the mediastinum, although around 100 cases have been described.7,8 About 36% of primary mediastinal cysts have been found in the thymic area of the anterior mediastinum.8 Large mediastinal cysts compress vital organs such as the esophagus, heart, trachea and great vessels, producing pressure symptoms.
The clinical manifestations of extrapulmonary intrathoracic hydatid cysts are similar to those of other cysts. Distinguishing hydatid disease from other problems may be extremely difficult, even with CT. Mistaken diagnoses can include diaphragmatic, dermoid, neuroenteric or enterogenous duplication cysts or masses. Intrathoracic extrapulmonary cysts should be suspected whenever another organ is involved with hydatid cysts. We use posteroanterior and lateral radiography, ultrasonography, CT and MRI to assist in diagnosis.
Chest radiography, our main diagnostic method, provided useful information about the anatomic location of the cyst. Radiographically, a cyst appears as a smooth, round, dense opacity. Chest CT was also helpful, providing information about the morphologic characteristics of cysts and their exact position in the thorax.5,9,10 CT may demonstrate mediastinal echinococcosis if there are daughter cysts, but is otherwise not diagnostic.11,12 The germinative membrane may be visible by CT. Such scans are helpful in showing the water density in intact cysts, but in complex cysts the increased density can be confused with mass lesions. Echocardiography should be used for myocardial and pericardial hydatid cysts, and MRI for extensions of primary diaphragmatic hydatid cysts. We believe that CT is necessary for all mediastinal cysts and should also be used in patients with pleural hydatid cysts, especially when a cyst is perforated or infected.
Skin tests, complement fixation, blood eosinophil count and indirect hemagglutination tests can also be used for diagnostic purposes, but one must remain aware of their tendency toward false-positive results. We do not use them routinely.
Chemotherapy alone is not dependable in controlling this disease.1,6,13 We do not use medical treatment in preoperative preparation. In addition to the side effects, complications occur mostly because of perforation of the cysts during medical treatment with albendazole or mebendazole. We believe that chemotherapy should be used only to prevent secondary recurrences. Medical treatment was applied postoperatively in patients with perforated cysts and the person with the pericardial hydatid cyst.
Conclusions
Intrathoracic but extrapulmonary hydatid cysts are uncommon. They may produce compression symptoms in surrounding vital structures. The therapy of choice should be surgical excision without delay, regardless of the strength of symptoms.
Competing interests: None declared.
Correspondence to: Dr. Refik Ülkü, Thoracic and Cardiovascular Surgery Department, Dicle University School of Medicine, Diyarbakir, 21280 Turkey; fax 90 412 2234141; refiku@dicle.edu.tr
Accepted for publication Apr. 15, 2003.
References
- 1.Burgos R, Varela A, Castedo E, Roda J, Carlos G, Serrano S, et al. Pulmonary hydatidosis: surgical treatment and follow-up of 240 cases. Eur J Cardiothorac Surg 1999;16:628-35. [DOI] [PubMed]
- 2.Dhaliwal RS, Kalkat MS. One-stage surgical procedure for bilateral lung and liver hydatid cysts. Ann Thorac Surg 1997;64:338-41. [DOI] [PubMed]
- 3.Dogan R, Yüksel M, Çetin G, Süzer K, Alp M, Kaya S, et al. Surgical treatment of hydatid cysts of the lung: report on 1055 patients. Thorax 1989;44:192-9. [DOI] [PMC free article] [PubMed]
- 4.Gupta RK, Kakkar AK, Bhagat R, Pant KC. Phrenomediastinal echinococcosis. Chest 1990;98:1528-30. [DOI] [PubMed]
- 5.Oguzkaya F, Akçali Y, Kahraman C, Emirogullari N, Bilgin M, Sahin A. Unusually located hydatid cysts: intrathoracic but extrapulmonary. Ann Thorac Surg 1997;64:334-7. [DOI] [PubMed]
- 6.Özçelik C, Inci I, Toprak M, Eren N, Özgen G, Yasar T. Surgical treatment of pulmonary hydatidosis in children: experience in 92 patients. J Pediatr Surg 1994;29:392-5. [DOI] [PubMed]
- 7.Heras F, Ramos G, Duque JL, Garcia-Yuste M, Cerazal LJ, Matilla JM. Mediastinal hydatid cysts: 8 cases. Arch Bronconeumol 2000;36:221-4. [DOI] [PubMed]
- 8.Shields TW. Mesothelial and other less common cysts of the mediastinum. In: Shields TW, LoCicero J 3rd, Ponn RB, editors. General thoracic surgery. Vol. 2, 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2000. p. 2423-35.
- 9.Karnak I, Çiftçi AO, Tanyel FC. Hydatid cyst: an unusual etiology for a cystic lesion of the posterior medistinum. J Pediatr Surg 1998;33:759-60. [DOI] [PubMed]
- 10.Von Sinner WN, Linjawi T, Al Watban JA. Mediastinal hydatid disease: report of three cases. Can Assoc Radiol J 1990;41:79-82. [PubMed]
- 11.Mathur RK, Doda SS, Buxi TB, Talwar JR. Primary mediastinal echinococcosis. J Comput Tomogr 1985;9:195-7. [DOI] [PubMed]
- 12.Shields TW. Primary lesions of the mediastinum and their investigation and treatment. In: Shields TW, editor. General thoracic surgery. 4th ed. Philadelphia: Williams and Wilkins Media; 1994. p. 724-66.
- 13.Michael S, Misiakos EP, Dosios T, Manti C, Lambrou P, Skalkeas G. Surgical treatment for lung hydatid disease. World J Surg 1999;23:1181-5. [DOI] [PubMed]


